Abstract
This is a 15-year-old female who presented with sudden onset left flank pain associated with nausea and vomiting and a history of weight loss. Radiological investigation revealed a large non-obstructive tumor involving the lower pole of the left kidney which was primarily thought to be a renal cell carcinoma. She underwent left open radical nephrectomy with adrenalectomy. Histopathology of the resected specimen showed features of Ewing’s sarcoma of the kidney which was confirmed by cytogenetic analysis. This is a rare disease especially in the pediatric group and in reporting such a rare case we hope it helps in identifying a potential course of the disease and its response to the involved treatment.
Keywords: Case report, Ewing’s sarcoma, Kidney, Tumor, Nephrectomy
1. Introduction
Primary renal Ewing sarcoma is a member of Ewing sarcoma family and is considered a rare type of tumor with cases being reported sporadicly since its identification in 1975 [1]. It is primarily a genetic disease with cases affected sporadically, mainly a translocation type of mutation causing a fusion between the EWS gene on chromosome 22 and FLI1 on chromosome 11. The cellular origin of this type of cancer is unknown, however, it is thought to be derived from the neural and neural crest cells [1], [2].
2. Case presentation
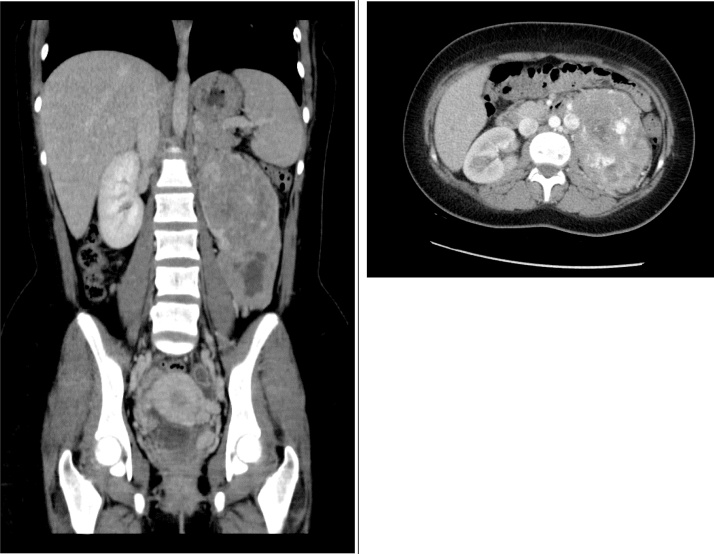
A 15 years old girl, otherwise healthy, was referred from a primary health care center for a history of severe left flank pain that started suddenly and lasted for 3 days associated with nausea and vomiting. The patient reported night sweats and weight loss of 16 kg due to loss of appetite over the last three months before her presentation. No other significant history of hematuria, dysuria, fever, or changes in bowel motions was experienced. No skin changes, body dysmorphic features or neurological deficit were present. Physical examination of this patient revealed left hypochondrial tenderness. A CT scan of the abdomen and pelvis showed a 16 × 10 × 8 left renal mass which was initially presumed to be a renal cell carcinoma Fig. 1. A chest x-ray was done which was unremarkable. No abnormalities were found in renal function tests neither liver profile, serum electrolytes or complete blood count except for normocytic hypochromic anemia with Hemoglobin of 10 g/dl.
Fig. 1.
Abdominal CT with contrast showing large malignant hypervascular left renal mass with exophytic component of the lower pole and central area of necrosis with no venous invasion.
Differential diagnosis:
Renal cell carcinoma
Wilm’s tumor
Treatment:
A decision was made for surgical intervention with open left radical nephrectomy and left adrenalectomy.
Outcome and follow-up:
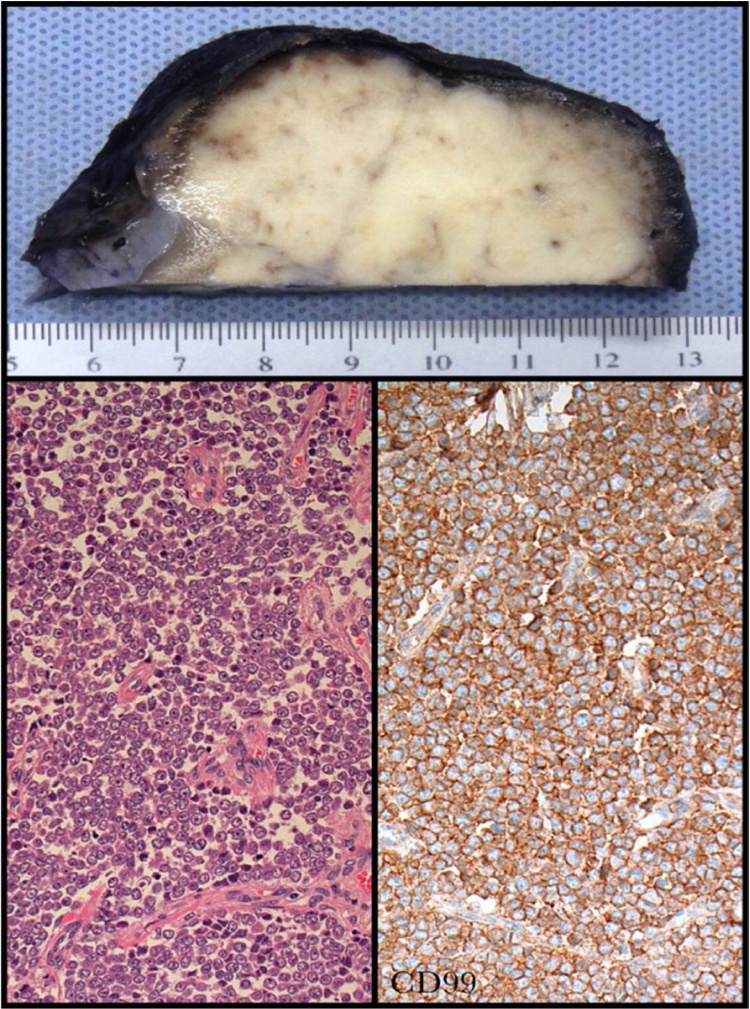
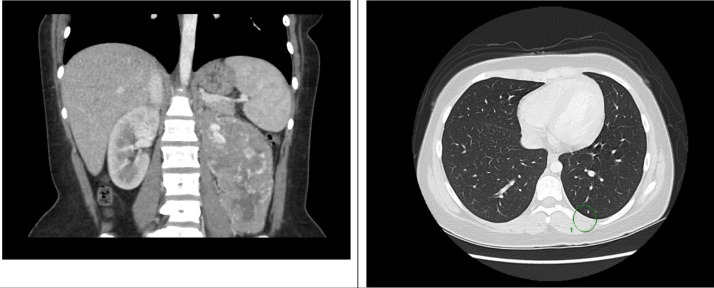
No complications arose during the operation and the post-operative period was uneventful. The patient was discharged on day 7 post-operatively. Histological sections from the kidney showed relatively hypercellular small round cell tumor with scant cytoplasm and areas of necrosis. Tumor cells were positive only for CD99 and Vimentin Fig. 2. The patient was seen after one week in the clinic with a chest CT and bone scan. She was asymptomatic. The chest CT revealed small nodules in both lungs worrisome for metastatic disease Fig. 3. No scintigraphic evidence of osteoblastic bone metastasis was observed in the bone scan. After multidisciplinary meeting with related specialties including urology, medical oncology and radiation oncology, the decision was to start her on chemotherapy and radiotherapy.
Fig. 2.
A gross sample of the resected tumor. In the lower left is a microscopic sample with H&E stain and immunohistochemistry in the lower right.
Fig. 3.
Chest CT showing a small nodule worrisome for metastatic disease.
3. Discussion
This case has been approached and reported according to the SCARE criteria [3]. Presentation of such tumors reported in the literature is non-specific and frequently involves localized pain which usually involves flank, subcostal or abdominal area with or without hematuria [4], [5], [6], [7]. The presence of a vascular thrombus has been reported as a distinctive feature of renal ESFT/PNET [7], [8], [9], [10], [11]. A systemic review of 48 cases of primary Ewing sarcoma of the kidney reported a mean age at diagnosis of 30.4 years with the majority being male. Almost none of the cases reviewed from the literature reported incidental finding of such tumors. As per Risi E et al. metastasis was present in 66% of patients at the time of diagnosis with the lung being the most common site [12]. Due to its dismal prognosis and aggressive behavior, establishing ESFT/PNET for diagnosis is pivotal for the treatment and follow-up. Diagnosis of such tumors is usually determined after resection of the tumor. Computed tomographic scan features, although consistent among different studies, are not specific as they can be the features of any renal neoplasm [11]. Microscopic features associated with ESFT/PNET are considered non-specific as they can be seen in many other tumors, hence, the use of immunochemistry and cytogenetic analysis for definitive diagnosis [11], [13]. There is no unified approach to the treatment of ESFT/PNET neither there are studies on the effectiveness of different treatment modalities on the outcome especially mortality. Surgical resection and adjuvant chemotherapy with or without neoadjuvant chemotherapy and radiotherapy have been implicated in the management of ESFT/PNET. In one systemic review of different case reports adopting different treatment approaches the mean survival of patients was 26 months in non-metastatic disease while in metastatic disease it was 5.6 months.
4. Conclusion
ESFT/PNET is an extremely rare tumor with aggressive behavior with clinical presentation mimicking other round cell tumors of the kidney. Imaging findings as well as microscopic features of the tumor are not specific and have to be reinforced by the use of immunochemistry and cytogenetic analysis for disease confirmation. Early detection of disease prior to metastasis with proper intervention is the principle objective of dealing with such tumors. Studies are needed to establish treatment protocols that diminish disease recurrence rates and improve survival of patients.
Conflicts of interest
I confirm that there is no conflict of interest in our case report.
Funding source
This is a case report and there is no funding sponsor for it.
Ethical approval
I confirm that the concent was taken from the patient and her parents to publish this paper.
And this case was done in an educational hospital (king Abdulaziz medical city).
Consent
I confirm that the concent was taken from the patient and her parents to publish this paper.
Author contribution
The case report written by Dr. Hani albadawe and Dr. Faris alasmari.
The pathologist are Dr. Fahad alsofiani and Dr. Samirah ghandurah.
The uro-oncologist consultant is Dr. Sultan alkhateeb.
Guarantor
King Abdulaziz medical city, Riyadh.
References
- 1.Seemayer T., Thelmo W., Bolande R. Peripheral neuroectodermal tumors. Perspect. Pediatr. Pathol. 1975;2:151–172. [PubMed] [Google Scholar]
- 2.Parham D., Roloson G., Feely M. Primary malignant neuroepithelial tumors of the kidney: a clinicopathologic analysis of 146 adult and pediatric cases from the national wilms’ tumor study group pathology center. Am. J. Surg. Pathol. 2001;25:133–146. doi: 10.1097/00000478-200102000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Abolhasani M., Salarinejad S., Moslemi M.K. Ewing sarcoma/primitive neuroectodermal tumor of the kidney: a report of three cases. Int. J. Surg. Case Rep. 2016;28:330–334. doi: 10.1016/j.ijscr.2016.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hakky T.S., Gonzalvo A.A., Lockhart J.L. Primary Ewing sarcoma of the kidney: a symptomatic presentation and review of the literature. Ther. Adv. Urol. 2013;5(3):153–159. doi: 10.1177/1756287212471095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Angel J.R., Alfred A., Sakhuja A. Ewing’s sarcoma of the kidney. Int. J. Clin. Oncol. 2010;15:314. doi: 10.1007/s10147-010-0042-0. [DOI] [PubMed] [Google Scholar]
- 7.Mellis A.M., Parker D.C., Slobodov G. Primary Ewing’s sarcoma of the kidney with caval involvement: a case report. J. Okla. State Med. Assoc. 2011;104(4):125–127. [PubMed] [Google Scholar]
- 8.Zollner S., Dirksen U., Jurgens H. Renal Ewing tumors. Ann. Oncol. 2013;24(9):2455–2461. doi: 10.1093/annonc/mdt215. [DOI] [PubMed] [Google Scholar]
- 9.Murphy S.M., Browne R.F., Finn S. Non-metastatic primitive peripheral neuroectodermal tumour of the kidney (extraskeletal Ewing’s sarcoma) with vena caval tumour thrombus. BJU Int. 2003;92:e44. doi: 10.1111/j.1464-410x.2003.04059.x. [DOI] [PubMed] [Google Scholar]
- 10.Karnes R.J., Gettman M.T., Anderson P.M. Primitive neuroectodermal tumor (extraskeletal Ewing’s sarcoma) of the kidney with vena caval tumor thrombus. J. Urol. 2000;164(3):772. doi: 10.1097/00005392-200009010-00036. [DOI] [PubMed] [Google Scholar]
- 11.Ekram T., Elsayes K.M., Cohan R.H. Computed tomography and magnetic resonance features of renal Ewing sarcoma. Acta Radiol. 2008;49:1085–1090. doi: 10.1080/02841850802345618. [DOI] [PubMed] [Google Scholar]
- 12.Risi E., Iacovelli R., Altavilla A. Clinical and pathological features of primary neuroectodermal tumor/Ewing sarcoma of the kidney. Urology. 2013;82(2):382–386. doi: 10.1016/j.urology.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 13.Zucman J., Delattre O., Desmaze C. Cloning and characterization of the Ewing’s sarcoma and peripheral neuroepithelioma t(11;22) translocation breakpoints. Genes Chromosomes Cancer. 1992;4:271–277. doi: 10.1002/gcc.2870050402. [DOI] [PubMed] [Google Scholar]