Abstract
Obesity is officially recognised as a chronic disease and a top public health priority by several global societies and healthcare bodies. In some European countries, the majority of the adult population is either overweight or obese, with major implications for patient health and healthcare systems. General practitioners (GPs) are well-placed to tackle this epidemic, yet their engagement with patients is fraught with challenges and barriers. These include time limitations, a lack of evidence base, sensitivities around raising the topic of obesity with patients, inadequate availability of supporting local weight loss services, a lack of training for healthcare professionals (HCPs) on the management of obesity and a limited number of effective therapies. A number of steps need to be implemented to promote engagement between GPs and individuals with obesity. This article provides a European perspective on the obstacles that patients face in accessing healthcare services and discusses a variety of approaches for engaging individuals with obesity and facilitating the management of obesity as a chronic disease.
Key Words: Obesity, Overweight, Primary health care, General practitioners
Introduction
Obesity is a growing global health problem and is officially recognised as a disease and health issue by several key societies and regulatory bodies, including the Organisation for Economic Co-Operation and Development, the European Medicines Agency and the World Health Organization [1,2,3,4,5].
In Europe, obesity presents an unprecedented and underestimated public health challenge. The latest estimates in European Union (EU) countries have shown that over half (53%) of adults are overweight or obese [6]. Although the prevalence of obesity varies between countries, on average across all EU member states, approximately 16.7% of adults had obesity in 2012 [6]. Childhood obesity rates are also worrying; the proportion of 11- and 13-year-olds who are overweight or obese ranges from 5 to >25% in some EU countries [7]. Importantly, almost two-thirds of children who are overweight before puberty will be overweight in early adulthood [7].
Obesity is a complex disease thought to be caused by biological, psychological and environmental factors [8]. It is typically associated with multiple, potentially life-threatening co-morbidities, including type 2 diabetes, certain types of cancer and cardiovascular disease [9]. Although the burden these complications place on individuals and healthcare systems is substantial [10], obesity is under-recognised and under-treated in the primary care setting [11,12,13].
General practitioners (GPs) are well-placed to tackle this obesity epidemic, yet their engagement with patients is fraught with challenges and barriers. This article identifies the key barriers in the European primary care setting and discusses the steps that can be taken to address them.
Barriers to Engaging Obesity
Lack of Recognition of Obesity as a Disease
The first barrier is the perception among patients that overweight and obesity is ‘normal’ [14], which may result in them not seeking medical support and physicians not actively addressing the issue. There is evidence that some healthcare professionals (HCPs) do not view obesity as a disease and, therefore, do not consider it to be the responsibility of primary care [15,16]. This is perhaps not surprising - it is only recently, with improved scientific understanding of its causes and underlying biology, that obesity has been officially recognised as a chronic disease [3,5]. Prior to this, it was considered by many to be simply a lifestyle choice.
Frustrations around the Ability to Effectively Manage Obesity
Although many overweight or obese individuals initially lose weight through dieting, maintenance of weight loss is a challenge for a substantial proportion [17]; therefore, patients may feel frustrated about their ability to lose weight. Some HCPs believe that the responsibility for weight loss lies solely with the patient and that many lack the motivation to change their behaviour, making the management of obesity ineffective [18,19]. Some GPs have reported that caring for patients with obesity is ineffective and frustrating owing to the low success rates [19]. Furthermore, there exists a perception among some GPs that the clinical evidence base supporting the management of obesity in primary care is limited [20]. Until recently, the lack of effective pharmacotherapies available for weight management may also have compounded the perception among physicians and patients that obesity cannot be successfully managed.
Challenges around Starting the Conversation
Another barrier for addressing obesity in primary care is raising the topic of obesity. Many patients present at the clinic with a separate health issue, which means that GPs need to pro-actively raise the topic of weight. This presents two challenges: firstly, time limitations may make it difficult for GPs to address the health concern that has prompted the consultation and raise the topic of obesity [16,21]. The length of GP consultations can be as short as 10 min in some European countries, including the UK and the Netherlands [22,23].
The second challenge is how to raise the topic of weight in a manner that will be acceptable to the patient. Patients expect their GP to raise the issue of excess weight, but if the topic is not discussed during their consultation, they may assume it is not a concern [24]. If the topic of excess weight is raised, there are often issues of disconnect between patients and their physicians, which may also prove challenging. Patients often attribute their excess weight to uncontrollable biological factors such as hormonal disorders, slow metabolism and stress, whereas GPs are more likely to attribute obesity to controllable factors (such as over-eating) that can be solved through behavioural changes by the patient [25,26]. Furthermore, some physicians have reported that addressing the topic of weight with their patients can be detrimental to the doctor-patient relationship [19,21].
Lack of Training, Resources and Infrastructure
As obesity has historically been perceived as a lifestyle choice, training and guidance on the topic has traditionally been lacking in undergraduate and postgraduate medical courses and in training programmes for HCPs [27]. In the UK, the Royal College of Physicians defined core aspects of knowledge in obesity in 2010 [28], but this has not translated into adequate training for GPs. As a consequence, many GPs report a lack of competency in addressing people with obesity, and many do not feel equipped with the knowledge and training to do so [16,19,21,29].
Compounding this deficit in training is the lack of resources and infrastructure required for obesity management. Guidelines outline the need for a multidisciplinary weight management programmes supported by a team of specialists, including psychologists, specialist nurses, dietitians and exercise physiologists [30,31]. Unfortunately, the provision of such multidisciplinary specialised weight management services (also known as ‘Tier 3 services’) is sparse in many European countries [32,33,34], where they may only be accessible at larger hospitals or specialist academic centres, or restricted to private sector clinics [34]. Consequently, many GPs and patients may not have access to these services.
Inadequate financial resources to fund specialist obesity management services are another barrier for the provision of an appropriate level of care [19,33]. In the UK, the Quality and Outcomes Framework (QOF) rewards GP practices for tackling chronic diseases, with points awarded based on their level of achievement against pre-defined targets [35]. Obesity management is not currently awarded QOF points, although it is likely that the introduction of QOF indicators for this disease may provide greater incentive for GPs to tackle the issue of obesity.
There are a number of approaches that can be taken to overcome some of these barriers to obesity management, and these will be summarised in the next section.
Approaches
Keep Up-to-Date
There is an unfilled need to train HCPs in obesity management. Currently, little training is provided for clinicians both at undergraduate and postgraduate level [27], and this is a problem that seems to extend beyond Europe. An survey in the USA targeting internists, paediatricians and psychiatrists demonstrated a critical need for training in several areas of obesity care, including patient assessment, counselling and motivational interviewing (MI), and goal setting [36].
It is imperative that this fundamental training gap is addressed so that doctors are empowered to improve the management of people with obesity. Training should begin in medical school and continue as a component of core medical training. Raising awareness of obesity among consultants and GPs alike through continuing medical education(CME)-based activities is important [37].
In the meantime, specialist training programmes are available through ‘Specialist Certification of Obesity Professional Education’ (SCOPE; www.worldobesity.org/scope), which provides internationally recognised training and accreditation [38].
The European Obesity Initiative (www.epgonline.org/obesity-cme/understanding-obesity) also offers an online CME learning module ‒ ‘Understanding Obesity’ ‒ which provides overviews of obesity as a disease and its clinical management. This e-module is aimed at obesity specialists, GPs and specialist nurses, and is accredited by the European Accreditation Council for Continuing Medical Education [39].
The European Association for the Study of Obesity (EASO) offers multiple resources for clinicians on their web site, including webinar courses on a number of topics relating to obesity and its clinical management (http://easo.org/education-portal/course). Furthermore, many EASO national member associations provide local guidelines for obesity management on their web sites, together with information of annual meetings and obesity-specific training courses (http://easo.org/membership) [40].
In the UK, the Royal College of GPs Nutrition Group has set up an e-learning course (‘The Introductory Certificate in Obesity, Malnutrition and Health’; http://elearning.rcgp.org.uk) [41], which includes attendance at a behaviour-change study day. Excellent learning opportunities are also provided by international obesity conferences - for example, the annual European Conference on Obesity and national obesity conferences, such as the UK Congress of Obesity, which is organised by the Association for the Study of Obesity in the UK. National societies such as the Society for Endocrinology (SfE) in the UK have expressed an interest in supporting education and research in obesity, and have recently developed an obesity and metabolic network to drive these activities forward. It is also worthwhile to consider additional training opportunities on specific interventions for behavioural counselling for weight loss, such as MI and cognitive behavioural therapy (CBT).
Finally, it is important that GPs keep up-to-date with the obesity management guidelines so that they are aware of the latest treatment options, including new pharmacotherapies, which will allow them to discuss the most appropriate treatment options for individual patients.
Use Appropriate Language
Robust communication skills are essential to successfully engage patients on the topic of their weight. It is essential to ask the patient's permission to discuss the topic of weight and to be empathetic and non-judgemental (see section on the ‘5 As’ below) [42].
Hurtful and offensive words should be avoided and terms preferred by patients should be used - for example, terms such as ‘weight’ and ‘BMI’ are more appropriate than ‘large size’, ‘fatness’ and ‘heaviness’ (table 1) [43]. To reduce negative feelings, it may be useful to emphasise that obesity is a clinical term rather than a description of the physical appearance [30].
Table 1.
Patient ratings of terms to describe excess weight [43]
| More desirable terms | Less desirable terms |
|---|---|
| Weight | Heaviness |
| Excess weight | Obesity |
| BMI | Large size |
| Weight problem | Excess fat |
| Unhealthy body weight | Fatness |
| Unhealthy BMI | Overweight status |
In the UK, the Royal College of Primary Physicians has recently published a ‘GP Ten Top Tips’ for raising the topic of weight with useful opening questions such as ‘How do you feel about your weight?’ or ‘Do you keep an eye on your weight?’[44]. These questions are non-judgemental and give the patient an opportunity to engage in the conversation without feeling defensive [44].
Ensure a Patient-Centric Approach
It is essential to make the person, not the obesity, the focus of the treatment [45]. It is important to address the individual's concerns first, which may not be weight-related, and ask to discuss general healthcare issues [42]. In a position statement, the EASO recommends that regulatory authorities should take the patient's viewpoint into consideration when conducting risk/benefit analyses of treatment or prevention strategies for obesity [46]. The EASO also recommends that treatment should be individually tailored to the patient, and a wide spectrum of clinically proven treatment options should be delivered by a comprehensive multidisciplinary obesity team [31].
The UK National Institute for Health and Care Excellence (NICE) guidelines on obesity management focus on the concept of patient-centred care, advising that the choice of interventions for weight management should be discussed and agreed with the individual [30]. The guidelines specifically recommend that ‘patients should have the opportunity to make informed decisions about their care and treatment, in partnership with their healthcare professionals’. Additionally, the Scottish Intercollegiate Guidelines Network published guidelines on the management of obesity in 2010, which include the recommendation to consider an individual's willingness to change in order to select the most appropriate behavioural therapy for weight loss [47].
Physician advice has a significant impact on promoting weight loss attempts and can help patients achieve positive behaviour changes [48], but it is also important to tailor the advice to the individual.
Remember the ‘5 As’
Developed by the Canadian Obesity Network, the ‘5 As’ of obesity counselling (ask, assess, advise, agree and assist) can help GPs to initiate the conversation about weight and health and provide effective support for obesity management and behavioural change [49].
The ‘5 As’ are defined as follows [50]:
-Ask permission to discuss weight, be non-judgemental and explore readiness for change
-Assess BMI, waist circumference and obesity stage, and explore drivers and complications of excess weight. Obesity staging criteria, such as the Edmonton Staging System [51] and the King's Obesity Staging Criteria [52], can be helpful for assessing co-morbidities, and for interacting with and motivating patients towards achieving a down-staging of the severity of their obesity through weight loss interventions
-Advise on the health risks of obesity, the benefits of modest weight loss, the need for a long-term strategy and the available treatment options
-Agree on realistic weight loss expectations and targets, behavioural changes and specific details of the treatment options
-Assist in identifying and addressing barriers, provide resources and assist in identifying and consulting with appropriate providers, and arrange regular follow-up.
Leverage the Resources and Infrastructure Available
Involve the Multidisciplinary Team
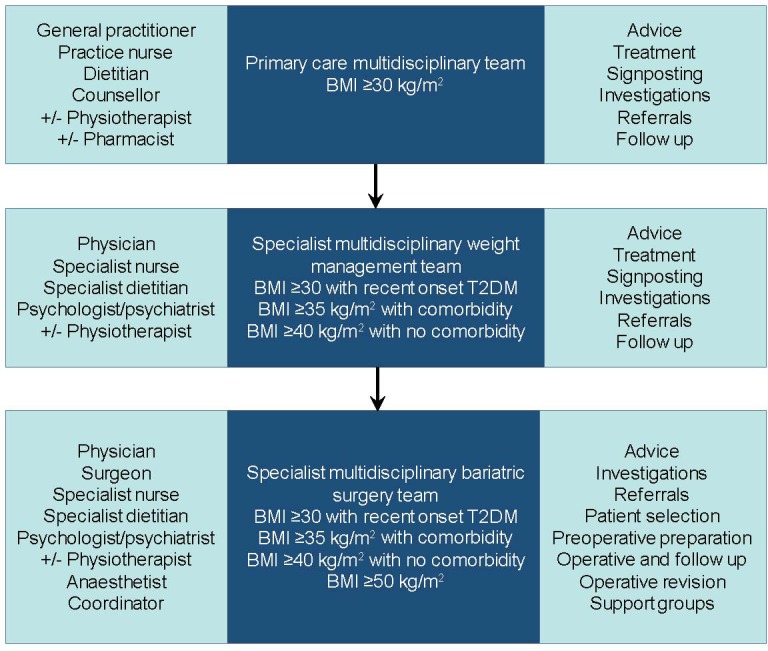
Given that GP consultations with patients are relatively short, the use of a team-based approach can potentially alleviate the impact on resources and may help to limit a patient's feeling of being ‘rushed’ [53] by signposting them to other members of the care team. A multidisciplinary approach in the management of people with obesity is necessary across all levels of care. In the primary care setting, GPs, nurses and counsellors should all be involved (fig. 1).
Fig. 1.
Behavioural Counselling and Lifestyle Interventions
Despite a lack of confidence among some GPs that counselling patients about their weight is worthwhile, evidence suggests it is positively associated with behavioural change, with those individuals who receive initial weight counselling from their GP being more likely to attempt weight loss than those who do not receive counselling [48,54]. GPs have a unique and strategically important role in initiating the dialogue on obesity, assessing patients and signposting them to the appropriate services. There is clearly an opportunity to improve patient-provider communication regarding the management of excess weight and a need for GPs to be better supported in this role.
Obesity management guidelines recommend that lifestyle interventions for obese individuals should be multicomponent in nature [30,31] and include behavioural change strategies to increase people's physical activity levels or decrease inactivity, improve eating behaviour and quality of diet, and reduce energy intake [30]. Furthermore, patients who are not ready to change should be offered the opportunity to return for further consultations when they feel ready to discuss their weight and are willing or able to make lifestyle changes [30].
Cognitive Behavioural Therapy
CBT is a psychological treatment that teaches behavioural and cognitive strategies focusing on achieving and maintaining lifestyle changes, and is now being utilised for weight management [55]. Patients are taught behavioural and cognitive strategies that focus on successfully achieving and maintaining lifestyle changes required for weight loss [55]. European clinical practice guidelines suggest that CBT should be delivered not only by registered psychologists but also by other HCPs, including GPs, dietitians, exercise physiologists and psychiatrists [56]. The guidelines also recommend that elements of CBT should be included in routine dietary management or as part of a larger structured programme [56]. If not directly available at primary care level, these services should be accessible in structured weight loss programmes or ‘Tier 3’ obesity services.
Motivational Interviewing
Motivating patients to take responsibility for their health is one of the key goals of primary care consultations when managing obesity [19]. MI is one approach to patient-centred communication that explores and attempts to resolve ambivalence toward behavioural change [57]. There is some evidence that MI can improve weight-related behaviours and attitudes, and lead to improved weight loss [58,59]. A meta-analysis of 11 randomised controlled trials found that the use of MI increased mean weight loss among overweight or obese individuals, compared with control groups who did not receive this intervention [59].
Although MI methodologies may be effective, many HCPs have not been taught this counselling approach, and teaching programmes can be costly and time-intensive. Techniques that can be applied without specific training, such as on-line educational interventions, have been developed and show potential for enhancing physician MI skills [24].
New Technologies
There is a need for new technologies that support self-monitoring among patients undertaking behaviour change programmes for weight loss. Internet-based weight management programmes have been associated with modest weight loss [60,61]. However, these programmes are restricted to participants who are computer literate and have internet access [47]. Over the past few years, mobile electronic devices, such as mobile phones and personal digital assistants, have been frequently used in the facilitation of weight loss [62]. Although the extent to which mobile electronic devices are more effective than usual care is debatable, a recent meta-analysis of randomised controlled trials evaluating their effectiveness concluded that they can be used to achieve successful weight loss [63].
Family Involvement
Family members can influence both an individual's decision to seek treatment and their adherence to treatment recommendations or lifestyle changes. NICE obesity management guidelines recommend that a patient's partner or spouse should be encouraged to support any weight management programme [30], as this is likely to promote success. When tackling obesity in children, a family approach is essential, and family-based programmes should be promoted and encouraged [64].
Clinic Space
Patients with obesity can face obstacles in accessing healthcare settings. Clinic settings for treating people with severe obesity should be equipped appropriately (e.g. with special seating, adequate weighing/monitoring equipment and large blood pressure cuffs). It is also important to be aware that people can feel anxious about being weighed and measured; therefore, taking steps to ensure privacy may help improve patient experiences [65].
Conclusions
GPs and other primary care professionals have a responsibility to recognise obesity as a disease and to help patients with obesity to receive appropriate treatment. They have a unique and strategically important role in starting the obesity dialogue, performing the initial assessment and signposting patients to the most appropriate services. There is clearly an opportunity to improve patient-provider communication regarding excess weight. However, there are several barriers that need to be overcome for GPs to be better supported in this role, although recognising them is the first step and the majority can be addressed. Tools are available to engage patients, including MI, CBT and new technologies. The emphasis should be placed on a patient-centred approach, empowering patients to take responsibility for their own health with support from their GP. Regardless of the treatment path that is chosen, patients will benefit from their doctors actively monitoring changes in their weight and health, congratulating them on their successes and reminding them of the need for long-term behavioural change. Importantly, a multidisciplinary approach to the care of patients with obesity is necessary across all levels of care, with physicians being at the centre of the weight management team.
Disclosure Statement
Dr Barbara McGowan was a principal investigator on the SCALE Obesity and Prediabetes Clinical Trial NN8022-1839. She has also undertaken advisory and educational work on obesity for Novo Nordisk, Sanofi, Astra Zeneca and Janssen.
Acknowledgements
Editorial assistance was provided by AXON Communications and funded by Novo Nordisk A/S who were also given the opportunity to perform a medical accuracy review of the manuscript.
References
- 1. Organisation for Economic Co-Operation and Development. OECD Factbook 2013 Economic, Environmental and Social Statistics. www.oecd-ilibrary.org/economics/oecd-factbook-2013_factbook-2013-en (last accessed May 20, 2016).
- 2.Mechanick JI, Garber AJ, Handelsman Y, Garvey WT. American Association of Clinical Endocrinologists' position statement on obesity and obesity medicine. Endocr Pract. 2012;18:642–648. doi: 10.4158/EP12160.PS. [DOI] [PubMed] [Google Scholar]
- 3. American Medical Association press release AMA adopts new policies on second day of voting at 2013 Annual Meeting. www.ama-assn.org/ama/pub/news/news/2013/2013-06-18-new-ama-policies-annual-meeting.page (last accessed May 20, 2016).
- 4. European Medicines Agency. EMA draft guideline on clinical evaluation of medicinal products used in weight control (EMA/CHMP/311805/2014) www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2014/07/WC500170278.pdf (last accessed May 20, 2016).
- 5.Word Health Organization. Report of a WHO consultation on obesity. Geneva, 3-5 June 1997 (WHO Technical Report Series 894). Geneva: WHO; 1997. Obesity: Preventing and managing the global epidemic. [PubMed] [Google Scholar]
- 6. Organisation for Economic Co-Operation and Development. Health at a Glance Europe 2014. OECD Publishing. http://dx.doi.org/10.1787/health_glance_eur-2014-en (last accessed May 20, 2016).
- 7. World Health Organization WHO Obesity Factsheet 2.3. Prevalence of overweight and obesity in children and adolescents. www.euro.who.int/_data/ assets/pdf_file/0005/96980/2.3.-Prevalence-of-overweight-and-obesity-EDITED_layouted_V3.pdf (last accessed May 20, 2016).
- 8.Atkinson RL. Etiologies of Obesity. In: Goldstein DJ, editor. The Management of Eating Disorders and Obesity. 2nd ed. Totowa: Humana Press; 2015. pp. 105–118. [Google Scholar]
- 9.Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health. 2009;9:88. doi: 10.1186/1471-2458-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta S, Richard L, Forsythe A. The humanistic and economic burden associated with increasing body mass index in the EU5. Diabetes Metab Syndr Obes. 2015;8:327–338. doi: 10.2147/DMSO.S83696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Booth HP, Prevost AT, Gulliford MC. Access to weight reduction interventions for overweight and obese patients in UK primary care: Population-based cohort study. BMJ Open. 2015;5:e006642. doi: 10.1136/bmjopen-2014-006642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gunther S, Guo F, Sinfield P, Rogers S, Baker R. Barriers and enablers to managing obesity in general practice: A practical approach for use in implementation activities. Qual Prim Care. 2012;20:93–103. [PubMed] [Google Scholar]
- 13.Laws R, Counterweight Project Team Current approaches to obesity management in UK primary care: the Counterweight Programme. J Hum Nutr Diet. 2004;17:183–190. doi: 10.1111/j.1365-277X.2004.00528.x. [DOI] [PubMed] [Google Scholar]
- 14.Johnson F, Beeken RJ, Croker H, Wardle J. Do weight perceptions among obese adults in Great Britain match clinical definitions? Analysis of cross-sectional surveys from 2007 and 2012. BMJ Open. 2014;4:e005561. doi: 10.1136/bmjopen-2014-005561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Derksen RE, Brink-Melis WJ, Westerman MJ, Dam JJ, Seidell JC, Visscher TL. A local consensus process making use of focus groups to enhance the implementation of a national integrated health care standard on obesity care. Fam Pract. 2012;29((suppl 1)):i177–i184. doi: 10.1093/fampra/cmr072. [DOI] [PubMed] [Google Scholar]
- 16.Hansson LM, Rasmussen F, Ahlstrom GI. General practitioners' and district nurses' conceptions of the encounter with obese patients in primary health care. BMC Fam Pract. 2011;12:7. doi: 10.1186/1471-2296-12-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mann T, Tomiyama AJ, Westling E, Lew AM, Samuels B, Chatman J. Medicare's search for effective obesity treatments: diets are not the answer. Am Psychol. 2007;62:220–233. doi: 10.1037/0003-066X.62.3.220. [DOI] [PubMed] [Google Scholar]
- 18.Epstein L, Ogden J. A qualitative study of GPs' views of treating obesity. Br J Gen Pract. 2005;55:750–754. [PMC free article] [PubMed] [Google Scholar]
- 19.Sonntag U, Brink A, Renneberg B, Braun V, Heintze C. GPs' attitudes, objectives and barriers in counselling for obesity - a qualitative study. Eur J Gen Pract. 2012;18:9–14. doi: 10.3109/13814788.2011.627424. [DOI] [PubMed] [Google Scholar]
- 20.Pryke R, Hughes C, Blackburn M. Addressing barriers for GPs in obesity management: the RCGP Nutrition Group. Br J Obes. 2015;1:1–40. [Google Scholar]
- 21.Blackburn M, Stathi A, Keogh E, Eccleston C. Raising the topic of weight in general practice: perspectives of GPs and primary care nurses. BMJ Open. 2015;5:e008546. doi: 10.1136/bmjopen-2015-008546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deveugele M, Derese A, van den Brink-Muinen A, Bensing J, De Maeseneer J. Consultation length in general practice: cross sectional study in six European countries. BMJ. 2002;325:472. doi: 10.1136/bmj.325.7362.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Silverman J, Kinnersley P. Calling time on the 10-minute consultation. Br J Gen Pract. 2012;62:118–119. doi: 10.3399/bjgp12X625102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bravender T, Tulsky JA, Farrell D, Alexander SC, Ostbye T, Lyna P, Dolor RJ, Coffman CJ, Bilheimer A, Lin PH, Pollak KI. Teen CHAT: Development and utilization of a web-based intervention to improve physician communication with adolescents about healthy weight. Patient Educ Couns. 2013;93:525–531. doi: 10.1016/j.pec.2013.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ogden J, Bandara I, Cohen H, Farmer D, Hardie J, Minas H, Moore J, Qureshi S, Walter F, Whitehead MA. General practitioners' and patients' models of obesity: whose problem is it? Patient Educ Couns. 2001;44:227–233. doi: 10.1016/s0738-3991(00)00192-0. [DOI] [PubMed] [Google Scholar]
- 26.Ogden J, Flanagan Z. Beliefs about the causes and solutions to obesity: a comparison of GPs and lay people. Patient Educ Couns. 2008;71:72–78. doi: 10.1016/j.pec.2007.11.022. [DOI] [PubMed] [Google Scholar]
- 27.Kopelman PG. Education and training of healthcare professionals. In: Kopelman PG, Caterson ID, Dietz WH, editors. Clinical Obesity in Adults and Children. 3rd ed. Oxford: Blackwell; 2010. pp. 265–274. [Google Scholar]
- 28. Royal College of Physicians The training of health professionals for the prevention and treatment of overweight and obesity. 2010 report prepared for foresight by the Royal College of Clinicians. www.rcplondon.ac.uk/file/268/download?token=Jq-7nmKw (last accessed May 20, 2016).
- 29.Chisholm A, Mann K, Peters S, Hart J. Are medical educators following general medical council guidelines on obesity education: if not why not? BMC Medical Education. 2013;13:53. doi: 10.1186/1472-6920-13-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. National Institute for Health and Care Excellence Obesity: Identification, assessment and management of overweight and obesity in children, young people and adults. NICE Guidelines CG189, 2014. www.nice.org.uk/guidance/cg189 (last accessed May 20, 2016). [PubMed]
- 31.Yumuk V, Frühbeck G, Oppert JM, Woodward E, Toplak H. An EASO position statement on multidisciplinary obesity management in adults. Obes Facts. 2014;7:96–101. doi: 10.1159/000362191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Read S, Logue J. Variations in weight management services in Scotland: A national survey of weight management provision. J Publ Health. 2015 doi: 10.1093/pubmed/fdv132. DOI: 10.1093/pubmed/fdv132. [DOI] [PubMed] [Google Scholar]
- 33.Hughes C. The rewards and challenges of setting up a Tier 3 adult weight management service in primary care. Br J Obes. 2015;1:25–31. [Google Scholar]
- 34.Tsigos C, Hainer V, Basdevant A, Finer N, Mathus-Vliegen E, Micic D, Maislos M, Roman G, Schutz Y, Toplak H, Yumuk V, Zahorska-Markiewicz B, Obesity Management Task Force of the European Association for the Study of Obesity Criteria for EASO-collaborating centres for obesity management. Obes Facts. 2011;4:329–333. doi: 10.1159/000331236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Doran T, Fullwood C, Gravelle H, Reeves D, Kontopantelis E, Hiroeh U, Roland M. Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med. 2006;355:375–384. doi: 10.1056/NEJMsa055505. [DOI] [PubMed] [Google Scholar]
- 36.Jay M, Gillespie C, Ark T, Richter R, McMacken M, Zabar S, Paik S, Messito MJ, Lee J, Kalet A. Do internists, pediatricians, and psychiatrists feel competent in obesity care?: Using a needs assessment to drive curriculum design. J Gen Intern Med. 2008;23:1066–1070. doi: 10.1007/s11606-008-0519-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grant P, Piya M, McGowan B, Taheri S. The bariatric physician. Clin Med. 2014;14:30–33. doi: 10.7861/clinmedicine.14-1-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Specialist certification of obesity professional education (SCOPE). www.worldobesity.org/scope (last accessed May 20, 2016).
- 39. The European Obesity Initiative eCME module. www.epgonline.org/obesity-cme/understanding-obesity/ (last accessed May 20, 2016).
- 40. European Association for the Study of Obesity. http://www.//easo.org (last accessed May 20, 2016).
- 41. Royal College of GPs Nutrition Group The Introductory Certificate in Obesity, Malnutrition and Health. http://elearning.rcgp.org.uk (last accessed May 20, 2016).
- 42.Campos C. Tips for communicating with overweight and obese patients. J Fam Pract. 2014;63((7 suppl)):S11–S14. [PubMed] [Google Scholar]
- 43.Wadden TA, Didie E. What's in a name? Patients' preferred terms for describing obesity. Obes Res. 2003;11:1140–1146. doi: 10.1038/oby.2003.155. [DOI] [PubMed] [Google Scholar]
- 44. R Pryke on behalf of the Nutrition for Health Royal College of General Practitioners RCGP GP ten top tips: Raising the topic of weight, 2015. www.rcgp.org.uk/clinical-and-research/clinical-resources/nutrition/∼/media/Files/CIRC/Clinical%20News/Top-Ten-Tips-Leaflet-2013.ashx (last accessed May 20, 2016).
- 45.Ahmed SM, Lemkau JP, Lee Birt S. Toward sensitive treatment of obese patients. Fam Pract Manag. 2002;9:25–28. [PubMed] [Google Scholar]
- 46.Frühbeck G, Toplak H, Woodward E, Halford JCG, Yumuk V. Need for a paradigm shift in adult overweight and obesity management - an EASO position statement on a pressing public health, clinical and scientific challenge in Europe. Obes Facts. 2014;7:408–416. doi: 10.1159/000370038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Scottish Intercollegiate Guidelines Network Management of obesity (SIGN Guideline No 115) 2010. www.sign.ac.uk/pdf/sign115.pdf (last accessed May 20, 2016).
- 48.Rose SA, Poynter PS, Anderson JW, Noar SM, Conigliaro J. Physician weight loss advice and patient weight loss behavior change: a literature review and meta-analysis of survey data. Int J Obes (Lond) 2013;37:118–128. doi: 10.1038/ijo.2012.24. [DOI] [PubMed] [Google Scholar]
- 49.Rueda-Clausen CF, Benterud E, Bond T, Olszowka R, Vallis MT, Sharma AM. Effect of implementing the 5As of obesity management framework on provider-patient interactions in primary care. Clin Obes. 2014;4:39–44. doi: 10.1111/cob.12038. [DOI] [PubMed] [Google Scholar]
- 50.Vallis M, Piccinini-Vallis H, Sharma AM, Freedhoff Y. Modified 5 As: Minimal intervention for obesity counseling in primary care. Can Fam Physician. 2013;59:21–31. [PMC free article] [PubMed] [Google Scholar]
- 51.Sharma AM, Kushner RF. A proposed clinical staging system for obesity. Int J Obes (Lond) 2009;33:289–295. doi: 10.1038/ijo.2009.2. [DOI] [PubMed] [Google Scholar]
- 52.Aasheim ET, Aylwin SJ, Radhakrishnan ST, Sood AS, Jovanovic A, Olbers T, le Roux CW. Assessment of obesity beyond body mass index to determine benefit of treatment. Clin Obes. 2011;1:77–84. doi: 10.1111/j.1758-8111.2011.00017.x. [DOI] [PubMed] [Google Scholar]
- 53.Brown I, Thompson J, Tod A, Jones G. Primary care support for tackling obesity: a qualitative study of the perceptions of obese patients. Br J Gen Pract. 2006;56:666–672. [PMC free article] [PubMed] [Google Scholar]
- 54.Jackson SE, Wardle J, Johnson F, Finer N, Beeken RJ. The impact of a health professional recommendation on weight loss attempts in overweight and obese British adults: A cross-sectional analysis. BMJ Open. 2013;3:e003693. doi: 10.1136/bmjopen-2013-003693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tsiros MD, Sinn N, Brennan L, Coates AM, Walkley JW, Petkov J, Howe PR, Buckley JD. Cognitive behavioral therapy improves diet and body composition in overweight and obese adolescents. Am J Clin Nutr. 2008;87:1134–1140. doi: 10.1093/ajcn/87.5.1134. [DOI] [PubMed] [Google Scholar]
- 56.Tsigos C, Hainer V, Basdevant A, Finer N, Fried M, Mathus-Vliegen E, Micic D, Maislos M, Roman G, Schutz Y, Toplak H, Zahorska-Markiewicz B, Obesity Management Task Force of the European Association for the Study of Obesity Management of obesity in adults: European Clinical Practice Guidelines. Obes Facts. 2008;1:106–116. doi: 10.1159/000126822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Christie D, Channon S. The potential for motivational interviewing to improve outcomes in the management of diabetes and obesity in paediatric and adult populations: A clinical review. Diabetes Obes Metab. 2014;16:381–387. doi: 10.1111/dom.12195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgarn BR. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2011;12:709–723. doi: 10.1111/j.1467-789X.2011.00892.x. [DOI] [PubMed] [Google Scholar]
- 59.Cox ME, Yancy WS, Coffman CJ, Ostbye T, Tulsky JA, Alexander SC, Brouwer RJ, Dolor RJ, Pollak KI. Effects of counseling techniques on patients' weight-related attitudes and behaviors in a primary care clinic. Patient Educ Couns. 2011;85:363–368. doi: 10.1016/j.pec.2011.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Aneni EC, Roberson LL, Maziak W, Agatston AS, Feldman T, Rouseff M, Tran TH, Blumenthal RS, Blaha MJ, Blankstein R, Al-Mallah MH, Budoff MJ, Nasir K. A systematic review of internet-based worksite wellness approaches for cardiovascular disease risk management: Outcomes, challenges & opportunities. PloS One. 2014;9:e83594. doi: 10.1371/journal.pone.0083594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kodama S, Saito K, Tanaka S, Horikawa C, Fujiwara K, Hirasawa R, Yachi Y, Iida KT, Shimano H, Ohashi Y, Yamada N, Sone H. Effect of web-based lifestyle modification on weight control: A meta-analysis. Int J Obes (Lond) 2012;36:675–685. doi: 10.1038/ijo.2011.121. [DOI] [PubMed] [Google Scholar]
- 62.Spring B, Duncan JM, Janke EA, Kozak AT, McFadden HG, DeMott A, Pictor A, Epstein LH, Siddique J, Pellegrini CA, Buscemi J, Hedeker D. Integrating technology into standard weight loss treatment: A randomized controlled trial. JAMA Intern Med. 2013;173:105–111. doi: 10.1001/jamainternmed.2013.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khokhar B, Jones J, Ronksley PE, Armstrong MJ, Caird J, Rabi D. Effectiveness of mobile electronic devices in weight loss among overweight and obese populations: A systematic review and meta-analysis. BMC Obes. 2014;1:22. doi: 10.1186/s40608-014-0022-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. National Institute for Health and Care Excellence Families need support to help tackle child obesity time-bomb 2013. www.nice.org.uk/news/article/families-need-support-to-help-tackle-child-obesity-timebomb (last accessed May 20, 2016).
- 65. National Institute for Health and Care Excellence Managing overweight and obesity in adults - lifestyle weight management services. NICE guidelines PH53, 2014. www.nice.org.uk/guidance/ph53 (last accessed May 20, 2016).
- 66. Royal College of Physicians Action on obesity: comprehensive care for all. Report of a working party. London, RCP, 2013. www.rcplondon.ac.uk/projects/outputs/action-obesity-comprehensive-care-all (last accessed May 25, 2016).


