Abstract
Background
This study examined the effects of the Couples Health CoOp intervention on heavy drinking, condom use, and HIV incidence.
Methods
Thirty neighborhoods from one South African township were cluster randomized into three intervention arms: Couples Health CoOp (CHC), Women’s Health CoOp/Men’s Health CoOp (WHC/MHC), or a comparison arm. We recruited 290 men from informal drinking establishments who reported drinking alcohol regularly. We also recruited their main heterosexual sex partners.
Results
At 6-month follow-up, men in the CHC arm were less likely to report heavy drinking (OR 0.47, 95% CI: 0.25, 0.90) and were more likely to report consistent condom use during the past month (OR 2.66, 95% CI: 1.23, 5.76) than men in the comparison arm. At baseline, 26% of women and 13% of men were HIV-infected; at 6-month follow-up, 16 females and 5 males had seroconverted. HIV incidence was significantly lower among women in the CHC arm (IRR 0.22, 95% CI: 0.04, 1.01) than in the WHC/MHC arm.
Conclusions
A couples-based intervention focusing on intersecting risks for HIV can improve biobehavioral outcomes, underscoring the importance of engaging couples together in HIV prevention.
Keywords: HIV prevention, HIV incidence, couples intervention outcomes, alcohol use, condom use, South Africa
1. INTRODUCTION
In 2012 and 2013, HIV prevalence among adults aged 15 to 49 in South Africa was 19% (Simbayi et al., 2014). Although South Africa has made tremendous progress in expanding HIV testing and counseling (HTC) programs and access to antiretroviral therapy (ART; Hontelez et al., 2013) as well as prevention of mother to child transmission during pregnancy, HIV incidence remains high (Joint United Nations Programme on HIV/AIDS, 2014). In 2013, an estimated 340,000 people in South Africa were newly diagnosed with HIV, accounting for 22% of the 1.5 million cases across sub-Saharan Africa. Despite that an estimated 90% of HIV-infected pregnant women received ART, only 56% of other eligible patients living with HIV in 2009 received ART. Moreover, when the threshold for ART eligibility changed from a CD4 count of 350 cells/ml to 500 cells/ml, the proportion dropped to 42%.
Efforts to increase HIV testing and treatment have helped to improve public health control; however, they have not adequately addressed some of the key drivers of HIV incidence in South Africa that intersect with alcohol use, relationship contexts, and gender norms (Doherty et al., 2015; Kalichman et al., 2011; 2013; Minnis et al., 2015; Sawyer et al., 2006; Townsend et al., 2010). A recent meta-analysis found a consistent association between alcohol use and prevalent HIV infection. Moreover, the strength of the association appeared to be greatest among problem drinkers and among people who reported drinking in sexual contexts (Woolf-King et al., 2013).
Heavy drinking among men in South Africa is associated with having multiple concurrent sex partners and low rates of condom use, both of which increase their partner’s risk for contracting HIV (Kalichman et al., 2011, 2013; Townsend et al., 2010; Wechsberg et al., 2013b). Additionally, when men spend much of their household’s income on alcohol, it can force women to seek sex partners outside of their main relationship for money to meet family needs (Mah and Maughan-Brown, 2013; Sawyer et al., 2006; Wechsberg et al., 2013b). Consequently, to reduce HIV incidence in South Africa, behavioral interventions are needed that address alcohol-related risks for HIV within relationships and the contextual drivers of these risks (El-Bassel and Wechsberg, 2012).
This article compares the outcomes of three different interventions to address the risk context between alcohol-using men and their main partners. The Women’s Health CoOp (WHC) is an evidence-based behavioral intervention designed to reduce substance use, violence, and sexual risks for HIV among vulnerable women (USAID, 2009). Field tests in South Africa demonstrated efficacy for the WHC in reducing alcohol use and HIV risk behavior (Wechsberg et al., 2013a; 2010; 2011). However, the WHC does not directly address the male partner’s alcohol use, and women in South African culture often have little agency to change their partner’s behaviors (Wechsberg et al., 2008). More recently, interventions for couples and men were adapted in South Africa and pilot tested to address this gap (Wechsberg et al., 2015).
Couples-based risk-reduction interventions have shown efficacy in increasing communication and problem-solving skills and reducing risk behaviors in couples. In South Africa, apart from couples-based HTC services (Allen et al., 2003; Kilembe et al., 2014), few efforts have addressed HIV risk behavior within the context of a couple or focused specifically on the male partner’s drinking within their community context. South Africa is a low-and-middle-income country, entering its third decade of the HIV epidemic, with high incidence in disadvantaged communities. A key question at this juncture in the epidemic is what type of intervention configuration will best address intersecting risks within couples, such as intervening with couples in a group or separately by gender? This article reports the findings from a cluster-randomized field experiment that tested three modalities of intervening with couples to reduce HIV risk behavior and alcohol use. We hypothesized that the intervention addressing both partners together (the Couples Health CoOp [CHC] arm) would be more efficacious with regard to reducing alcohol use and risk behaviors.
2. METHODS
2.1 Study design
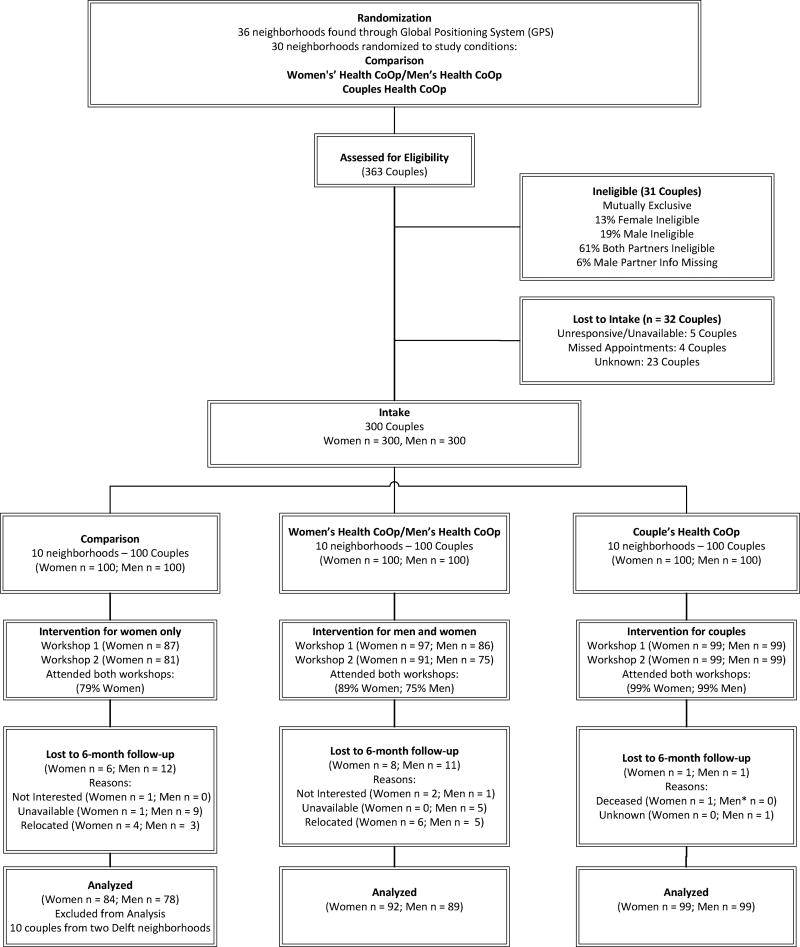
To minimize contamination across study arms, we randomized neighborhoods. From June 2010 through April 2012, we recruited heterosexual couples from shebeens (informal drinking establishments) in Khayelitsha, a high-density township in the Western Cape Province of South Africa. Approximately 99% of Khayelitsha residents are Black African and 100% of study participants were Black African. Three fourths of residents in Khayelitsha identify as being Christian and 20% follow traditional beliefs. There is some variation in socioecomnomic between residents in the informal and the formal sections of the township; however, this did not differ between study arms. Additional detail about identification and mapping of neighborhoods has been presented elsewhere (Wechsberg et al., 2014). The sampling plan and power analyses account for the effect of neighborhood-based recruitment on sample size. Intracluster correlations ranged from 0.01 to 0.04 for key study characteristics. The study’s Data Manager randomized each neighborhood to one of three arms using a computer-generated randomization sequence. We recruited between 6 and 13 couples from each of the 30 neighborhood clusters. Participants were not blinded to the intervention that they received. During their initial intake visit, all participants were scheduled to complete a follow-up interview approximately 6 months later. The mean number of days between completion of the second intervention session and the 6-month follow-up interview was 158 (median = 156). The study conforms to CONSORT guidelines for cluster randomized trials (Campbell et al., 2012; see Figure 1). The Institutional Review Boards at RTI International and at Stellenbosch University’s Faculty of Health Sciences granted ethical approval for the study.
Fig 1.
CONSORT diagram for cluster-randomized trial
2.2 Participant recruitment and enrollment
Field staff used community outreach to recruit couples (Wechsberg et al., 2014). First, staff approached men in shebeens and described the study. After obtaining verbal permission from men interested in the study, they screened men and their main partners at or near the shebeen. Gender-matched field staff screened men and women separately, with sufficient space apart from each other to maintain confidentiality and to ensure that they did not hear each other’s responses. Screening was conducted at the same time to avoid coercion. Staff then met to determine eligibility of the couple (Doherty et al., 2015; Minnis et al., 2015; Wechsberg et al., 2014).
Eligibility criteria for men included the following: 18 to 35 years of age; Black African; live in the targeted community; report drinking alcohol and frequenting shebeens at least weekly in the past 90 days; and report unprotected sex with their main partner in the past 90 days. Each partner had to independently report the following: being in the relationship for at least 12 months; planning to stay together for at least another year; and that they did not intend to conceive a child in the next year. Consistent answers by both members of the couple provided confirmation that they were in a stable relationship.
At the baseline appointment, each partner provided informed consent, completed a face-to-face interview, and completed biological testing for HIV and for alcohol and other drug (AOD) use. Although ample evidence supports conducting HTC with couples in South Africa to reduce HIV transmission (Minnis et al., 2015), each member of the partnership in this study received HTC separately by design. Interviews were conducted 90% of the time by field staff who were the same gender and ethnicity as the participants. Questionnaires were administered in English using Computer-Assisted Personal Interviewing (CAPI) technology. The questionnaire, the Revised Risk Behavior Assessment (RRBA; Wechsberg, 1998b), has been used in previous studies with South African women (Wechsberg et al., 2013a, 2010). Some questions on the RRBA were modified so that items were applicable to men and women. The adaptation of the RRBA used in this study was divided into 16 sections. The primary topics covered by the sections included sociodemographic characteristics, AOD use, condom use and communication with main partner, sexual behavior, conflict and victimization, gender roles, HIV testing history, criminal history, and history of substance abuse treatment. Field staff was fluent in isiXhosa (the indigenous language) and translated phrases as needed. At each study visit, participants received refreshments and a grocery voucher valued at ZAR 100 (USD 11.50).
2.3 Intervention arms
The intervention arms included (1) the comparison arm in which women received the WHC and men received HTC, (2) the WHC/MHC arm in which women received the WHC and men received the Men’s Health CoOp (MHC), and (3) the CHC arm (Wechsberg et al., 2015). These interventions are based in social cognitive theory (Bandura, 1986) and the AIDS Risk Reduction Model and Ecological Perspective (El-Bassel et al., 2003), with an empowerment framework for women learning skills for harm reduction and negotiation (Wechsberg, 1998a). Peer leaders within the community delivered all three interventions using a manualized cue-card flip-chart in workrooms at the community libraries. All three interventions addressed the following: AOD use, harm reduction and AOD treatment; symptoms and signs of sexually transmitted infections; HIV risks and symptoms; safer sex practices and pleasuring each other; gender roles and gendered expectations about sex; effective communication and conflict resolution skills; dealing with stress; violence prevention; and role modeling for the community. Each intervention consists of a 3-hour workshop session that the peer educators delivered with interactive role-play exercises spaced one week apart, with two modules per workshop and with breaks in between. With the exception of men in the comparison arm, all sessions ended with participants developing action plans containing key messages and homework from their respective interventions.
2.3.1 Women’s Health CoOp intervention
Two of the intervention arms utilized the WHC for women participants, which has been described previously (Wechsberg et al., 2013a; 2010). To ensure cultural and gender congruence with these communities and region, the WHC was modified slightly to include more visuals and to incorporate focus group participants’ voices from the formative phase findings (Wechsberg et al., 2013b). This adaptation also added more material about risks associated with drinking venues, reproductive organs, traditional versus modern gender roles with male partners, and activities to improve communication skills.
2.3.2 Men’s Health CoOp intervention
The MHC parallels the WHC’s format and duration, but it also includes elements from the Men as Partners (MAP) program, which was developed by Engender Health and the Planned Parenthood Association of South Africa (Peacock and Levack, 2004). The original MAP curriculum was designed to engage men in reducing gender-based violence by challenging their attitudes, values and behaviors, and by promoting positive sexual and reproductive health, including HIV prevention (Babor et al., 2001). Several of the concepts and activities related to gender roles were integrated into the intervention.
2.3.3 Couples Health CoOp Intervention
The CHC extends the WHC by integrating essential components from Project Connect (El-Bassel et al., 2003; Wechsberg et al., 2015), an efficacious couples-based HIV intervention that has been used in other settings and populations (El-Bassel et al., 2014; 2011; 2010) and was adapted and pilot tested as descibed by Wechsberg et al. (2015). The CHC reinforced positive dimensions of couples’ relationships with skill-building exercises, particularly around communication and sexual expectations, and the use of a handbook that bolstered sessions with a commitment pledge and take-home activities that couples were asked to complete together. Although the content material is the same relative to the other two interventions, this enhanced intervention presents the material with both a male and female facilitator in a dyadic nature along with communication exercises for the couples during the workshops and as a group.
2.4 Measures
2.4.1 Primary behavioral outcomes
The primary sex risk outcomes were consistent condom use and the number of unprotected vaginal sex acts during the past 30 days among participants who did not report consistent condom use. The primary outcome for alcohol use was heavy drinking.
At baseline, we classified participants according to their scores on the Alcohol Use Disorders Identification Test (AUDIT). Women with scores of 7 or more and men with scores of 8 or more on the AUDIT were classified as hazardous or harmful drinkers (Babor et al., 2001).
In the efficacy analyses, the models controlled for heavy drinking at baseline, defined as drinking 5 or more drinks on an occasion at least weekly. The outcome variable for alcohol use at follow-up was derived from the questions “How many days in the past month did you have 5 or more drinks containing alcohol?” for men and “4 or more drinks” for women. Men who reported drinking 5 or more drinks on 5 or more days in the past 30 days were classified as heavy drinkers. Similarly, women who reported drinking 4 or more drinks on at least 5 days in the past 30 days were classified as heavy drinkers. We used these slightly different measures of heavy drinking at baseline and follow-up because the follow-up question was not originally included in the baseline questionnaire and because the AUDIT question is not gender sensitive.
2.4.2 Secondary biological outcome
HIV serostatus was determined by testing a finger stick blood sample using Unigold and Determine Rapid Tests. If either test was reactive (positive) or indeterminate, a confirmatory Reveal G3 Rapid HIV-1 Antibody Test I was performed. Participants were classified as HIV-infected if any two of the three test results were positive.
To calculate incidence rates, we computed person-time as the number of days between the baseline visit date and the 6-month follow-up visit date contributed by each participant who was not a prevalent case at the baseline visit. Prevalent cases were coded as having zero-person time. Incident cases included participants whose HIV tests were nonreactive at baseline and were classified as HIV-infected at follow-up. One participant was excluded because her HIV test results at baseline indicated she was in the process of seroconversion.
2.5 Analysis
All analyses were stratified by gender. To test for equivalency and randomization across intervention arms, we compared the distribution of sociodemographic factors and behavioral risks using chi-square tests for categorical variables and t-tests for continuous variables. We performed the outcome analyses using an intent-to-treat approach, with participants analyzed on the basis of the intervention arm to which their neighborhood had been assigned, regardless of the number of intervention sessions attended. In preliminary analyses, we applied multilevel modeling to adjust for the neighborhood clusters. We did not observe appreciable differences between methods that accounted for clustering (e.g., generalized estimating equations) versus those that did not (e.g., standard regression). Accordingly, to streamline the presentation of our findings, we opted for the more simplistic presentation on order to concentrate the focus on key findings. Analyses were not blinded.
Because the outcome for heavy drinking is binomially distributed, we performed logistic regression analyses that adjusted for heavy drinking at baseline to assess the intervention effects. We estimated the effects of the CHC arm on consistent condom use during every act of sexual intercourse in the previous 30 days and on the number of unprotected sex acts. We used zero-inflated negative binomial regression because (1) the variance of the outcome/response variable was greater than the mean (therefore, Poisson regression was not appropriate), (2) visual inspection of the histogram revealed a large cluster of zeros and that the responses were overdispersed, and (3) the Vuong fit statistics, which compared the zero-inflated negative binomial regression with standard negative binomial regression count (Hu et al., 2011), indicated the distribution was zero-inflated.
We assessed model fit across non-nested models using the Akaike information criterion (AIC). The analysis yielded a logit model predicting consistent condom use during vaginal sex and a negative binomial model predicting counts for participants whose outcome value is non-zero (i.e., the number of unprotected sex acts). Both odds ratios and incidence rate ratios (with 95% confidence intervals) are derived and reported separately. All models were adjusted for baseline condom use. Participants who reported not having sexual intercourse in the previous 30 days were excluded from the analysis (n = 10 women and n = 16 men).
We applied Poisson regression to compute HIV incidence rate ratios (IRR), comparing individuals in the CHC arm to each of the other two study arms. The models accounted for variability in person-time by treating it as an offset, which constrains the coefficient for each unit increase to the value one.
All statistical analyses used Stata Version 13 (StataCorp, College Station, TX).
3. RESULTS
A total of 36 neighborhoods were mapped and 30 neighborhoods were selected for randomization (Wechsberg et al., 2014). Of the 363 couples screened for eligibility, 31 couples (8.5%) were not eligible and 32 couples (8.8%) did not complete the baseline visit, resulting in 300 couples (100 couples in each of the three intervention arms) who participated in the study. Ten couples recruited from two neighborhoods—both assigned to the comparison arm—outside of Khayelitsha were not included in the analysis.
3.1 Intervention dose and study retention
Intervention completion rates were high, with 99% of the couples in the CHC arm, 89% of the women and 75% of the men in the WHC/MCH arm, and 79% of the women in the comparison arm completing all the intervention sessions. Among the 290 couples (580 individuals), we achieved 93.3% retention over 6 months (Figure 1). No extra effort was made to track couples in any of the intervention arms, and all workshops, irrespective of study arm and target audience, were held in the community center workroom in their neighborhood.
3.2 Baseline characteristics of study participants
Characteristics of the sample by gender and intervention arm are shown in Table 1. At baseline, nearly all characteristics were balanced across the intervention arms for women and men.
Table 1.
Baseline characteristics of participants, by gender and intervention arm, Western Cape Couples Health CoOp, Cape Town, South Africa, 2010–2012
| Women | ||||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Overall N=290 |
CHC N=100 |
WHC/MHC N=100 |
Comparison N=90 |
|||||
|
|
|
|
|
|||||
| Characteristic | N/mean | %/SD | N/mean | %/SD | N/mean | %/SD | N/mean | %/SD |
| Sociodemographic background | ||||||||
| Age, in years (mean, SD) | 24.2 | (5.1) | 23.4 | (4.6) | 24.6 | (5.4) | 24.6 | (5.2) |
| Completed high school education | 74 | (26) | 22 | (22) | 28 | (28) | 24 | (27) |
| Unemployed | 232 | (80) | 77 | (77) | 83 | (83) | 72 | (80) |
| Married/cohabitating | 79 | (27) | 30 | (30) | 27 | (27) | 22 | (24) |
| Housing conditions | ||||||||
| Running water | 126 | (43) | 41 | (41) | 50 | (50) | 35 | (39) |
| Electricity | 254 | (88) | 96 | (96) | 82 | (82) | 76 | (84)** |
| Hazardous or harmful alcohol use (AUDIT) | 84 | (29) | 33 | (33) | 19 | (19) | 32 | (36)* |
| Heavy drinkers (≥5 drinks on ≥5 days past 30 days) | 34 | (12) | 17 | (17) | 5 | (5) | 12 | (13)* |
| Sexual behavior | ||||||||
| Multiple partners | 30 | (10) | 12 | (12) | 12 | (12) | 6 | (7) |
| Last vaginal sexual episode | ||||||||
| Main partner | 289 | (100) | 100 | (100) | 100 | (100) | 89 | (99) |
| Casual partner | 1 | (<1) | 0 | (0) | 0 | (0) | 1 | (1) |
| Alcohol / drug use | 23 | (8) | 11 | (11) | 5 | (5) | 7 | (8) |
| Protected with condom | 61 | (21) | 30 | (30) | 18 | (18) | 13 | (15)* |
| Alcohol / drug use and unprotected | 21 | (7) | 11 | (11) | 4 | (4) | 6 | (7) |
| HIV-infected | 76 | (26) | 30 | (30) | 25 | (25) | 21 | (23) |
| Sociodemographic background | ||||||||
| Age, in years (mean, SD) | 26.1 | (4.8) | 25 | (4.8) | 27.1 | (5.1) | 26.1 | (4.1) |
| Completed high school education | 79 | (28) | 30 | (30) | 24 | (24) | 25 | (29) |
| Unemployed | 201 | (69) | 68 | (68) | 76 | (76) | 57 | (63) |
| Married/cohabitating | 87 | (30) | 32 | (32) | 31 | (31) | 24 | (27) |
| Housing conditions | ||||||||
| Running water | 141 | (49) | 46 | (46) | 50 | (51) | 45 | (52) |
| Electricity | 233 | (81) | 84 | (84) | 78 | (79) | 71 | (82) |
| Hazardous or harmful alcohol use (AUDIT) | 225 | (79) | 74 (74) | (74) | 79 | (81) | 72 | (84) |
| Heavy drinkers (≥5 drinks on ≥5 days past 30 days) | 139 | (49) | 55 | (55) | 44 | (44) | 40 | (46) |
| Sexual behavior | ||||||||
| Multiple partners | 102 | (36) | 43 | (43) | 28 | (28) | 31 | (36) |
| Last vaginal sexual episode | ||||||||
| Main partner | 275 | (96) | 96 | (96) | 96 | (97) | 83 | (97) |
| Casual partner | 10 | (4) | 4 | (4) | 3 | (3) | 3 | (3) |
| Alcohol / drug use | 69 | (24) | 27 | (27) | 23 | (23) | 19 | (22) |
| Protected with condom | 73 | (26) | 16 | (16) | 30 | (30) | 27 | (33)* |
| Alcohol / drug use and unprotected | 55 | (19) | 23 | (23) | 16 | (16) | 16 | (19) |
| HIV-infected | 38 | (13) | 11 | (11) | 17 | (17) | 10 | (11) |
Note. CHC = Couples Health CoOp; WHC/MHC = Women’s Health CoOp/Men’s Health CoOp; Comparison = WHC only
p<0.05;
p<0.01.
At baseline, 29% of the women and 79% of the men were classified as hazardous or harmful drinkers. Significantly fewer women (19%) in the WHC/MHC arm met the criteria for hazardous or harmful drinking compared with the women in the comparison arm (36%) and in the CHC arm (33%). The prevalence of hazardous drinking did not vary for men across the study arms.
Among women and men, 10% and 36%, respectively, reported having multiple sex partners in the past 3 months, with some variation by intervention arm. Nearly all women (99.9%) and men (96%) reported that their main partner was the last person with whom they had sex. Among men, 26% reported that their last episode of vaginal sex was protected; this also varied significantly across intervention arms.
HIV prevalence was twice as high among women (26%) as men (13%) (OR=2.34; 95% CI: 1.52, 3.59, not shown).
3.3 Primary outcomes
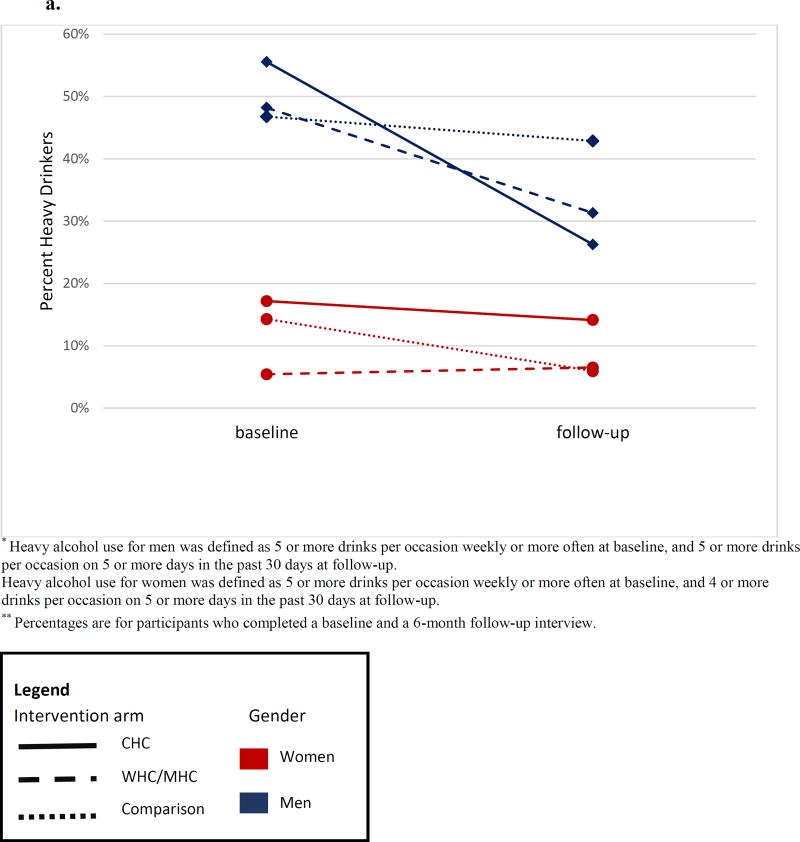
Intervention effects on heavy drinking differed by gender. Between baseline and 6-month follow-up, heavy drinking decreased significantly among women in the CHC arm and the comparison arm, and increased slightly in the WHC/MHC arm (Figure 2a). Relative to the comparison arm, women in the CHC arm were somewhat more likely to report heavy drinking (OR 2.47, 95% CI (0.64, 9.55)); however, the difference was not significant.
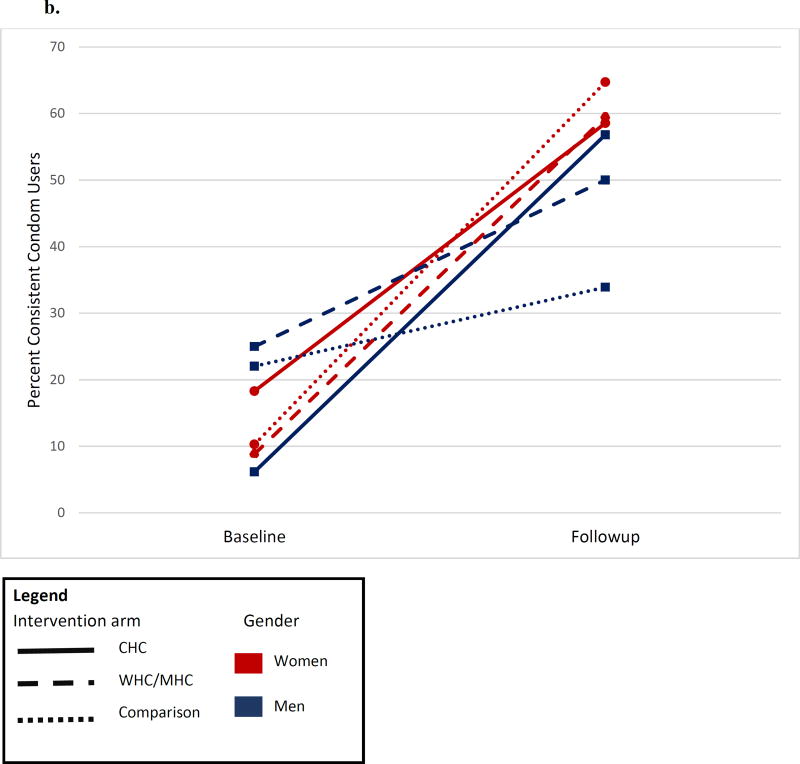
Fig 2.
a. Changes in heavy alcohol use* between baseline and 6-month follow-up interviews**, by intervention arm and gender
b. Changes in consistent condom use between baseline and 6-month follow-up interviews, by intervention arm and gender
Heavy drinking among men decreased in all three arms (Figure 2a). Men in the CHC arm were half as likely to report heavy drinking at 6-month follow-up as men in the comparison arm (OR 0.47, 95% CI: 0.25, 0.89) (Table 2). There were no other significant differences in intervention effects in heavy drinking among men or among women.
Table 2.
Effect estimates of the Couples Health CoOp Study at 6-month follow-up for alcohol use and condom use
| Men (n=258) | Women (n=275) | |||
|---|---|---|---|---|
| Heavy drinkinga | OR | (95% CI) | OR | (95% CI) |
| Comparison | Ref | Ref | ||
| CHC | 0.47 | (0.25, 0.90) | 2.55 | (0.87, 7.48) |
| WHC/MHC | Ref | Ref | ||
| CHC | 0.76 | (0.40, 1.46) | 1.85 | (0.65, 5.24) |
| All sexual acts protected with condomb | OR | OR | ||
| Comparison | Ref | Ref | ||
| CHC | 2.66 | (1.23, 5.76) | 0.78 | (0.36, 1.72) |
| WHC/MHC | Ref | Ref | ||
| CHC | 1.41 | (0.70, 2.84) | 0.86 | (0.41, 1.77) |
| Number of unprotected sexual actsc | IRR | IRR | ||
| Comparison | Ref | Ref | ||
| CHC | 0.56 | (0.38, 0.83) | 1.28 | (0.78, 2.10) |
| WHC/MHC | Ref | Ref | ||
| CHC | 0.88 | (0.59, 1.33) | 0.90 | (0.58, 1.39) |
Note. WHC/MHC = Women’s Health CoOp/Men’s Health CoOp; CHC = Couples Health CoOp; Comparison = WHC only; CI = confidence interval; OR = odds ratio; IRR = incidence rate ratio; Ref = referent
Multiple logistic regression models adjusted for heavy drinking at baseline.
Zero-inflated, negative binomial regression models adjusted for baseline levels of outcome. Each model estimates two components: ORs and IRRs.
Count of unprotected sexual acts among individuals who reported having sex without a condom at least once.
Self-reported consistent condom use for all vaginal sex acts during the previous 30 days increased by 40, 50, and 54 percentage points among women in the comparison arm, the WHC/MHC arm, and the CHC arm, respectively (Figure 2b). The proportion of men reporting consistent condom use in the past 30 days increased in each intervention arm (Figure 2b). At 6-month follow-up, the men in the CHC arm were more likely to report consistent condom use (OR=2.66; 95% CI: 1.23, 5.76) (Table 2) compared with the men in the comparison arm. Among men who reported at least one sex act without using a condom, the men in the CHC arm had a lower rate of unprotected sex acts than the men in the comparison arm (IRR: 0.56; 95% CI: 0.38, 0.83) (Table 2).
3.4 HIV incidence by gender and intervention arm
At 6-month follow-up, 21 participants (16 women and 5 men) seroconverted (not shown). The HIV incidence rates were 16.2 cases per 100 person-years (95% CI: 9.9, 26.5) among women and 4.2 cases per 100 person-years (95% CI: 1.8, 10.1) among men. HIV incidence among women differed by intervention arm: 5.9 per 100 person-years (95% CI: 1.5, 23.4) for the CHC arm, 26.6 per 100 person-years (95% CI: 13.8, 51.0) for the WHC/MHC arm, and 16.3 per 100 person-years (95% CI: 6.8, 39.2) for the comparison arm. HIV incidence was lower among the women in the CHC arm, relative to the WHC/MHC arm (IRR 0.22, 95% CI: 0.04, 1.01), but not for the women in the comparison arm (IRR 0.36, 95% CI: 0.07, 1.85). HIV incidence did not vary by study arm among men, in part because there were only five seroconversions over the follow-up period.
4. DISCUSSION
This study tested the efficacy of the Couples Health CoOp intervention on behavioral outcomes among couples in a low-income township in Cape Town, South Africa. Heavy alcohol use in combination with gender norms that disempower women increases HIV risk in couples (Wechsberg et al., 2013b). The study findings are consistent with previous studies demonstrating that the WHC reduces high-risk behaviors (Wechsberg et al., 2013a; 2010; 2011). The lack of significant differences in sex risk behaviors among the women in the three study arms may be explained by the fact the women in each arm received the WHC or the CHC.
The findings suggest that couples-based interventions are important for HIV prevention among women. We found that when women and men received the intervention together, women had a lower incidence of HIV compared with when women received the intervention alone. This may be because the CHC intervention was efficacious in reducing men’s alcohol consumption and increasing men’s condom use. The explanation for this may rest in the skill-building exercises within the group, the exercises asked of the couple, and the homework given to strengthen the couple’s relationship in a more positive direction. The CHC intervention was associated with increased condom use for men as compared with the men in the comparison arm; yet, condom use did not significantly differ between the men in the CHC arm and the WHC/MHC arm. This suggests the need to further study if male partners can benefit from an intervention regardless of whether they receive it as a couple or in male-only groups.
4.1 Limitations
We conducted this study with a high-risk population in a densely populated low-income township, which may limit its generalizability to other lower risk populations. The behavioral outcomes are based on self-report, which can be subject to social desirability and poor recall. However, the RRBA has demonstrated adequate reliability (Wechsberg et al., 2003). The intervention effects on HIV incidence should be interpreted cautiously because they are from a very small number (n=21) of incident cases and the study was not powered to detect this effect. Follow-up was limited to 6 months; consequently, the longer term sustainability of the intervention effects is not known.
4.2 Future steps
The CHC intervention improved behavioral outcomes and reduced HIV incidence among women. These findings raise the possibility that couple-based HIV prevention interventions that combine shared activities as a dyad with separate activities for men and women may be particularly efficacious, which is supported by other analyses of women participants (Minnis et al., 2015). It is possible that even greater reductions in HIV incidence may be achieved by combining these behavioral interventions with biomedical interventions, such as antiretroviral therapy for infected partners (Cohen et al., 2011), pre-exposure prophylaxis for uninfected partners (Baeten et al., 2012), and vaginal microbicides (Karim et al., 2010). Further study regarding the scale-up of combination interventions in high-risk communities is essential to address HIV gender disparities in South Africa.
Highlights.
Men in the couples arm were less likely to report heavy drinking at 6-months
Men in the couples arm were more likely to report past-month consistent condom use
Women tested at twice the prevalence of HIV (26%) as men (13%)
At 6-months, HIV incidence was significantly lower among women in the intervention
Couples-based interventions focusing on intersecting HIV risks can improve outcomes
Acknowledgments
The authors would like to thank all of the study participants. We would also like to thank Jeffrey Novey for editorial assistance.
Role of the funding source
This research was supported by the U.S. National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism (NIAAA) grant R01 AA018076. Preliminary findings were presented at AIDS2014 in Melbourne, Australia. The views and conclusions are those of the authors and do not necessarily reflect the views of NIAAA. The funding agency had no role in the research design; in the collection, analysis, and interpretation of the data; in the writing of this article, or in the decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Trial Registration: ClinicalTrials.gov registration NCT01121692.
Contributors
WMW developed and designed the study, interpreted the findings, and finalized the revised manuscript. WAZ contributed to the study design, analyses, writing and revision. NEB contributed to the study design and writing. IAD conducted the analyses and contributed to the writing and revision. AMM conducted quality assurance of the analyses. SDN directed, reviewed, and interpreted the revised analyses. BM contributed to interpretation of the findings and the writing. TC contributed to study development, data collection, and writing. All authors have read and approved the manuscript for submission.
Conflict of interest statement
The authors declare that there are no conflicts of interest.
References
- Allen S, Meinzen-Derr J, Kautzman M, Zulu I, Trask S, Fideli U, Musonda R, Kasolo F, Gao F, Haworth A. Sexual behavior of HIV discordant couples after HIV counseling and testing. AIDS. 2003;17:733–740. doi: 10.1097/00002030-200303280-00012. [DOI] [PubMed] [Google Scholar]
- Babor TF, Biddle-Higgins JC, Saunders JB, Monteiro MG. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for use in primary health care. World Health Organization; Geneva, Switzerland: 2001. [Google Scholar]
- Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, Tappero JW, Bukusi EA, Cohen CR, Katabira E, Ronald A, Tumwesigye E, Were E, Fife KH, Kiarie J, Farquhar C, John-Stewart G, Kakia A, Odoyo J, Mucunguzi A, Nakku-Joloba E, Twesigye R, Ngure K, Apaka C, Tamooh H, Gabona F, Mujugira A, Panteleeff D, Thomas KK, Kidoguchi L, Krows M, Revall J, Morrison S, Haugen H, Emmanuel-Ogier M, Ondrejcek L, Coombs RW, Frenkel L, Hendrix C, Bumpus NN, Bangsberg D, Haberer JE, Stevens WS, Lingappa JR, Celum C Partners for the PrEP Study Team. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N. Engl. J. Med. 2012;367:399–410. doi: 10.1056/NEJMoa1108524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Social Foundations Of Thought And Action : A Social Cognitive Theory. Prentice-Hall; Englewood Cliffs, N.J: 1986. [Google Scholar]
- Campbell MK, Piaggio G, Elbourne DR, Altman DG Group, C. Consort 2010 statement: extension to cluster randomised trials. BMJ. 2012;345:e5661. doi: 10.1136/bmj.e5661. [DOI] [PubMed] [Google Scholar]
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, Hakim JG, Kumwenda J, Grinsztejn B, Pilotto JH, Godbole SV, Mehendale S, Chariyalertsak S, Santos BR, Mayer KH, Hoffman IF, Eshleman SH, Piwowar-Manning E, Wang L, Makhema J, Mills LA, de Bruyn G, Sanne I, Eron J, Gallant J, Havlir D, Swindells S, Ribaudo H, Elharrar V, Burns D, Taha TE, Nielsen-Saines K, Celentano D, Essex M, Fleming TR for the HPTN Study Team. Prevention of HIV-1 infection with early antiretroviral therapy. N. Eng. J. Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doherty IA, Myers B, Zule WA, Minnis AM, Kline T, Parry CD, El-Bassel N, Wechsberg WM. Seek, test, and disclose: knowledge of HIV testing and serostatus among high-risk couples in a South African township. Sex. Transm. Infect. 2015 doi: 10.1136/sextrans-2014-051882. Epub date July 14, 2015. [DOI] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Terlikbayeva A, Beyrer C, Wu E, Chang M, Hunt T, Ismayilova L, Shaw SA, Primbetova S, Rozental Y, Zhussupov B, Tukeyev M. Effects of a couple-based intervention to reduce risks for HIV, HCV, and STIs among drug-involved heterosexual couples in Kazakhstan: a randomized controlled trial. J. Acquir. Immune Defic. Syndr. 2014;67:196–203. doi: 10.1097/QAI.0000000000000277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Wu E, Witte SS, Chang M, Hill J, Remien RH. Couple-based HIV prevention for low-income drug users from New York City: a randomized controlled trial to reduce dual risks. J. Acquir. Immune Defic. Syndr. 2011;58:198–206. doi: 10.1097/QAI.0b013e318229eab1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Jemmott JB, Landis JR, Pequegnat W, Wingood GM, Wyatt GE, Bellamy SL NIMH Multisite HIV/STD Prevention Trial for African American Couples Group. National Institute of Mental Health Multisite Eban HIV/STD Prevention Intervention for African American HIV serodiscordant couples: a cluster randomized trial. Arch. Intern. Med. 2010;170:1594–1601. doi: 10.1001/archinternmed.2010.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Wechsberg WM. Couple-based behavioral HIV interventions: placing HIV risk-reduction responsibility and agency on the female and male dyad. Couple Family Psychol. Res. Pract. 2012;1:94–105. [Google Scholar]
- El-Bassel N, Witte SS, Gilbert L, Wu E, Chang M, Hill J, Steinglass P. The efficacy of a relationship-based HIV/STD prevention program for heterosexual couples. Am. J. Public Health. 2003;93:963–969. doi: 10.2105/ajph.93.6.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hontelez JA, Lurie MN, Barnighausen T, Bakker R, Baltussen R, Tanser F, Hallett TB, Newell ML, de Vlas SJ. Elimination of HIV in South Africa through expanded access to antiretroviral therapy: a model comparison study. PLoS Med. 2013;10:e1001534. doi: 10.1371/journal.pmed.1001534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu MC, Pavlicova M, Nunes EV. Zero-inflated and hurdle models of count data with extra zeros: examples from an HIV-risk reduction intervention trial. Am. J. Drug Alcohol Abuse. 2011;37:367–375. doi: 10.3109/00952990.2011.597280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. The Gap Report. Geneva: UNAIDS; 2014. [Google Scholar]
- Kalichman SC, Cain D, Simbayi LC. Multiple recent sexual partnerships and alcohol use among sexually transmitted infection clinic patients, Cape Town, South Africa. Sex. Transm. Dis. 2011;38:18–23. doi: 10.1097/OLQ.0b013e3181e77cdd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Pitpitan E, Eaton L, Cain D, Carey KB, Carey MP, Harel O, Mehlomakhulu V, Simbayi LC, Mwaba K. Bringing it home: community survey of HIV risks to primary sex partners of men and women in alcohol-serving establishments in Cape Town, South Africa. Sex. Transm. Infect. 2013;89:231–236. doi: 10.1136/sextrans-2012-050569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karim QA, Karim SSA, Frohlich JA, Grobler AC, Baxter C, Mansoor LE, Kharsany AB, Sibeko S, Mlisana KP, Omar Z. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329:1168–1174. doi: 10.1126/science.1193748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilembe W, Mokgoro M, Mwaanga A, Kamusoko M, Reddy T, Dissen E, Davitte J, Hilda SP, Brockman M, Ndung'u T. Opportunities for HIV prevention among couples in Durban, South Africa. AIDS Res. Hum. Retroviruses. 2014;30:A111–A112. [Google Scholar]
- Mah TL, Maughan-Brown B. Social and cultural contexts of concurrency in a township in Cape Town, South Africa. Cult. Health Sex. 2013;15:135–147. doi: 10.1080/13691058.2012.745951. [DOI] [PubMed] [Google Scholar]
- Minnis AM, Doherty IA, Kline TL, Zule WA, Myers B, Carney T, Wechsberg WM. Relationship power, communication, and violence among couples: results of a cluster-randomized HIV prevention study in a South African township. Int. J. Womens Health. 2015;7:517–525. doi: 10.2147/IJWH.S77398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peacock D, Levack A. The men as partners program in South Africa: Reaching men to end gender-based violence and promote sexual and reproductive health. Int. J. Mens Health. 2004;3:173–188. [Google Scholar]
- Sawyer KM, Wechsberg WM, Myers BJ. Cultural similarities and differences between a sample of Black/African and colored women in South Africa: convergence of risk related to substance use, sexual behavior, and violence. Women Health. 2006;43:73–92. doi: 10.1300/J013v43n02_05. [DOI] [PubMed] [Google Scholar]
- Simbayi L, Shisa O, Rehle T, Onoya D, Jooste S, Zungu N, Labadarios D, Zuma K. South African National HIV Prevalence, Incidence and Behaviour Survey, 2012. Human Sciences Research Council Press; Cape Town, South Africa: 2014. [DOI] [PubMed] [Google Scholar]
- Townsend L, Rosenthal SR, Parry CD, Zembe Y, Mathews C, Flisher AJ. Associations between alcohol misuse and risks for HIV infection among men who have multiple female sexual partners in Cape Town, South Africa. AIDS Care. 2010;22:1544–1554. doi: 10.1080/09540121.2010.482128. [DOI] [PubMed] [Google Scholar]
- USAID. Integrating Multiple Gender Strategies to Improve HIV and AIDS Interventions: A Compendium of Programs in Africa. International Center for Research on Women 2009 [Google Scholar]
- Wechsberg WM. Facilitating empowerment for women substance abusers at risk for HIV. Pharmacol. Biochem. Behav. 1998a;61:158. [Google Scholar]
- Wechsberg WM. Revised Risk Behavior Assessment, Part I and Part II. Research Triangle Institute; Research Triangle Park, NC: 1998b. [Google Scholar]
- Wechsberg WM, Doherty IA, Myers B, Morgan-Lopez AA, Emanuel A, Carney T, Kline TL, Zule WA. Contextualizing gender differences and methamphetamine use with HIV prevalence within a South African community. Int. J. Drug Policy. 2014;25:583–590. doi: 10.1016/j.drugpo.2013.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, El-Bassel N, Carney T, Browne FA, Myers B, Zule WA. Adapting an evidence-based HIV behavioral intervention for South African couples. Subst. Abuse Treat. Prev. Policy. 2015;10:6. doi: 10.1186/s13011-015-0005-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Jewkes R, Novak SP, Kline T, Myers B, Browne FA, Carney T, Morgan Lopez AA, Parry C. A brief intervention for drug use, sexual risk behaviours and violence prevention with vulnerable women in South Africa: a randomised trial of the Women's Health CoOp. BMJ Open. 2013a;3 doi: 10.1136/bmjopen-2013-002622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Lam WK, Zule W, Hall G, Middlesteadt R, Edwards J. Violence, homelessness, and HIV risk among crack-using African-American women. Subst. Use Misuse. 2003;38:669–700. doi: 10.1081/ja-120017389. [DOI] [PubMed] [Google Scholar]
- Wechsberg WM, Luseno W, Riehman K, Karg R, Browne F, Parry C. Substance use and sexual risk within the context of gender inequality in South Africa. Subst. Use Misuse. 2008;43:1186–1201. doi: 10.1080/10826080801918247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Luseno WK, Kline TL, Browne FA, Zule WA. Preliminary findings of an adapted evidence-based woman-focused HIV intervention on condom use and negotiation among at-risk women in Pretoria, South Africa. J. Prev. Interv. Community. 2010;38:132–146. doi: 10.1080/10852351003640799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Myers B, Reed E, Carney T, Emanuel AN, Browne FA. Substance use, gender inequity, violence and sexual risk among couples in Cape Town. Cult. Health Sex. 2013b;15:1221–1236. doi: 10.1080/13691058.2013.815366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Zule WA, Luseno WK, Kline TL, Browne FA, Novak SP, Ellerson RM. Effectiveness of an adapted evidence-based woman-focused intervention for sex workers and non-sex workers: the Women's Health Coop in South Africa. J. Drug Issues. 2011;41:233–252. [Google Scholar]
- Woolf-King SE, Steinmaus CM, Reingold AL, Hahn JA. An update on alcohol use and risk of HIV infection in sub-Saharan Africa: meta-analysis and future research directions. Int. J. Alcohol Drug Res. 2013;2:99–110. [Google Scholar]