Abstract
Objective
While there is a dose-response relationship between physical activity (PA) and health benefit, little is known about the effectiveness of different PA prescriptions on total daily PA.
Aim
To test, under real-life conditions and using an objective, non-invasive measurement technique (accelerometry), the effect of prescribing additional physical activity (walking only) of different durations (30, 60 and 90 min/day) on compliance (to the activity prescribed) and compensation (to total daily PA). Participants in each group were prescribed 5 sessions of walking per week over 4 weeks.
Methods
55 normal-weight and overweight women (mean BMI 25 ± 5 kg/m2, height 165 ± 1 cm, weight 68 ± 2 kg and mean age 27 ± 1 years) were randomly assigned to 3 prescription groups: 30, 60 or 90 min/day PA.
Results
Walking duration resulted in an almost linear increase in the number of steps per day during the prescription period from an average of about 10,000 steps per day for the 30-min prescription to about 14,000 for the 90-min prescription. Compliance was excellent for the 30-min prescription but decreased significantly with 60-min and 90-min prescriptions. In parallel, degree of compensation subsequent to exercise increased progressively as length of prescription increased.
Conclusion
A 30-min prescription of extra walking 5 times per week was well tolerated. However, in order to increase total PA further, much more than 60 min of walking may need to be prescribed in the majority of individuals. While total exercise ‘volume’ increased with prescriptions longer than 30 min, compliance to the prescription decreased and greater compensation was evident.
Key Words: Walking prescription, Compliance, Effectiveness, Physical activity
Introduction
The benefits of physical activity for health are widely acknowledged, with research evidence consolidated in a number of landmark reports [1,2,3]. To address decreases in physical activity at the population level, physical activity guidelines were developed for adults [4] and later updated based on new research evidence [5]. Despite some variations, physical activity guidelines have consistently referenced ‘putting together at least 30-min of moderate-intensity physical activity on most, preferably all, days of the week’ [5] to confer health benefits. However, this recommended prescription may not be sufficient to compensate for the typical reductions in habitual physical activity and predominance of sedentary lifestyle behaviours characteristic of many adults. Further, many people regard 30 min of activity as a target rather than a minimum [6]. The degree of compliance to a prescription of 30 min physical activity (or multiples of 30 min) per day, and compensation to different physical activity prescriptions have not been thoroughly investigated. Both poor compliance and compensatory effects associated with engagement in physical activity are key factors likely to decrease the effectiveness of physical activity prescriptions.
Brisk walking at an individual's preferred pace is the most commonly reported [7] and recommended physical activity as it meets the minimum intensity to achieve a cardiorespiratory benefit and decrease adiposity in the unfit [8,9,10]. Walking is a natural, accessible and safe physical activity and does not require special skill or equipment [6,11]. However, an ongoing challenge relates to the specifics of the activity prescription [12,13]. To use self-paced walking as an example, common questions relate to the duration (how long), frequency (how often) and intensity (how hard) of the walking prescription.
In addition, we ignore how individuals respond to prescriptions of different duration (for example, 30 vs. 60 vs. 90 min/day). Depending on the desired health outcome, promotion of physical activity has typically referenced benefits associated with increasing physical activity in blocks of time ranging from 10 min to more than 1 h [1,4,5,12]. However, little is known about the effectiveness of different prescriptions on the increase in total daily physical activity [5].
For example, some research has indicated that at least 60 min/day of moderate-intensity physical activity is necessary to prevent weight gain and maximize health benefits [2]. Other reports have claimed that 60-90 min/day of brisk walking is necessary to achieve either long-term weight loss or the maintenance of body weight [14,15]. In addition, the effectiveness of physical activity prescriptions is likely to be compromised by both poor compliance and compensatory effects.
We investigated the response to three walking prescriptions (30, 60 and 90 min/day) in a group of normal-weight and overweight women. We measured physical activity using accelerometry, calculated intensity scores and estimated physical activity levels and subsequently converted data to physical activity energy expenditure (AEE). Further, we calculated both compliance and compensation to each prescription.
Material and Methods
Subjects
55 normal-weight and overweight women were recruited to the study (mean BMI 25 ± 5 kg/m2, height 165 ± 1 cm, weight 68 ± 2 kg and average age 27 ± 1 years). Women were randomly assigned to 3 walking prescription groups: 30, 60 or 90min/day. Selection criteria included: healthy (taking no medication), female, aged 18-40 years, non-smokers, no orthopaedic problems limiting mobility, non-obese (BMI < 30 kg/m2). As a substantial fraction of the Swiss population (ca. 90%), are normal-weight or overweight, we recruited both categories of women.
Objectives
Given the controversy regarding the specifics of physical activity participation required for health and weight maintenance, the purpose of the proposed study was to test, under real-life conditions and using an objective, non-invasive measurement (accelerometry), the effect of prescribing additional physical activity (walking only) of different duration (30, 60 and 90 min/day) on compliance (to the activity prescribed) and compensation (to total daily physical activity). Our interest was to study both normal-weight and overweight women as this population are susceptible to weight gain and therefore are a primary target for physical activity programmes and interventions.
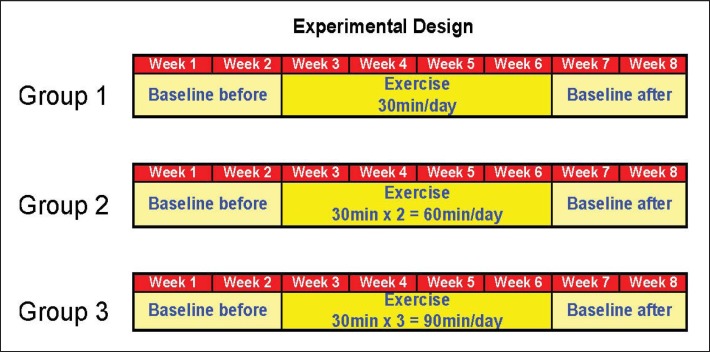
Experimental Design
A 2-week baseline was used to record habitual physical activity (baseline ‘before’). During week 3-6, the physical activity prescription consisted of daily walking (either 30 or 60 or 90 min duration) at the preferred walking speed. Participants were asked to add the assigned walking duration to their normal daily activity 5 times per week across the 4-week intervention. Two sub-periods (weeks 3 and 4, plus weeks 5 and 6) were also compared (fig. 1). Although a cross-over design would have been ideal, it was not practical for all participants to complete each of the 3 walking prescriptions. Participants were also advised that it was acceptable to split the walking duration into blocks of 30 min (i.e., 60 min or 2 × 30 min, 90 min or 3 × 30 min etc.). No activity prescription was imposed during the final 2-week block (week 7 and 8) during which participants spontaneously returned to their habitual activity (baseline ‘after’). There was a standardized way of indicating to the subjects that the prescribed walking physical activity was abandoned and that she was free to adopt the strategy she desired.
Fig. 1.
Experimental design. Note the double baseline periods before and after intervention (2 weeks each), allowing first a comparison of activity between the 2 baseline periods and second the ability to track any continuation of walking (carry over) beyond the completion of the 4-week physical activity prescription.
Research Questions
Five questions were raised:
i) What is the compliance to daily walking prescriptions of 30 min vs. 60-min vs. 90 min?
ii) Does compliance decrease as the duration of prescription increases (i.e., are women less compliant to a 90-min vs. 60-min vs. 30-min prescription)?
iii) Is there a compensation effect to the walking prescription with a concomitant spontaneous decrease in physical activities of daily living?
iv) Is the putative compensatory effect greater with increased duration of walking prescription?
v) What is the net effect (true effect) of each of the walking prescriptions on daily AEE?
Data Acquisition and Analysis
Physical activity level was inconspicuously monitored using a miniaturized uniaxial accelerometer weighing less than 30 g (Lifecorder; Suzuken Co. Ltd., Nagoya, Japan). Physical activity was then categorized into 11 levels (0, 0.5 and 1-9; level 0 corresponding to <0.06 gravity unit) based on the pattern of the acceleration signal. Activity levels were subsequently converted by a proprietary algorithm to obtain AEE. Resting metabolic rate was calculated taking into account anthropometric data of participants (body weight, height, gender and age). In addition, the number of steps/day was measured by the accelerometer with great accuracy. The device has been extensively tested and validated in our laboratory using a whole-body calorimeter [16,17].
Calculation of Indices
Compliance during the prescription period was defined as the ratio of continuous walking duration (measured by accelerometry) to prescribed walking duration:
Compliance index (%) = effective walking duration (min) / prescribed walking duration (min) × 100.
Compensation was defined as the ratio between the expected and the observed increase in steps per day (measured by accelerometry) resulting from the walking prescription.
Net walking activity duration was the difference in measured continuous walking between baseline and prescription period:
Compensation index (%) = observed rise in steps/day due to prescription / expected increase in steps/day due to effective exercise duration × 100.
Statistical Methods
Between-treatment comparisons (30 vs. 60 vs. 90 min) were analysed by ANOVA. In order to track which of the treatments was different from another, a multiple comparison t-test was performed with Bonferroni corrections.
Results
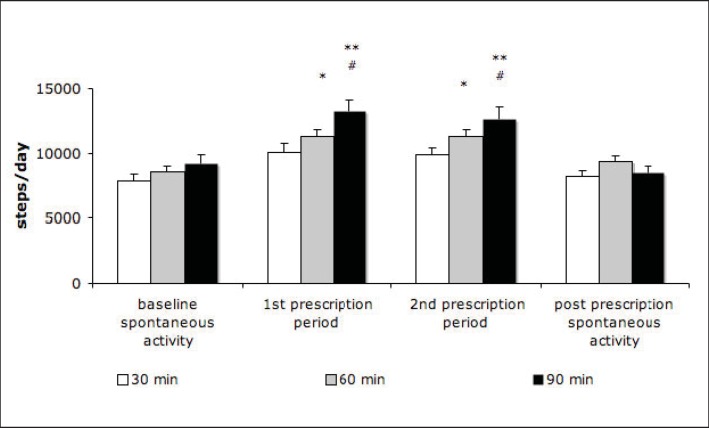
Steps per Day
As anticipated, an increase in walking duration resulted in an almost linear increase in the number of steps/day during the prescription period (fig. 2). The baseline numbers of steps/day (before and after the prescription) were not significantly different between the 3 groups. Mean steps/day varied from about 7,500 to 9,000. These data indicate that activity levels of participants were similar to those of earlier studies in Swiss women [18] but somewhat higher than in a recent study [19]. From baseline to the first prescription period there was a significant increase in steps for both 60- and 90-min groups (from about 8,000 to 11,000 and from about 9,000 to 13,000, respectively). A similar pattern was evidenced during the second prescription period. In each case, total steps/day were significantly greater in the 90-min than in the 30-min groups (p < 0.01). Further, total steps in the 90-min group were significantly different to the post-prescription activity level (p < 0.01).
Fig. 2.
Total number of steps over 24 h during the baseline, prescription periods (first and second) and post-prescription periods. Values are shown as mean ± SEM. **p < 0.001 versus baseline and post prescription. *p < 0.01 versus baseline. #p < 0.05 versus 30-min prescription.
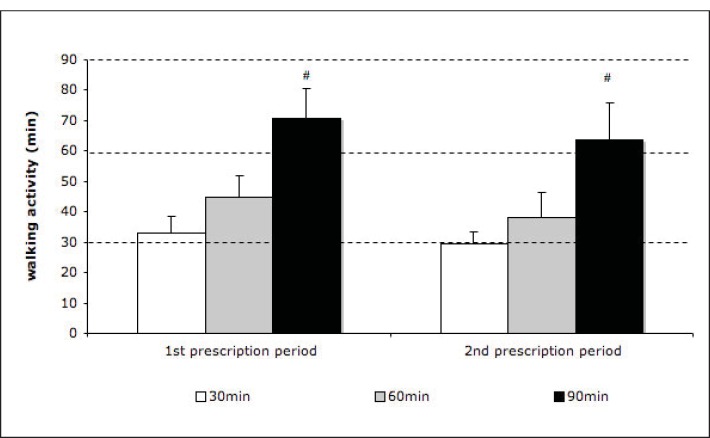
Walking Duration
There was a net increase in walking duration (min/day) across each prescription group for both 2-week prescription blocks (fig. 3). Mean walk time in each 2-week block was significantly greater in the 90-min group (70 and 65 min), than in the 60-min group (47.5 and 40 min) and 30-min group (33 and 30 min).
Fig. 3.
Net increase in walking duration (over baseline) during the first and second walking prescription period (2 weeks each). Dotted lines represent the 3 durations prescribed. Values are shown as mean ± SEM.
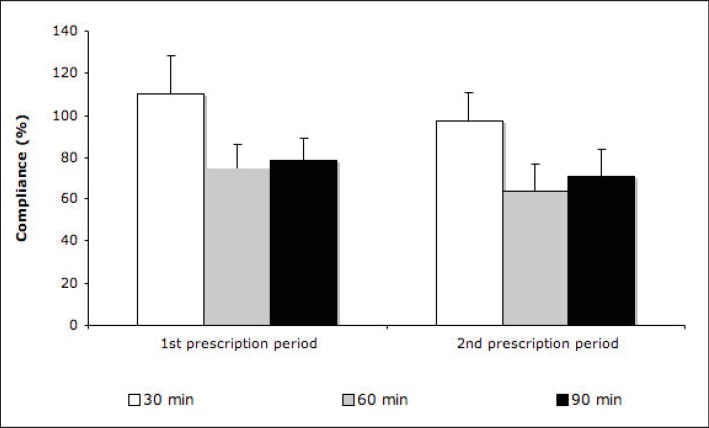
Compliance to Exercise
Compliance to walking prescription (the ability to complete the daily walking prescription) was high during each 2-week period (110 and 100%) for the 30-min group but reduced substantially with longer prescriptions to 75 and 60% for the 60-min and 80 and 70% for the 90-min group. In short, compliance was excellent for the 30-min walking prescription but decreased significantly for the 60-min and 90-min prescriptions (fig. 4).
Fig. 4.
Relative compliance (adherence) to walking prescription during each walking prescription period. Values are shown as mean ± SEM.
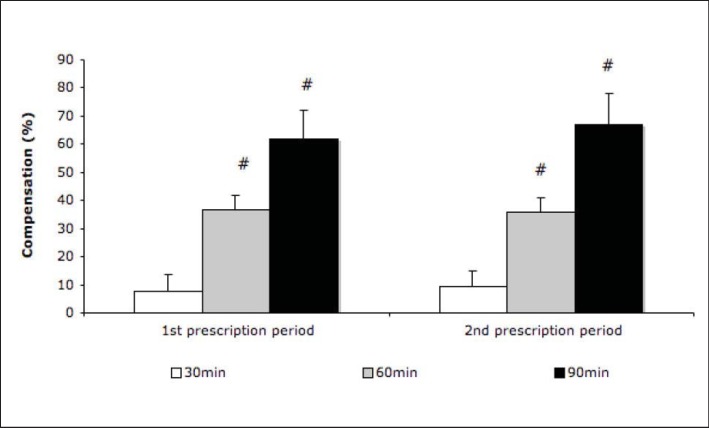
Compensatory Effect to Activity Prescription
Similar to compliance, compensation (%) increased progressively as length of prescription increased. The average compensation rate (based on change in steps/day and exercise duration), was 25 ± 16% with substantial inter-individual variation. Compensation ranged from less than 10% for 30-min walking prescription – i.e. extra activity prescription did not significantly reduce the baseline activity level – to 65% for 90-min prescription (p < 0.05) – i.e. two thirds of the additional prescription was offset by a blunting of physical activity in the post-intervention period (fig. 5).
Fig. 5.
Relative compensation (%) to walking prescription. Values are shown as mean ± SEM. #p < 0.05 versus 30-min prescription.
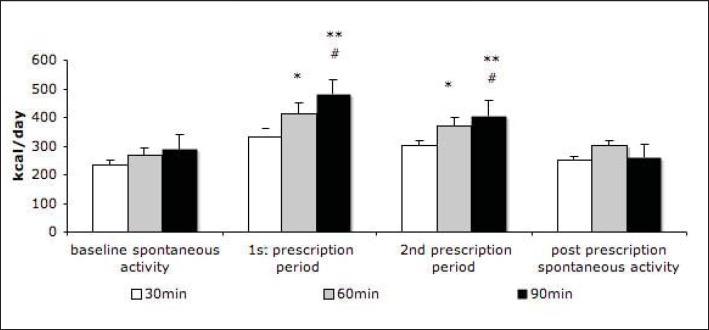
Activity Energy Expenditure
Finally, as shown in fig. 6, activity energy expenditure (AEE) increased significantly with an increase in duration of walking prescription (p < 0.01 vs. baseline and p< 0.05 vs. 30-min prescription). The expected effect on AEE was higher than the real effect as compliance to the prescribed exercise was never 100%, as identified above.
Fig. 6.
AEE. Values are shown as mean ± SEM. **p < 0.001 versus baseline and post-prescription. *p < 0.01 versus baseline. #p < 0.05 versus 30-min prescription.
On average, the walking prescription increased total energy expenditure by 3% (30-min prescription), by 6% (60-min prescription) and by 9% (90-min prescription).
Discussion
Based on the very low proportion of adults who meet physical activity guidelines when assessed using objective measures [20,21], the promotion of physical activity, particularly walking, is a public health priority [6,22]. Earlier research has demonstrated the health benefits of both accumulated and continuous bouts of physical activity [1,4]. However, very few studies have assessed the relationship between physical activity prescriptions of different durations and compliance and compensation. As far as we are aware, this is the first study to evaluate differences between walking prescription of various durations in healthy, normal-weight and overweight European women.
The current analyses provide some key pointers in relation to the public health promotion of physical activity. From a practical perspective, the commonly employed prescription of 30 min/day of self-paced walking, in addition to habitual physical activity, was well tolerated in our sample of women. Due to good compliance and limited compensation, the 30-min prescription resulted in participants increasing their daily continuous walking by about 30 min.
In contrast, and as a function of reduced compliance and increased compensation, the longer prescriptions (60 and 90 min) were not achieved by most participants. Abel et al. [23] recently reported that an objective and practical guide to individuals meeting the moderate-intensity activity level necessary to achieve the current recommendation is to use a pedometer/accelerometer to count 100 steps/min. Such an approach, which assumes a reasonably constant gait cycle (step rate and step length, hence speed), may also be valuable as the length of walking prescription increases.
The rationale for promoting walking as the preferred mode of activity to meet physical activity recommendations is based on the simplicity of the activity, its relative safety and its effectiveness in promoting health. An additional underlying principle is that moderate-intensity activity was enjoyable for adults across a wide age and fitness range. Whilst not the focus of the current study, Ekkikakis et al. [24] have postulated that greater attention should be paid to the causal chain linking intensity of physical activity to affect and adherence. For some individuals, the impost of longer prescriptions in the current study may have influenced the enjoyment of walking and both compliance and compensation. Practical constraints certainly exist of finding an extra time window in their daily routine.
In a recent randomized controlled trial in adult men and women, Samuels et al. [19] examined differences between groups prescribed i) 10,000 steps/day ii) 30-min/day of continuous moderate-intensity physical activity or iii) 30 min/day of moderate-intensity physical activity accumulated in bouts of at least 10 min. Physical activity was assessed by pedometers/accelerometers, and self-efficacy was measured over the 5-week intervention. The authors found that, as compared to the other approaches, the 10,000 step/day guideline resulted in the greatest increase in physical activity above baseline values.
While walking at a moderate-intensity, the expectation is that most individuals would accumulate 3-4,000 steps in a 30-min walk at 100-130 steps/min. This was confirmed in the current study, with the daily step count for participants in the 30-min prescription group being almost 10,000 during the intervention period (fig. 2). The 30-min group in the study by Samuels et al. [19] was of particular interest since, on days they met the physical activity recommendation, the subjects increased daily steps by 3,500 above baseline and reached about 10,000 steps/day. Our study confirms this observation.
Practical Recommendations
A walking prescription of 90 min/day may be an unrealistic recommendation for many working women as we found evidence of a degradation in compliance to the prescription with a correspondingly large compensation. However, the net walking duration completed by those prescribed 60 or 90 min/day was higher than in those subjects with 30-min prescription. An alternative option to obviate this poor compliance may be to encourage, where possible, an increase in the intensity of exercise by performing more vigorous activities such as very brisk walking. Such advice parallels the more recent physical activity recommendations which encompass both moderate- and vigorous-intensity activities [5].
In summary, a 30-min prescription of extra walking was well tolerated across the 4-week intervention with participants consistently achieving the prescription. To significantly increase total physical activity beyond 30 min/day, much more than 60 min of walking should be prescribed to account for both high compensation and low compliance to the extra exercise. Due to time constraints, prescriptions of 60 min/day of physical activity or longer may be difficult to follow for an extended period in some individuals, since it involves a reorganization of daily leisure activities. Williams [25] recently reported that distance walked provides a better assessment of the volume of activity undertaken than time spent walking. Potentially, greater compliance to longer prescriptions (>30 min/day) may be achieved using a distance as opposed to target time, particularly recognising the common overestimation of self-reported physical activity. In practical terms, this means that the distance should be tracked rather than the time: today a simple smartphone with an appropriate application using accelerometry/GPS is capable of doing this with reasonable accuracy.
Limitations
We acknowledge a number of limitations related to the current study. Participants were healthy volunteers who were reasonably active compared to physically inactive participants in other studies [19]. It would also have been preferable to employ a cross-over design but, as noted, this was not possible in the present study. Future research should also examine the impact of different activity prescriptions on compliance over a longer time period than 1 month. Further, as this work was only undertaken in women, it is unclear whether there are gender differences in responsiveness to different prescriptions. In addition, similar work should be undertaken in obese adults to better understand the impact of activity prescription across the normal-weight to obesity continuum. These limitations notwithstanding, we believe that the results of the present study provide important information regarding the impact of walking prescriptions of different duration in normal-weight and overweight European women.
Conclusion
The classical minimal recommendation of 30 min/day walking prescription was found to be realistic and assured excellent adherence in both non-obese and overweight individuals.
Disclosure Statement
The authors declared no conflict of interest.
Acknowledgement
This work was supported by the Swiss Federal Sport Commission (research commission) and by the National Science Foundation (grant 3200B0-113365). We thank Dr V. Lecoultre (who refused to be co-author) for his participation in the study.
References
- 1.U.S. Department of Health and Human Services . Physical Activity and Health: A Report of the Surgeon General in National Center for Chronic Disease Prevention and Health Promotion. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 1996. [Google Scholar]
- 2.Institute of Medicine . Dietary Reference Intake, Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein and Amino Acids. Washington, DC: National Academy Press; 2002. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization . Global Recommendations on Physical Activity for Health. Geneva: World Health Organization; 2010. [PubMed] [Google Scholar]
- 4.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. J Am Med Assoc. 1995;273:402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 5.Haskell WL, Lee I-M, Pate RP, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 6.Lee IM, Buchner DM. The importance of walking to public health. Med Sci Sports Exerc. 2008;40(suppl 7):S512–S518. doi: 10.1249/MSS.0b013e31817c65d0. [DOI] [PubMed] [Google Scholar]
- 7.Simpson ME, Serdula M, Galuska DA, et al. Walking trends among US adults: the Behavioral Risk Factor Surveillance System, 1987-2000. Am J Prev Med. 2003;25:95–100. doi: 10.1016/s0749-3797(03)00112-0. [DOI] [PubMed] [Google Scholar]
- 8.Pollock M, Gaesser G, Butcher J, Despres J, Dishman R, Franklin B. American College of Sports Medicine position stand: the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;30:975–991. doi: 10.1097/00005768-199806000-00032. [DOI] [PubMed] [Google Scholar]
- 9.Hills AP, Byrne NM, Wearing S, Armstrong T. Validation of the intensity of walking for pleasure in obese adults. Prev Med. 2006;42:47–50. doi: 10.1016/j.ypmed.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 10.Williams PT. Association between walking distance and percentiles of body mass index in older and younger men. Br J Sports Med. 2008;42:352–356. doi: 10.1136/bjsm.2007.041822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brooks AG, Gunn SM, Withers RT, Gore CJ, Plummer JL. Predicting walking METs and energy expenditure from speed or accelerometry. Med Sci Sports Exerc. 2005;37:1216–1223. doi: 10.1249/01.mss.0000170074.19649.0e. [DOI] [PubMed] [Google Scholar]
- 12.Rhodes RE, Warburton DE, Murray H. Characteristics of physical activity guidelines and their effect on adherence: a review of randomized trials. Sports Med. 2009;39:355–375. doi: 10.2165/00007256-200939050-00003. [DOI] [PubMed] [Google Scholar]
- 13.Williams PT. Advantage of distance- versus time-based estimates of walking in predicting adiposity. Med Sci Sports Exerc. 2012;44:1728–1737. doi: 10.1249/MSS.0b013e318258af3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weinsier RL, Hunter GR, Desmond RA, Byrne NM, Zuckerman PA, Darnell BE. Free-living activity energy expenditure in women successful and unsuccessful at maintaining a normal body weight. Am J Clin Nutr. 2002;75:499–504. doi: 10.1093/ajcn/75.3.499. [DOI] [PubMed] [Google Scholar]
- 15.Saris WH, Blair SN, Van Baak MA, et al. How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obes Res. 2003;4:101–114. doi: 10.1046/j.1467-789x.2003.00101.x. [DOI] [PubMed] [Google Scholar]
- 16.Kumahara H, Schutz Y, Ayabe M, Yoshioka M, Yoshitake Y, Shindo M, Ishii K, Tanaka H. The use of uniaxial accelerometry for the assessment of physical-activity-related energy expenditure: a validation study against whole-body indirect calorimetry. Br J Nutr. 2004;91:235–243. doi: 10.1079/BJN20031033. [DOI] [PubMed] [Google Scholar]
- 17.Kumahara H, Tanaka H, Terrier P, Ishii K, Oppert JM, Guy-Grand B, Schutz Y. Comparison of two accelerometers for assessing daily energy expenditure in adults. J Phys Act Health. 2004;1:270–280. [Google Scholar]
- 18.Sequeira MM, Rickenbach M, Wietlisbach V, Tullen B, Schutz Y. Physical activity assessment using a pedometer and its comparison with a questionnaire in a large population survey. Am J Epidemiol. 1995;142:989–999. doi: 10.1093/oxfordjournals.aje.a117748. [DOI] [PubMed] [Google Scholar]
- 19.Samuels TY, Raedeke TD, Mahar MT, Karvinen KH, DuBose KD. A randomized controlled trial of continuous activity, short bouts, and a 10,000 step guideline in inactive adults. Prev Med. 2011;52:12–125. doi: 10.1016/j.ypmed.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 20.Hagströmer M, Oja P, Sjöström M. Physical activity and inactivity in an adult population assessed by accelerometry. Med Sci Sports Exerc. 2007;39:1502–1508. doi: 10.1249/mss.0b013e3180a76de5. [DOI] [PubMed] [Google Scholar]
- 21.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 22.Haskell WL, Blair SN, Hill JO. Physical activity: health outcomes and importance for public health policy. Prev Med. 2009;49:280–282. doi: 10.1016/j.ypmed.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 23.Abel M, Hannon J, Mullineaux D, Beighle A. Determination of step rate thresholds corresponding to physical activity intensity classifications in adults. J Phys Act Health. 2011;8:45–51. doi: 10.1123/jpah.8.1.45. [DOI] [PubMed] [Google Scholar]
- 24.Ekkekakis P, Backhouse SH, Gray C, Lind E. Walking is popular among adults but is it pleasant? A framework for clarifying the link between walking and affect as illustrated in two studies. Psychol Sport Exerc. 2008;9:246–264. [Google Scholar]
- 25.Williams PT. Advantage of distance- versus time-based estimates of walking in predicting adiposity. Med Sci Sports Exerc. 2012;44:1728–1737. doi: 10.1249/MSS.0b013e318258af3f. [DOI] [PMC free article] [PubMed] [Google Scholar]