Abstract
Background
The Chiranjeevi Yojana (CY) is a Public-Private-Partnership between the state and private obstetricians in Gujarat, India, since 2007. The state pays for institutional births of the most vulnerable households (below-poverty-line and tribal) in private hospitals. An innovative remuneration package has been designed to disincentivise unnecessary cesareans. This study examines characteristics of private facilities which participated in the program.
Methods
We conducted a cross-sectional survey of all facilities which had conducted any births between June 2012 and April 2013 in three districts. We identified 111 private and 47 public facilities. Ninety of the 111 private facilities did caesarean sections in the last three months and were eligible to participate in the CY program. Of these, 40 (44%) participated in the CY program. We conducted descriptive and bivariate analyses followed by a Poisson regression model to estimate prevalence ratios of facility characteristics that predicted participation.
Results
We found that facilities participating in the CY program had a significantly higher likelihood of being general facilities (PR 1.9, 95% CI 1.3–2.9), or conducting lower proportion of cesarean births (PR 2.1, 95% CI 1.2–3.5) or having obstetricians new in private practice (PR 1.9, 95% CI 1.2–3.1) or being less expensive (PR 1.8, 95% CI 1.1–3.0). But none of these factors retained significance in a multi variable model.
Conclusion
Private obstetricians who participate in the CY program tend to be new to private practice, provide general services, conduct fewer caesareans and are also less expensive. This is advantageous to the PPP and widens the target beneficiary groups that can be serviced by the PPP. The state should design remuneration packages with the aim of attracting relatively new obstetricians to set up practices in more remote areas. It is possible that the CY remuneration package design is effective in keeping caesarean rates in check, and needs to be studied further.
Introduction
Globally, Maternal Mortality Ratio (MMR) has declined by 45%, from 380 to 210 per 100,000 births between 1990 and 2013, the period of the Millennium Development Goals. But it still stands at 190 and 510 in LMICs of South Asia and Sub-Saharan Africa respectively [1]. There is now a global commitment to reduce the maternal mortality ratio to less than 70 per 100,000 live births in every country by 2030 as part of the sustainable development goals [2].
The unpredictability of most direct obstetric complications which usually arise as emergencies during childbirth contributes to a large proportion of maternal deaths [3,4]. The presence of Skilled Birth Attendants, who are trained to perform signal functions for emergency obstetric care (EmOC) at the time of childbirth, is key to reducing maternal mortality [5,6]. It is recognized that all the 7 basic EmOC (BEmOC) functions (Injectable Antibiotics, Injectable Uterotonics, Injectable Anticonvulsants, Manual removal of placenta, Removal of retained products, Assisted Vaginal delivery, Neonatal resuscitation) and 2 comprehensive EmOC (CEmOC) functions (Caesarean section and Blood transfusions) require incremental levels of training and skill. Some and/or all of these functions may be performed by a physician, a nurse or a midwife, although all of them are grouped under the broad term of Skilled Birth Attendants (SBAs). An appropriate enabling environment, often a health facility, would ensure that these SBAs can perform effectively [7]. Therefore, the management of childbirths by SBAs in facilities has been advocated as a key strategy to reduce maternal and perinatal deaths [5,6].
As a result, in order to reduce maternal and perinatal deaths, a number of lower middle-income countries (LMICs) have promoted institutional births both in public and private facilities over the last few decades [8]. The use of the private sector for obstetric care has increased substantially all over the world. The World Bank estimates that the formal and informal private sectors have provided obstetric services for more than half of all births in South Asia and Sub-Saharan Africa [9,10]. In five South and South-east Asian countries, private provision was responsible for almost the entire increase in institutional births in the last two decades [11]. The provision of obstetric care by SBAs in facilities, and the consequent possibility of a reduction in maternal mortality is increasingly happening through the private sector.
However, this reduction has mostly happened among wealthier households and among educated women as these women are more likely to have the resources to pay the out-of-pocket costs that private care often requires [12]. Neglected populations in developing countries are unable to access and utilize maternal health care services due to socio-economic deprivation, geographical attributes and low literacy levels [13]. Improving maternal health outcomes can only be possible if health inequalities of these disadvantaged women are addressed in health interventions and policies [14].
It is expected that the inclusion of Universal Health Coverage (UHC) as a Sustainable Development Goal will address such disparities in the future by accelerating equity in access to quality health services [15]. Public-Private-Partnerships (PPPs) between the public and private health sector is one of the essential strategies to attain UHC [16], especially so in regions where private providers supply the bulk of health services as in the case of childbirth services in South Asia and Sub-Saharan Africa [9,10].
There have been numerous PPPs in LMICs in the 90s. But most of these have been in the area of sexual and reproductive health. PPPs for childbirth services have been few [17]. Voucher schemes for safe childbirth through private partners have been implemented in Uganda, Kenya, Cambodia, Bangladesh, Nepal and Pakistan [18,19]. Although some of these have been classified as large scale programs (outlay more than $ 1 million/year) they have been implemented in populations of 1.5 to 5 million, partnered with less than 50 private partners [20] and have not been evaluated for the attributes of private providers. In India, where 70% of all health care expenditure is made in the private sector [21], the recent National Health Policy has recommended the exploration of PPPs as one of the means towards Universal Health Coverage [22]. However, none of the state-wide PPPs for childbirth services which were implemented in Delhi, Haryana, Uttarakhand, Rajasthan and Kolkata were evaluated to elucidate provider characteristics that predict participation in a PPP. This is probably because these PPPs were on a small to medium scale (annual budget of less than $1 million) when compared to the Chiranjeevi (long-life) Yojana program (CY) of Gujarat state [20]. The CY program with an annual budget of more than $1 million, covered 40% of the state’s population (24 million eligible vulnerable population) and has lasted longer than a decade. At its pinnacle, the program partnered with one-third of the private providers in the state (865/2000) [23].
Gujarat, is the western-most state of India with a population of 60.4 million. Fifty-seven percent of the population is rural, 15% belong to Scheduled Tribes and 20% live below the poverty line [24]. The CY was a PPP designed in 2005 by the state of Gujarat in India, as a counter measure to the low availability of emergency obstetric care in the public sector; only eight obstetricians served in public sub-district level hospitals in rural areas [25]. The department of health invited specialist post-graduate qualified obstetricians practicing in the private sector to partner in the CY program if they possessed functioning in-patient facilities with (at least) 15 beds, labor and operating rooms, the ability to manage complicated births, perform caesarean sections and arrange for blood transfusions. Eight hundred and sixty-five obstetricians enrolled into the CY program in 2006–7. Each obstetrician was paid a fixed lump sum of 3600 USD (raised to 4800 USD during our survey) for childbirth services provided to every 100 vulnerable women belonging to below-poverty-line or Scheduled Tribe households (BPL/ST). The poverty line and scheduled tribe criteria for vulnerability which were used for targeting the beneficiaries of the CY program have been defined in the Indian constitution and are regularly updated based on planned and diverse sample surveys conducted across the nation. The calculation of the payment package for the CY program was made on the assumption that the 100 births would include 85 uncomplicated vaginal births, 8 complicated births and 7 caesarean sections [26]. This removed any monetary incentive for private partners to do unnecessary cesarean sections. More than a million births have already occurred under this program between 2005 and 2015. Participation has varied from a high of 865 to a low of 360 private obstetricians over this decade [27].
In order to be able to engage private actors in the pursuit of Universal Health Coverage, we need to know how many and which private providers might be willing to engage in such partnerships [28]. There are no studies reporting on the characteristics of private obstetricians who partner with the government for a public health program geared towards improving maternal health outcomes. This paper aims to study the characteristics of eligible private obstetricians who chose to enter into a partnership with the state government to increase access to intrapartum care to disadvantaged women under the CY PPP program.
Methods
Ethical approval for this study was obtained from institutional review board at Indian Institute of Public Health Gandhinagar, Gujarat, India (ethical approval number: TRC-IEC No. 23/2012).
Study area
Three heterogeneous districts from the western, central and eastern belts of the state, Sabarkantha, Surendranagar and Dahod, each with an average population of 2 million were selected. Each district is further sub divided into10 sub-districts each with a population of 100 000 to 200 000. These districts were purposively selected to represent varying geographic areas [29] socio-demographic indicators, and CY uptake in the state (Table 1). Together, these three districts had a considerably higher proportion of vulnerable subpopulations, defined here as being those living below poverty line or belonging to scheduled tribes. Nearly 60% of the population would be ‘vulnerable’ using this definition and therefore eligible for the CY benefit, but only 21% had received it till 2011. All three districts ranked among the lowest third of the state’s 26 districts on the human development indices.
Table 1. Profile of study districts.
| Population (in millions) [24] | Crude Birth Rate per 1000 [30] | % population rural [24] | % population Scheduled Tribe [24] | % population Below Poverty Line [30] | % eligible for CY benefit (BPL+ST) [24,31] | % of births conducted under Chiranjeevi in 2006–11 out of total registered [32] | |
|---|---|---|---|---|---|---|---|
| Gujarat state | 60.4 | 22.7 | 57.0 | 14.8 | 39.6 | 40.7 | 10.9 |
| Sabarkantha dist | 2.4 | 28.0 | 85.0 | 19.7 | 32.9 | 43.3 | 22.0 |
| Surendranagar dist | 1.7 | 23.0 | 72.0 | 0.9 | 46.5 | 45.4 | 10.1 |
| Dahod dist | 2.1 | 30.2 | 90.0 | 72.4 | 71.6 | 87.9 | 29.7 |
| Total of 3 study districts | 6.2 | 27.0 | 82.3 | 31 | 50.3 | 58.9 | 20.6 |
Study design
A cross-sectional facility survey was conducted between June 2012 and April 2013 of all facilities which had provided any childbirth services in the past year in the three districts.
Data collection
An initial master list of all public and private facilities which conducted any childbirth in the last one year was created from secondary data. We accessed data on public facilities from the website of the state’s department of health and private facilities from the state headquarters of the professional association of Obstetricians and Gynaecologists. All public and private facilities in this list were visited and occurrence of child births in the last one year was verbally verified. These initial facilities were asked to identify any further facilities in their neighborhood which may have conducted births in the past year. These were added to the list and again physically verified and further requested to identify more facilities. This method of snowballing was continued throughout the data collection period until no more new facilities could be identified.
All facilities which had provided any childbirth services in the past year were administered a modified version of the survey forms developed by the WHO, UNICEF, UNFPA and AMDD for the Monitoring emergency obstetric care handbook [33]. Sixteen surveyors and four supervisors were trained to administer questionnaires and carry out field supervision. The data used for this study was collected through two schedules, (i) The facility survey form which assessed facility characteristics, such as their location, years of functioning, bed strength, provision of services other than maternity, as well as information regarding referral services and routine patient care practices in the facility. This form included a section which had to be administered to the facility’s obstetrician regarding his/her age, years of experience, participation in the CY program, charges for a normal or caesarean delivery. There was also a section with a few items to be filled out by reviewing records such as number of vaginal, caesarean and complicated births in the last six months. (ii) The human resources form that recorded details of all staff working in each facility. Data collection for the elements that were used in this analysis was as follows;
Clerical or para-medical staff in each facility responded to questions pertaining to years of functioning of the facility, its bed strength and type (purely obstetric or combined with other specialties).
Obstetricians responded to the question regarding their completed years of experience as an obstetrician.
Facility records were reviewed for numbers and types of births over last six months.
Surveyors observed the availability of an obstetrician 24*7, confirmed the same through interviews with labor room nurses, and recorded this data as full-time or part-time.
Facilities that were eligible to participate in the CY program based on criteria set by the state [34] were tagged onto a GPS map.
Definitions of variables used
Facility participation in the CY program: A CY participant facility was one that met the eligibility criteria set by the state [32] and was part of the CY program. A CY non-participant facility was one that met these criteria but was not a partner in the CY program at the time of the study.
Location of facilities: Private facilities could be located either in the three district headquarter towns (largest towns in the district) or in 18 out of 27 smaller sub-district headquarter towns in each of the three districts.
Facility Type: Facilities either provided purely maternity (and gynecological) in-patient care or they were general hospitals which provided out and inpatient care to men and children with or without the presence of specialists like a general physician, pediatrician, orthopaedician or surgeon.
Bed Strength: This indicated the number of beds in a facility. The state prescribes a preferable bed strength of ‘approximately’ 15 for CY participation, though actual bed strengths of facilities vary.
Obstetrician’s years of experience: Obstetricians reported the number of years they had been in practice since they completed their post-graduate training.
Average number of vaginal births performed over last six months by each facility: Surveyors reviewed facility records and documented the number of normal vaginal births each of the facilities had conducted during the six months before the survey. This was averaged to provide the mean number of births each month.
Proportion of caesarean sections: This variable was the average number of caesareans per month over the last six months as a percentage of all births over last six months in each facility.
Cost: Private obstetricians reported the minimum and maximum amount they charged for a vaginal or a caesarean birth. This was averaged to arrive at costs at each private facility for these services.
Analysis
We conducted descriptive analyses, specifically medians, interquartile ranges and proportions to describe public and private obstetric facility characteristics. Bivariate analyses including Chi-square and Wilcoxon-Mann Whitney tests were used to compare characteristics between CY participant and non-participant facilities.
As CY participation was not rare (>40%), we created a Poisson Regression model with robust 95% confidence intervals to estimate prevalence ratios of facility characteristics that would predict CY participation [35,36]. Characteristics with p-values < 0.05 were included in the final model.
We used Research Electronic Data Capture (REDCap) for data entry and analyzed data using Stata (Version 12.0, StataCorp)
Results
Childbirth services in the three districts had been provided by 300 facilities during the past year. They had attended to 53,896 births in the 6 months prior to the visit of the research team. While 135 facilities conducted less than 10 births per month, 165 facilities conducted ten or more births per month. This latter group accounted for 96% of the total births in the last six months in the three districts. Therefore we worked with this subgroup of facilities in the subsequent analyses presented. Seventy-one percent of these births occurred in private facilities, 31% in CY participant and 40% in CY non-participant facilities, while 29% occurred in public facilities. Births by caesareans took place predominantly in private facilities (Table 2).
Table 2. Distribution of numbers of facilities, self-reported childbirths and proportion of caesarean sections (CS) by facility categories.
| Category of facility | Number of facilities | Births in last 6 months (%) | % Caesarean sections |
|---|---|---|---|
| Private CY participant | 41 | 15935 (31) | 10.5 |
| Private CY non-participant | 70 | 20383 (40) | 21.4 |
| Public | 47 | 15376 (29) | 2.6 |
| Total | 158 | 51694 | 11.0 |
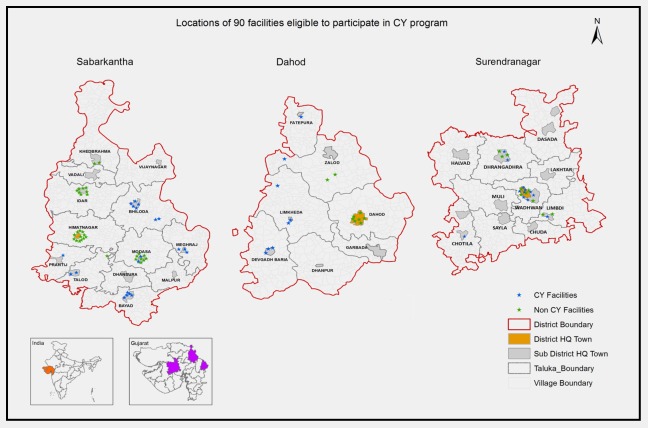
Of the 111 private facilities, 90 were eligible to participate in the CY program as per the criteria set by the state; however, only 40 did (44%). Our map revealed a pattern of CY participation. (Fig 1) CY participant facilities tended to be located in sub-district towns. In seven (Bhiloda, Meghraj, Bayad, Prantij, Talod, Devgadh Baria, Limkheda) out of 14 sub-district towns, all eligible facilities participated en masse in the program; while in two (Himmatnagar and Dahod) out of three district headquarter towns none of the private facilities participated. Three CY participant and four CY non-participant facilities did not consent to participate in the survey.
Fig 1. ‘En masse’ participation/non-participation by eligible private providers in 9 out of 14 towns.
A descriptive analysis of the background characteristics of the participant and non-participant facilities has been presented in Table 3. Although both CY participant and non-participant facilities had been functioning since a median period of about 10 to 13 years, the median period of experience of obstetricians in participant facilities was significantly less by 7 years. While 40 CY facilities conducted a median of 35 vaginal and 6 caesarean births every month, 47 non-CY facilities conducted 41 vaginal and 11 caesarean births. (3 CY non-participant facilities did not allow us to review their records) The proportion of births by caesarean in CY (9%) and nonCY (23%) facilities in the last six months was significantly different. Costs for both vaginal and caesarean births were significantly different in CY and non-CY facilities.
Table 3. Comparison of characteristics of CY and NonCY facilities.
| Facility characteristics (descriptive) | CY | NonCY) | Wilcoxon Mann Whitney test | |||
|---|---|---|---|---|---|---|
| (n = 40) | (n = 50) | |||||
| Median | Median | p value | ||||
| (IQR) | (IQR) | |||||
| Bed Strength | 15 | 17 | 0.55 | |||
| (10–23) | (12–22) | |||||
| Years of functioning | 9.9 | 13 | 0.09 | |||
| (2–17) | (7.4–20) | |||||
| Obstetrician’s years of experience | 10 | 17 | 0.01 | |||
| (3–30) | (10–24) | |||||
| Num of vaginal births recorded per month in last six months | 35 | 41 | 0.90 | |||
| (16–88) | (20–67) | |||||
| Num of caesarean births recorded per month in last six months | 6 | 11 | 0.00 | |||
| (1.5–10.5) | (6.7–18) | |||||
| Proportion of caesarean births in last six months | 8.9 | 22.6 | 0.00 | |||
| (2.8–23.9) | (12.4–37) | |||||
| Costs (Rs) | ||||||
| Normal Delivery Costs | ||||||
| Median | 2500 | 3000 | 0.005 | |||
| Cost range | 225–4500 | 250–7500 | ||||
| Caesarean Costs | ||||||
| Median | 8500 | 10000 | 0.006 | |||
| Cost range | 600–12500 | 1000–30000 | ||||
A simple comparison of CY participant and non-participant facilities showed that CY facilities tended to be located in sub-district headquarter towns and function as general hospitals, providing out and in-patient care for men and children along with maternity care (Table 4). They performed a lower proportion of caesarean sections, were owned by less experienced obstetricians and were cheaper. When individually tested in a Poisson model, a facility possessing each of the following characteristics separately, a general facility type, a facility performing less than 20% of births by caesareans, a facility with an obstetrician with less than 10 years of experience and a facility that charged less than Rs 2500 for vaginal births, was nearly twice as likely to participate in the CY program as a facility not possessing any of these characteristics. In the adjusted Poisson model, none of these variables retained significance (see Table 4).
Table 4. Facility characteristics which predicted CY participation: bivariate and multivariate prevalence ratios using a poisson regression model.
| Facility characteristics | CY participants | CY non-participants | Unadjusted | Adjusted | ||
|---|---|---|---|---|---|---|
| n (%) | n (%) | PR | 95% CI | PR | 95% CI | |
| DistHQ / SubdistHQ | ||||||
| Dist HQ town | 8 (20.0) | 21 (42.0) | Ref | - | ||
| Sub district HQ town | 32 (80.0) | 29 (58.0) | 1.9 | 1.0–3.6 | - | - |
| Facility Type | ||||||
| Purely Maternity | 23 (57.5) | 42 (84.0) | Ref | Ref | ||
| General (Maternity with other) | 17 (42.5) | 8 (16.0) | 1.9 | 1.3–2.9 | 1.2 | 0.8–2.0 |
| Total Bed Strength | ||||||
| <15 | 25 (62.5) | 21 (42.0) | 1.6 | 0.9–2.6 | - | - |
| >15 | 15 (37.5) | 29 (58.0) | Ref | |||
| Ave # of Vaginal Births per month | ||||||
| <40 | 23 (57.5) | 23 (48.9) | 1.2 | 0.7–1.9 | - | - |
| >40 | 17 (42.5) | 24 (51.1) | Ref | |||
| Proportion of births by C-section per month* | ||||||
| <20% | 28 (70.0) | 18 (38.3) | 2.1 | 1.2–3.5 | 1.7 | 0.9–3.0 |
| >20% | 12 (30.0) | 29 (61.7) | Ref | Ref | ||
| Obstetrician’s yrs of experience | ||||||
| Less than 10 yrs | 22 (55.0) | 14 (28.0) | 1.9 | 1.2–3.1 | 1.4 | 0.8–2.3 |
| More than 10 yrs | 17 (42.5) | 36 (72.0) | Ref | Ref | ||
| Median cost of vaginal births | ||||||
| Less than Rs. 2500 | 24 (61.5) | 17 (34.7) | 1.8 | 1.1–3.0 | 1.2 | 0.7–2.0 |
| More than Rs. 2500 | 15 (38.5) | 32 (65.3) | Ref | |||
Discussion
Our study found that 44% of eligible facilities participated in the program. Private facility attributes of being general hospitals, run by younger, less-experienced obstetricians, performing fewer Caesarean sections, and being less expensive were independently associated with likelihood of CY participation. However, this association did not persist in the multivariable model.
Participating facilities tended to be general hospitals. These hospitals tended to provide a broad range of services to children and men from the surrounding areas, not just maternity services. The shortage of health workers in more rural parts of the country has been well-documented. Qualified private providers are reluctant to work there and the public sector is unable to attract and adequately staff rural health facilities [39]. It is possible that a qualified specialist’s willingness to provide general services is indicative of the private provider’s long term commitment to the site of his practice and his urgency to establish his practice quicker by attracting a wider client base through participation in the CY program. This broader range of care provision by CY facilities can be used to mutual advantage by the state when designing PPPs in future since general facilities can provide a wider care package to the entire household.
We found that facilities owned by obstetricians new to private practice, tended to partner with the CY program. This supports the findings of the qualitative study of CY practitioners in the same districts [40], conducted under the same (MATIND) project which had reported that younger obstetricians in the process of establishing their private practices participated in the CY program to quickly “get name and fame”.
An associated finding in our study was that the median costs of both vaginal and caesarean births were significantly lower in CY participant compared to non-participant facilities. These findings were resonated in the qualitative study about CY where private obstetricians reported that market costs in sub-district towns was similar to the CY compensation package. In district towns, not only were routine charges well above the CY package, some obstetricians also perceived CY participation as ‘going down market’ making them less attractive to the wealthier clientele [40]. Similar to CY program, was the MAMTA program implemented in the capital city (Delhi) [41]. Almost 2/3rds of the private partners had reported their intention to leave the program because the compensation was lower than the real costs [42]. This may indicate that private obstetricians who charge less for their services tend to partner with the PPPs.
CY participant facilities performed significantly fewer caesarean sections than non-participants, though whether this characteristic was a precursor or a result of their participation in the CY program was not discernible due to the cross-sectional study design. This finding assumes significance in light of the fact that evidence from private practices in India and from other middle and low income countries such as Mexico, China, Lebanon, Egypt, Tunisia, Turkey and Dominican Republic [43–48]have shown an increasing rate of medical interventions (caesareans and induction) during the intrapartum period.
Although our study across three districts did not establish a significant difference between the characteristics of facilities that might predict participation in the multivariable model, it is possible that our sample was too small to detect heterogeneity within the groups. Based on the bivariate model and the map, it is possible that the more remote location in sub-district towns and newness of practices could account for the significant association of individual predictors like smaller hospitals, lower charges, lesser caesarean sections and the broad general services (not just maternity) provided by these facilities with CY participation.
CY in the context of Public-Private-Partnerships (PPPs) for child birth services
PPPs have improved access to maternal services in many low and middle income countries [19] and have been recommended as an essential strategy to attain UHC [2,9]. Among the 5 countries that have instituted large scale PPPs for childbirth services, only Armenia’s program was universal (3 million population) [20].
In Kenya, Uganda, Bangladesh and Nepal, PPPs were targeted at poor populations of sizes varying from 3 million to 27 million [18]. Of these too, only Kenya and Uganda partnered with a reasonable number of for-profit private providers, 34 and 47 respectively [49,50]. Literature reveals that within India too, 5 states have implemented statewide PPPs targeted at poor populations for childbirth services, with 36 to over 200 for-profit private providers; but none of these lasted more than 2–3 years. Although none of these partnerships have been rigorously evaluated, most of them led to an increase in institutional deliveries as well as a rise in caesarean sections [20,42,51]. The urban location of private providers limited the reach of these programs. At least two of them reported that provider remuneration needed to be raised [42].
In comparison, Gujarat’s CY program was targeted at vulnerable households which constitute approximately 40% (24 million) of the state’s population. It has partnered with 350 to 850 qualified obstetricians for over a decade now, and more than a million deliveries have occurred under the scheme [23]. The remuneration package has been raised over the years but, due to its bulk-purchase character, has always been lower than the prevalent market rates (Table 3). Past assessments of the CY program have shown varying results; both beneficial effects such as reduction in maternal and neonatal mortality among the beneficiaries [26,52] and detrimental practices like participating private facilities treating only low-risk, uncomplicated cases, and referring the more complicated cases to public hospitals [53].One multivariate difference-in-difference study showed that, the CY program had no effect on institutional deliveries, maternal morbidity or out-of-pocket expenditures [54]. But it examined these outcomes after only one year of roll-out of the program in 5 pilot districts known to be underdeveloped [55]. A recent analysis of secondary data from the department of health showed that although the CY program did not lead to a rise in institutional deliveries in the targeted vulnerable group, it did result in a rise in caesarean rates. But this rise has been only 6% (compared to the prevalent rate of 18% in the private sector [37,38]) which is more in agreement with the WHO recommended range of 1–5% for ideal maternal outcomes [56,57]. The authors argued that this may indicate increased access to comprehensive EmOC care in the vulnerable population as a result of the CY program. The CY partnership contracts were designed to pay for EmOC intervention in only 15 out of 100 births, in accordance with indicator 3 of WHO/UNICEF/UNFPA guidelines [33]. This may have deterred unnecessary medical interventions and led to the significantly lower proportion of caesarean sections in CY facilities in our sample. But it is also possible that deserving cases were shifted out of the CY program. Thus the effectiveness of a CY-type payment package design to limit caesareans rates still needs to be investigated, because this could serve as a strategy for expanding PPPs in the future for Universal Health Coverage.
The same secondary analysis also showed that over the last decade, CY benefits have reached only one-third of the target population Table 1, [56]. One of the reasons for this could be the wide temporal and spatial variation of CY participation over the last decade in our study districts as shown by another study [58]. Even though, as per this study, the availability of EmOC care was not much affected across the districts, the fluctuations in local availability could be causing beneficiaries to drop-off locally.
However such variation is not unexpected and underlines the challenges that PPPs pose to achieve a fair distribution of free EmOC provision, even in areas where private obstetricians are abundantly available. We found that private obstetricians’ participation at the time of our survey was a group phenomenon (Fig 1). District headquarter towns had 20 to 30 private obstetricians who collectively stayed out of the CY program. While in smaller towns with less than 10 obstetricians, all of them tended to participate in the CY program. The study was unable to capture the reason for this group behavior of private practices. However, the objective of en masse participation in or out of the partnership can only be to level out any competitive edge within a town that would result from such participation.
The private sector in India is large and will continue to expand rapidly [59] PPPs are essential to achieving universal health coverage for India [40].The Universal Health Coverage plan for India needs to develop a framework for partnerships with the private sector in variable circumstances across the country. Experts argue that in the Indian setting, bureaucratic approaches to implementing regulations for health care delivery have failed. We now need to implement a market-oriented approach through collaborative mechanisms that enhance accountability [60]. Enhancing implementation of PPPs requires multi-sectorial inputs and rigorous implementation science which need to be built into public health governance [48]. The state must aim to produce effective health managers and leaders who can provide stewardship to PPPs for eg. control caesarean rates, design remuneration packages as per need, deal with collective phenomena like en masse participation or non-participation in the program, ensure geographic spread of participant facilities, as well as create trusting relations among providers, local regulators and the public.
Strengths and limitations
This study is among the very few that explore details about PPPs and private sector maternity care in less developed areas of the world. Although we surveyed across a large geographic area, our yield of facilities eligible to participate in the CY program was only 90. A larger sample across more districts may have improved validity of our multivariable model, yielding a better explanatory power of predictor characteristics of facilities. Our final analysis for characteristics of CY participation excluded all private facilities with <10 births/ month. However, less than 5% of births occur in such facilities and therefore our results are representative of the majority of childbirths in the private sector. The generalizability of this study is limited to the more prosperous western and southern states of India which have comparable levels of urbanization and large numbers of qualified private providers [61].
Conclusions
The CY partnership is a unique example of a PPP for maternity care, operating at scale for over a decade now. Our study provides clues to some gaps in the CY program that may be addressed to improve CY partnerships—attracting relatively newer obstetricians and general hospitals, tailoring remuneration packages to address need and remoteness, and minimizing spatial and temporal variations in partnerships. The government could now strategize the program and build it further around these characteristics. Maximizing the effectiveness of such partnerships requires that the state have strong managerial and analytical capacity to steer its course consistently over time.
Supporting information
(DTA)
(DTA)
(DOCX)
(DO)
(DO)
(DO)
Acknowledgments
The authors acknowledge the Gujarat state health department, and the numerous private obstetricians for their cooperation. We would also like to acknowledge Kayleigh Ryan, Gaetano Marrone and Divya Nair for their support with data analysis. We would like to thank the EU FP7 MATIND project which made this research possible. We would also like to thank reviewers of previous version of our manuscript for their constructive comments.
Data Availability
All the data necessary to replicate the findings of this study have been provided as Supporting Information.
Funding Statement
The study was conducted as a part of the MATIND project which is financially supported by a grant under the European Union Framework Program 7 (to ADC).
References
- 1.WHO, UNICEF, UNFPA, The World Bank, United Nations Population Division. Trends in Maternal Mortality: 1990 to 2013 Estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division [Internet]. World Health Organization, Geneva, Switzerland: 2014. Available: http://apps.who.int/iris/bitstream/10665/112697/1/WHO_RHR_14.13_eng.pdf?ua=1 [Google Scholar]
- 2.United Nations. Sustainable Development Goals: 17 Goals to transform our World. In: UN Web Services Section, Department of Public Information [Internet]. Available: http://www.un.org/sustainabledevelopment/sustainable-development-goals/
- 3.Paxton A, Maine D, Freedman L, Fry D, Lobis S. The evidence for emergency obstetric care. Int J Gynecol Obstet. 2005;88: 181–193. doi: 10.1016/j.ijgo.2004.11.026 [DOI] [PubMed] [Google Scholar]
- 4.Campbell OM, Graham WJ. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368: 1284–1299. doi: 10.1016/S0140-6736(06)69381-1 [DOI] [PubMed] [Google Scholar]
- 5.De Brouwere V, Tonglet R, Van Lerberghe W. Strategies for reducing maternal mortality in developing countries: what can we learn from the history of the industrialized West? Trop Med Int Heal. 1998;3: 771–782. doi: 10.1046/j.1365-3156.1998.00310.x [DOI] [PubMed] [Google Scholar]
- 6.Graham WJ, Bell JS, Bullough CHW. Can skilled attendance at delivery reduce maternal mortality in developing countries? Stud HSO&P. 2001;17: 97–129. [Google Scholar]
- 7.World Health Organization. Making pregnancy safer: The critical role of the skilled attendant A joint statement by WHO, ICM and FIGO; 2004. [Google Scholar]
- 8.Wang W, Alva S, Wang S, Fort A. Levels and Trends in the Use of Maternal Health Services in Developing Countries. DHS Comparative Reports. 2011;26. [Google Scholar]
- 9.Benova L, Macleod D, Footman K, Cavallaro F, Lynch CA, Campbell OMR. The role of the private sector in delivery in low-income and middle-income countries: a retrospective, observational analysis of Demographic and Health Surveys from 57 countries. Lancet. Elsevier Ltd; 2014;384 doi: 10.1016/S0140-6736(14)61867-5 [Google Scholar]
- 10.Qureshi Z. Global Monitoring Report 2009: A Development Emergency [Internet]. 2009. doi: 10.1111/j.1553-2712.2009.00606.x [Google Scholar]
- 11.Pomeroy A, Koblinsky M, Alva S. Private Delivery Care in Developing Countries: Trends and Determinants. 2010. [Google Scholar]
- 12.Campbell OMR, Benova L, Macleod D, Baggaley RF, Rodrigues LC, Hanson K, et al. Family planning, antenatal and delivery care: Cross-sectional survey evidence on levels of coverage and inequalities by public and private sector in 57 low- and middle-income countries. Trop Med Int Heal. 2016;21: 486–503. doi: 10.1111/tmi.12681 [DOI] [PubMed] [Google Scholar]
- 13.Yuan B, Qian X, Thomsen S. Disadvantaged populations in maternal health in China who and why? Glob Health Action. 2013;6: 1–13. doi: 10.3402/gha.v6i0.19542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Countdown 2008 Equity Analysis, Boerma JT, Bryce J, Kinfu Y, Axelson H, Victora CG. Mind the gap:equity and trends in coverage of maternal, newborn, and child health services in 54 countdown countries. Lancet. 2008;371: 1259–1267. doi: 10.1016/S0140-6736(08)60560-7 [DOI] [PubMed] [Google Scholar]
- 15.Tangcharoensathien V, Mills A, Palu T. Accelerating health equity: the key role of universal health coverage in the Sustainable Development Goals. BMC Med. 2015;13 doi: 10.1186/s12916-015-0342-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Hanlon B. The Vital Role of the Private Sector in Reproductive Health Governments. Private Sector Partnerships-One Abt Associates Inc. 2009. [Google Scholar]
- 17.Ravindran T. Health sector reform and public-private partnerships for health in Asia: Implications for sexual and reproductive health services Johannesburg: Women’s Health Project, School of Public Health, University of the Witwatersrand; 2002; [Google Scholar]
- 18.Witter S, Somanathan A. Demand-side financing for sexual and reproductive health services in low and middle-income countries: a review of the evidence. 2012; doi: 10.1596/1813-9450-6213 [Google Scholar]
- 19.Jehan K, Sidney K, Smith H, de Costa A. Improving access to maternity services: An overview of cash transfer and voucher schemes in South Asia. Reprod Health Matters. Reproductive Health Matters; 2012;20: 142–154. doi: 10.1016/S0968-8080(12)39609-2 [DOI] [PubMed] [Google Scholar]
- 20.Grainger C, Gorter A, Okal J, Bellows B. Lessons from sexual and reproductive health voucher program design and function: a comprehensive review. Int J Equity Health. 2014;13: 33 doi: 10.1186/1475-9276-13-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Central Statistical Office. Manual on health statistics in India. New Delhi: Ministry of Statistics and Programme Implementation, Government of India; 2015. [Google Scholar]
- 22.MoHFW. Draft National Health Policy 2015 [Internet]. 2014. Available: https://www.nhp.gov.in/sites/default/files/pdf/draft_national_health_policy_2015.pdf
- 23.Iyer V, Sidney K, Mehta R, Mavalankar D. Availability and provision of emergency obstetric care under a public–private partnership in three districts of Gujarat, India: lessons for Universal Health Coverage; 2016; doi: 10.1136/bmjgh-2015-000019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chandramouli C, Registrar G. CENSUS of INDIA 2011. In: Registrar General Census Commissioner. Government of India; 2011.
- 25.Government of India. Rural Health Statistics Bulletin 2006. Rural Health Division, Ministry of Ministry of Health and Family Welfare, Government of India; 2006.
- 26.Mavalankar D, Singh A, Patel SR, Desai A, Singh P V. Saving mothers and newborns through an innovative partnership with private sector obstetricians: Chiranjeevi scheme of Gujarat, India. Int J Gynecol Obstet. International Federation of Gynecology and Obstetrics; 2009;107: 271–276. doi: 10.1016/j.ijgo.2009.09.008 [DOI] [PubMed] [Google Scholar]
- 27.Government of Gujarat. HIMS Reports. Department of Health and Family Welfare; 2014.
- 28.Nishtar S. Can the private sector help achieve universal health coverage? In: World Economic Forum [Internet]. 2016. Available: https://www.weforum.org/agenda/2016/02/how-can-we-achieve-universal-health-coverage/
- 29.Joshi V. Cultural Context of Development in Gujarat In: Hirway I, Kashyap S, Shah A, editors Dynamics of Development in Gujarat Ahmedabad. Concept Publishing Company; 2002. [Google Scholar]
- 30.Commissionerate oRD. Socio Economic Survey Government of Gujarat; 2002–03.
- 31.Indian Census Bureau. Census of India: provisional population totals- India data sheet. Office of the Register General Commissioner, India. 2011.
- 32.Department oHaFW. HIMS Report 2006–2011. Government of Gujarat; 2012.
- 33.WHO, UNICEF, UNFPA, AMDD. Monitoring emergency obstetric care: a handbook. Geneva: World Health Organization; 2009. [Google Scholar]
- 34.Department NIHFW, Department MoHFW. Chiranjeevi Yojana An innovative partnership with the private sector obstetricians to provide skilled care at birth to the poor in Gujarat. Available: https://www.nhp.gov.in/sites/default/files/pdf/chiranjeevi-yojana-details.pdf
- 35.Barros AJD, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3 doi: 10.1186/1471-2288-3-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Deddens JA, Petersen MR. Approaches for estimating prevalence ratios. Occup Environ Med. 2008;65: 501–506. doi: 10.1136/oem.2007.034777 [DOI] [PubMed] [Google Scholar]
- 37.Choudhury C. Caesarean births: the Indian scenario. Population Association of America. 2008; 1–18.
- 38.Ghosh S. Increasing trend in caesarean section delivery in India: Role of medicalisation of maternal health Institute for Social and Economic Change; 2010. [Google Scholar]
- 39.Rao KD, Peters DH. Urban health in India: Many challenges, few solutions. Lancet Glob Heal. Open Access article distributed under the terms of CC BY; 2015;3: e729–e730. doi: 10.1016/S2214-109X(15)00210-7 [DOI] [PubMed] [Google Scholar]
- 40.Ganguly P, Jehan K, de Costa A, Mavalankar D, Smith H. Considerations of private sector obstetricians on participation in the state led “Chiranjeevi Yojana” scheme to promote institutional delivery in Gujarat, India: a qualitative study. BMC Pregnancy Childbirth. 2014;14 doi: 10.1186/1471-2393-14-352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.NIHFW. NIHFW. Evaluation of MAMTA Scheme in National Capital Territory of Delhi. 2010. New Delhi;
- 42.Ravindran T. Public-private partnerships in maternal health services. Econ Polit Weekly. 2011;46: 43. [Google Scholar]
- 43.Neuman M, Alcock G, Azad K, Kuddus A, Osrin D, More NS, et al. Prevalence and determinants of caesarean section in private and public health facilities in underserved South Asian communities: cross-sectional analysis of data from Bangladesh, India and Nepal. BMJ Open. 2014;4 doi: 10.1136/bmjopen-2014-005982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Heredia-Pi I, Servan-Mori EE, Wirtz VJ, Avila-Burgos L, Lozano R. Obstetric Care and Method of Delivery in Mexico: Results from the 2012 National Health and Nutrition Survey. Neu J, editor. PLoS One. 2014;9: e104166 doi: 10.1371/journal.pone.0104166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Feng XL, Wang Y, An L, Ronsmans C. Cesarean section in the People’s Republic of China: Current perspectives. Int J Womens Health. 2014;6: 59–74. doi: 10.2147/IJWH.S41410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.DeJong J, Akik C, El Kak F, Osman H, El-Jardali F. The safety and quality of childbirth in the context of health systems: Mapping maternal health provision in Lebanon. Midwifery. Elsevier; 2010;26: 549–557. doi: 10.1016/j.midw.2010.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Betrán AP, Ye J, Moller A-B, Zhang J, Gülmezoglu AM, Torloni MR. The Increasing Trend in Caesarean Section Rates: Global, Regional and National Estimates: 1990–2014. Zeeb H, editor. PLoS One. 2016;11: e0148343 doi: 10.1371/journal.pone.0148343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Miller S, Abalos E, Chamillard M, Ciapponi A, Colaci D, Comandé D, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet. 2016;388: 2176–2192. doi: 10.1016/S0140-6736(16)31472-6 [DOI] [PubMed] [Google Scholar]
- 49.Arur A, Gitonga N, O’Hanlon B, Kundu F, Senkaali M, Ssemujju R. Insights from innovations: Lessons from designing and implementing family planning / reproductive health voucher programs in Kenya and Uganda [Internet]. Bethesda, MD: Private Sector Partnerships-One project, Abt Associates Inc; 2009. Available: http://shopsproject.org/sites/default/files/resources/5361_file_FINAL_FP_Voucher_Innovations.pdf [Google Scholar]
- 50.Bellows B, Hamilton M, Kundu F. Vouchers for Health: Increasing Utilization of Facility- based family planning and safe motherhood services in Kenya Maternal and Child Health P4P Case Study. Bethesda, Maryland: Health Systems 20/20 project, Abt Associates Inc; 2009. [Google Scholar]
- 51.Government of India. Directory of Innovations Implemented in the Health Sector. Ministry of Health and Family Welfare, Government of India; 2009.
- 52.Singh A, Mavalankar D V., Bhat R, Desai A, Patel SR, Singh P V., et al. Providing skilled birth attendants and emergency obstetric care to the poor through partnership with private sector obstetricians in Gujarat, India. Bull World Health Organ. 2009;87: 960–964. doi: 10.2471/BLT.08.060228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Acharya A, Mcnamee P. Assessing Gujarat’s “Chiranjeevi” Scheme. 2009;XLIV: 13–15. [Google Scholar]
- 54.Mohanan M, Bauhoff S, La Forgia G, Babiarz KS, Singh K, Miller G. Effect of Chiranjeevi Yojana on institutional deliveries and neonatal and maternal outcomes in Gujarat, India: a difference-in-differences analysis. Bull World Health Organ. 2014;92: 187–194. doi: 10.2471/BLT.13.124644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hirway I, Mahadevia D. Gujarat Human Development Report. Mahatma Gandhi Labour Institute, Ahmedabad; 2004. [Google Scholar]
- 56.De Costa A, Vora KS, Ryan K, Raman PS, Santacatterina M, Mavalankar D. The state-led large scale public private partnership “chiranjeevi program” to increase access to institutional delivery among poor women in Gujarat, India: How has it done? What can we learn? PLoS One. 2014;9 doi: 10.1371/journal.pone.0095704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gibbons L, Belizán JM, Lauer J a, Betrán AP, Merialdi M, Althabe F. The Global Numbers and Costs of Additionally Needed and Unnecessary Caesarean Sections Performed per Year: Overuse as a Barrier to Universal Coverage. World Heal Rep Backgr Pap. 2010; 1–31. doi: 10.1017/CBO9781107415324.004 [Google Scholar]
- 58.Vora KS, Yasobant S, Patel A, Upadhyay A, Mavalankar D V. Has Chiranjeevi Yojana changed the geographic availability of free comprehensive emergency obstetric care services in Gujarat, India? Glob Health Action. 2015;8: 1–11. doi: 10.3402/gha.v8.28977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sengupta A, Nundy S. The private health sector in India is burgeoning, but at the cost of public health care. BMJ Br Med J. 2005;331: 1157–1158. doi: 10.1136/bmj.331.7526.1157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Peters DH, Muraleedharan VR. Regulating India’s health services: To what end? What future? Soc Sci Med. 2008;66: 2133–2144. doi: 10.1016/j.socscimed.2008.01.037 [DOI] [PubMed] [Google Scholar]
- 61.Kesterton AJ, Cleland J, Sloggett A, Ronsmans C. Institutional delivery in rural India: the relative importance of accessibility and economic status. BMC Pregnancy Childbirth. 2010;10: 30 doi: 10.1186/1471-2393-10-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DTA)
(DTA)
(DOCX)
(DO)
(DO)
(DO)
Data Availability Statement
All the data necessary to replicate the findings of this study have been provided as Supporting Information.