Abstract
Background
Asthma disproportionately affects minority and low-income children. Investigations that focus on high-risk pediatric populations outside the inner city are limited.
Objective
To compare asthma prevalence and morbidity in urban and rural children in Arkansas.
Methods
We administered a validated survey to parents of children enrolled in urban and rural school districts in Arkansas. Rates of asthma diagnosis, asthma symptoms, medication use, and health care utilization were compared between urban and rural groups.
Results
Age and sex distributions were similar; however, 85% of rural and 67% of urban children were black and 78% of rural and 37% of urban children had state-issued medical insurance (P <.001 for both). Provider-diagnosed asthma was similar in the rural vs urban groups (19% vs 20%); however, rural children were more commonly diagnosed as having chronic bronchitis (7% vs 2%, P <.001). Rural children had more asthma morbidity compared with urban children, including recurrent trouble breathing (odds ratio [OR], 1.9; 95% confidence interval [CI], 1.5–2.2), recurrent cough (OR, 2.2; 95% CI, 1.9–2.6), recurrent chest tightness (OR, 1.8; 95% CI, 1.5–2.2), and repeated episodes of bronchitis (OR, 2.2; 95% CI, 1.7–2.8) during the preceding 2 years. Rural children were more likely to report symptoms consistent with moderate to severe asthma compared with urban children (46% vs 35%, P <.001). There were no differences in health care utilization between groups.
Conclusion
Asthma prevalence was similar between representative rural and urban groups in Arkansas, but asthma morbidity was significantly higher in the rural group.
INTRODUCTION
Asthma is the most common chronic illness of childhood and an important cause of childhood disability. It is estimated that more than 6 million US children younger than 17 years have been diagnosed as having asthma,1 with the overall prevalence doubling from the 1980s to the 1990s. Despite advancements in the medical management of asthma, its prevalence remains high and its economic impact continues to grow. The most recent published data from the Centers for Disease Control and Prevention in 2006 reported more than 7.5 million asthma-related visits to ambulatory care centers, with 750,000 emergency department visits and nearly 200,000 hospitalizations annually.1 Asthma is also responsible for direct health care costs of nearly $15 billion annually. Although mortality has declined during the past decade,2 persistently high asthma morbidity remains problematic, particularly in minority and low-income populations.2,3 For example, black children are 1.5 times more likely to be diagnosed as having asthma and are 7 times more likely to die of their asthma than are white children.1,4,5
To address this public health problem, recent research and intervention programs have been designed to improve asthma diagnosis, management, and morbidity for children with asthma. Most of these efforts have focused on inner-city children due to reports of an increased asthma burden in this population.6 Studies of rural asthma morbidity are limited, and little is known about high-risk populations in rural US environments. Nationwide data in the United States suggest that asthma prevalence is similar between urban and rural populations, and previous studies have revealed high rates of undiagnosed asthma in at-risk rural schoolchildren.7 In addition, based on a systematic review of the literature, Ownby8 concludes that asthma in rural areas may be underdiagnosed; thus, asthma prevalence is likely to be higher than previously estimated. These data suggest that the asthma crisis affects children in many regions of the United States and is not a problem limited to the inner city. We compared the prevalence of asthma diagnosis and asthma-related morbidity between urban and rural schoolchildren in Arkansas, a predominantly rural agricultural state.
METHODS
Study Population
The study population consisted of children aged 4 to 17 years enrolled in public schools in the Little Rock School District (LRSD) (urban) and in the Marvell and Eudora school districts (rural). The LRSD is in the state’s capital city located in Pulaski County and is encompassed in an urban area as defined by the 2000 US Census.9 The LRSD is the largest school district in the state, serving approximately 25,738 students, and it consists of 69% black students, with 54% of all students meeting the federal requirements for the free or reduced price school lunch program.10 Parents of LRSD students completed the survey in the 2002–2003 school year. The rural population consisted of all children enrolled in the Marvell (n = 559) and Eudora (n = 631) school districts during the 2005–2006 school year. The schools are located in 2 noncontiguous counties in the Delta region of Arkansas. The Delta region of Arkansas is located primarily in the eastern half of the state. It is part of the larger Mississippi Delta region of the United States and is severely impoverished and medically underserved.7 There is a high concentration of black residents and families with children aged 5 to 17 years living in poverty (US Census Bureau, 2004). Counties in this region are rural, with predominantly agricultural farming communities producing cotton, rice, soybean, and wheat. In both participating rural school districts, most students were black (97% in Eudora and 91% in Marvell), and 98% or more of the students met the federal requirements for the free or reduced price school lunch program.10
Survey
The primary caregiver of each student was asked to complete the University of Southern California Asthma Health Screening Survey11 regarding his or her child. The University of Southern California survey has been widely used and validated in the Breathmobile program. The survey has been used in low-income and minority populations to identify children at risk for asthma in other disadvantaged US populations. The validated survey instrument consists of 7 multiple-choice questions that focus on the presence and frequency of asthma-related symptoms, previous provider diagnosis of asthma, and health care utilization for asthma-related problems (Fig 1). In addition to the 7 questions of the original survey, an eighth question was added, “Has a provider ever told you that your child has: asthma, chronic bronchitis, or reactive airway disease?” The asthma screening survey was designed to identify children with asthma and to estimate prevalence in the population under study. The asthma identification algorithm was validated against blinded physician assessment11 and showed 87% sensitivity and 84% specificity for correctly identifying children with asthma (sensitivity of 91% for persistent asthma). As previously published,11–13 the 7-model, tiered scoring algorithm uses a combination of asthma symptoms, activity limitations, emergency health care utilization, and medication use. The survey was distributed by and returned to the local school nurse. To maintain confidentiality, personal identifiers were not available to study personnel, and informed consent was waived. The study was approved by the University of Arkansas for Medical Sciences institutional review board.
Figure 1.
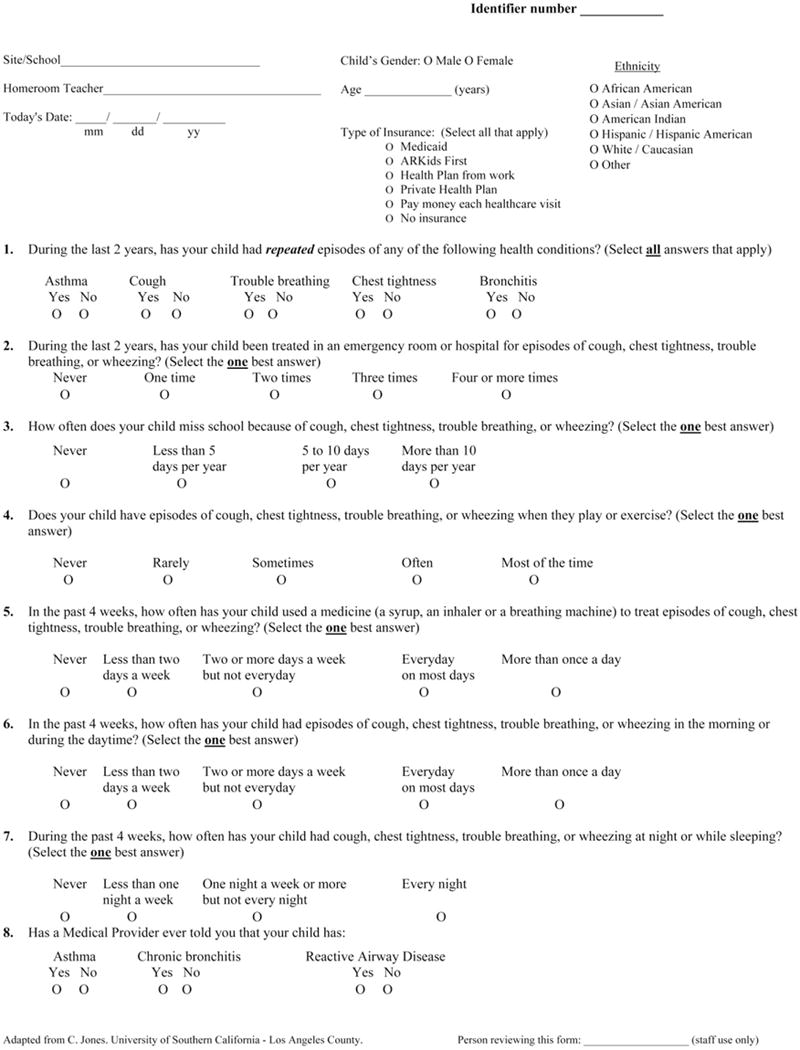
University of Southern California Asthma Health Screening Survey. Revised and used with permission from C. A. Jones.
Asthma Severity Classification
Asthma severity was assigned based on parental report of asthma symptoms and according to published guidelines from the 2007 National Asthma Education and Prevention Program Expert Panel Report 3.14 Individuals were assigned to the most severe category in which any feature occurred. Severity classification was determined for children with algorithm- or physician-diagnosed asthma based on responses to the questions regarding activity limitations and daytime or nocturnal symptoms in the past 4 weeks. The child was classified as having persistent asthma if he or she was reported to have daytime symptoms at least 2 times per week or exercise limitations due to asthma. Children were further classified as having moderate to severe persistent asthma if daytime symptoms occurred 1 or more times per day, if nocturnal symptoms occurred at least 1 night a week, or if exercise limitations were reported as often or most of the time.
Covariates
Caregivers were asked to report demographic information on their child, including age, race (white, black, or other), sex, and type of insurance (private, Medicaid, Arkansas’ State Children’s Health Insurance Program, or uninsured).
Statistical Analysis
All data processing and statistical tests were performed using a software program (SAS version 9.1; SAS Institute Inc, Cary, North Carolina). Fisher exact tests were used to compare differences in proportions between rural and urban children and between mild persistent and moderate to severe persistent asthma. Bivariate logistic regressions were used to measure the effects of rural vs urban location on patient characteristics such as asthma symptoms, medication use, and health care utilization. Results are presented as odds ratios (ORs) with 95% confidence intervals (CIs). Multivariate logistic regression analysis was also performed to consider the independent effect of rural vs urban location on asthma outcomes controlling for age, sex, race, and insurance. All P values are 2-sided, with P < .05 considered statistically significant.
RESULTS
The survey was distributed to 10,895 urban children enrolled in 36 schools in the LRSD and to 1,190 rural children enrolled in the Marvell and Eudora school districts. To reduce the risk of selection bias in the LRSD, schools with a response rate of less than 50% were excluded from the analysis. The remaining schools had a response rate of 86%, and 94% of the surveys (n = 5,412) contained sufficient information for further analysis. There was no statistically significant difference between students of low-responder and high-responder schools regarding the proportion of students eligible for free or reduced price lunches. In the rural school districts, the response rate was 81% (n = 964). For both populations, the most common unanswered questions were sex and insurance type. The demographic characteristics of the 2 groups are depicted in Table 1. Age and sex distributions were similar between groups. Consistent with the demographic makeup of the school districts, most respondents were black, with 3,611 of 5,412 (66.7%) from the LRSD and 818 of 964 (84.9%) from the rural school districts (P <.001). Government-issued insurance was more common in rural children, with 77.9% of rural children having Medicaid or Arkansas’ State Children’s Health Insurance Program compared with 37.2% of urban children (P <.001).
Table 1.
Demographic Information by Urban vs Rural School Districta
| Demographics | Urban district (n 5,412) |
Rural districts (n 964) |
|---|---|---|
| Age, mean (SD), y | 9.3(2.8) | 10.3 (3.8) |
| Sex, No. (%) | ||
| Male | 2,428 (44.9) | 402 (41.7) |
| Missing/declined | 96 (1.8) | 80 (8.3) |
| Race, No. (%) | ||
| Whiteb | 1,235 (22.8) | 45 (4.7) |
| Blackb | 3,611 (66.7) | 818 (84.9) |
| Other | 408 (7.5) | 32 (3.3) |
| Missing/declined | 158 (2.9) | 39 (4.0) |
| Insurance, No. | ||
| (%) | ||
| Private | 1,888 (34.9) | 53 (5.5) |
| Medicaid | 1,604 (29.6) | 252 (26.1) |
| ARKidsb | 414 (7.6) | 499 (51.8) |
| Uninsured | 316 (5.8) | 39 (4.0) |
| Missing/declined | 1,190 (22.0) | 121 (12.6) |
Abbreviation: ARKids, Arkansas’ State Children’s Health Insurance Program.
Data are missing for some participants.
P <.001.
Morbidity Comparisons Between the Urban and Rural Groups
When the 2 groups were compared for markers of asthma morbidity, the parents of rural children reported significantly more symptoms than did the urban parents. Rural children were more likely to report recurrent trouble breathing (OR, 1.9; 95% CI, 1.5–2.2), recurrent cough (OR, 2.2; 95% CI, 1.9–2.6), recurrent chest tightness (OR, 1.8; 95% CI, 1.5–2.2), and repeated episodes of bronchitis (OR, 2.2; 95% CI, 1.7–2.8) during the preceding 2 years. Rural children were more likely to report missing 5 or more school days due to asthma in the previous school year (OR, 1.3; 95% CI, 1.2–1.5), exercise limitations (OR, 1.8; 95% CI, 1.5–2.0), and rescue medication use at least 2 days per week (OR, 1.3; 95% CI, 1.1–1.5). Nocturnal symptoms 1 or more nights per week and daytime symptoms 2 or more days per week were more commonly reported by rural parents (P < .001) (data not shown); however, there were no significant differences in emergency department visits or hospitalizations between the urban and rural groups. Except for rescue medication use, these findings remained statistically significant in a multivariate regression analysis controlling for age, sex, race, and insurance type.
Racial Comparisons Between the Urban and Rural Groups
The data were analyzed to compare overall provider diagnosis of asthma and markers of asthma morbidity between the urban and rural groups by race. There were no differences in provider diagnosis between the urban (20%) and rural (19%) groups. When race was considered, no statistically significant difference in provider-diagnosed asthma was found between urban and rural white children; however, urban black children were more likely to be diagnosed as having asthma by their provider than were rural black children (22.8% vs 19.1%, P =.02). Although the provider-diagnosed asthma prevalence was lower in rural black children compared with urban black children, morbidity markers, including recurrent breathing problems, recurrent cough, missed school days, exercise limitations, and rescue asthma medication use, were significantly higher in the rural black group (P < .001). Similarly, rural white children reported significantly more asthma morbidity compared with urban white children and were more likely to report having frequent daytime and nighttime symptoms, repeated episodes of coughing, exercise-induced symptoms, and more missed school days (P < .001). There was no statistically significant difference between urban and rural white children for rescue medication use or health care utilization.
Comparison of Algorithm- and Provider-Diagnosed Asthma and Asthma Risk
In addition to identifying children with a provider diagnosis of asthma, survey responses were used to identify undiagnosed children at risk for asthma. At-risk children were identified using a validated asthma algorithm11 based on frequency of symptoms, rescue medication use, and activity limitations. Provider-diagnosed asthma was similar in the rural and urban groups (19% vs 20%); however, rural children were more likely to report provider-diagnosed chronic bronchitis (7% vs 2%; P < .001) (Fig 2A). In the urban group, 1,333 of 5,412 children (24.6%) were classified as being at risk due to a provider diagnosis or algorithm-based identification compared with 268 of 964 rural children (27.8%) (Fig 2 A). Children at risk were classified as having intermittent or persistent asthma. Of those meeting the persistent asthma criteria, 873 of 1,333 urban children (65.5%) and 145 of 268 rural children (54.1%) were classified as having mild asthma (P < .001), whereas 460 of 1,333 urban children (34.5%) and 123 and 268 rural children (45.9%) were classified as having moderate to severe asthma (P < .001) (Fig 2B).
Figure 2.
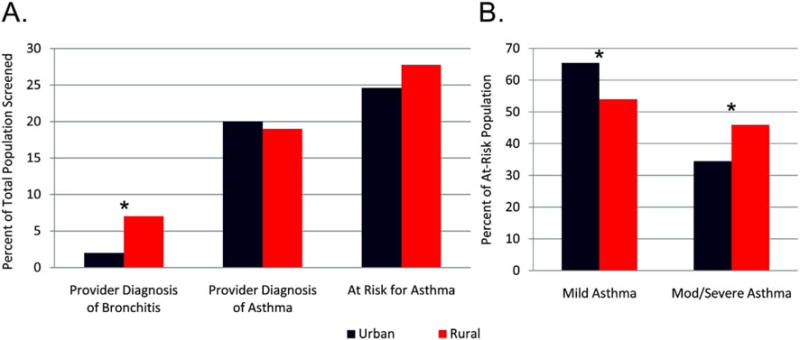
A, Comparison of provider-diagnosed chronic bronchitis, provider-diagnosed asthma, and at-risk children in urban and rural settings. B, Asthma severity in at-risk urban and rural children. *P < .001.
At-risk children in both groups were compared for health care utilization, school days missed, and rescue medication use. At-risk urban children were more likely to have more than 1 hospitalization or emergency department visit in the preceding 2 years (25.0% vs 20.9%, P = .04), but at-risk rural children were more likely to miss 5 or more days from school per year due to asthma-related symptoms (19% vs 16%, P = .03). At-risk rural children were also more likely to report rescue medication use 2 or more days per week (24% vs 16%), but the difference was not statistically significant.
DISCUSSION
In the present study, we compared the prevalence of asthma (diagnosed by a provider or identified using an algorithm), asthma morbidity, and asthma severity between rural and urban schoolchildren in Arkansas using a validated asthma screening survey and an asthma identification algorithm.11,13 These findings revealed a higher percentage of parents reporting an asthma diagnosis than did previously published national data,1,15 with at least 19% of both populations reporting physician-diagnosed asthma. Compared with urban children, rural children in the Arkansas Delta region had a similar prevalence of physician-diagnosed asthma and significantly higher prevalences of chronic bronchitis and uncontrolled asthma symptoms. Rural children were more likely to fit the criteria for moderate to severe persistent asthma. These findings suggest that asthma may be underdiagnosed or inadequately treated in the rural population. This study also establishes the need for enhanced strategies to improve asthma management for rural children, particularly those living in medically underserved communities, such as the Delta region of Arkansas.
Most research focusing on asthma prevalence in rural children has been conducted outside the United States.16–18 Findings from key international studies16–20 have suggested a protective link between livestock farm animal exposure and atopy, thought to be at least in part due to early endotoxin exposure. Few studies have been conducted in rural US populations, and those published to date have produced varied results. Chrischilles et al21 found that children living in rural farm communities in Iowa were less likely to wheeze compared with those in nearby towns. Similar findings were reported by Adler et al,22 who showed that children raised in a US farming environment were less likely to wheeze or to be diagnosed as having asthma than were non–farm-reared children. However, a study by Merchant et al23 revealed that agricultural-farming rural areas did not have the same protective benefits on asthma or other atopic diseases as reported in livestock farming environments. Similarly, the present study demonstrates that an agricultural-farming rural environment is not protective in terms of asthma diagnosis or symptoms due to asthma.
Rural children in the Arkansas Delta region were less likely to have a physician diagnosis of asthma compared with urban children, yet rural children reported significantly more asthma morbidity. In fact, these data suggest that children living in the rural Arkansas Delta region have more severe or more poorly controlled asthma symptoms compared with children living in an urban region of the state. One likely contributing factor to these findings is the large proportion of minority children in the rural Delta region compared with previous rural asthma studies. Increased asthma burden has been previously reported in predominantly black populations living in urban regions24; therefore, the present findings might reflect a similar pattern of increased asthma burden in a predominantly black population living in a rural environment. Rural white children reported more asthma morbidity compared with urban white children, and asthma morbidity markers remained statistically higher in rural children after controlling for race in multivariate analysis, suggesting that these findings were not solely due to race.
The large number of children living at or below the poverty level is likely another key contributing factor to these findings. The US Census Bureau data25 for the Arkansas Delta region suggest that it is one of the most impoverished regions in the nation. Data on family income and maternal education were not obtained in the present study, so insurance status was used as a proxy for socioeconomic status. Significantly more children in the rural group had government-issued medical insurance, suggesting a lower-income status in the rural group. As past studies have shown, minority children living at or below the poverty level have higher asthma prevalence and increased asthma-related morbidity26; therefore, differences in socioeconomic status may be an important factor in the increased asthma burden in the rural Delta population. Higgins et al27 examined asthma severity in nonfarming rural and urban children in Connecticut. In that study, low-income minority children, especially black children, were at increased risk for severe asthma regardless of geographic location. The present study revealed that a predominantly black, low-income population of rural children had a higher prevalence of moderate to severe asthma compared with urban children, supporting the concept that children with risk factors such as low socioeconomic and minority status may be at increased risk for more severe asthma regardless of geographic location.
Increased asthma morbidity in the rural group remained statistically significant in multivariate analysis after controlling for race, age, sex, and insurance status, suggesting that other factors may be important in increased asthma morbidity in the rural group. Barriers to health care can be significant for rural children.28,29 Many families living in rural areas have to travel long distances to access pediatric health care services, and they may not have adequate access to subspecialty providers or emergency health care services. These barriers to care can lead to failure to properly diagnosis asthma and subsequent lack of proper treatment. We found that emergency health care utilization (emergency department visits and hospitalizations) was not statistically significantly different between groups. This is an important finding in terms of health care costs because rural children invariably have less convenient access to these services and are more likely to have increased costs associated with transportation, lodging, or both. Despite the presumed increased financial burden, rural children were just as likely to use emergency health care services as were urban children. This suggests that rural children have comparable, or possibly increased, levels of asthma severity compared with urban children.
The strengths of this study include the large population size and the high response rate. Also, the demographic makeup of the survey respondents was similar to that of the school districts. There are several limitations of this study as well. Using a parental survey may have introduced selection bias, and parents of children with asthma may have been more apt to participate than others. Also, the survey asked symptom recall during the past 8 weeks and health care utilization recall across a 2-year period, which may have led to inaccurate reporting of symptoms by some participants. The surveys were conducted 3 years apart in the urban vs rural areas, and it is possible that the prevalence of asthma in rural children was inflated by the later survey. However, there is no evidence that Arkansas experienced a change in childhood asthma prevalence during this time frame, and, in fact, national data suggest that a plateau in overall asthma prevalence occurred in all ages of children during 2001 to 2004.30 Also, the survey did not include questions about other factors that may have contributed to differences in asthma morbidity, such as environmental triggers, exposure to farm animals, barriers to health care utilization, and parental employment and education.
This study reveals significant asthma-related morbidity in 2 distinct pediatric populations in Arkansas. Rural children were at increased risk for uncontrolled asthma compared with their urban counterparts. Although findings might be related to barriers to health care access and subsequent inadequate medication use, the prevalence of asthma and symptoms consistent with persistent asthma is compelling. These findings suggest that not all rural environments are protective against atopic disorders such as asthma and warrant further investigation of the impact of environmental and socio-demographic factors on high-risk rural children. In addition, innovative interventions aimed at meeting the needs of rural children need to be developed. Interventions developed for at-risk inner-city children, such as in-home case management and individualized home allergen reduction, cannot be easily applied to rural regions with a low population density such as the Arkansas Delta region. The specific challenges to providing care and implementing interventions for children in a rural and underserved region must be considered to reduce the significant asthma burden.
Acknowledgments
We thank Phaedra Yount for her technical assistance and editorial comments and Rita Brown and Debra Watkins, research coordinators, for their hard work and efforts in support of the study.
Funding Sources:
This study was supported by the University of Arkansas for Medical Sciences Dean’s Research Development Fund; grant N01-HO-99230 from the National Institutes of Health-National Heart, Lung, and Blood Institute; and the Arkansas Biosciences Institute.
Footnotes
Disclosures
Authors have nothing to disclose.
References
- 1.Akinbami L. The state of childhood asthma, United States, 1980–2005. Adv Data. 2006;381:1–24. [PubMed] [Google Scholar]
- 2.American Lung Association. Trends in Asthma Morbidity and Mortality. Washington, DC: American Lung Association Epidemiology and Statistics Unit, Research and Program Services; 2007. [Google Scholar]
- 3.Akinbami LJ, Rhodes JC, Lara M. Racial and ethnic differences in asthma diagnosis among children who wheeze. Pediatrics. 2005;115:1254–1260. doi: 10.1542/peds.2004-0897. [DOI] [PubMed] [Google Scholar]
- 4.McDaniel M, Paxson C, Waldfogel J. Racial disparities in childhood asthma in the United States: evidence from the National Health Interview Survey, 1997 to 2003. Pediatrics. 2006;117:e868–e877. doi: 10.1542/peds.2005-1721. [DOI] [PubMed] [Google Scholar]
- 5.Quinn K, Shalowitz MU, Berry CA, et al. Racial and ethnic disparities in diagnosed and possible undiagnosed asthma among public-school children in Chicago. Am J Public Health. 2006;96:1599–1603. doi: 10.2105/AJPH.2005.071514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crain EF, Weiss KB, Bijur PE, et al. An estimate of the prevalence of asthma and wheezing among inner-city children. Pediatrics. 1994;94:356–362. [PubMed] [Google Scholar]
- 7.Perry TT, Vargas PA, McCracken A, Jones SM. Underdiagnosed and uncontrolled asthma: findings in rural schoolchildren from the Delta region of Arkansas. Ann Allergy Asthma Immunol. 2008;101:375–381. doi: 10.1016/S1081-1206(10)60313-4. [DOI] [PubMed] [Google Scholar]
- 8.Ownby DR. Asthma in rural America. Ann Allergy Asthma Immunol. 2005;95(suppl 1):S17–S22. doi: 10.1016/s1081-1206(10)61005-8. [DOI] [PubMed] [Google Scholar]
- 9.US Census Bureau. Census 2000 urban and rural classification. http://www.census.gov/geo/www/ua/ua_2k.html. Accessed May 6, 2005.
- 10.Arkansas Department of Education Website. http://www.arkansased.org. Accessed May 6, 2005.
- 11.Jones CA, Morphew T, Clement LT, et al. A school-based case identification process for identifying inner city children with asthma: the Breathmobile program. Chest. 2004;125:924–934. doi: 10.1378/chest.125.3.924. [DOI] [PubMed] [Google Scholar]
- 12.Vargas PA, Simpson PM, Bushmiaer M, et al. Symptom profile and asthma control in school-aged children. Ann Allergy Asthma Immunol. 2006;96:787–793. doi: 10.1016/S1081-1206(10)61340-3. [DOI] [PubMed] [Google Scholar]
- 13.Kachru R, Morphew T, Kehl S, et al. Validation of a single survey that can be used for case identification and assessment of asthma control: the Breathmobile Program. Ann Allergy Asthma Immunol. 2006;97:775–783. doi: 10.1016/S1081-1206(10)60969-6. [DOI] [PubMed] [Google Scholar]
- 14.National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: National Heart, Lung, and Blood Institute; 2007. [Google Scholar]
- 15.Akinbami LJ, Schoendorf KC, Parker J. US childhood asthma prevalence estimates: the impact of the 1997 National Health Interview Survey redesign. Am J Epidemiol. 2003;158:99–104. doi: 10.1093/aje/kwg109. [DOI] [PubMed] [Google Scholar]
- 16.Eder W, von Mutius E. Hygiene hypothesis and endotoxin: what is the evidence? Curr Opin Allergy Clin Immunol. 2004;4:113–117. doi: 10.1097/00130832-200404000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Braun-Fahrlander C, Riedler J, Herz U, et al. Environmental exposure to endotoxin and its relation to asthma in school-age children. N Engl J Med. 2002;347:869–877. doi: 10.1056/NEJMoa020057. [DOI] [PubMed] [Google Scholar]
- 18.Waser M, Schierl R, von Mutius E, et al. Determinants of endotoxin levels in living environments of farmers’ children and their peers from rural areas. Clin Exp Allergy. 2004;34:389–397. doi: 10.1111/j.1365-2222.2004.01873.x. [DOI] [PubMed] [Google Scholar]
- 19.Eduard W, Douwes J, Omenaas E, Heederik D. Do farming exposures cause or prevent asthma? results from a study of adult Norwegian farmers. Thorax. 2004;59:381–386. doi: 10.1136/thx.2004.013326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Douwes J, Travier N, Huang K, et al. Lifelong farm exposure may strongly reduce the risk of asthma in adults. Allergy. 2007;62:1158–1165. doi: 10.1111/j.1398-9995.2007.01490.x. [DOI] [PubMed] [Google Scholar]
- 21.Chrischilles E, Ahrens R, Kuehl A, et al. Asthma prevalence and morbidity among rural Iowa schoolchildren. J Allergy Clin Immunol. 2004;113:66–71. doi: 10.1016/j.jaci.2003.09.037. [DOI] [PubMed] [Google Scholar]
- 22.Adler A, Tager I, Quintero DR. Decreased prevalence of asthma among farm-reared children compared with those who are rural but not farm-reared. J Allergy Clin Immunol. 2005;115:67–73. doi: 10.1016/j.jaci.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 23.Merchant JA, Naleway AL, Svendsen ER, et al. Asthma and farm exposures in a cohort of rural Iowa children. Environ Health Perspect. 2005;113:350–356. doi: 10.1289/ehp.7240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Persky VW, Slezak J, Contreras A, et al. Relationships of race and socioeconomic status with prevalence, severity, and symptoms of asthma in Chicago school children. Ann Allergy Asthma Immunol. 1998;81:266–271. doi: 10.1016/S1081-1206(10)62824-4. [DOI] [PubMed] [Google Scholar]
- 25.US Census Bureau. Small Area Income and Poverty Estimates. Washington, DC: US Census Bureau; 2005. [Google Scholar]
- 26.Lieu TA, Lozano P, Finkelstein JA, et al. Racial/ethnic variation in asthma status and management practices among children in managed Medicaid. Pediatrics. 2002;109:857–865. doi: 10.1542/peds.109.5.857. [DOI] [PubMed] [Google Scholar]
- 27.Higgins PS, Wakefield D, Cloutier MM. Risk factors for asthma and asthma severity in nonurban children in Connecticut. Chest. 2005;128:3846–3853. doi: 10.1378/chest.128.6.3846. [DOI] [PubMed] [Google Scholar]
- 28.Skinner AC, Slifkin RT. Rural/urban differences in barriers to and burden of care for children with special health care needs. J Rural Health. 2007;23:150–157. doi: 10.1111/j.1748-0361.2007.00082.x. [DOI] [PubMed] [Google Scholar]
- 29.Valet RS, Perry TT, Hartert TV. Rural health disparities in asthma care and outcomes. J Allergy Clin Immunol. 2009;123:1220–1225. doi: 10.1016/j.jaci.2008.12.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moorman JE, Rudd RA, Johnson CA, et al. National surveillance for asthma–United States, 1980–2004. MMWR Surveill Summ. 2007;56:1–54. [PubMed] [Google Scholar]


