Abstract
The proposition of so-called ‘food addiction’ (FA) in the scientific literature has stimulated a recent surge in research and debate. The concept of FA is controversial, and opinion is divided. Many of the findings depend upon the use of a single instrument called the Yale Food Addiction Scale (YFAS). This review systematically examined FA, as defined by the YFAS, reported in 40 experimental human studies published in or after 2009. The results indicated that much of the literature makes the supposition that food addiction is an accepted neurobiological disease, consistent with substance use disorders; an interpretation based on very limited data. This raises the question as to whether those individuals who meet the YFAS criteria for diagnosis are truly ‘addicted’ to food or if they experience significant impairment to their psychological wellbeing and quality of life as would be expected in clinically recognised addictive disorders. At the present time, little research has investigated the extent to which a psychometric self-assessment of FA symptomatology can elucidate a harmful relationship with target foods in the diet. A positive YFAS diagnosis is usually positively associated with BMI and strongly linked with the presence of binge eating, but certain exceptions within the literature were revealed. Further clarification is required as to whether so-called FA is sufficiently different to existing conditions and traits to warrant classification as a distinctive disease phenotype rather than an expression of strong habits and preferences.
Key Words: Food addiction, Eating addiction, Systematic research review
Introduction
Since 1980, worldwide obesity has nearly doubled according to the World Health Organisation (WHO) [1], prompting large amounts of research investigating the aetiology of this condition. Vast amounts of resources are invested each year to target the prevention and treatment of obesity, but results tend to be unsatisfactory, and most people regain any lost weight within 5 years [2]. There is considerable evidence that obesity is driven by an obesogenic environment characterised by an overall abundance of food [3,4] or by a decrease in work-related energy expenditure [5]. However, a recent notion has proposed that obesity may be driven by a person's dependence on food in a manner similar to a person's dependence on drugs of abuse, potentially stimulating a pathway contributing to sustained overeating and obesity. This concept has been widely termed ‘food addiction’ (FA), although ‘addiction-like eating’ and ‘eating addiction’ have also been used [6].
In 1956, Theron G. Randolph [7] first reported ‘(…) a common pattern of symptoms descriptively similar to those of other addictive processes’ (p. 221) in individuals' responses to regularly consumed foods. Conditions synonymous with so-called FA have been proposed in scientific literature for many years, particularly the popular labelling of many individuals as ‘chocoholics’ or ‘chocolate addicts’. Such individuals are shown to endorse many criteria associated with addiction, such as tolerance [8] and lack of control [9], and experience intense cravings in response to external chocolate cues [10]. Such research has led to investigators alleging the addictive properties of either sugar (e.g. [11,12]), fat (e.g. [13]) or salt [14]. Similar ‘addiction’ symptoms in association with sugar-sweetened beverages, particularly Cola, have also been reported [15].
The idea that certain foods and beverages may have addictive potential is not new [16], yet recent developments in research have led to contradictory positions regarding the aetiology of FA. From a biological perspective, the possibility that certain individuals may be genetically or physiologically predisposed to develop an addiction to certain foods has been proposed (e.g. [17,18]). Additionally, researchers (e.g. [19,20]) have claimed that so-called FA may be a neurological condition, consistent with substance dependence and addictive behaviour disorders, as diagnosed by the Diagnostic and Statistical Manual (DSM) [21]. Furthermore, specific foods or ingredients, labelled ‘addictive agents’ [13], have been suggested to possess the potential to elicit an ‘addictive response’ in susceptible individuals [11,14,16]. Alternatively, behavioural explanations have implied that FA could be a consequence of a sustained maladaptive pattern of food choice and consumption [22]. Thus, there is uncertainty over whether the existence of FA is a conceivable cause, a co-morbid condition or rather a possible consequence of obesity [23].
The supposition of a condition termed FA – its definition, aetiology, validity and value – is not clear, nor fully understood. In addition, the contradictions in the arguments promoting the existence of FA are exacerbated by a lack of balance in the scientific discussion to date. In part, this disparity in the literature can be explained by the development and popularity of a specific questionnaire designed to quantify hypothesised symptoms of FA called the Yale Food Addiction Scale (YFAS). The YFAS is a 25-item self-report instrument, based upon the seven symptomatic criteria for substance dependence as defined by the DSM-IV-TR (table 1) including two items that assess significant clinical impairment or distress resulting from overeating. A dichotomous diagnosis of FA is applied when at least three criteria and a significant clinical impairment are endorsed. Alternatively, a ‘symptom count’ can be measured to provide a score between 1 and 7, indicating the severity of the symptomatology. The YFAS was therefore designed to identify or ‘diagnose’ individuals with addictive eating behaviour patterns and the frequency (‘severity’) of symptoms endorsed. The scale is widely available, simple to administer and has been shown to demonstrate reliable psychometric properties [24]. Nevertheless, the use of this metric does not validate the construct of FA, but merely assigns to people a score based on their responses to certain questions. The interpretation of these responses is not a simple matter and cannot be automatically assumed to reveal an underlying pathology or psychological condition until such time as the evidence shows otherwise.
Table 1.
The DSM-IV-TR criteria for substance dependence [25]
| 1) Substance taken in larger amount and for longer period than intended |
| 2) Persistent desire or repeated unsuccessful attempts to quit |
| 3) Much time/activity to obtain, use, recover |
| 4) Important social, occupational, or recreational activities given up or reduced |
| 5) Use continues despite knowledge of adverse consequences (e.g., failure to fulfil role obligation, use when physically hazardous) |
| 6) Tolerance (marked increase in amount; marked decrease in effect) |
| 7) Characteristic withdrawal symptoms; substance taken to relieve withdrawal |
| 8) Use causes clinically significant impairment or distress |
Objectives
To our knowledge, there have been no systematic research reviews conducted to critically examine both the prevalence and correlates of FA as measured by the YFAS. However, a recent publication by Pursey et al. [26] has estimated the prevalence of FA as defined by the YFAS in 25 studies published before July 2014. Similarly, numerous studies have investigated specific correlates of FA, including measures of psychological distress such as depression [27] and attention deficit hyperactivity disorder (ADHD) [28], pathological eating behaviours such as binge eating disorder (BED) [29] and bulimia nervosa (BN) [30], and weight loss outcomes [31]. However, no review has been conducted to summarise and critically examine these correlates. The present systematic research review therefore provides a critical examination of both the prevalence and correlates of so-called FA, as defined by the YFAS. Specifically, this review aimed to:
– Critically evaluate the prevalence of YFAS-determined FA in multiple groups, including obese and overweight individuals, patients with BED and BN, children and the general population.
– Examine the correlates of YFAS-determined FA, including, but not limited to, psychological distress, weight loss outcomes and susceptibility to maladaptive eating behaviours.
– Evaluate the utility of the YFAS and its application of the DSM-IV-TR criteria for substance dependence in identifying dysfunctional patterns of eating.
– Determine to what extent YFAS-determined FA is successful in identifying a novel behavioural phenotype of overeating, which is diagnostically and behaviourally different to existing eating disorder phenotypes.
Method
A systematic review of the literature relating to YFAS-determined FA was performed. Titles, abstracts and full texts were screened to assess their eligibility for inclusion using the following search strategy:
Key Terms and Limits
The literature search was carried out using the key terms ‘food addiction’, ‘food addict*’, ‘Yale Food Addiction Scale’, ‘YFAS’ or ‘eating addict’. The search results were limited to humans and the English language. As the YFAS was developed in 2009, literature published before this date was not considered.
Databases
The search strategy was conducted using the databases Embase, PsycINFO, MEDLINE, Science Direct and Web of Science. Hand searching of citations in review articles provided additional sources.
Inclusion and Exclusion Criteria
No exclusion criteria were applied to sample demographics. Male and female participants of all ages, including children, were included, as were normal-weight, overweight and obese samples. Only experimental studies measuring the prevalence or correlates of YFAS-determined FA were included. As such, all review papers (N = 23), case studies (N = 1), validation studies (N = 7) or non-experimental uses of the YFAS (N = 24) were excluded. Only peer-reviewed articles were included, thus dissertation and thesis papers (N = 3), conference abstracts (N = 22) and books (N = 8) were excluded.
Data Extraction
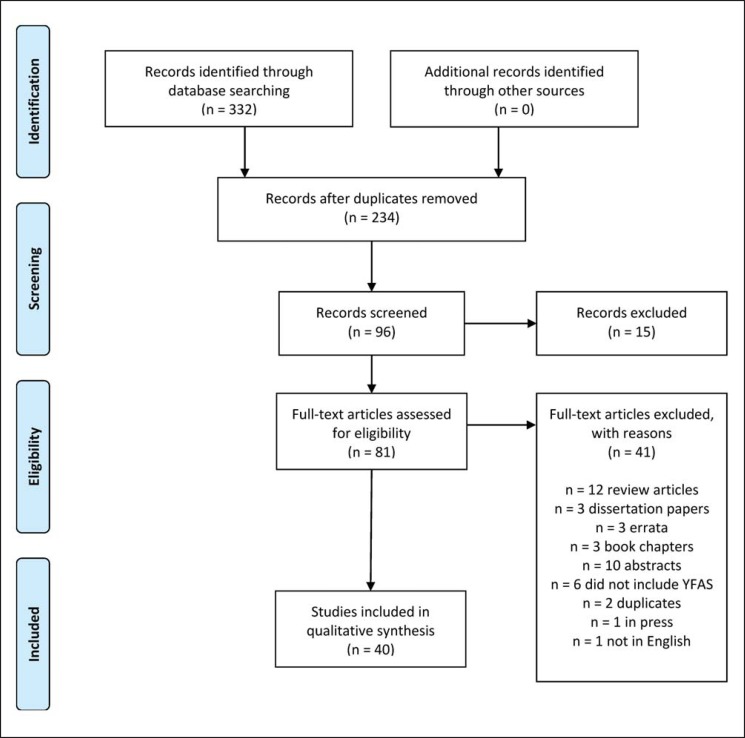
332 studies were initially identified using the search strategy. A flowchart outlining the data extraction method is presented in figure 1. After removing duplicates, 40 relevant studies met the predefined criteria for inclusion in this systematic review. Studies most commonly excluded were those that analysed or reviewed the validity and reliability of the YFAS or similar eating behaviour scales without reporting the prevalence or correlates of FA. Results were summarised according to two main categories: prevalence and correlates. A summary of results is included in supplemental table 1 (available at http://content.karger.com/ProdukteDB/produkte.asp?doi=442403).
Fig. 1.
PRISMA flowchart outlining the search strategy.
19 of the included studies recruited samples of obese or overweight individuals. Of these studies, 12 investigated the associations between YFAS diagnosis and weight loss treatment or surgery, including the prevalence of a YFAS endorsement before and after treatment (N = 4), weight loss outcomes (N = 5), remission of YFAS diagnosis following weight loss surgery (N = 1) and associations between YFAS diagnoses pre-surgery and substance or alcohol misuse post-surgery (N = 3). Two studies recruited individuals with BED. In both of these studies the participants were also overweight or obese, and in one of these investigations the sample was also seeking weight loss treatment. 18 studies investigated the prevalence and correlates of FA in the general population. Ten studies focused on female samples only; however, no studies recruited solely male participants, thus the remaining studies recruited both males and females (N = 30). One study used a sample of children whilst 2 studies recruited samples with eating disorders. The total number of participants across all included studies was 248,474, with sample sizes ranging from 27 to 57,321. 21 studies were published after 2013, whilst only one was published before 2010.
Results
Prevalence of Food Addiction
36 studies reported the prevalence of YFAS-determined FA in their respective samples. Seven studies reported the YFAS symptom count only, 14 reported the percentage of the sample meeting a dichotomous YFAS diagnosis, and a further 14 reported both. The remaining study did not adhere to the standardised scoring criteria for the YFAS [32]. Of these investigations, 19 reported the prevalence of a YFAS diagnosis in overweight or obese samples, 19 in the general population, 1 in children and 2 in samples with eating disorders, one of which specified BN only and the other included a sample with various ED subtypes. The prevalence of YFAS diagnosis within these clinical and non-clinical populations will be discussed further.
Overweight and Obese Samples
The prevalence of reported YFAS diagnoses was consistently greater in overweight and obese samples, relative to normal-weight or underweight individuals. Specifically, the prevalence of a dichotomous YFAS diagnosis in overweight or obese individuals ranged from 15.2% [33] to 56.8% [29] whilst the mean YFAS symptom count reported in these samples ranged from 2.57 [33] to 4.56 [29] out of a possible 7. A comparison of the median prevalence in the overweight or obese samples (33%) and general population (6.8%) reflects a 4 to 5 times greater YFAS prevalence in overweight and obese samples. This value exceeds previous findings by Avena et al. [34], who reported a two- to threefold increase in YFAS diagnosis in obese individuals compared to normal-weight samples, and the results of a meta-analysis by Pursey et al. [26], who reported that the prevalence of FA was doubled in the overweight/obese population compared with healthy weight individuals. The highest prevalence rates were reported in overweight and obese patients seeking weight loss surgery, in whom prevalence rates reached 53.7% [35].
Binge Eating Disorder and Bulimia Nervosa
Across all relevant studies, participants who met the YFAS diagnosis were significantly more likely to also fulfil BED criteria, supporting similar findings by Davis et al. [28]. The highest prevalence amongst individuals with BED was reported by Gearhardt et al. [29] and reached 56.8%, whilst the highest mean YFAS symptom count of 4.56 in a sample with BED was reported in the same study.
The prevalence of a YFAS diagnosis was found to be greater still in patients with BN. For example, Gearhardt et al. [36] reported the prevalence in BN patients to reach 83.6%, compared to 47.2% in individuals with BED. Additionally, in a study conducted by Meule et al. [30], all 26 patients with current BN scored sufficiently to qualify for YFAS diagnosis, compared with only 30% of remitted BN participants and none of the healthy control group.
Adult General Population
In the 19 studies that reported the prevalence of YFAS-diagnosed FA in the general population, the prevalence ranged from 0% [30] to 8.7% [37] whilst the mean YFAS symptom count ranged from 0.86 [30] to 3.05 [36].
Children
Only one study reported the prevalence of a YFAS diagnosis in children [38]. In this sample of 75 children, 7.2% met the YFAS diagnostic criteria. This study utilised the adapted version of the YFAS for children (YFAS-C), adapted from the original YFAS by referring to age-appropriate activities and adapting the questions to a lower reading grade. The YFAS-C was reviewed for clarity by a panel with expertise in addiction and childhood obesity and includes 25 questions that relate to the same diagnostic criteria as the original YFAS.
Additionally, in two retrospective studies [39,41], a positive association was found between the likelihood of endorsing a YFAS diagnosis and experiencing physical abuse, sexual abuse or post-traumatic stress disorder (PTSD) in childhood or adolescence. Furthermore, Davis et al. [28] reported a significant association between current YFAS diagnosis and those retrospectively meeting the criteria of a probable diagnosis of childhood ADHD.
Correlates of Food Addiction
Across all reviewed studies, a range of psychometric and demographic measures were assessed and their relationships with YFAS diagnoses were considered and quantified. The most commonly implicated outcome measures will be discussed further.
BMI
The majority of studies measured BMI within the sample, but not all reported the relationship between the YFAS and BMI. In studies recruiting participants with a range of BMIs (N = 18), YFAS diagnosis was found to be positively correlated with a higher current BMI [40] and a greater maximum reported adult BMI [36]. Specifically, Mason et al. [39] reported that female nurses meeting YFAS diagnostic criteria were 6 BMI units (kg/m2) heavier than those who did not meet the criteria, supporting the conclusions of Flint et al. [41] that those meeting a YFAS diagnosis are more likely to be overweight. In addition to this, Pedram et al. [42] reported that when individuals endorsing the YFAS criteria were classified according to their BMI, 11.4% of the so-called food addicts were under- or normal-weight whilst 88.6% were overweight/obese. A relationship between YFAS diagnosis and BMI was also found in children, whereby elevated scores on the YFAS-C were significantly positively correlated with higher BMI.
Conversely however, no difference in BMI between YFAS-diagnosed ‘food addicts’ and ‘non-food addicts’ was reported by Meule and Kubler [43] in a sample with a wide range of BMIs. A similar finding was reported in a sample where BMI fell within a healthy range [44]. Similarly, Gearhardt et al. [19] and Eichen et al. [33] found no correlation between BMI and YFAS scores; however, subjects who reported binge eating or compensatory behaviours were excluded from the sample. Additionally, Burgess et al. [45] reported that YFAS scores did predict some of the variance in BMI in their college student sample, but this association disappeared after binge eating scores were controlled for. Competing interpretations of this finding support either a moderating role for binge eating in the association between YFAS-diagnosed FA and BMI or that YFAS items may be confounded with binge eating scores and explain no additional variance.
Binge Eating Behaviour
17 studies measured binge eating behaviour in overweight or obese samples (N = 11), the general or healthy population (N = 5) and patients with eating disorders (N = 2). Results were consistent across studies, demonstrating that those meeting a YFAS diagnosis were more likely to report binge eating behaviour (e.g. [35,36]) or meet criteria for a BED diagnosis (e.g. [28,37]). For example, among subjects who met the YFAS diagnosis, 28.9% also endorsed clinical criteria for BED, compared with 4.1% of those who did not fulfil YFAS criteria [46].
Specifically, so-called food addicts reported more frequent binge eating episodes whereby number of binges per week was found to be correlated with YFAS scores [29,40,47]. YFAS symptom count was a significant correlate of frequency of binge eating episodes, even after controlling for troubled and emotional eating [24]. A dichotomous YFAS diagnosis was also identified as a significant predictor of the frequency of binge episodes in overweight or obese BED patients [29]. Furthermore, contrary to Boggiano et al. [48], YFAS score accounted for 11.1% of unique variance in binge eating episodes after controlling for the variance accounted for by depressive mood and eating disorder psychopathology [49]. In addition to this, YFAS symptom count correlated significantly with binge eating scores in both overweight patients and healthy weight controls [48]. This suggests that the relationship between binge eating and so-called FA can be found irrespective of weight status.
Psychological Wellbeing
Given the compromised psychological wellbeing commonly associated with substance addictions, for FA to warrant classification as an addiction it should be assumed that a clinical level of psychological impairment should exist. As such, 27 of the included studies have investigated associations between YFAS diagnoses and various markers of psychological wellbeing. These include depression (N = 10), general psychopathology (N = 2), substance (N = 6) and alcohol abuse (N = 6), ADHD (N = 1), PTSD (N = 1) and physical or sexual abuse in childhood or adolescence (N = 1).
The relationship between YFAS diagnoses and depression has generated mixed results. Several studies have reported a positive association of both a dichotomous YFAS diagnosis [30,33,41,50] and YFAS symptom count [27,51] with depression, whilst self-reported ‘food addicts’ have been reported to have a significantly higher prevalence of severe depression compared with ‘non-food addicts’ [28]. Such effects have persisted even in studies where subjects with major depressive disorder were excluded [33]. However, this association has not been replicated across the board, with some studies failing to report an association between YFAS diagnosis and mood disorders, negative affect as well as emotion dysregulation [49]. In a study by Imperatori et al. [46] on overweight and obese patients seeking weight loss therapy, it was reported that the relationship between YFAS diagnosis and psychopathology was fully accounted for by binge eating severity, therefore raising the likelihood of redundancy between binge eating scores and YFAS scores.
Researchers have investigated the relationship between so-called FA and clinically defined substance use disorders, such as alcohol and drug dependence. Again, findings have been mixed, with some researchers reporting an association between YFAS diagnosis and problematic substance use [35] and alcohol use [24]. However, in 2 samples of overweight or obese adults, no correlation between YFAS diagnosis and alcohol or drug use was reported [29,49], whilst Meule et al. [50] found that subjects endorsing YFAS criteria had lower scores on the Alcohol Use Disorder Identification Test (AUDIT).
In a sample of 141 adults post weight loss surgery, those meeting a pre-surgical YFAS diagnosis were more likely to report problematic substance use post-surgery [52]. Furthermore, those participants meeting a post-surgery problematic substance use were found to lose less weight. The authors argued that YFAS assessment of FA pre-surgery could help to prevent post-surgery substance use, a process consistent with ‘addiction transfer’ [52].
In the studies reporting ADHD, PTSD and sexual or physical abuse in childhood or adolescence [28,39,53], such disturbances were all found to be risk factors for so-called FA in adulthood. The likelihood of a YFAS diagnosis was further amplified if the abuse or trauma began at a younger age or lasted longer, suggesting a potential antecedence of psychological disturbance in childhood or adolescence in the presence of so-called FA in later life.
Weight Loss Outcomes
12 studies were reviewed that focused on the relationship between YFAS diagnostic criteria and weight loss. Of these, the majority (N = 9) recorded patients seeking weight loss treatment or bariatric surgery, whilst 1 reported patients currently undergoing treatment and 2 measured samples post treatment. Findings in this area were mixed. For example, Lent et al. [54] reported that, after controlling for treatment type, baseline weight and sex, YFAS symptom count did not significantly contribute to the variance in weight change following treatment. Furthermore, the presence of a dichotomous YFAS diagnosis at the start of the weight loss intervention study did not reduce subsequent weight loss, with patients who met YFAS criteria losing comparable amounts of weight as those who did not.
Interestingly, surgery-induced weight loss was reported to induce a remission in YFAS diagnoses in 93% of obese/overweight so-called food addicts [31]. In contrast however, Burmeister et al. [27] reported that those individuals with a YFAS diagnosis showed a reduced weight loss after a 7-week intervention. A similar but non-significant effect was also found by Clark and Saules [35]. These results outline the uncertainty of the status of FA in the treatment of obesity and cannot conclusively determine whether a YFAS diagnosis provides any useful information in a weight loss setting.
Discussion
The present systematic research review aimed to critically examine the existing literature investigating the prevalence and correlates of so-called FA in order to increase understanding of its current status as a hypothesised condition. The specific aims of this review are discussed below along with some critical issues encountered.
Prevalence and Correlates of Food Addiction
The prevalence of so-called FA, as diagnosed by the YFAS, has been reported in numerous populations. The highest prevalence rates of YFAS diagnoses were found in samples of overweight or obese individuals. However, contrary to some researchers' assumptions, the increased prevalence of a YFAS diagnosis in these samples does not validate the existence of FA as a novel behavioural phenotype which explains over-consumption. The high prevalence of YFAS-determined FA in obese and overweight samples has been suggested to provide evidence that so-called FA is contributing to the rising obesity epidemic in the general population. However, it is premature to suggest that this construct plays a causal role in the development of obesity, especially given that the vast majority of studies reviewed relied on cross-sectional designs, a point which is also acknowledged by Pursey et al. [26] as clouding ‘interpretation of cause and effect among variables’ (p. 4582). The label of FA may become attached to people destined to become obese due to a positive energy balance arising from multiple features of the obesogenic environment.
Similarly, high YFAS prevalence rates were identified in samples who engaged in binge eating behaviour. This has prompted authors to propose that so-called FA may be an atypical subtype of BED. However, the prevalence of YFAS diagnoses in obese samples with BED generally failed to reach 50% (e.g. [49]), suggesting either that a YFAS diagnosis is not synonymous with BED or obesity and therefore warrants consideration as a unique condition, or equally that the YFAS does not capture the full spectrum of heterogeneity that characterises the experience of individuals with BED or obesity. The question of whether a label of FA contributes any unique variance to a diagnosis of binge eating is an important issue that needs to be clarified.
It has been argued that so-called FA may be an extreme subtype of BED. Support for this idea comes from research by Davis et al. [55] who reported that a dopaminergic genetic profile could differentiate between those obese individuals who received a YFAS diagnosis and those who did not. This notion is further supported by Imperatori et al. [46] who noted that, although the prevalence of a YFAS diagnosis in obese samples with BED was very high, the prevalence was lower when studying obese populations without BED. The authors concluded that an atypical binge eating phenotype might exist in a small subgroup of obese individuals who also manifest other symptoms that are best captured by the YFAS compared to the Binge Eating Scale. However, even the most conservative prevalence estimates are still much higher than would be expected if so-called FA were simply a subtype of BED. Whether this suggests that FA may in fact be a less extreme subtype, reflecting a greater overlap and encompassing more of the behavioural phenotype associated with BED, or conversely that it is in fact distinct from BED to a greater extent than primarily suggested, is yet to be conclusively determined. To suggest that an obese individual who meets a YFAS diagnosis is at greater risk than a BED patient who does not meet a YFAS diagnosis therefore remains unsubstantiated.
One possibility proposed to explain the interrelationship between YFAS diagnosis, obesity status and binge eating is that binge eating could mediate the relationship between YFAS diagnosis and increasing BMI [45,46]. However, these mediation effects could also be attributed to the idea that the characteristics displayed by ‘addicted’ individuals may already be accounted for by scientifically validated binge eating diagnoses and definitions [30]. Longitudinal studies are required to disentangle these associations.
Despite this possibility, attempts to draw parallels between substance dependence and binge eating are restricted due to the differences in core psychopathology between these disorders. As suggested by Meule et al. [30], in BED and other eating disorders concerns regarding body weight and shape often drive dysfunctional eating patterns which, in turn, lead to binge eating episodes and possible compensatory behaviours. Such aspects are absent in other addictive behaviours like compulsive drug taking, rendering similarities between drug dependence and so-called FA tentative. Even when investigations are restricted to BED samples, many characteristics that are essential for diagnosis of substance dependence are not fully applicable to eating behaviours. For example, tolerance and withdrawal are particularly difficult to discern from processes of hunger and satiety when related to eating behaviour [33,56,57], This idea is supported by Ziauddeen and Fletcher [56] who concluded that the inconsistent nature of reported similarities between obesity, binge eating and so-called FA reflects the limited applicability of the ‘FA hypothesis’ which may be better represented by binge eating.
This idea can be extended to explain the high prevalence of YFAS diagnoses in patients with BN. Such a prevalence could be attributed simply to the overlapping symptoms between this condition and BED [48]. Few data are available with only 3 studies investigating the prevalence of YFAS diagnosis in BN patients. Interestingly, BN has been described as an extreme form of BED [58] with additional compensatory behaviours (such as purging, laxative use and excessive exercise). This might explain the increased prevalence of YFAS diagnoses seen in BN patients but also calls into question whether so-called FA in and of itself has a role as a biological cause of overeating.
Problems in Defining Food Addiction
Attempts to evaluate the literature on so-called FA are hindered by the lack of formal definition for this condition [23,34,59]. Few instruments other than the YFAS have been utilised to identify addictive eating behaviour [60]. For example, the Eating Behaviours Questionnaire (EBQ) developed for paediatric samples, consists of 20 hypothesised symptoms of FA based on adaptations of DSM-IV criteria for substance dependence [61]. Whilst Goodman's [62] broadened diagnostic criteria for addictive disorders have also been assessed in women with BED [63], the authors concluded that the classification of BED should remain an eating disorder. However, the most commonly used tool to quantify so-called FA symptomatology is the YFAS itself [24]. This poses problems in disentangling the existence of so-called FA as a clinical entity from the psychometric measurement of FA provided by the YFAS. The assessment of so-called FA using the YFAS has fuelled support for its existence as a valid clinical condition [23], despite diagnoses being based on self-report responses, frequently in individuals who are motivated to assign responsibility for their problematic eating behaviour to factors beyond their control, a point that was also raised in the meta-analysis by Pursey et al. [26].
Applying the term ‘addiction’ to food is further impeded as the semantics of this label are fluid and may no longer be appropriate. For example, drug-related conditions are no longer labelled addictions but ‘substance-related disorders’. It therefore seems unhelpful to persist with the term FA, especially as its supposed diagnosis arises from a questionnaire based on the criteria for substance dependence. There is a risk that the term ‘FA’ could be used by some investigators for dramatic effect or to make the diagnosis appear toxic.
Whilst YFAS-diagnosed FA does seem to identify individuals with certain maladaptive eating behaviours [19,24,33,39], problems are inherent in the direct application of the DSM-IV-TR criteria for substance dependence as the basis of a psychometric tool for so-called FA. The diagnostic labels in the DSM are intended for trained and experienced clinicians rather than a checklist for self-diagnosis. Indeed, the diagnosis of any other scientifically validated addictive or eating disorder would not rely on a self-report questionnaire as justification for diagnosis. Furthermore, defining so-called FA under the same criteria as substance dependence and addictive behaviour is controversial because, unlike drugs or gambling, food and eating are essential for survival. There is disagreement over the equivalence of symptoms of substance use disorders and the appropriateness of their application to so-called FA [23,30], especially given the abundance of foods in the diet that contain high proportions of the various candidate ‘addictive agents’ (e.g. fats, sugars and salt).
One feature of the YFAS is the inclusion of two items designed to indicate ‘clinical impairment’, which must both be met in order to warrant an affliction on a similar level as would be expected in a drug-addicted individual. However, few studies have actually investigated the level of clinical impairment experienced by individuals who meet the YFAS diagnosis [28]. Instead, researchers tend to favour the YFAS symptom count score as it yields more power to detect relationships in small samples [27], despite there being a lack of evidence to support this continuum [56]. However, the use of the YFAS score or symptom count does not in itself imply an identification of FA. The use of a single instrument (the YFAS) to identify FA introduces the possibility of a circular argument. To the question ‘Why is this person a food addict?’, the answer is ‘Because of a high score on the YFAS’. But the answer to the question ‘Why does this person score high on the YFAS?’, the answer is ‘Because he/she is a food addict’. The circularity of this deduction can only be broken by the assignation of separate clinical symptoms of FA that are independent of the YFAS score.
Whilst there is a plausible rationale for adopting an addiction model in understanding the spectrum of overeating across individuals [23], for this concept to progress into a distinct clinical entity will require scientific development and understanding beyond those existing clinical diagnoses of eating disorders and definitions of addiction, and into a coherent model of FA, encompassing and identifying the precise psychological impairments specific to those endorsing the spectrum of traits associated with the condition.
The methodologies adopted to examine the context of so-called FA are to date limited. Only three studies [19,42,64] analysed the YFAS and its relationship with actual food choice or intake. This weakens the argument suggesting that certain foods or food groups may be addictive (e.g. [11,13]) as the behavioural evidence in human populations to support such claims is not yet established. Furthermore, several authors have adopted language in their studies that appears to confirm the existence of so-called FA, such as ‘hyper-palatable’ and ‘addictive response’. Just like the term ‘FA’ itself, these terms do not have a clear definition and can be used to layer a biased interpretation on top of otherwise neutral data.
As mentioned previously, a further limitation of the YFAS is its design based on the now outdated DSM-IV symptom criteria. In 2013, the 5th edition of the DSM was published, reflecting major changes made to the previously titled ‘Substance-Related Disorders’ chapter [21]. This category was re-named to ‘Substance-Related and Addictive Disorders’ and further subdivided into ‘Substance-Related Disorders’ and ‘Non-Substance-Related Disorders’ [65]. Despite some postulations (e.g. [13,66,67]), no specific food or ingredient has yet to be conclusively characterised as an addictive agent in humans, furthermore gambling disorder was the sole behavioural condition acknowledged under the non-substance-related disorders category. One explanation for the lack of recognition of FA under the DSM-V can be attributed to the idea that the term generates confusion and conflicting accounts as it straddles both substance-related and non-substance-related disorders [17]. There are researchers who strongly implicate certain foods, such as highly processed foods [13], which they argue may be more likely to trigger an addiction in susceptible individuals via similar mechanisms as drugs of abuse [19]. However, contrasting views have suggested that simply the behaviour of eating is potentially addictive [17,68], triggering debate over whether overeating, to the extent where it reflects an addiction, is best conceptualised as a maladaptive pattern of behaviour or as a substance-related disorder. In response to this, the term ‘eating addiction’ [6] has been proposed to acknowledge addiction to eating on a behavioural level, although this label is yet to be debated in the literature. Moreover the term ‘eating addiction’ retains the semantically charged term ‘addiction’ rather than a more neutral term which might be better suited to the provisional recognition of the condition.
In light of the DSM-V, only two symptoms now need to be met in order for an individual to be given a diagnosis of substance dependence, compared to three symptoms in the DSM-IV. If such criteria are adapted for the psychometric assessment of so-called FA, it is likely that the current prevalence estimates for the diagnosis of FA will no longer apply due to lower diagnostic thresholds [68]. Future research that utilises the DSM-V should therefore attempt to extricate the diagnostic criteria for FA from the existing classification for substance use disorders in order to avoid over-diagnosis and misleading prevalence estimates.
Problems in Identifying Addictive Foods
Many researchers are turning their attention to identifying specific foods or ingredients that may have the ability to trigger a so-called addictive response in susceptible individuals. Such ‘addictive agents’ [13] include ingredients that are added to enhance the palatability of foods, without necessarily increasing the nutritional value. Refined carbohydrates, fat and salt, often in combination, are commonly identified in highly processed foods and are frequently associated with excessive consumption [69]. It is unsurprising, therefore, that patients with BED often identify foods high in these ingredients as triggering binge episodes [28]. Furthermore, the foods listed on the YFAS, which individuals commonly identify as having difficulty controlling, are mostly highly processed foods, such as chips, pizza, pastries, savoury snacks and soda pop [24].
However, the extrapolation of these limited reports to support the idea that highly processed foods can trigger an addiction is as yet unwarranted, given that the majority of these outputs rely on a very small number of studies conducted in animal models. Whilst rodents can display behavioural phenomena resembling addiction symptomatology, such as withdrawal from high-fat foods (whereby behavioural anxiety and depression are displayed) [70] and persistent seeking of sugar via lever pressing [11], behavioural evidence of these effects has not been replicated in humans [56]. At this stage, the most scientifically secure conclusion is that the availability and consumption of palatable foods has the potential to alter behaviour and activate the neural circuitry implicated in food reward. Whether these activations have the power to develop a dependence on such foods in the same way as would be expected with drugs of abuse is yet to be established. This is particularly difficult to achieve as, unlike drugs, foods are consumed ubiquitously and are necessary for survival [56].
Usefulness of the Term ‘Food Addiction’
One issue still to resolve is the extent to which so-called FA is a novel label for susceptibility to already known forms of overeating [22]. This behaviour is well documented and defined by clinically recognised conditions such as BED [63]. Vainik et al. [71] suggested that many common eating-related traits can all be captured by a single factor, labelled ‘uncontrolled eating’ (p. 229), presented on a continuum indicating severity. This continuum model is in line with that proposed by Davis [22] and further highlights the overlaps between the hypothesised classification of FA and existing maladaptive eating behaviour phenotypes. However, such a continuum does not justify the acceptance of so-called FA as a distinct clinical entity. At the present time, the concept of so-called FA at the individual level as a putative biological cause of overeating is controversial and lacks convincing support. The term is also not widely regarded as helpful by clinicians in advancing scientific understanding of eating disorders or as an explanation for obesity.
Conclusion
This systematic review of 40 studies is the largest to date and has uncovered mixed results regarding the prevalence and correlates of so-called FA. Notably, YFAS scores were higher in overweight or obese samples or those with BED, prompting researchers to conclude that FA may be a subtype of BED, reflecting many of the problematic eating behaviours endorsed by those who have been unsuccessful in controlling their weight. However, the existence of a growing body of uncritical scientific literature, which makes the assumption that so-called FA is a true condition, may hinder progress in identifying preventable causes of overeating. The designation of any new putative mental disorder should not be taken lightly but should contribute novel information to the field which assists in explaining or treating pathology and should not overlap extensively with existing validated explanations and disorders. As a counter to this, a body of objective scientific research is required to investigate the utility of the concept of FA in the current scientific literature before it is accepted by the scientific population and communicated to the public, for example, by objectively measuring energy intake (EI) and macronutrient choice following a dietary manipulation and comparing EI in ‘food addicted’ versus healthy individuals. At the present time there is a need for well-funded large-scale scientifically controlled trials preferably carried out by un-biased researchers. At this stage, and consistent with scientific practice, the existence of so-called FA and its relationship with other psychological processes should be regarded as inconclusive until such time as the evidence base becomes stronger.
Disclosure Statement
The authors declared no conflict of interest.
References
- 1.World Health Organisation (WHO) Factsheet on Obesity and Overweight. Fact sheet N°311, updated January2015. Geneva: WHO; 2015. www.who.int/mediacentre/factsheets/fs311/en/ (last accessed November 16, 2015). [Google Scholar]
- 2.National Heart Lung and Blood Institute . Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda: National Heart Lung and Blood Institute; 1998. [Google Scholar]
- 3.Swinburn B., Sacks G, Ravussin E. Increased food energy supply is more than sufficient to explain the US epidemic of obesity. Am J Clin Nutr. 2009;90:1453–1456. doi: 10.3945/ajcn.2009.28595. [DOI] [PubMed] [Google Scholar]
- 4.Vandevijvere S., Chow CC, Hall KD, Umalia E, Swinburn BA. Increased food energy supply as a major driver of the obesity epidemic: a global analysis. Bull World Health Organ. 2015;93:446–456. doi: 10.2471/BLT.14.150565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Church TS, Martin CK, Thompson AM, Earnest CP, Mikus CR, Blair SN. Changes in weight, waist circumference and compensatory responses with different doses of exercise among sedentary, overweight postmenopausal women. PloS ONE. 2009;4:e4515. doi: 10.1371/journal.pone.0004515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hebebrand J, Albayrak Ö, Adan R, Antel J, Dieguez C, de Jong J, Leng G, Menzies J, Mercer JG, Murphy M, van der Plasse G, Dickson SL. ‘Eating addiction’, rather than ‘food addiction’, better captures addictive-like eating behavior. Neurosci Biobehav Rev. 2014;47:295–306. doi: 10.1016/j.neubiorev.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 7.Randolph TG. The descriptive features of food addiction; addictive eating and drinking. Q J Stud Alcohol. 1956;17:198–224. [PubMed] [Google Scholar]
- 8.Hetherington MM, Macdiarmid JI. ‘Chocolate addiction’: a preliminary study of its description and its relationship to problem eating. Appetite. 1993;21:233–246. doi: 10.1006/appe.1993.1042. [DOI] [PubMed] [Google Scholar]
- 9.Rozin P, Levine E, Stoess C. Chocolate craving and liking. Appetite. 1991;17:199–212. doi: 10.1016/0195-6663(91)90022-k. [DOI] [PubMed] [Google Scholar]
- 10.Tuomisto T, Hetherington MM, Morris MF, Tuomisto MT, Turjanmaa V, Lappalainen R. Psychological and physiological characteristics of sweet food ‘addiction’. Int J Eat Disord. 1999;25:169–175. doi: 10.1002/(sici)1098-108x(199903)25:2<169::aid-eat6>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 11.Avena NM, Rada P, Hoebel BG. Evidence for sugar addiction: behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev. 2008;32:20–39. doi: 10.1016/j.neubiorev.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Benton D. The plausibility of sugar addiction and its role in obesity and eating disorders. Clin Nutr. 2010;29:288–303. doi: 10.1016/j.clnu.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Schulte EM, Avena NM, Gearhardt AN. Which foods may be addictive? the roles of processing, fat content, and glycemic load. PLoS ONE. 2015;10:e0117959. doi: 10.1371/journal.pone.0117959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cocores JA, Gold MS. The salted food addiction hypothesis may explain overeating and the obesity epidemic. Med Hypotheses. 2009;73:892–899. doi: 10.1016/j.mehy.2009.06.049. [DOI] [PubMed] [Google Scholar]
- 15.Kromann CB, Nielsen CT. A case of cola dependency in a woman with recurrent depression. BMC Res Notes. 2012;5:692. doi: 10.1186/1756-0500-5-692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gold MS, Frost-Pineda K, Jacobs WS. Overeating, binge eating, and eating disorders as addictions. Psychiatric Ann. 2003;33:117–122. [Google Scholar]
- 17.Davis C, Loxton NJ. A psycho-genetic study of hedonic responsiveness in relation to ‘food addiction’. Nutrients. 2014;6:4338–4353. doi: 10.3390/nu6104338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Montague CT, Farooqi IS, Whitehead JP, Soos MA, Rau H, Wareham NJ, Sewter CP, Digby JE, Mohammed SN, Hurst JA, Cheetham CH, Earley AR, Barnett AH, Prins JB, O'Rahilly S. Congenital leptin deficiency is associated with severe early-onset obesity in humans. Nature. 1997;387:903–908. doi: 10.1038/43185. [DOI] [PubMed] [Google Scholar]
- 19.Gearhardt AN, Yokum S, Orr PT, Stice E, Corbin WR, Brownell KD. Neural correlates of food addiction. Arch Gen Psychiatry. 2011;68:808–816. doi: 10.1001/archgenpsychiatry.2011.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parylak SL, Koob GF, Zorrilla EP. The dark side of food addiction. Physiol Behav. 2011;104:149–156. doi: 10.1016/j.physbeh.2011.04.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Text Revision (DSM-IV-TR). Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 22.Davis C. Compulsive overeating as an addictive behavior: overlap between food addiction and binge eating disorder. Curr Obes Rep. 2013;2:171–178. [Google Scholar]
- 23.Ziauddeen H, Farooqi IS, Fletcher PC. Obesity and the brain: how convincing is the addiction model? Nat Rev Neurosci. 2012;13:279–286. doi: 10.1038/nrn3212. [DOI] [PubMed] [Google Scholar]
- 24.Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the Yale Food Addiction Scale. Appetite. 2009;52:430–436. doi: 10.1016/j.appet.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 25. Gearhardt AN, Corbin WR, Brownell KD. Yale Food Addiction Scale (YFAS). Measurement Instrument Database for the Social Sciences 2012. www.midss.org/content/yale-food-addiction-scale-yfas (last accessed November 16, 2015).
- 26.Pursey KM, Stanwell P, Gearhardt AN, Collins CE, Burrows TL. The prevalence of food addiction as assessed by the Yale Food Addiction Scale: a systematic review. Nutrients. 2014;6:4552–4590. doi: 10.3390/nu6104552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Burmeister JM, Hinman N, Koball A, Hoffmann DA, Carels RA. Food addiction in adults seeking weight loss treatment. Implications for psychosocial health and weight loss. Appetite. 2013;60:103–110. doi: 10.1016/j.appet.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 28.Davis C, Curtis C, Levitan RD, Carter JC, Kaplan AS, Kennedy JL. Evidence that ‘food addiction’ is a valid phenotype of obesity. Appetite. 2011;57:711–717. doi: 10.1016/j.appet.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 29.Gearhardt AN, White MA, Masheb RM, Morgan PT, Crosby RD, Grilo CM. An examination of the food addiction construct in obese patients with binge eating disorder. Int J Eat Disord. 2012;45:657–663. doi: 10.1002/eat.20957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meule A, von Rezori V, Blechert J. Food addiction and bulimia nervosa. Eur Eat Disord Rev. 2014;22:331–337. doi: 10.1002/erv.2306. [DOI] [PubMed] [Google Scholar]
- 31.Pepino MY, Stein RI, Eagon JC, Klein S. Bariatric surgery-induced weight loss causes remission of food addiction in extreme obesity. Obesity (Silver Spring) 2014;22:1792–1798. doi: 10.1002/oby.20797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Karlsson HK, Tuominen L, Tuulari JJ, Hirvonen J, Parkkola R, Helin S, Salminen P, Nuutila P, Nummenmaa L. Obesity is associated with decreased micro-opioid but unaltered dopamine D2 receptor availability in the brain. J Neurosci. 2015;35:3959–3965. doi: 10.1523/JNEUROSCI.4744-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eichen DM, Lent MR, Goldbacher E, Foster GD. Exploration of ‘food addiction’ in overweight and obese treatment-seeking adults. Appetite. 2013;67:22–24. doi: 10.1016/j.appet.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Avena NM, Gearhardt AN, Gold MS, Wang GJ, Potenza MN. Tossing the baby out with the bathwater after a brief rinse? The potential downside of dismissing food addiction based on limited data. Nat Rev Neurosci. 2012;13:514–514. doi: 10.1038/nrn3212-c1. [DOI] [PubMed] [Google Scholar]
- 35.Clark SM, Saules KK. Validation of the Yale Food Addiction Scale among a weight-loss surgery population. Eat Behav. 2013;14:216–219. doi: 10.1016/j.eatbeh.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 36.Gearhardt AN, Boswell RG, White MA. The association of ‘food addiction’ with disordered eating and body mass index. Eat Behav. 2014;15:427–433. doi: 10.1016/j.eatbeh.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brunault P, Ballon N, Gaillard P, Réveillère C, Courtois R. Validation of the French version of the Yale Food Addiction Scale: an examination of its factor structure, reliability, and construct validity in a nonclinical sample. Can J Psychiatry. 2014;59:276–284. doi: 10.1177/070674371405900507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gearhardt AN, Roberto CA, Seamans MJ, Corbin WR, Brownell KD. Preliminary validation of the Yale Food Addiction Scale for children. Eat Behav. 2013;14:508–512. doi: 10.1016/j.eatbeh.2013.07.002. Erratum in Eat Behav 2014;15:334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mason SM, Flint AJ, Field AE, Austin SB, Rich-Edwards JW. Abuse victimization in childhood or adolescence and risk of food addiction in adult women. Obesity (Silver Spring) 2013;21:E775–781. doi: 10.1002/oby.20500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Granero R, Hilker I, Agüera Z, Jiménez-Murcia S, Sauchelli S, Islam MA, Fagundo AB, Sánchez I, Riesco N, Dieguez C, Soriano J, Salcedo-Sánchez C, Casanueva FF, De la Torre R, Menchón JM, Gearhardt AN, Fernández-Aranda F. Food addiction in a Spanish sample of eating disorders: DSM-5 diagnostic subtype differentiation and validation data. Eur Eat Disord Rev. 2014;22:389–396. doi: 10.1002/erv.2311. [DOI] [PubMed] [Google Scholar]
- 41.Flint AJ, Gearhardt AN, Corbin WR, Brownell KD, Field AE, Rimm EB. Food-addiction scale measurement in 2 cohorts of middle-aged and older women. Am J Clin Nutr. 2014;99:578–586. doi: 10.3945/ajcn.113.068965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pedram P, Wadden D, Amini P, Gulliver W, Randell E, Cahill F, Vasdev S, Goodridge A, Carter JC, Zhai G, Ji Y, Sun G. Food addiction: its prevalence and significant association with obesity in the general population. PLoS One. 2013;8:e74832. doi: 10.1371/journal.pone.0074832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Meule A, Kubler A. Food cravings in food addiction: the distinct role of positive reinforcement. Eat Behav. 2012;13:252–255. doi: 10.1016/j.eatbeh.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 44.Meule A, Lutz A, Vögele C, Kübler A. Women with elevated food addiction symptoms show accelerated reactions, but no impaired inhibitory control, in response to pictures of high-calorie food-cues. Eat Behav. 2012;13:423–428. doi: 10.1016/j.eatbeh.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 45.Burgess EE, Turan B, Lokken KL, Morse A, Boggiano MM. Profiling motives behind hedonic eating. Preliminary validation of the Palatable Eating Motives Scale. Appetite. 2014;72:66–72. doi: 10.1016/j.appet.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 46.Imperatori C, Innamorati M, Contardi A, Continisio M, Tamburello S, Lamis DA, Tamburello A, Fabbricatore M. The association among food addiction, binge eating severity and psychopathology in obese and overweight patients attending low-energy-diet therapy. Compr Psychiatry. 2014;55:1358–1362. doi: 10.1016/j.comppsych.2014.04.023. [DOI] [PubMed] [Google Scholar]
- 47.Meule A, Hermann T Kübler A. Food addiction in overweight and obese adolescents seeking weight-loss treatment. Eur Eat Disord Rev. 2015;23:193–198. doi: 10.1002/erv.2355. [DOI] [PubMed] [Google Scholar]
- 48.Boggiano MM, Burgess EE, Turan B, Soleymani T, Daniel S, Vinson LD, Lokken KL, Wingo BC, Morse A. Motives for eating tasty foods associated with binge-eating. Results from a student and a weight-loss seeking population. Appetite. 2014;83:160–166. doi: 10.1016/j.appet.2014.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gearhardt AN, White MA, Masheb RM, Grilo CM. An examination of food addiction in a racially diverse sample of obese patients with binge eating disorder in primary care settings. Compr Psychiatry. 2013;54:500–505. doi: 10.1016/j.comppsych.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Meule A, Heckel D, Jurowich CF, Vögele C, Kübler A. Correlates of food addiction in obese individuals seeking bariatric surgery. Clin Obes. 2014;4:228–236. doi: 10.1111/cob.12065. [DOI] [PubMed] [Google Scholar]
- 51.Meule A, Kübler A. Food cravings in food addiction: the distinct role of positive reinforcement. Eat Behav. 2012;13:252–255. doi: 10.1016/j.eatbeh.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 52.Reslan S, Saules KK, Greenwald MK, Schuh LM. Substance misuse following Roux-en-Y gastric bypass surgery. Subst Use Misuse. 2014;49:405–417. doi: 10.3109/10826084.2013.841249. [DOI] [PubMed] [Google Scholar]
- 53.Mason SM, Flint AJ, Roberts AL, Agnew-Blais J, Koenen KC, Rich-Edwards JW. Posttraumatic stress disorder symptoms and food addiction in women by timing and type of trauma exposure. JAMA Psychiatry. 2014;71:1271–1278. doi: 10.1001/jamapsychiatry.2014.1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lent MR, Eichen DM, Goldbacher E, Wadden TA, Foster GD. Relationship of food addiction to weight loss and attrition during obesity treatment. Obesity (Silver Spring) 2014;22:52–55. doi: 10.1002/oby.20512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Davis C, Loxton NJ, Levitan RD, Kaplan AS, Carter JC, Kennedy JL. ‘Food addiction’ and its association with a dopaminergic multilocus genetic profile. Physiol Behav. 2013;118:63–69. doi: 10.1016/j.physbeh.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 56.Ziauddeen H, Fletcher PC. Is food addiction a valid and useful concept? Obes Rev. 2013;14:19–28. doi: 10.1111/j.1467-789X.2012.01046.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Meule A., Kübler A. The translation of substance dependence criteria to food-related behaviors: different views and interpretations. Front Psychiatry. 2012;3:64. doi: 10.3389/fpsyt.2012.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fairburn CG, Cooper Z, Doll HA, Norman P, OʼConnor M. The natural course of bulimia nervosa and binge eating disorder in young women. Arch Gen Psychiatry. 2000;57:659–665. doi: 10.1001/archpsyc.57.7.659. [DOI] [PubMed] [Google Scholar]
- 59.Ziauddeen H, Farooqi IS, Fletcher PC. Food addiction: is there a baby in the bathwater? Nat Rev Neurosci. 2012;13:514–514. [Google Scholar]
- 60.Meule A. Food addiction and body-mass-index: a non-linear relationship. Med Hypotheses. 2012;79:508–511. doi: 10.1016/j.mehy.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 61.Merlo LJ, Klingman C, Malasanos TH, Silverstein JH. Exploration of food addiction in pediatric patients: a preliminary investigation. J Addict Med. 2009;3:26–32. doi: 10.1097/ADM.0b013e31819638b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Goodman A. Addiction: definition and implications. Br J Addict. 1990;85:1403–1408. doi: 10.1111/j.1360-0443.1990.tb01620.x. [DOI] [PubMed] [Google Scholar]
- 63.Cassin SE, von Ranson KM. Is binge eating experienced as an addiction? Appetite. 2007;49:687–690. doi: 10.1016/j.appet.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 64.Davis C, Levitan RD, Kaplan AS, Kennedy JL, Carter JC. Food cravings, appetite, and snack-food consumption in response to a psychomotor stimulant drug: the moderating effect of ‘food-addiction’. Front Psychol. 2014;5:403. doi: 10.3389/fpsyg.2014.00403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 66.Gearhardt AN, Grilo CM, DiLeone RJ, Brownell KD, Potenza MN. Can food be addictive? Public health and policy implications. Addiction. 2011;106:1208–1212. doi: 10.1111/j.1360-0443.2010.03301.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rizk MT, Treat TA. The association of food characteristics and individual differences with ratings of craving and liking. Appetite. 2014;79:166–173. doi: 10.1016/j.appet.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 68.Meule A, Gearhardt AN. Food addiction in the light of DSM-5. Nutrients. 2014;6:3653–3671. doi: 10.3390/nu6093653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Weingarten HP, Elston D. Food cravings in a college population. Appetite. 1991;17:167–175. doi: 10.1016/0195-6663(91)90019-o. [DOI] [PubMed] [Google Scholar]
- 70.Avena NM, Rada P, Hoebel BG. Sugar and fat bingeing have notable differences in addictive-like behavior. J Nutr. 2009;139:623–628. doi: 10.3945/jn.108.097584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vainik U, Neseliler S, Konstabel K, Fellows LK, Dagher A. Eating traits questionnaires as a continuum of a single concept. Uncontrolled eating. Appetite. 2015;90:229–239. doi: 10.1016/j.appet.2015.03.004. [DOI] [PubMed] [Google Scholar]