Abstract
Objective
The question of whether breastfeeding has a protective effect against the development of overweight or obesity later in life remains controversial, especially during adolescence. The objective was to assess the relationship between breastfeeding and adolescents’ body composition.
Methods
The HELENA study is a cross-sectional study involving 3,528 adolescents from 10 European cities. The outcome measures were body weight and height, subscapular skinfolds as well as waist circumferences. Breastfeeding, smoking status, and parental socioeconomic status were assessed by self-administered questionnaires. Dietary intake was recorded using two 24-hour recall surveys. Two adjustment approaches were used: i) covariance analysis adjusted for confounding factors (propensity score adjustment) and ii) multivariate quantile regression.
Results
After adjustment, no significant associations were observed between breastfeeding and body composition parameters (BMI Z-score; sum of skinfolds; waist-to-height ratio). An adjusted quantile regression analysis showed a non-significant trend for a protective effect of breastfeeding toward the highest percentiles of adiposity in boys but not in girls. This is of particular interest with respect to the superiority of the waist-to-height ratio over waist circumference and BMI for detecting cardiometabolic risk factors.
Conclusion
This first European study, including a large set of factors influencing adolescents’ body composition, showed a non-significant trend toward a protective effect of breastfeeding on highest percentiles of adolescent's abdominal adiposity.
Key Words: Breastfeeding, Body composition, Adolescents, Waist-to-height ratio, BMI, Propensity score
Introduction
Breastfeeding is the recommended mode of infant feeding [1] and has several advantages compared with formula feeding, the most of which important is a lower risk of infectious diseases. Breastfeeding is also thought to be associated with a lower risk of developing obesity in childhood and adolescence. This last point is still a matter of debate [2,3,4].
Breastfeeding was first suggested to influence body composition in 1980 by Marmot et al. [5]. Since then, several meta-analyses have been published on this topic [6,7,8]. The last two published meta-analyses have shown a beneficial effect of breastfeeding on body composition, The first one was limited to children aged less than 1 year [9], and the other one, conducted for the World Health Organization (WHO) without age limitation, found a protective effect of breastfeeding but results were attenuated by a clear evidence of publication biases [2].
Adolescence is a key period for nutritional issues. It has been shown that the likelihood of becoming obese as an adult is greater for obese adolescents; the odds ratio of being obese in adulthood is 16 for the highest BMI [10]. BMI is the most common way to assess body composition in clinical practice and in many studies, but is only an estimate of adiposity. The relationship between breastfeeding and body composition should be explored with better accuracy by analyzing subcutaneous and abdominal adiposity [11,12].
Our analysis is based on the Healthy Lifestyle in Europe by Nutrition in Adolescence (HELENA) study. This is a European multicenter and cross-sectional study that aims to investigate the nutritional status and lifestyle of European adolescents [13]. 3,910 adolescents were recruited for anthropometric measurements and questionnaires about their way of life. Collected data for analysis of the effect of breastfeeding on body composition included data about breastfeeding as well as many confounding factors to take in consideration.
As previous publications were discordant, due to power weakness and/or to adjustment inadequacy, the objective of the present study was to assess the relationship between breastfeeding and adiposity in a large population of adolescents taking into account a large set of confounding factors.
Material and Methods
Design
Data derived from the HELENA-Cross Sectional Study (CSS), a multicenter study aiming to obtain reliable and comparable data on nutrition and health-related parameters. A total of 3,528 adolescents (age range 12.5-17.5 years) were assessed at school between 2006 and 2007 in 10 European cities from 9 countries, all fulfilling the general HELENA-CSS inclusion criteria [13]. Details on sampling procedures and study design have been reported elsewhere [14]. The ethical committee of each clinic involved approved the study [15]. Written informed consent was obtained from both adolescents and their parents.
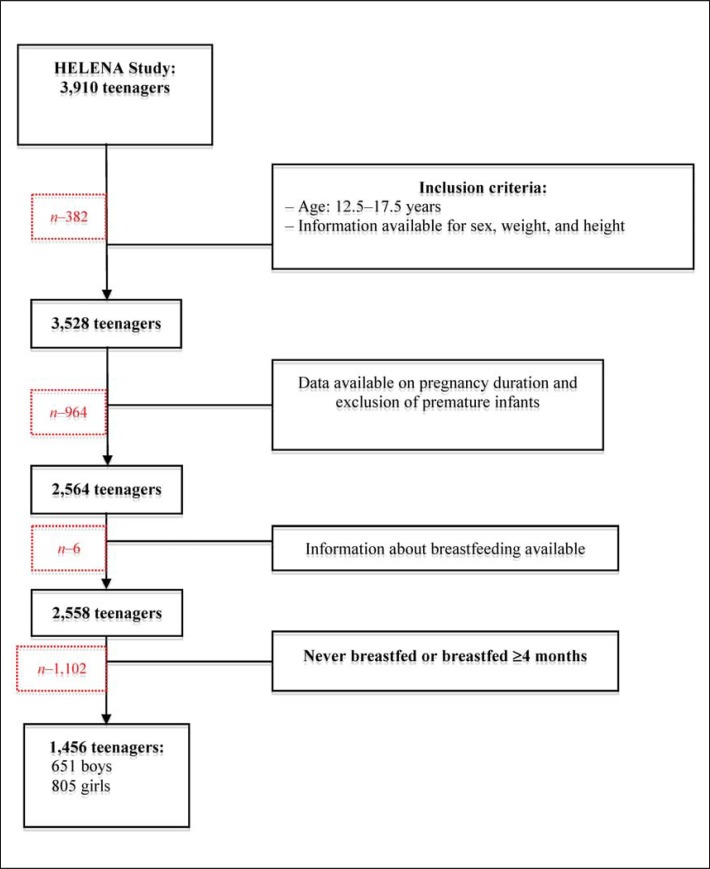
Information about breastfeeding was available for 2,848 adolescents from a specific parental questionnaire. In our analysis, we included adolescents who were not born prematurely (<35 weeks gestation), for whom we had data on pregnancy duration (n = 2,564), and who were either never breastfed (n = 440) or breastfed for ≥4 months (n = 1,016) (fig. 1). In order to raise the capability to assess the role of breastfeeding we excluded subjects who were breastfed for less than 4 months as this is a heterogeneous category including very short times of breastfeeding. The group excluded is not different considering sex ratio, age, or socioeconomic status (SES).
Fig. 1.
Selection of the population studied.
Anthropometric Data
The following anthropometric parameters were measured: i) Height (Seca225; precision 1 mm; Seca GmbH & Co, Hamburg, Germany) and weight (electronic scale: Seca861; precision 0.05 kg; Seca GmbH & Co); ii) skinfolds: biceps, triceps, subscapular, suprailiac, calf, and hip (in triplicate on the left side of the body using Holtain calipers; precision 0.2 mm; Holtain Ltd., Crymych, UK); and iii) waist circumference (in triplicate with a nonelastic tape; Seca200, precision 0.1 cm; Seca GmbH & Co). These measures were obtained under standardized conditions [16]. BMI and waist-to height ratio were calculated. Sexual maturation was assessed by a medical doctor using the method of Tanner and Whitehouse [17].
SES
The SES of the adolescents was assessed using the Family Affluence Scale (FAS III) [18]. The FAS III records items, such as ‘having his/her own bedroom’, ‘number of cars’ and ‘number of computers’, and produces a score from 0 to 6 points where 0 is the lowest grade and 6 is the highest. The SES was also evaluated according to the parents’ educational level as elementary school / high school / college degree / engineering or university degree; subjective family affluence (very well off, quite well off, average well off, not very well off, not very well off at all) [19]; and the International Standard Classification of Occupations (ISCO) category of the father's occupation, which was classified into one of four categories. The evaluation of SES has been described in detail previously [19].
Neonatal Information
Characteristics of breastfeeding and its duration were collected from parents using a specific questionnaire. All countries participating in the HELENA study used a health booklet that referred to the type of infant feeding and its duration. The other neonatal data collected were weight, length at birth, and gestational age.
Physical Fitness
Several physical fitness parameters were measured: cardiorespiratory fitness (20 m shuttle run); muscular speed, agility, and coordination (4 4 10 m shuttle run); muscular strength (hand grip); lower limb explosive strength and coordination (squat jump, Abalakov jump, countermovement jump); flexibility (back saver sit and reach); and explosive strength (standing broad jump). These tests have been described in detail previously [20].
Nutritional Intake
The instrument Young Adolescents’ Nutrition Assessment on Computer [21] was adapted for the HELENA study and called HELENA-DIAT [22]. It is a 24-hour recall assessment tool based on six meal occasions referring to the day before the interview. The validity of the instrument has been investigated against food records and interviews, and is described in detail elsewhere [21]. The data were cross-checked with the German BLS database [23] to extract energy and nutrient intake. Underreporters were identified with the Goldberg method [24]. All mean intakes for the 2 nonconsecutive days were calculated by applying the multiple source method using two different strategies: including the underreporters versus excluding the underreporters. For our analysis, we included energy consumed per day (kcal/day) and fat consumed per day (g/day).
Reliability
All measurements followed written detailed operating procedures translated into the local language to ensure that the same verbal information was given to all participants in the HELENA study.
Two workshops were conducted in which all field workers in charge of measurements were trained in the methods to obtain the anthropometric measurements in each of the 10 centers. A pilot study involving 202 adolescents from the 10 centers was also performed to check for inaccuracy and to adapt the procedure and questionnaires before the study began. Socioeconomic and parental questionnaire items that caused problems or raised questions as well as those completed by <85% of the adolescents were reviewed for deletion or modification [19,25].
Because anthropometric and fitness measurements are sensitive to interobserver variability, reliability was tested [25,26]. For skinfolds and circumference, the interobserver reliability was tested and was always >90%. The reliability of physical fitness tests was acceptable; no learning or fatigue effects were found for any of the physical fitness tests when repeated.
Ethical Considerations
This study was conducted according to the guidelines laid down in the Declaration of Helsinki in its revised version, and all procedures involving human subjects were approved by the ethics committee in each participating country. Written informed consent was obtained from all subjects and their parents [15].
Variable Selection
Several body composition variables were selected a priori: BMI Z-score (following the Cole calculation [27]), sum of six skinfolds (log-transformed) to investigate subcutaneous adiposity (biceps, triceps, subscapular, suprailiac, thigh, calf), and waist-to-height ratio to explore abdominal adiposity [28,29,30,31].
Confounders that could influence body composition were selected: adolescents’ smoking habit (dichotomized as ≤10 cigarettes/week and >10 cigarettes/week), age, all fitness data as continuous variables, sedentary lifestyle (time spent watching TV and playing videogames during school days and sleep duration on weeknights), mother's and father's body composition (assessed as obese/overweight, normal, underweight according to adolescents’ perception), study center, puberty (Tanner staging), SES, parental educational level (elementary school / high school / college degree / engineering or university degree), energy, and fat intake.
Statistical Analysis
Numeric variables are expressed as mean and standard deviation (SD), and qualitative variables as frequency and percentage. Because the distribution of the sum of six skinfolds was skewed, all analyzes involving the sum of six skinfolds were performed after log-transformation (natural logarithm). Continuous and qualitative variables were analyzed by Student's t test or χ2 test, respectively.
Body composition variables were studied for the whole population and then for boys and girls separately.
Each body composition variable (BMI Z-score, waist-to-height ratio, log-transformation of the sum of skinfolds) was examined as follows. The potential confounding variables were analyzed successively by bivariate analysis. The binary and nominal variables were tested with Student's t test and analysis of variance (ANOVA), respectively. Continuous and ordinal variables were tested with Pearson's and Spearman's correlation, respectively.
The adjustment for confounders was performed using the propensity score method. This method is a two-step procedure. In the first step, logistic regression was performed with breastfeeding as the dependent variable and the confounders as independent variables. In the second step, the effect of breastfeeding on each body composition parameter was adjusted for the propensity score using covariance analysis. The selected confounders were related both with breastfeeding and with the outcome [32]; propensity score method provides better results than multivariable linear regression for adjustment on confounders (it is less concerned by the problem of overadjustment). Co-linearity was pursued with exclusion of each variable with variance inflation factor ≥3. Finally, a quantile regression [33] was performed to integrate the propensity score to adjust for confounding factors related to breastfeeding.
Data were analyzed using Statistical Analysis Systems statistical software, version 9.1 (SAS Institute, Cary, NC, USA). p < 0.05 was considered significant.
Results
The mean age of participating adolescents was 14.7 ± 1.2 years and was the same in each sex group (males 14.7 ± 1.2, females 14.7 ± 1.2 years). Compared with adolescents who were never breastfed (table 1), the breastfed group had lower BMI for the whole group and for boys but not for girls. The same pattern was observed for the sum of skinfolds and the waist-to-height ratio.
Table 1.
Effect of breastfeeding on body composition variables in the bivariate analysis
| Relationship with breastfeeding (never vs. ≥4 months) | Boys (n = 651) |
p Value | Girls (n = 805) |
p Value | Total population (n = 1,456) |
p Value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| breastfed |
not breastfed |
breastfed |
not breastfed |
breastfed |
not breastfed |
||||||||||
| mean | SD | mean | SD | mean | SD | mean | SD | mean | SD | mean | SD | ||||
| BMI Z score | 0.48 | 1.11 | 0.70 | 1.21 | 0.027 | 0.32 | 1.07 | 0.41 | 1.19 | 0.32 | 0.4 | 1.04 | 0.53 | 1.20 | 0.04 |
| Skinfolds | 4.13 | 0.44 | 4.24 | 0.45 | 0.04 | 4.5549 | 0.34 | 4.58 | 0.36 | 0.44 | 4.38 | 0.43 | 4.46 | 0.43 | 0.001 |
| WHR | 0.43 | 0.05 | 0.45 | 0.06 | 0.001 | 0.4312 | 0.05 | 0.44 | 0.05 | 0.13 | 0.43 | 0.05 | 0.44 | 0.05 | <0.001 |
The bivariate analysis between the outcomes and confounding factors identified factors with a significance level <0.2 that were introduced in the propensity score for the adjusted analysis (table 2).
Table 2.
Significance of bivariate associations with body composition
| BMI-Z score (p value) |
Sum of six skinfolds (p value) |
Waist-to-height ratio (p value) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| boy | girls | total | boys | girls | total | boys | girls | total | |
| Smoking | 0.8* | 0.01* | 0.1* | 0.04* | 0.24* | 0.38* | 0.66* | 0.07* | 0.01* |
| Sex | - | - | <0.001* | - | - | <0.001* | - | - | 0.08* |
| Center | <0.001** | <0.001** | <0.001** | <0.001** | <0.001** | <0.001** | <0.001** | <0.001** | <0.001** |
| ISCO (father) | 0.27** | <0.001** | <0.001** | 0.11** | 0.001** | <0.001** | 0.03** | <0.001** | <0.001** |
| Pubertal status | 0.002 # | <0.001 # | <0.001 # | 0.02 # | <0.001 # | <0.001 # | 0.59 # | <0.001 # | <0.001 # |
| Mother's weight | 0.02 # | <0.001 # | <0.001 # | 0.42 # | <0.001 # | <0.001 # | 0.02 # | <0.001 # | <0.001 # |
| Father's weight | 0.02 # | 0.006 # | <0.001 # | 0.28 # | 0.31 # | 0.11 # | 0.06 # | 0.04 # | 0.005 # |
| Perceived affluence | 0.68 # | 0.98 # | 0.95 # | 0.35 # | 0.36 # | 0.29 # | 0.62 # | 0.24 # | 0.22 # |
| Mother's educational level | 0.003 # | <0.001 # | <0.001 # | 0.08 # | 0.002 # | <0.001 # | <0.001 # | <0.001 # | <0.001 # |
| Father's educational level | 0.01 # | <0.001 # | <0.001 # | 0.12 # | <0.001 # | <0.001 # | <0.001 # | <0.001 # | <0.001 # |
| FAS III | 0.001 # | <0.001 # | <0.001 # | 0.01 # | <0.001 # | <0.001 # | 0.002 # | 0.002 # | <0.001 # |
| TV duration | 0.002 # | 0.01 # | <0.001 # | 0.004 # | <0.001 # | <0.001 # | 0.004 # | <0.001 # | <0.001 # |
| Video game duration | <0.001 # | 0.05 # | <0.001 # | <0.001 # | 0.85 # | <0.001 # | <0.001 # | 0.05 # | <0.001 # |
| Age | 0.06 ## | 0.04 ## | 0.006 ## | <0.001 ## | <0.001 ## | 0.1 ## | 0.05 ## | 0.01 ## | 0.77 ## |
| Birth weight | 0.14 ## | 0.06 ## | 0.003 ## | 0.31 ## | 0.2 ## | 0.36 ## | 0.99 ## | 0.27 ## | 0.59 ## |
| Birth length | 0.06 ## | 0.07 ## | 0.001 ## | 0.12 ## | 1. ## | 0.09 ## | 0.52 ## | 0.2 ## | 0.25 ## |
| Sleep duration | 0.98 ## | 0.01 ## | 0.12 ## | 0.03 ## | 0.01 ## | 0.34 ## | 0.01 ## | 0.05 ## | 0.58 ## |
| Standing broad jump | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## |
| 4 × 10 m shuttle run | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## |
| 20 m shuttle run | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## |
| Squat jump | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## |
| Countermovement jump | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## |
| Abalakov jump | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## | <0.001 ## |
| Hand grip | <0.001 ## | <0.001 ## | <0.001 ## | 0.14 ## | 0.004 ## | <0.001 ## | 0.61 ## | 0.002 ## | 0.008 ## |
| Back-saver sit and reach | 0.001 ## | 0.91 ## | 0.87 ## | 0.33 ## | 0.003 ## | <0.001 ## | 0.84 ## | 0.08 ## | 0.1 ## |
| Energy consumption (kcal/day) | 0.07 ## | <0.001 ## | 0.02 ## | <0.001 ## | <0.001 ## | <0.001 ## | 0.013 ## | <0.001 ## | <0.001 ## |
| Fat consumption (g/day) | 0.24 ## | <0.001 ## | 0.04 ## | <0.001 ## | <0.001 ## | <0.001 ## | 0.05 ## | 0.005 ## | 0.002 ## |
ISCO = International Standard Classification of Occupations; FAS = Family Affluence Scale.
Student's t test
ANOVA
Spearman correlation
Pearson correlation.
Multivariate analysis using the propensity score did not show any significant associations between breastfeeding and BMI, fat free mass index (FFMI), skinfold thickness, or waist-to-height ratio (table 3). Multivariate analyzes by sex did not show any significant association.
Table 3.
Effect of breastfeeding on body composition variable in adjusted analysis*
| Relationship with breastfeeding (never vs. ≥4 months] |
Boys
a
|
p Value | Girls b | p Value | Total population c | p Value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| breastfed |
not breastfed |
breastfed |
not breastfed |
breastfed |
not breastfed |
||||||||||
| mean | SE | mean | SE | mean | SE | mean | SE | mean | SE | mean | SE | ||||
| BMI Z score | 0.42 | 0.06 | 0.46 | 0.12 | 0.76 | 0.27 | 0.06 | 0.34 | 0.1 | 0.58 | 0.34 | 0.05 | 0.42 | 0.08 | 0.4 |
| Skinfolds | 4.14 | 0.03 | 4.2131 | 0.06 | 0.3 | 4.54 | 0.02 | 4.57 | 0.03 | 0.46 | 4.36 | 0.02 | 4.4 | 0.03 | 0.26 |
| Waist-to-height ratio | 0.43 | 0.003 | 0.4367 | 0.006 | 0.19 | 0.43 | 0.003 | 0.43 | 0.005 | 0.36 | 0.43 | 0.002 | 0.44 | 0.004 | 0.096 |
For multivariate analysis, propensity score was computed with all variables related to each outcome in the bivariate analysis (p ≤ 0.2].
For each outcome: age, center, FAS III scale, time spent watching TV, time spent playing video games, mother's and father's educational levels, fitness data (20 m shuttle run). For BMI Z score: sexual maturation, neonatal weight and height, perception of paternal and maternal BMI, hand grip, squat jump, 4 × 10 m shuttle run, back-saver sit and reach, kcal/day. For log of six skinfolds: sexual maturation, neonatal height, adolescents' tobacco smoking, time spent sleeping, ISCO of the father, hand grip, squat jump, 4 × 10 m shuttle run. For waist-to-height ratio: time spent sleeping, perception of paternal and maternal BMI, ISCO of the father, squat jump, 4 × 10 m shuttle run.
For each outcome: age, sexual maturation, center, FAS III scale, time spent sleeping, perception of maternal BMI, mother's and father's educational levels, ISCO of the father, fitness data (20 m shuttle run, hand grip, squat jump, 4 × 10 m shuttle run], kcal/day. For BMI Z score: neonatal weight and height, adolescents' tobacco smoking, time spent watching TV, time spent playing video games, perception of paternal BMI. For log of six skinfolds time spent watching TV, back-saver sit and reach. For waist-to-height ratio: neonatal height, time spent watching TV, time spent playing video games, perception of paternal BMI, back-saver sit and reach.
For each outcome: sex, sexual maturation, center, FAS III scale, time spent playing video games, perception of maternal and paternal BMI, mother's and father's educational levels, fitness data (20 m shuttle run, hand grip, squat jump, 4 × 10 m shuttle run] kcal/day. For BMI Z score: adolescents' tobacco smoking, age, neonatal weight and height, time spent sleeping, time spent watching TV, ISCO of the father. For log of six skinfolds: age, neonatal height, time spent watching TV, ISCO of the father, back-saver sit and reach. For waist-to-height ratio: adolescents' tobacco smoking, time spent watching TV, ISCO of the father, back-saver sit and reach.
Quantile regression provided results by percentiles for each outcome. The quantile regression for whole population showed that breastfeeding was not significantly associated with BMI, FFMI, skinfold thickness, or waist-to-height ratio, except for the 90th percentile of waist-to-height ratio in the total population (data not shown).
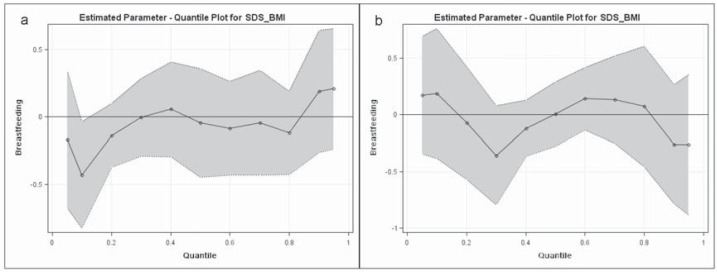
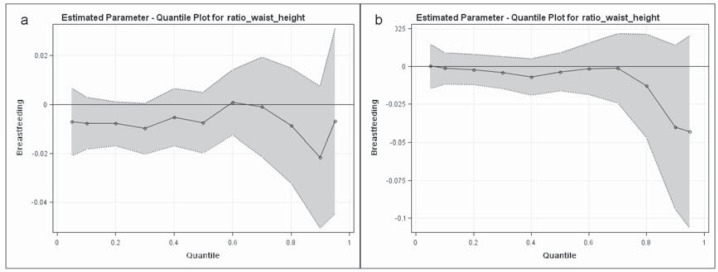
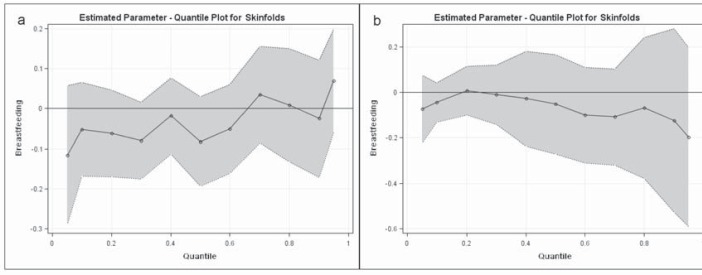
The analysis was performed separately for girls and boys (fig. 2, 3, 4). In girls, breastfeeding was not associated with any of the outcomes. In boys, quantile regression analysis showed a non-significant tendency toward a protective effect of breastfeeding on the highest percentiles of skinfolds and waist-to-height ratio. BMI did not correlate with breastfeeding in any percentile.
Fig. 2.
Quantile repartition of BMI Z score (SDS-BMI). a Girls, b boys. The black points represent the adjusted protective effect of breastfeeding following the values of BMI Z score. A point below zero means that breastfeeding has a lowering effect on the considered BMI Z score. The grey zone represents the confidence interval. Same adjustment as in table 3. SDS-BMI = Standard deviation score for BMI.
Fig. 3.
Quantile repartition of waist-to-height ratio. a Girls, b boys. The black points represent the adjusted protective effect of breastfeeding following the values of waist-to-height ratio. A point below zero means that breastfeeding has a lowering effect on the considered waist-to-height ratio. The grey zone represents the confidence interval. Same adjustment as in table 3.
Fig. 4.
Quantile repartition of sum of skinfolds. a Girls, b boys. The black points represent the adjusted protective effect of breastfeeding following the values of sum of skinfolds. A point below zero means that breastfeeding has a lowering effect on the considered sum of skinfolds. The grey zone represents the confidence interval. Same adjustment as in table 3.
Discussion
Our study confirms that, when confounders such as sociocultural factors, physical fitness and dietary data (daily fat, energy consumption) are taken into account, no effect of breastfeeding on adiposity can be observed in the whole population of adolescents. The new finding of our study is that quantile regression analysis suggests a protective effect of breastfeeding on the highest percentiles of abdominal adiposity and subcutaneous fatness. This might be of clinical interest because people with higher visceral fat are the most likely to develop cardiovascular diseases later in life [34].
Five studies have investigated the relationship between breastfeeding and body composition in adolescence [35,36,37,38,39], but there are some discrepancies between their results. Two studies concluded to a relationship: The first study showed a beneficial association between breastfeeding and BMI and skinfolds in girls. However, the authors did not adjust for confounding factors [35]. In 2012, Yin et al. [39] reported a negative association between breastfeeding and adolescents’ fat mass. Three other studies did not find any influence of breastfeeding [36,37,38].
All together these studies and our results suggest that, when taking into account confounders, there is no protective effect of breastfeeding on fatness in adolescents. To avoid the risk of underestimation of the effect when taking into account multiple confounders, we used the propensity score. Indeed the propensity score is a tool allowing to compare two groups when counfounders are numerous and randomization is impossible [40], as is the case for breastfeeding, thus strengthens the conclusion. This is the first time that such method is used to assess precisely the relationship between breastfeeding and adiposity in adolescents.
The composition of infant formula is different from breast milk, not only for the amount of protein but also for the amino acid composition. These differences in protein content in infant milk lead to higher dosage of insulin-like growth factor 1 in 12-month-old children [41]. This ‘early protein hypothesis’ could track until the age of 6 years, as recently demonstrated by Koletzko et al. [42] in a randomized study that showed higher mean BMI in children who were fed higher protein formula for the first year of life. However, whether or not such difference persists until adolescence remains to be assessed.
It was suggested recently that the beneficial effect of breastfeeding might act by reducing the prevalence of overweight, obesity, and underweight [43]; quantile regression analysis is required to further investigate possible breastfeeding effects. The quantile regression analysis did not identify any effect of breastfeeding on the BMI Z-score, regardless of the percentile studied. However, our results apply only to a healthy population and cannot be generalized to an obese population. One interesting finding of this study is that it suggests that breastfeeding has a protective effect in the highest percentiles of abdominal fatness. We choose to analyze the waist-to-height ratio owing to its superiority on waist circumference and BMI for detecting cardiometabolic risk factors [44], but also for detecting all-cause mortality [45].
Our study has strengths but also limitations. It included a large cohort of well-phenotyped adolescents, with a very large set of data that included most of the factors known to influence body composition such as physical fitness, physical activity, environmental factors, SES, and food intake. Our study used a high standard of methodology and involved a large population of adolescents within Europe, and it is likely that its results can be generalized to industrialized countries.
The lack of a finding of beneficial effects of breastfeeding on body composition raises the question of a lack of statistical power. We performed a posteriori power calculations based on BMI. Considering an α risk of 5% and given the number of subjects included, our study had a power of 95% to detect a 0.2 effect size, meaning that our sample should identify a significant BMI difference of 0.7 between the breastfed and non-breastfed groups (observed SD 3.7).
Our study has also weaknesses. Parental body composition was estimated by the adolescents because the investigators could not obtain these measurements from the parents. Our study used a cross-sectional design, which does not allow the demonstration of a causal relationship. Another limitation of the study is the retrospective assessment of breastfeeding. Several articles have however suggested that this procedure is a valid and reliable measure of infant feeding habits [46] and Natland et al. [47] recently confirmed in a great cohort analysis that maternal recall of breastfeeding duration was fairly accurate 20 years after delivery, meaning that our recalled duration of breastfeeding could be used in adolescents’ population. In the HELENA study, breastfeeding recording was probably less exposed to recall bias than in previous studies conducted in the USA [48] because each European country participating in the HELENA study used a standardized health booklet that referred specifically to the type of infant feeding and its duration at all ages.
In conclusion this is the first European study to examine the relationship between breastfeeding and adolescents’ body composition. The linkage study did not reveal a significant effect of breastfeeding on several variables reflecting body composition in the whole population. However a non-significant trend toward a protective effect of breastfeeding was highlighted on highest percentiles of abdominal adiposity. This observation suggests that the effect of breastfeeding on abdominal adiposity should be investigated in populations of high-risk adolescents.
Disclosure Statement
Frédéric Gottrand has received consulting fees from Numico Clinical Nutrition, lecture fees from SMS and grant support from Danone Research. The remaining authors state no conflict of interest.
Acknowledgements
The HELENA Study was carried out with the financial support of the European Community Sixth RTD Framework Programme (Contract FOOD-CT-2005-007034). The content of this paper reflects only the authors’ views, and the European Community is not liable for any use that may be made of the information contained therein. The researchers from the University of Zaragoza, Spain are complementary supported by FUNDACION MAPFRE (Spain).
We thanks the ethics committees of all participating countries and the children involved in the HELENA study: The Hellenic National Bioethics Commission, Athens; The Ethics Committee of Forschungsinstitut für Kinderernährung Dortmund; The Ethics Commitee of Gent University Hospital; The Comité de Protection des Personnes Nord-Ouest IV Lille; The Regional Research Ethics Committee of the Medical Center of Pécs; The Comitato Etico Per Le Attivita’ Biomediche, Università Degli Studi di Napoli Federico II, Rome; The Regionala Etikprövningsnämnden Stockholm; The Ethik-Kommission der Medizinischen Universität Wien und des Allgemeinen Krankenhauses der Stadt Wien AKH Vienna; The Comité Ético de Investigacion Clinica de Aragon (CEICA), Zaragoza.
RJ carried out data analyses and drafted the manuscript. DA carried out data analyses and contributed revising the article. TD contributed revising the article. MD participated in the design and carried out the study. SJ carried out data analyses. AEG participated in the design and carried out the study and contributed revising the article. DHS participated in the design and carried out the study. DS participated in the design and carried out the study. MY participated in the design and carried out the study and contributed revising the article. PR participated in the design and carried out the study and contributed revising the article. SM participated in the design and carried out the study. MLA participated in the design and carried out the study and contributed revising the article. GF participated in the design and carried out the study and contributed drafting the article. All authors read and approved the final manuscript.
References
- 1.World Health Organization . Infant and Young Child feeding: Model Chapter for Textbooks for Medical Students and Allied Health Professionals. Geneva: World Health Organization; 2009. [PubMed] [Google Scholar]
- 2.Horta BL, Bahl R, Martines JC, Victora CG. Evidence of the Long-Term Effects of Breastfeeding: Systematic Reviews and Meta-Analysis. Geneva: World Health Organization Publication; 2007. pp. 25–33. [Google Scholar]
- 3.Cope MB, Allison DB. Critical review of the World Health Organization's (WHO) 2007 report on ‘evidence of the long-term effects of breastfeeding: systematic reviews and meta-analysis’ with respect to obesity. Obes Rev. 2008;9:594–605. doi: 10.1111/j.1467-789X.2008.00504.x. [DOI] [PubMed] [Google Scholar]
- 4.Agostoni C, Braegger C, Decsi T, Kolacek S, Koletzko B, Michaelsen KF, Mihatsch W, Moreno LA, Puntis J, Shamir R, Szajewska H, Turck D, van Goudoever J. Breast-feeding: a commentary by the ESPGHAN committee on nutrition. J Pediatr Gastroenterol Nutr. 2009;49:112–125. doi: 10.1097/MPG.0b013e31819f1e05. [DOI] [PubMed] [Google Scholar]
- 5.Marmot MG, Page CM, Atkins E, Douglas JW. Effect of breast-feeding on plasma cholesterol and weight in young adults. J Epidemiol Community Health. 1980;34:164–167. doi: 10.1136/jech.34.3.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arenz S, Ruckerl R, Koletzko B, von Kries R. Breast-feeding and childhood obesity - a systematic review. Int J Obes Relat Metab Disord. 2004;28:1247–1256. doi: 10.1038/sj.ijo.0802758. [DOI] [PubMed] [Google Scholar]
- 7.Owen CG, Martin RM, Whincup PH, Davey-Smith G, Gillman MW, Cook DG. The effect of breastfeeding on mean body mass index throughout life: a quantitative review of published and unpublished observational evidence. Am J Clin Nutr. 2005;82:1298–1307. doi: 10.1093/ajcn/82.6.1298. [DOI] [PubMed] [Google Scholar]
- 8.Harder T, Bergmann R, Kallischnigg G, Plagemann A. Duration of breastfeeding and risk of overweight: a meta-analysis. Am J Epidemiol. 2005;162:397–403. doi: 10.1093/aje/kwi222. [DOI] [PubMed] [Google Scholar]
- 9.Gale C, Logan KM, Santhakumaran S, Parkinson JR, Hyde MJ, Modi N. Effect of breastfeeding compared with formula feeding on infant body composition: a systematic review and meta-analysis. Am J Clin Nutr. 2012;95:656–669. doi: 10.3945/ajcn.111.027284. [DOI] [PubMed] [Google Scholar]
- 10.Engeland A, Bjorge T, Tverdal A, Sogaard AJ. Obesity in adolescence and adulthood and the risk of adult mortality. Epidemiology. 2004;15:79–85. doi: 10.1097/01.ede.0000100148.40711.59. [DOI] [PubMed] [Google Scholar]
- 11.Bhat DS, Yajnik CS, Sayyad MG, Raut KN, Lubree HG, Rege SS, Chougule SD, Shetty PS, Yudkin JS, Kurpad AV. Body fat measurement in Indian men: comparison of three methods based on a two-compartment model. Int J Obes (Lond) 2005;29:842–848. doi: 10.1038/sj.ijo.0802953. [DOI] [PubMed] [Google Scholar]
- 12.Freedman DS, Sherry B. The validity of BMI as an indicator of body fatness and risk among children. Pediatrics. 2009;124((suppl 1)):S23–34. doi: 10.1542/peds.2008-3586E. [DOI] [PubMed] [Google Scholar]
- 13.Moreno LA, De Henauw S, Gonzalez-Gross M, Kersting M, Molnar D, Gottrand F, Barrios L, Sjostrom M, Manios Y, Gilbert CC, Leclercq C, Widhalm K, Kafatos A, Marcos A. Design and implementation of the Healthy Lifestyle in Europe by Nutrition in Adolescence Cross-Sectional Study. Int J Obes (Lond) 2008;32((suppl 5)):S4–11. doi: 10.1038/ijo.2008.177. [DOI] [PubMed] [Google Scholar]
- 14.Moreno LA, Gonzalez-Gross M, Kersting M, Molnar D, de Henauw S, Beghin L, Sjostrom M, Hagstromer M, Manios Y, Gilbert CC, Ortega FB, Dallongeville J, Arcella D, Warnberg J, Hallberg M, Fredriksson H, Maes L, Widhalm K, Kafatos AG, Marcos A. Assessing, understanding and modifying nutritional status, eating habits and physical activity in European adolescents: The HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) study. Public Health Nutr. 2008;11:288–299. doi: 10.1017/S1368980007000535. [DOI] [PubMed] [Google Scholar]
- 15.Beghin L, Castera M, Manios Y, Gilbert CC, Kersting M, De Henauw S, Kafatos A, Gottrand F, Molnar D, Sjostrom M, Leclercq C, Widhalm K, Mesana MI, Moreno LA, Libersa C. Quality assurance of ethical issues and regulatory aspects relating to good clinical practices in the HELENA cross-sectional study. Int J Obes (Lond) 2008;32((suppl 5)):S12–18. doi: 10.1038/ijo.2008.179. [DOI] [PubMed] [Google Scholar]
- 16.Lohman TG, Roche AF, Martorell R. Anthropometric Standardization Reference Manual. Champaign: Human Kinetics Books; 1988. [Google Scholar]
- 17.Tanner JM, Whitehouse RH. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976;51:170–179. doi: 10.1136/adc.51.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Currie C, Molcho M, Boyce W, Holstein B, Torsheim T, Richter M. Researching health inequalities in adolescents: the development of the Health Behaviour in School-Aged Children (HBSC) family affluence scale. Soc Sci Med. 2008;66:1429–1436. doi: 10.1016/j.socscimed.2007.11.024. [DOI] [PubMed] [Google Scholar]
- 19.Iliescu C, Beghin L, Maes L, De Bourdeaudhuij I, Libersa C, Vereecken C, Gonzalez-Gross M, Kersting M, Molnar D, Leclercq C, Sjostrom M, Manios Y, Wildhalm K, Kafatos A, Moreno LA, Gottrand F. Socioeconomic questionnaire and clinical assessment in the HELENA cross-sectional study: methodology. Int J Obes (Lond) 2008;32((suppl 5)):S19–25. doi: 10.1038/ijo.2008.178. [DOI] [PubMed] [Google Scholar]
- 20.Ortega FB, Artero EG, Ruiz JR, Espana-Romero V, Jimenez-Pavon D, Vicente-Rodriguez G, Moreno LA, Manios Y, Beghin L, Ottevaere C, Ciarapica D, Sarri K, Dietrich S, Blair SN, Kersting M, Molnar D, Gonzalez-Gross M, Gutierrez A, Sjostrom M, Castillo MJ. Physical fitness levels among European adolescents: the HELENA study. Br J Sports Med. 2011;45:20–29. doi: 10.1136/bjsm.2009.062679. [DOI] [PubMed] [Google Scholar]
- 21.Vereecken CA, Covents M, Matthys C, Maes L. Young adolescents' nutrition assessment on computer (YANA-C) Eur J Clin Nutr. 2005;59:658–667. doi: 10.1038/sj.ejcn.1602124. [DOI] [PubMed] [Google Scholar]
- 22.Vereecken CA, Covents M, Sichert-Hellert W, Alvira JM, Le Donne C, De Henauw S, De Vriendt T, Phillipp MK, Beghin L, Manios Y, Hallstrom L, Poortvliet E, Matthys C, Plada M, Nagy E, Moreno LA. Development and evaluation of a self-administered computerized 24-h dietary recall method for adolescents in Europe. Int J Obes (Lond) 2008;32((suppl 5)):S26–34. doi: 10.1038/ijo.2008.180. [DOI] [PubMed] [Google Scholar]
- 23.Dehne LI, Klemm C, Henseler G, Hermann-Kunz E. The German Food Code and Nutrient Data Base (BLS II.2) Eur J Epidemiol. 1999;15:355–359. doi: 10.1023/a:1007534427681. [DOI] [PubMed] [Google Scholar]
- 24.Elliott SA, Davies PS, Nambiar S, Truby H, Abbott RA. A comparison of two screening methods to determine the validity of 24-h food and drink records in children and adolescents. Eur J Clin Nutr. 2011;65:1314–1320. doi: 10.1038/ejcn.2011.126. [DOI] [PubMed] [Google Scholar]
- 25.Nagy E, Vicente-Rodriguez G, Manios Y, Beghin L, Iliescu C, Censi L, Dietrich S, Ortega FB, De Vriendt T, Plada M, Moreno LA, Molnar D. Harmonization process and reliability assessment of anthropometric measurements in a multicenter study in adolescents. Int J Obes (Lond) 2008;32((suppl 5)):S58–65. doi: 10.1038/ijo.2008.184. [DOI] [PubMed] [Google Scholar]
- 26.Ortega FB, Artero EG, Ruiz JR, Vicente-Rodriguez G, Bergman P, Hagstromer M, Ottevaere C, Nagy E, Konsta O, Rey-Lopez JP, Polito A, Dietrich S, Plada M, Beghin L, Manios Y, Sjostrom M, Castillo MJ. Reliability of health-related physical fitness tests in European adolescents. The HELENA study. Int J Obes (Lond) 2008;32((suppl 5)):S49–57. doi: 10.1038/ijo.2008.183. [DOI] [PubMed] [Google Scholar]
- 27.Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child. 1995;73:25–29. doi: 10.1136/adc.73.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ketel IJ, Volman MN, Seidell JC, Stehouwer CD, Twisk JW, Lambalk CB. Superiority of skinfold measurements and waist over waist-to-hip ratio for determination of body fat distribution in a population-based cohort of caucasian Dutch adults. Eur J Endocrinol. 2007;156:655–661. doi: 10.1530/EJE-06-0730. [DOI] [PubMed] [Google Scholar]
- 29.Brambilla P, Bedogni G, Moreno LA, Goran MI, Gutin B, Fox KR, Peters DM, Barbeau P, De Simone M, Pietrobelli A. Crossvalidation of anthropometry against magnetic resonance imaging for the assessment of visceral and subcutaneous adipose tissue in children. Int J Obes (Lond) 2006;30:23–30. doi: 10.1038/sj.ijo.0803163. [DOI] [PubMed] [Google Scholar]
- 30.Nambiar S, Truby H, Abbott RA, Davies PS. Validating the waist-height ratio and developing centiles for use amongst children and adolescents. Acta Paediatr. 2009;98:148–152. doi: 10.1111/j.1651-2227.2008.01050.x. [DOI] [PubMed] [Google Scholar]
- 31.Mokha JS, Srinivasan SS, Dasmahapatra P, Fernandez C, Chen W, Xu J, Berenson GS. Utility of waist-to-height ratio in assessing the status of central obesity and related cardiometabolic risk profile among normal weight and overweight/obese children: the Bogalusa Heart Study. BMC Pediatr. 2010;10:73. doi: 10.1186/1471-2431-10-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.D'Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 33.Rehkopf DH. Quantile regression for hypothesis testing and hypothesis screening at the dawn of big data. Epidemiology. 2012;23:665–667. doi: 10.1097/EDE.0b013e318261f7be. [DOI] [PubMed] [Google Scholar]
- 34.Marques MD, Santos RD, Parga JR, Rocha-Filho JA, Quaglia LA, Miname MH, Avila LF. Relation between visceral fat and coronary artery disease evaluated by multidetector computed tomography. Atherosclerosis. 2010;209:481–486. doi: 10.1016/j.atherosclerosis.2009.10.023. [DOI] [PubMed] [Google Scholar]
- 35.Novotny R, Daida YG, Grove JS, Acharya S, Vogt TM. Formula feeding in infancy is associated with adolescent body fat and earlier menarche. Cell Mol Biol (Noisy-le-grand) 2003;49:1289–1293. [PubMed] [Google Scholar]
- 36.Victora CG, Barros F, Lima RC, Horta BL, Wells J. Anthropometry and body composition of 18 year old men according to duration of breast feeding: birth cohort study from Brazil. BMJ. 2003;327:901. doi: 10.1136/bmj.327.7420.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grjibovski AM, Ehrenblad B, Yngve A. Infant feeding in Sweden: socio-demographic determinants and associations with adiposity in childhood and adolescence. Int Breastfeed J. 2008;3:23. doi: 10.1186/1746-4358-3-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Holmes VA, Cardwell C, McKinley MC, Young IS, Murray LJ, Boreham CA, Woodside JV. Association between breast-feeding and anthropometry and CVD risk factor status in adolescence and young adulthood: the Young Hearts Project, Northern Ireland. Public Health Nutr. 2009:1–8. doi: 10.1017/S1368980009991704. [DOI] [PubMed] [Google Scholar]
- 39.Yin J, Quinn S, Dwyer T, Ponsonby AL, Jones G. Maternal diet, breastfeeding and adolescent body composition: a 16-year prospective study. Eur J Clin Nutr. 2012;66:1329–1334. doi: 10.1038/ejcn.2012.122. [DOI] [PubMed] [Google Scholar]
- 40.West SG, Duan N, Pequegnat W, Gaist P, Des Jarlais DC, Holtgrave D, Szapocznik J, Fishbein M, Rapkin B, Clatts M, Mullen PD. Alternatives to the randomized controlled trial. Am J Public Health. 2008;98:1359–1366. doi: 10.2105/AJPH.2007.124446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Socha P, Grote V, Gruszfeld D, Janas R, Demmelmair H, Closa-Monasterolo R, Subias JE, Scaglioni S, Verduci E, Dain E, Langhendries JP, Perrin E, Koletzko B, European Childhood Obesity Trial Study Group Milk protein intake, the metabolic-endocrine response, and growth in infancy: data from a randomized clinical trial. Am J Clin Nutr. 2011;94((6 suppl)):1776S–1784S. doi: 10.3945/ajcn.110.000596. [DOI] [PubMed] [Google Scholar]
- 42.Weber M, Grote V, Closa-Monasterolo R, Escribano J, Langhendries JP, Dain E, Giovannini M, Verduci E, Gruszfeld D, Socha P, Koletzko B, for The European Childhood Obesity Trial Study Group Lower protein content in infant formula reduces BMI and obesity risk at school age: follow-up of a randomized trial. Am J Clin Nutr. 2014;99:1041–1045. doi: 10.3945/ajcn.113.064071. [DOI] [PubMed] [Google Scholar]
- 43.Beyerlein A, Toschke AM, von Kries R. Risk factors for childhood overweight: shift of the mean body mass index and shift of the upper percentiles: results from a cross-sectional study. Int J Obes (Lond) 2010;34:642–648. doi: 10.1038/ijo.2009.301. [DOI] [PubMed] [Google Scholar]
- 44.Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13:275–286. doi: 10.1111/j.1467-789X.2011.00952.x. [DOI] [PubMed] [Google Scholar]
- 45.Carmienke S, Freitag MH, Pischon T, Schlattmann P, Fankhaenel T, Goebel H, Gensichen J. General and abdominal obesity parameters and their combination in relation to mortality: a systematic review and meta-regression analysis. Eur J Clin Nutr. 2013;67:573–585. doi: 10.1038/ejcn.2013.61. [DOI] [PubMed] [Google Scholar]
- 46.Li R, Scanlon KS, Serdula MK. The validity and reliability of maternal recall of breastfeeding practice. Nutr Rev. 2005;63:103–110. doi: 10.1111/j.1753-4887.2005.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 47.Natland ST, Andersen LF, Nilsen TI, Forsmo S, Jacobsen GW. Maternal recall of breastfeeding duration twenty years after delivery. BMC Med Res Methodol. 2012;12:179. doi: 10.1186/1471-2288-12-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gillespie B, d'Arcy H, Schwartz K, Bobo JK, Foxman B. Recall of age of weaning and other breastfeeding variables. Int Breastfeed J. 2006;1:4. doi: 10.1186/1746-4358-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]