Abstract
Objective
To examine the relationship between sleep duration and non-alcoholic fatty liver disease (NAFLD).
Methods
We evaluated 3,968 subjects who underwent health check-ups from June 2012 to May 2013 at the Watari Hospital Health Center in Fukushima Prefecture in Japan. Fatty liver was detected by ultrasonography. Sleep duration and lifestyle factors were estimated using a questionnaire. Sleep duration was categorized into the following groups: ≤6, 6 to ≤7, >7 to ≤8, and >8 h. The four sleep duration groups were compared using the χ2 test and Kruskal-Wallis test.
Results
In total, 2,172 subjects were enrolled. The overall prevalence of NAFLD was 29.6% (men, 38.0%; women, 25.3%). The proportion of NAFLD tended to decrease as sleep duration increased in men. The proportion with NAFLD was lowest in the group with a sleep duration of 6 to ≤7 h and highest in the groups with sleep durations of ≤6 and >8 h in women. The distribution showed a U-shaped curve. The age-adjusted odds ratio (OR) (95% confidence interval (CI)) for subjects with NAFLD with a sleep duration ≤6 h compared to the reference (6 to ≤7 h) was 1.44 (1.06-1.96) in women.
Conclusion
Sleep shortage tends to be associated with NAFLD in women and may be mediated by body adiposity.
Key Words: NAFLD, s; Short sleep duration; U-shaped curve; Women
Introduction
Sleep is important to maintain body homeostasis, and sleep disturbances are common health problems in modern societies. One epidemiologic study estimated that 21.4% of the Japanese general population suffered from insomnia [1].
Usual sleep duration is closely associated with the risk for obesity, diabetes mellitus, hypertension, cardiovascular disease, and detrimental serum lipid levels [2,3,4,5,6,7]. Recently, Kim et al. [8] indicated that there was a significant association between an increased risk of non-alcoholic fatty liver disease (NAFLD) and short sleep duration or poor sleep quality in middle-aged Koreans. Similarly, short sleep duration was closely associated with fatty liver among Japanese men, although alcoholic fatty liver was not excluded from the analysis [9].
Sleep apnea syndrome (SAS) is the most well-known and well-described sleep disturbance associated with NAFLD [10]; however, the prevalence of SAS in Japan is estimated to be only 2-4% [11]. NAFLD is present in 29.7% of adults in Japan [12]. Therefore, it is impossible to explain the association between sleep disturbance and NAFLD only by SAS. Here, we investigated the association of sleep duration with NAFLD.
Material and Methods
Subjects
Subjects for this study consisted of 3,968 Japanese men and women who underwent health check-ups from June 2012 through May 2013 at the Watari Hospital Health Center in Fukushima, Japan. We excluded 1,065 subjects with insufficient data, 400 subjects reporting an alcohol intake of ≥20 g/day, 305 subjects taking sleeping pills, and 26 subjects with evidence of liver disease. NAFLD was defined as fatty liver detected by ultrasonography in the absence of other causes of chronic liver disease (i.e., hepatitis C antibody-negative, hepatitis B surface antigen-negative, and alcoholic consumption < 20 g/day). Accordingly, 2,172 subjects (731 men, 1,441 women) were eligible for this study. Because characteristics differed by sex, we examined men and women separately. The study protocol was approved by the Ethics Committee of Watari Hospital and Fukushima Medical University School of Medicine (both in Fukushima, Japan). All patients provided written informed consent prior to study participation, and this study was conducted in conformity with the ethical guidelines of the 1975 Declaration of Helsinki [13] and its amendments of 1983, 1989, and 1996 [14].
Measurements
Before the examination, subjects were asked to complete a questionnaire regarding their ordinary sleep habits, sleep duration, presence or absence of sleep apnea, poor sleep (deficiency of sleep satisfaction or difficulty of awakening easily), current medication for diabetes or insomnia, and lifestyle factors (regular exercise, eating habits such as no breakfast and snacking). Regular exercise was defined as at least one 30-min session at least once per week. No breakfast was defined as not eating breakfast at least three times per week, and snacking was defined as snacking or eating meals after dinner at least three times per week. Subjects were examined after an overnight fast. Ultrasonography (LogiQ 7; GE Health Care, Piscataway, NJ, USA, and Pro Sound alpha-7; Hitachi Aloka Medical, Tokyo, Japan) was used to evaluate hepatic steatosis. An ultrasonographic diagnosis of fatty liver was defined as a bright liver, increased liver echotexture compared with kidneys, vascular blurring, and deep attenuation of the liver. Diabetes was defined as fasting plasma glucose ≥ 126 mg/dl and/or current medication for diabetes.
Statistical Analysis
Sleep duration was categorized into the following groups: ≤ 6, 6 to ≤7, >7 to ≤8, and >8 h. The two groups (men and women) were compared using Mann-Whitney U test. The four sleep duration groups were compared using the χ2 test and the Kruskal-Wallis test. Odds ratios (OR) and 95% confidence intervals (95% CI) were used to measure the association of the risk of NAFLD or lifestyle factors with sleep duration categories. The age-adjusted ORs for NAFLD or lifestyle factors were compared by logistic regression with sleep duration. Sleep duration of 6 to ≤7 h was defined as a reference point because this was the most frequent classification provided by subjects. Statistical analyses were performed using SPSS 17.0 for Windows (SPSS, Inc., Chicago, IL, USA). A p value < 0.05 was considered significant.
Results
In total, 2,172 subjects were enrolled. The overall prevalence of NAFLD was 29.6% (men 38.0%; women 25.3%). Table 1 shows baseline characteristics of all study participants. Although mean age did not differ between men and women, BMI (p < 0.001) and the proportion of patients with NAFLD (p < 0.001) were significantly higher in men than in women. The mean sleep duration was significantly longer in men than in women (7.3 ± 1.1 vs. 6.9 ± 1.1 h; p < 0.001). The proportion of subjects with sleep apnea was significantly higher in men than in women (19.2 vs. 3.7%; p < 0.001), and the proportion of subjects with poor sleep was significantly higher in women than in men (36.6 vs. 30.8%; p = 0.007).
Table 1.
Subjects’ characteristics a
| Total | Men | Women | p value | |
|---|---|---|---|---|
| Number | 2172 | 731 | 1441 | – |
| Age, years* | 60.9 ± 12.7 | 61.5 ± 13.7 | 60.6 ± 12.2 | 0.152 |
| Sleep duration, h* | 7.0 ± 1.1 | 7.3 ± 1.1 | 6.9 ± 1.1 | <0.001 |
| BMI, kg/m2 * | 22.8 ± 3.3 | 23.5 ± 3.2 | 22.5 ± 3.3 | <0.001 |
| BMI ≤25 to <30 kg/m2, % | 19.8 | 24.9 | 17.2 | <0.001 |
| BMI ≤ 30 kg/m2, % | 2.9 | 3.6 | 2.5 | 0.162 |
| Current smoker, % | 10.9 | 21.2 | 5.6 | <0.001 |
| Regular exercise, % | 50.3 | 54.4 | 48.2 | 0.006 |
| Sleep apnea, % | 8.8 | 19.2 | 3.7 | <0.001 |
| Poor sleep, % | 34.6 | 30.8 | 36.6 | 0.007 |
| Diabetes, % | 6.5 | 10.1 | 4.6 | <0.001 |
| Fatty liver, % | 29.6 | 38.0 | 25.3 | <0.001 |
| AST, U/l** | 22 (9–168) | 21 (10–93) | 20 (9–168) | <0.001 |
| ALT, U/l** | 17 (4–202) | 20 (6–127) | 16 (4–202) | <0.001 |
| γ-GTP, U/l** | 21 (7–380) | 27 (7–380) | 17 (7–180) | <0.001 |
| ALP, U/l** | 204 (74–760) | 205 (74–760) | 206 (79–722) | 0.245 |
| Triglyceride, mg/dl** | 87 (20–567) | 93 (31–567) | 81 (20–380) | <0.001 |
| LDL-C, mg/dl** | 120 (37–248) | 118 (48–232) | 125 (37–248) | <0.001 |
| HDL-C, mg/dl** | 57 (28–123) | 51 (28–104) | 61 (28–123) | <0.001 |
AST = Asparate aminotransferase; ALT = alanine aminotransferase; γ-GTP = gamma-glutamyl transpeptidase; ALP = alkaline phosphatase; LDL-C = low-density lipoprotein cholesterol; HDL-C = high-density lipoprotein cholesterol.
Data were statistically analyzed using Mann-Whitney U and χ2 tests.
Means (± standard deviation).
Medians (range).
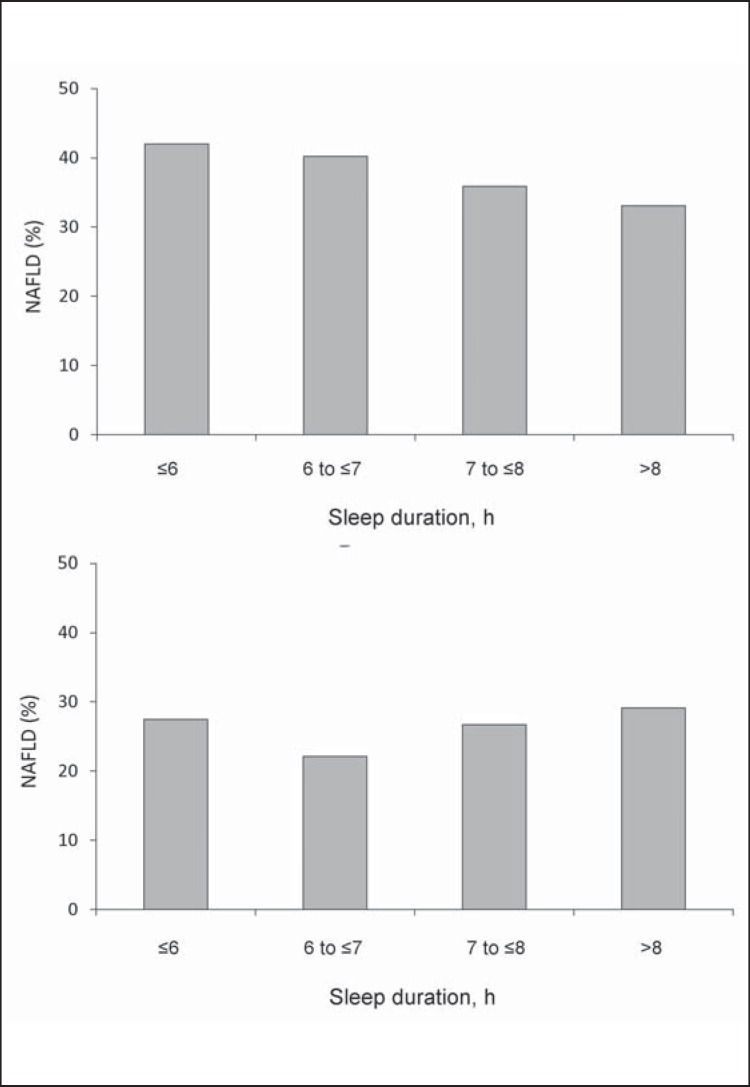
The Proportions of NAFLD According to Sleep Duration and Gender (Tables 2, 3, Fig. 1)
Table 2.
Characteristics of men and women according to sleep duration a
| total | Sleep duration, h |
p value | ||||
|---|---|---|---|---|---|---|
| >8 | 7 to ≤8 | 6 to ≤7 | ≤6 | |||
| Men | ||||||
| Number | 731 | 124 | 229 | 259 | 119 | – |
| Age, years* | 61.5 ± 13.7 | 71.5 ± 10.5 | 64.1 ± 12.1 | 58.6 ± 12.8 | 52.1 ± 13.1 | <0.001 |
| BMI, kg/m2 * | 23.5 ± 3.2 | 22.9 ± 3.2 | 23.3 ± 3.2 | 23.8 ± 3.0 | 23.7 ± 3.7 | 0.043 |
| BMI ≤25 to <30 kg/m2, % | 24.9 | 21.8 | 21.8 | 28.2 | 26.9 | 0.315 |
| BMI ≤ 30 kg/m2, % | 3.6 | 3.2 | 2.6 | 3.5 | 5.9 | 0.474 |
| Current smoker, % | 21.2 | 14.5 | 17.5 | 22.8 | 31.9 | 0.003 |
| Regular exercise, % | 54.4 | 55.6 | 59.0 | 54.1 | 45.4 | 0.116 |
| Sleep apnea, % | 19.2 | 18.5 | 18.3 | 21.2 | 16.8 | 0.670 |
| Poor sleep, % | 30.8 | 22.6 | 25.8 | 32.4 | 45.4 | <0.001 |
| Diabetes, % | 10.1 | 19.4 | 9.2 | 9.3 | 4.2 | <0.001 |
| Fatty liver, % | 38.0 | 33.1 | 36.2 | 40.2 | 42.0 | 0.406 |
| AST, U/l** | 21 (10–93) | 23 (10–89) | 22 (10–65) | 21 (12–93) | 20 (11–75) | 0.068 |
| ALT, U/l** | 20 (6–127) | 19 (9–123) | 20 (6–114) | 21 (9–123) | 21 (8–127) | 0.028 |
| γ-GTP, U/l** | 27 (7–380) | 27 (9–183) | 27 (7–444) | 27 (8–380) | 27 (11–252) | 0.331 |
| ALP, U/l** | 205 (74–760) | 216 (94–557) | 206 (74–474) | 203 (74–440) | 199 (116–760) | 0.524 |
| Triglyceride, mg/dl** | 93 (31–567) | 90 (31–345) | 94 (31–491) | 95 (33–546) | 91 (32–567) | 0.679 |
| LDL-C, mg/dl** | 118 (48–232) | 114 (58–214) | 115 (56–223) | 121 (48–232) | 118 (60–194) | 0.012 |
| HDL-C, mg/dl** | 51 (28–104) | 49 (28–92) | 52 (30–88) | 51 (29–103) | 50 (32–104) | 0.009 |
|
| ||||||
| Women | ||||||
| Number | 1,441 | 127 | 376 | 587 | 351 | |
| Age, years* | 60.6 ± 12.2 | 69.7 ± 10.4 | 64.1 ± 11.5 | 59.7 ± 11.8 | 55.3 ± 11.1 | <0.001 |
| BMI, kg/m2 * | 22.5 ± 3.3 | 22.5 ± 2.8 | 22.4 ± 3.1 | 22.4 ± 3.4 | 22.7 ± 3.5 | 0.448 |
| BMI ≤25 to <30 kg/m2, % | 17.2 | 17.3 | 16.5 | 15.0 | 21.7 | 0.079 |
| BMI ≤ 30 kg/m2, % | 2.5 | 0.8 | 2.4 | 2.7 | 2.8 | 0.605 |
| Current smoker, % | 5.6 | 4.7 | 3.5 | 5.8 | 8.0 | 0.064 |
| Regular exercise, % | 48.2 | 49.6 | 52.9 | 47.0 | 44.4 | 0.131 |
| Sleep apnea, % | 3.7 | 0.8 | 4.3 | 3.9 | 3.7 | 0.330 |
| Poor sleep, % | 36.6 | 26.0 | 28.2 | 35.3 | 51.6 | <0.001 |
| Diabetes, % | 4.6 | 7.9 | 7.2 | 4.1 | 3.4 | 0.149 |
| Fatty liver, % | 25.3 | 29.1 | 26.7 | 22.1 | 27.6 | 0.062 |
| AST, U/l** | 20 (9–168) | 20 (8–48) | 20 (8–58) | 19 (8–73) | 19 (9–168) | 0.014 |
| ALT, U/l** | 16 (4–202) | 15 (7–71) | 16 (6–83) | 16 (4–122) | 16 (6–202) | 0.577 |
| γ-GTP, U/l** | 17 (7–180) | 18 (9–73) | 18 (7–148) | 16 (8–180) | 17 (7–137) | 0.080 |
| ALP, U/l** | 206 (79–722) | 215 (105–368) | 215 (82–468) | 205 (79–655) | 195 (85–722) | 0.002 |
| Triglyceride, mg/dl** | 81 (20–380) | 102 (30–240) | 84 (26–314) | 77 (20–380) | 76 (22–328) | <0.001 |
| LDL-C, mg/dl** | 125 (37–248) | 130 (62–211) | 127 (44–228) | 123 (61–226) | 122 (37–248) | 0.117 |
| HDL-C, mg/dl** | 61 (28–123) | 57 (30–104) | 60 (32–114) | 62 (28–123) | 63 (28–115) | <0.001 |
AST = Asparate aminotransferase; ALT = alanine aminotransferase; γ-GTP = gamma-glutamyl transpeptidaseM; ALP = alkaline phosphatase; LDL-C = low-density lipoprotein cholesterol; HDL-C = high-density lipoprotein cholesterol.
The four sleep duration groups were compared using the χ2 test and the Kruskal-Wallis test.
Data means (± standard deviation).
Medians (range).
Table 3.
Association between sleep duration and the risk for fatty liver a
| Sleep duration, h | Person | Prevalent case | Age-adjusted OR (95% CI) | p value | Multivariate OR (95% CI) |
|||
|---|---|---|---|---|---|---|---|---|
| model 1 | p value | model 2 | p value | |||||
| Men | ||||||||
| >8 | 124 | 41 | 0.89 (0.55–1.44) | 0.640 | 0.88 (0.54–1.43) | 0.608 | 1.14 (0.64–2.02) | 0.666 |
| 7 to ≤8 | 229 | 83 | 0.91 (0.62–1.32) | 0.604 | 0.92 (0.63–1.34) | 0.657 | 1.09 (0.69–1.71) | 0.707 |
| 6 to ≤7 | 259 | 104 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |||
| ≤6 | 119 | 50 | 0.98 (0.62–1.54) | 0.927 | 1.02 (0.64–1.60) | 0.950 | 1.18 (0.67–2.08) | 0.572 |
|
| ||||||||
| Women | ||||||||
| >8 | 127 | 37 | 1.23 (0.79–1.92) | 0.360 | 1.19 (0.75–1.88) | 0.461 | 1.39 (0.82–2.35) | 0.217 |
| 7 to ≤8 | 376 | 101 | 1.20 (0.88–1.62) | 0.252 | 1.20 (0.89–1.63) | 0.256 | 1.36 (0.94–1.96) | 0.101 |
| 6 to ≤7 | 587 | 130 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |||
| ≤6 | 351 | 97 | 1.44 (1.06–1.96) | 0.020 | 1.43 (1.04–1.97) | 0.027 | 1.38 (0.95–2.01) | 0.095 |
The age-adjusted ORs for NAFLD were compared by logistic regression with the group with sleep duration. Model 1: adjusted for age, smoking status, no breakfast, snacking, and regular exercise. Model 2: model 1 plus adjustment for BMI.
Fig. 1.
Proportion of A men and B women with NAFLD according to sleep duration.
The proportion of NAFLD tended to decrease as sleep duration increased in men. The proportion with NAFLD was lowest in the group with a sleep duration of 6 to ≤7 h and highest in the groups with sleep durations of ≤6 h and >8 h in women. The distribution showed a U-shaped curve. However, a significant association was not demonstrated between sleep duration and the proportion of subjects with NAFLD in either men (p = 0.406) or women (p = 0.062). The proportion of subjects with sleep apnea was higher in subjects with NAFLD than without NAFLD in both men (25.5 vs. 15.2%; p < 0.001) and women (7.7 vs. 2.3%; p < 0.001); however, the proportions of subjects with sleep apnea did not differ in subjects with or without poor sleep in both men (22.2 vs. 17.6%; p = 0.105) and women (4.6 vs 3.2%; p = 0.180) (data not shown). The proportion of subjects with poor sleep significantly increased as sleep duration decreased in both men (p < 0.001) and women (p < 0.001).
Association between Sleep Duration and Risk of NAFLD (Table 3)
Compared with subjects with a sleep duration of 6 to ≤7 h, the age-adjusted OR (95% CI) of subjects with a sleep duration ≤6 h was significantly higher for subjects with NAFLD (1.44 (1.06-1.96)) in women. No significant differences were seen in men. After adjustment for behavior factors (smoking, no breakfast, snacking, regular exercise), the adjusted OR (95% CI) for women with NAFLD with a sleep duration ≤6 h compared to the reference (6 to ≤7 h) was 1.43 (1.04-1.97). After further adjustment for BMI, this association was not significant. In subjects without sleep apnea, after adjusting for confounding factors (age, smoking status, no breakfast, snacking, and regular exercise), the adjusted OR for NAFLD when comparing women with a sleep duration ≤6 h to the reference (6 to ≤7 h) was 1.37 (1.00-1.88; p = 0.052) (data not shown).
Associations between Lifestyle and Sleep Duration (Table 4)
Table 4.
Age-adjusted odds ratios of lifestyle factors in relation to sleep duration a
| Sleep duration, h |
||||
|---|---|---|---|---|
| >8 | 7 to ≤8 | 6 to ≤7 | ≤6 | |
| Men | ||||
| Smoking | 1.02 (0.55–1.91) | 0.93 (0.59–1.49) | 1.00 (reference) | 1.19 (0.72–1.98) |
| Regular exercise | 0.78 (0.49–1.24) | 1.10 (0.76–1.59) | 1.00 (reference) | 0.82 (0.52–1.29) |
| No breakfast | 0.77 (0.30–1.99) | 0.65 (0.34–1.27) | 1.00 (reference) | 0.92 (0.48–1.76) |
| Snacking | 0.96 (0.45–2.05) | 0.74 (0.41–1.32) | 1.00 (reference) | 1.37 (0.77–2.43) |
|
| ||||
| Women | ||||
| Smoking | 1.08 (0.40–2.89) | 0.74 (0.39–1.40) | 1.00 (reference) | 1.24 (0.74–2.07) |
| Regular exercise | 0.84 (0.55–1.26) | 1.09 (0.83–1.43) | 1.00 (reference) | 1.04 (0.79–1.38) |
| No breakfast | 0.69 (0.30–1.56) | 0.58 (0.35–0.96)* | 1.00 (reference) | 1.53 (1.05–2.23)* |
| Snacking | 0.91 (0.31–2.68) | 0.94 (0.51–1.73) | 1.00 (reference) | 1.55 (0.94–2.56) |
The age-adjusted ORs for lifestyle factors were compared by logistic regression with the group with sleep duration.
Significant differences (p < 0.05).
Sleep duration affects multiple behaviors. Thus, we evaluated several lifestyle factors (regular exercise, eating habits such as no breakfast and snacking) and sleep duration. Compared with subjects with a sleep duration of 6 to ≤7 h, the age-adjusted OR for subjects with a sleep duration ≤6 h was significantly higher for those who did not eat breakfast (1.53 (1.05-2.23)), whereas that of subjects with a sleep duration >7 to ≤8 h was significantly lower for those who did not eat breakfast (0.58 (0.35-0.96)).
Discussion
NAFLD is a hepatic form of metabolic syndrome; thus, obesity and insulin resistance are strongly associated with onset of NAFLD or nonalcoholic steatohepatitis [15,16]. In addition, short sleep duration has been reported to be a risk factor for diabetes mellitus and obesity [2,3]. The association between fatty liver and short sleep duration was first reported in Japanese men [9]. However, that study did not control for alcohol consumption, which affects fatty liver and sleep duration. Recently, a large-scale study reported that short sleep duration and poor sleep quality were risk factors for NAFLD in a middle-aged Korean general population [8].
In the current study, we confirmed the short sleep duration tends to be associated with NAFLD in women. Moreover, the proportion of NAFLD in women showed a U-shaped curve. This shape is commonly seen with other metabolic disorders such as dyslipidemia or diabetes mellitus [3,7]. These results coincide with a mega-study of middle-aged Korean females [8].
Insomnia and sleep duration are influenced by many factors such as sex, health, sociodemographic factors, environmental factors, and their combination [17,18]. Moreover, sleep duration is different in different age groups. One study showed that sleep duration was shortest in a Japanese general population aged 45-49 years [19]. Therefore, the association between sleep duration and NAFLD needs to be evaluated in subjects with a wide age range. This study is the first study that assessed the association of short sleep duration with NAFLD in women aged 23-95 years.
Lifestyle is an important factor for metabolic syndrome and is associated with NAFLD. In the present study, we confirmed that short sleep duration could be an independent risk factor for NAFLD in women after adjusting for lifestyle factors. In addition, short sleep duration in the present study was also an independent risk factor for unhealthy eating habits, such as skipping breakfast.
Previous studies reported that skipping breakfast is associated with obesity [20,21]. Thus, short sleep duration induces unhealthy eating habits and might affect NAFLD onset indirectly in women, although we could not confirm the association between skipping breakfast and NAFLD (data not shown).
Although the precise mechanism of sleep duration in NAFLD onset remains unknown, some potential explanations are proposed. It has been shown that short sleep duration and poor sleep quality can impair insulin signaling and glucose tolerance [22,23]. Moreover, short sleep duration and poor sleep quality may induce the development of insulin resistance and subclinical inflammation in women [24]. Sleep disturbances induce inflammatory cytokines such as tumor necrosis factor-alpha and interleukin-6, which are associated with progression of NAFLD [25]. Chronic sleep restriction alters the hormonal balance of leptin and ghrelin, which regulate appetite [26]. However, the effect of short sleep duration on NAFLD in men is controversial. Recently, a study reported that short sleep duration reduces the risk of NAFLD onset in Japanese men [27]. In the present study, there was no significant association between sleep duration and NAFLD in men. Further studies are needed to assess the pathophysiology of NAFLD as well as to determine the impact of gender differences.
The present study has several limitations. First, this study was based on an analysis of questionnaire results; thus, it was difficult to perform a detailed analysis of behavioral factors and quality of sleep. In particular, sleep quality should be evaluated by the Pittsburgh Sleep Quality Index, a standardized self-administered questionnaire that is widely used to evaluate subjective sleep quality [28]. Second, the present study included SAS, an important risk factor for NAFLD [11]. Apart from a confirmed diagnosis of SAS, we confirmed the proportion of sleep apnea to be higher in subjects with NAFLD than without NAFLD in this study. However, sleep apnea was not significantly associated with poor sleep, and the proportion was only 7.7% in women with NAFLD. Third, this study did not evaluate mental status, which affects behavior. Previous studies reported that depression is higher in patients with NAFLD [29] and associated with the histological severity of NAFLD [30]. This study was performed in subjects who underwent health check-ups from June 2012 to May 2013 at Watari Hospital Health Center in Fukushima, Japan. Thus, most subjects experienced the Great East Japan Earthquake and the Fukushima Daiichi Nuclear power plant accident. As a consequence, study subjects may have been affected directly or indirectly by mental stress after this disaster. Depression and insomnia affect each other [17,31]; thus, an evaluation of mental status in addition to sleep duration is necessary in the future.
In conclusion, short sleep duration tends to be associated with NAFLD in women and may be mediated by body adiposity. Appropriate sleep duration should be taken into account in the comprehensive strategies for prevention and treatment of NAFLD, particularly in women.
Disclosure Statement
The authors report no conflicts of interest.
Acknowledgements
The authors thank the staff members of the health check-up division at Watari Hospital.
References
- 1.Kim K, Uchiyama M, Okawa M, Liu X, Ogihara R. An epidemiological study of insomnia among the Japanese general population. Sleep. 2000;23:41–47. [PubMed] [Google Scholar]
- 2.Vorona RD, Winn MP, Babineau TW, Eng BP, Feldman HR, Ware JC. Overweight and obese patients in a primary care population report less sleep than patients with a normal body mass index. Arch Intern Med. 2005;165:25–30. doi: 10.1001/archinte.165.1.25. [DOI] [PubMed] [Google Scholar]
- 3.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33:414–420. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG, Rundle AG, Zammit GK, Malaspina D. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47:833–839. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 5.Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32:1484–1492. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 6.Holliday EG, Magee CA, Kritharides L, Banks E, Attia J. Short sleep duration is associated with risk of future diabetes but not cardiovascular disease: a prospective study and meta-analysis. PLoS One. 2013;8:e82305. doi: 10.1371/journal.pone.0082305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaneita Y, Uchiyama M, Yoshiike N, Ohida T. Associations of usual sleep duration with serum lipid and lipoprotein levels. Sleep. 2008;31:645–652. doi: 10.1093/sleep/31.5.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim CW, Yun KE, Jung HS, Chang Y, Choi ES, Kwon MJ, et al. Sleep duration and quality in relation to non-alcoholic fatty liver disease in middle-aged workers and their spouses. J Hepatol. 2013;59:351–357. doi: 10.1016/j.jhep.2013.03.035. [DOI] [PubMed] [Google Scholar]
- 9.Hsieh SD, Muto T, Murase T, Tsuji H, Arase Y. Association of short sleep duration with obesity, diabetes, fatty liver and behavioral factors in Japanese men. Intern Med. 2011;50:2499–2502. doi: 10.2169/internalmedicine.50.5844. [DOI] [PubMed] [Google Scholar]
- 10.Musso G, Cassader M, Olivetti C, Rosina F, Carbone G, Gambino R. Association of obstructive sleep apnoea with the presence and severity of non-alcoholic fatty liver disease. A systematic review and meta-analysis. Obes Rev. 2013;14:417–431. doi: 10.1111/obr.12020. [DOI] [PubMed] [Google Scholar]
- 11.Kayukawa Y, Okada T. Prevalence of obstructive sleep apnea syndrome (in Japanese). Chiryogaku. 1996;30:179–182. [Google Scholar]
- 12.Eguchi Y, Hyogo H, Ono M, Mizuta T, Ono N, Fujimoto K, Chayama K, Saibara T, JSG-NAFLD Prevalence and associated metabolic factors of nonalcoholic fatty liver disease in the general population from 2009 to 2010 in Japan: a multicenter large retrospective study. J Gastroenterol. 2012;47:586–595. doi: 10.1007/s00535-012-0533-z. [DOI] [PubMed] [Google Scholar]
- 13.Whalan DJ. The ethics and morality of clinical trials in man. Med J Aust. 1975;1:491–494. [PubMed] [Google Scholar]
- 14.World Medical Association declaration of Helsinki Recommendations guiding physicians in biomedical research involving human subjects. JAMA. 1997;277:925–926. [PubMed] [Google Scholar]
- 15.Koda M, Kawakami M, Murawaki Y, Senda M. The impact of visceral fat in nonalcoholic fatty liver disease: cross-sectional and longitudinal studies. J Gastroenterol. 2007;42:897–903. doi: 10.1007/s00535-007-2107-z. [DOI] [PubMed] [Google Scholar]
- 16.El-Serag HB, Tran T, Everhart JE. Diabetes increases the risk of chronic liver disease and hepatocellular carcinoma. Gastroenterology. 2004;126:460–468. doi: 10.1053/j.gastro.2003.10.065. [DOI] [PubMed] [Google Scholar]
- 17.American Academy of Sleep Medicine . The International Classification of Sleep Disorders, 2nd ed (ICD-2): Diagnostic and Coding Manual. Westchester: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 18.Ohida T, Kamal AM, Uchiyama M, Kim K, Takemura S, Sone T, Ishii T. The influence of lifestyle and health status factors on sleep loss among the Japanese general population. Sleep. 2001;24:333–338. doi: 10.1093/sleep/24.3.333. [DOI] [PubMed] [Google Scholar]
- 19. Ministry of Internal Affairs and Communications Social Life Basic Survey 2011 (in Japanese) www.stat.go.jp/data/shakai/2011/ (last accessed June 19, 2015).
- 20.Horikawa C, Kodama S, Yachi Y, Heianza Y, Hirasawa R, Ibe Y, Saito K, Shimano H, Yamada N, Sone H. Skipping breakfast and prevalence of overweight and obesity in Asian and Pacific regions: a meta-analysis. Prev Med. 2011;53:260–267. doi: 10.1016/j.ypmed.2011.08.030. [DOI] [PubMed] [Google Scholar]
- 21.Huang CJ, Hu HT, Fan YC, Liao YM, Tsai PS. Associations of breakfast skipping with obesity and health-related quality of life: evidence from a national survey in Taiwan. Int J Obes (Lond) 2010;34:720–725. doi: 10.1038/ijo.2009.285. [DOI] [PubMed] [Google Scholar]
- 22.Byberg S, Hansen AL, Christensen DL, Vistisen D, Aadahl M, Linneberg A, Witte DR. Sleep duration and sleep quality are associated differently with alterations of glucose homeostasis. Diabet Med. 2012;29:e354–360. doi: 10.1111/j.1464-5491.2012.03711.x. [DOI] [PubMed] [Google Scholar]
- 23.Rafalson L, Donahue RP, Stranges S, Lamonte MJ, Dmochowski J, Dorn J, Trevisan M. Short sleep duration is associated with the development of impaired fasting glucose: the Western New York Health Study. Ann Epidemiol. 2010;20:883–889. doi: 10.1016/j.annepidem.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu R, Zee PC, Chervin RD, Arguelles LM, Birne J, Zhang S, Christoffel KK, Brickman WJ, Zimmerman D, Wang B, Wang G, Xu X, Wang X. Short sleep duration is associated with insulin resistance independent of adiposity in Chinese adult twins. Sleep Med. 2011;12:914–919. doi: 10.1016/j.sleep.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prather AA, Marsland AL, Hall M, Neumann SA, Muldoon MF, Manuck SB. Normative variation in self-reported sleep quality and sleep debt is associated with stimulated pro-inflammatory cytokine production. Biol Psychol. 2009;82:12–17. doi: 10.1016/j.biopsycho.2009.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Magee CA, Huang XF, Iverson DC, Caputi P. Examining the pathways linking chronic sleep restriction to obesity. J Obes. 2010;2010:821710. doi: 10.1155/2010/821710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miyake T, Kumagi T, Furukawa S, Hirooka M, Kawasaki K, Koizumi M, Todo Y, Yamamoto S, Tokumoto Y, Ikeda Y, Abe M, Kitai K, Matsuura B, Hiasa Y. Short sleep duration reduces the risk of nonalcoholic fatty liver disease onset in men: a community-based longitudinal cohort study. J Gastroenterol. 2015;50:583–589. doi: 10.1007/s00535-014-0989-0. [DOI] [PubMed] [Google Scholar]
- 28.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 29.Elwing JE, Lustman PJ, Wang HL, Clouse RE. Depression, anxiety, and nonalcoholic steatohepatitis. Psychosom Med. 2006;68:563–569. doi: 10.1097/01.psy.0000221276.17823.df. [DOI] [PubMed] [Google Scholar]
- 30.Youssef NA, Abdelmalek MF, Binks M, Guy CD, Omenetti A, Smith AD, Diehl AM, Suzuki A. Associations of depression, anxiety and antidepressants with histological severity of nonalcoholic fatty liver disease. Liver Int. 2013;33:1062–1070. doi: 10.1111/liv.12165. [DOI] [PubMed] [Google Scholar]
- 31.Kaneita Y, Ohida T, Uchiyama M, Takemura S, Kawahara K, Yokoyama E, Miyake T, Harano S, Suzuki K, Fujita T. The relationship between depression and sleep disturbances: a Japanese nationwide general population survey. J Clin Psychiatry. 2006;67:196–203. doi: 10.4088/jcp.v67n0204. [DOI] [PubMed] [Google Scholar]