Abstract
Introduction
Estimating body fat content has shown to be a better predictor of adiposity-related cardiovascular risk than the commonly used body mass index (BMI). The white-light 3D body volume index (BVI) scanner is a non-invasive device normally used in the clothing industry to assess body shapes and sizes. We assessed the hypothesis that volume obtained by BVI is comparable to the volume obtained by air displacement plethysmography (Bod-Pod) and thus capable of assessing body fat mass using the bi-compartmental principles of body composition.
Methods
We compared BVI to Bod-pod, a validated bicompartmental method to assess body fat percent that uses pressure/volume relationships in isothermal conditions to estimate body volume. Volume is then used to calculate body density (BD) applying the formula density=Body Mass/Volume. Body fat mass percentage is then calculated using the Siri formula (4.95/BD - 4.50) × 100.
Subjects were undergoing a wellness evaluation. Measurements from both devices were obtained the same day. A prediction model for total Bod-pod volume was developed using linear regression based on 80% of the observations (N=971), as follows: Predicted Bod-pod Volume (L)=9.498+0.805*(BVI volume, L)-0.0411*(Age, years)-3.295*(Male=0, Female=1)+0.0554*(BVI volume, L)*(Male=0, Female=1)+0.0282*(Age, years)*(Male=0, Female=1). Predictions for Bod-pod volume based on the estimated model were then calculated for the remaining 20% (N=243) and compared to the volume measured by the Bod-pod.
Results
Mean age among the 971 individuals was 41.5 ± 12.9 years, 39.4% were men, weight 81.6 ± 20.9 kg, BMI was 27.8 ± 6.3kg/m2. Average difference between volume measured by Bod-pod- predicted volume by BVI was 0.0 L, median: -0.4 L, IQR: -1.8 L to 1.5 L, R2=0.9845. Average difference between body fat measured-predicted was-1%, median: -2.7%, IQR: -13.2 to 9.9, R2=0.9236.
Conclusion
Volume and BFM can be estimated by using volume measurements obtained by a white- light 3D body scanner and the prediction model developed in this study.
Keywords: Obesity, 3D-scanner, Body volume, Body composition, Fat mass
Introduction
Measuring body fat (BF) content has shown to be a better predictor of adiposity-related cardiovascular risk factors and diseases than the commonly used body mass index (BMI) [1]. An increase in adiposity as indicated by elevated BF percentage is associated with the presence of hypertension, coronary heart disease, type 2 diabetes and increased mortality risk [1,2]. In order to accurately calculate BF in cardiovascular risk assessment, reliable, practical and cost-efective methods to measure are needed. Hydrostatic weighing, dual-energy X-ray Absorptiometry (DEXA) and air displacement plethysmography (Bod-Pod) are the most accepted methods to assess body composition due to accuracy, [3] however; these measurements tend to be complex, costly and not accessible in all settings. Other more accessible and uncomplicated techniques such as skin fold and bio-impedance appear to be more practical but tend to be less accurate[4,5]. This has led to a delay in the use of these methods in clinical and research practice and exploration of alternative methods to estimate body composition.
We propose the use of the white-light 3D Body Volume Index Scanner (BVI) as an alternative, cost-efective and practical method to assess body composition. BVI is a non-invasive device normally used to assess body shapes and sizes. The objective of this study is to determine if the body composition measurements obtained by BVI are comparable to those obtained by Bod-Pod.
Methods
This study included healthy volunteers older than 18 years of age; that attended an employee wellness center between December 2008 and June 2011. We excluded those patients with claustrophobia and those unable to stand still.
All subjects underwent all study measurements on the same day which included height without shoes recorded to the nearest cm with a stadiometer (Seca; Hanover, MD) and weight measured with a high-sensitivity scale (Tanita Corporation; Arlington Heights, IL) recorded to the nearest 0.1 of a Kg. Subjects also underwent measurements by air displacement plethysmography [(Bod-pod®)COSMED Concord; CA, USA] and a 3D Body Volume Index scanner (BVI®, Select Research; Worcester, UK).
For this study, Bod-Pod was designated as the goldstandard for measuring body composition parameters and body volume, as it is a well-validated method to assess body composition [4-7]. It measures body volume under isothermal conditions and applies the principals of densitometry to determine body density:
Then, the Siri equation is used to calculate body fat mass using body density [8]:
Proper Bod-pod scanning procedures were followed as reported elsewhere [9].
The BVI [10] is a non-invasive optical scanner composed of 32 cameras, forming 16 sensors (located in 4 angles at 4 heights) of white light that collect up to 1.600.000 linear data points over the scan feld (2.1 m high × 1.2 m width × 0.6 m depth). The 3D body volume software (Select Research BVI software V.1.3.21.0) uses the data points to produce cubic measurements at each of the cross sections with a point accuracy of less than 1mm3 over the scan field in 7 seconds.
During the scan, the subject is instructed to be facing forward and motionless, with both feet on standard landmarks (centered 60 cm from the front scanner wall) and holding adjustable side handles so the body landmark points can be accurately located for measurement purposes. The subject must wear form-fitting gray clothing and an elastic swim cap to reduce the amount of air between the hair and skull and allow for the neck circumference to be measurable.
Proper calibration of the 3D scanner to measure circumference was performed before each measurement session by using a cylinder with known volume as the reference standard. The pre-set rule was that whenever the scanner would deliver an error of > 0.1 cm3 during calibration, it would prompt a full recalibration process.
Statistical Methods
We present subject characteristics as frequencies with percentages, mean values and standard deviations (SD) or median and Inter quartile range (IQR, 25th and 75th percentiles) depending on the distribution of the variable. We developed a prediction model that compared BVI volume to the volume obtained by Bod-pod using linear regression based on the first 80% observations of the total available data (sorted by date of measurement). Predictions for Bod-pod volume based on the estimated model were then calculated on the remaining 20% observations from the full dataset, to represent linear association, findings were summarized using coefficients of variation (R2), regression and residual plots. All analyses were performed using SAS®9.3 (SAS Institute Inc., Cary, NC)and figures were generated with R.
Results
The analysis included 1215 individuals, (971 in the development dataset, 244 in the validation dataset). For individuals in the development dataset, mean age was 41.5 ± 12.9 years, 39.4% were men, average weight was 81.6 ± 20.9 kg, average BMI was 27.8 ± 6.3kg/m2. Additional subject characteristics are presented in Table 1.
Table 1.
Patient baseline characteristics and model results.
| Test set (N=971) | Validation set (N=244) | |
|---|---|---|
| Gender | ||
| Female | 588 (60.6%) | 139 (57.0% |
| Male | 383 (39.4%) | 105 (43.0% |
| Age | 41.5 ± 12.9 | 43.7 ± 13.3 |
| Weight (kg) | 81.6 ± 20.9 | 78.9 ± 19.7 |
| Height (cm) | 170.1 ± 9.2 | 169.9 ± 9.9 |
| BMI (Kg/m2) | 27.8 ± 6.3 | 26.7 ± 5.4 |
| Bod-pod: Total volume | 79.6 ± 21.5 | 77.1 ± 20.4 |
| BVI: Total volume | 87.6 ± 25.3 | 84.5 ± 23.5 |
| Observed BFMα | 31.6 ± 10.9 | 30.6 ± 12.3 |
| Predicted BFMπ | 31.5 ± 16.8 | |
| Observed - Predicted volume | 0.0 ± 2.7 | |
| Observed – Predicted BFM | -1.0 ± 16.8 | |
Values presented as mean ± standard deviation and frequencies (%).
Bod-pod=air displacement plethysmography.
BVI= Body volume index obtained from the 3D scanner.
BFM=Body fat mass
Observed values were obtained from Bod-pod.
Predicted values were estimated in the validation set using BVI parameters.
Derived with the Siri equation using observed Bod-pod volume and total mass.
Derived with the Siri equation using predicted Bod-pod volume and total mass.
Predictions for Bod-pod volume based on the estimated model were then calculated for the remaining 20% of the dataset (N=243) and compared to the volume measured by the Bod-pod. The average difference between volume measured by Bod-pod- predicted volume by BVI was 0.0 L, median: -0.4 L, IQR: -1.8 L to 1.5 L. The correlation between volume measured by Bod-pod and predicted volume by BVI using the model was R2 = 0.9845, See Figure 1-A. The average difference between Body fat % measured - predicted was -1%, median: -2.7%, IQR: -13.2 to 9.9, the correlation between BFM measured by Bod-pod and predicted percent fat by BVI using the model was R2 = 0.9236, See Figure 1-B.
Figure 1.
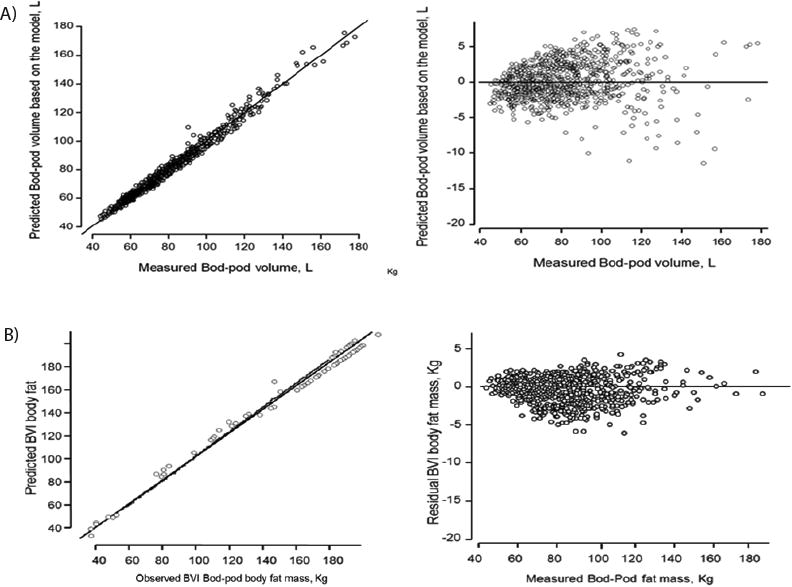
Predicted versus measured Bod-Pod Volume and body fat mass and the corresponding residuals
A: Predicted versus measured Bod-pod volume, L. Figure-1-B: Predicted versus measured body fat mass, Kg.
Discussion
We demonstrated that measurements obtained by this automated 3D-scanner can be used to accurately estimate body volume and BFM.
Increasing evidence is showing the limitations of BMI to assess body adiposity as multiple studies have shown the limited accuracy to diagnose obesity, particularly among subjects with intermediate BMI values. There is also increasing evidence supporting the potential clinical role of measuring body composition in clinical practice. Because individuals with normal BMI can have excessive amounts of body fat and be at high risk for metabolic dysregulation and total cardiovascular mortality, having simple ways to assess body composition in clinical practice becomes of paramount importance [11,12]. Furthermore, because individuals who exercise regularly will have increasing amounts of muscle mass, they may be mistakenly labeled as being overweight when indeed their amount of body fat might still be low, but the BMI will be considered above normal due to the preserved muscle mass. For those individuals an accurate estimation of body composition will also be important to avoid mislabeling an unnecessary anxiety or being in weight loss programs.
Although measuring body composition has gained more attention in recent years and the scientific evidence supports the use of measurement techniques that will be more accurate than the BMI to diagnose obesity, the methods available to measure body composition are still limited. On one end, overly simplistic methods have been proposed to measure body composition like the skinfold technique, but its accuracy has shown to be as limited or even more limited than the BMI to assess body adiposity [5].
In the other extreme are methods that can assess body composition with extreme accuracy like total body MRI, underwater plethysmography, or DEXA scans, but their practicality and cost make them impractical to be implemented in medicine [3]. Therefore, methods that are accurate but not necessarily expensive or technically complicated are urgently needed to fill the gap to measure body composition. The 3D-scanner represents a novel, simple alternative to assess body composition in clinical practice and other settings.
This study has several strengths, including the large sample size, the use of air-displacement plethysmography as the gold standard and the relative simplicity of the methods used to calculate body volume and derive body composition. Because our study population included primarily Caucasian individuals, our results might not be applicable to other races or ethnicities, limiting the generalizability of the findings.
Although the 3D-scanner is noninvasive and technically simple to perform, it is not a portable machine that could be used in the field or places outside an office or medical facility. Finally, we did not compare the results using methods to be considered “gold standard” for body composition, like DEXA or MRI to provide a more robust validation. In despite of those limitations, the simplicity of measuring body composition with a 3D-scanner using white light still represents a viable technique to be considered in medicine and other settings where measuring body composition will be important.
In conclusion, volume and BFM can be estimated by using volume measurements obtained by a white- light 3D body scanner and the prediction model developed in this study.
Acknowledgments
This work was supported by the European Regional Development Fund-Project FNUSA-ICRC (No. Z.1.05/1.1.00/02.0123) (To FLJ and VKS). National Institute of Healthgrants (R01HL65176 and R01HL114024 to VKS).
Abbreviations
- BMI
Body Mass Index
- BVI
Body Volume Index
- Bod-pod
Air Displacement Plethysmography
Footnotes
Conflicts of interest: All authors declare no conflict of interest. Select Research (Worcester, UK), the company that designed the 3D BVI body scanner and software provided without charge the scanner used for this and other studies taking place at Mayo Clinic.
References
- 1.Després JP. Body Fat Distribution and Risk of Cardiovascular Disease: An Update. Circulation. 2012;126:1301–1313. doi: 10.1161/CIRCULATIONAHA.111.067264. [DOI] [PubMed] [Google Scholar]
- 2.Bigaard J, Frederiksen K, Tjønneland A, Thomsen BL, Overvad K, et al. Body fat and fat-free mass and all-cause mortality. Obes Res. 2004;12:1042–1049. doi: 10.1038/oby.2004.131. [DOI] [PubMed] [Google Scholar]
- 3.Medicine ACoS. ACSM's health-related physical fitness assessment manual. 4. Wolters Kluwer; Philadelphia: USA: 2013. [Google Scholar]
- 4.Biaggi RR, Vollman MW, Nies MA, Brener CE, Flakoll PJ, et al. Comparison of air-displacement plethysmography with hydrostatic weighing and bioelectrical impedance analysis for the assessment of body composition in healthy adults. Am J Clin Nutr. 1999;69:898–903. doi: 10.1093/ajcn/69.5.898. [DOI] [PubMed] [Google Scholar]
- 5.Rodriguez-Escudero JP, Pack QR, Somers VK, Thomas RJ, Squires RW. Diagnostic performance of skinfold method to identify obesity as measured by air displacement plethysmography in cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2014;34:335–342. doi: 10.1097/HCR.0000000000000052. [DOI] [PubMed] [Google Scholar]
- 6.Dewit O, Fuller N, Fewtrell M, Elia M, Wells J. Whole body air displacement plethysmography compared with hydrodensitometry for body composition analysis. Arch Dis Child. 2000;82:159–164. doi: 10.1136/adc.82.2.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fields DA, Hunter GR, Goran MI. Validation of the BOD POD with hydrostatic weighing: influence of body clothing. Int J Obes Relat Metab Disord. 2000;24:200–205. doi: 10.1038/sj.ijo.0801113. [DOI] [PubMed] [Google Scholar]
- 8.We S. Body composition from fluid spaces and density: Analysis of methods. In: Brozek J HA, editor. Techniques for Measuring Body Composition. Vol. 1961. Washington: National Academy of Sciences; 1961. pp. 224–244. [Google Scholar]
- 9.McCrory MA, Gomez TD, Bernauer EM, Mole PA. Evaluation of a new air displacement plethysmograph for measuring human body composition. Medicine and science in sports and exercise. 1995;27:1686–1691. [PubMed] [Google Scholar]
- 10.Haycock GB, Schwartz GJ, Wisotsky DH. Geometric method for measuring body surface area: a height-weight formula validated in infants, children, and adults. J Pediatr. 1978;93:62–66. doi: 10.1016/s0022-3476(78)80601-5. [DOI] [PubMed] [Google Scholar]
- 11.Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes. 2008;32:959–966. doi: 10.1038/ijo.2008.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Okorodudu DO, Jumean MF, Montori VM, Romero-Corral A, Somers VK, et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: a systematic review and meta-analysis. Int J Obes. 2010;34:791–799. doi: 10.1038/ijo.2010.5. [DOI] [PubMed] [Google Scholar]


