Abstract
With support from the U.S. President’s Emergency Plan for AIDS Relief and the global fund for HIV, tuberculosis, and malaria, Nigeria offers free services for prevention of mother-to-child transmission of HIV. However, uptake of these services is low, and pediatric transmission of HIV remains a significant public health challenge. Using the PEN-3 cultural model as the theoretical framework, we examined social, cultural, and contextual factors that influenced uptake of HIV counseling and testing among pregnant women and their male partners. This was a qualitative study of participants in the Healthy Beginning Initiative (HBI), a congregation-based program to prevent mother-to-child transmission of HIV in Enugu, southeast Nigeria. We conducted eight focus group discussion sessions with 83 pregnant women and their male partners. Participants’ perspectives on why they did or did not test for HIV were obtained. The most cited reasons for getting tested for HIV included the following: “the need to know one’s status”, “the role of prenatal testing” (positive perceptions); “the role of the church”, “personal rapport with healthcare worker” (positive enablers); and the “influence of marriage” (positive nurturer). The most cited reason for not testing were: “fear of HIV test”, “shame associated with HIV+ test results”, “conspiratorial beliefs about HIV testing” (negative perceptions); “lack of confidentiality with HIV testing”, (negative enabler); and “HIV-related stigma from family and community systems” (negative nurturer). Overall, numerous facilitators and barriers influence uptake of HIV testing in the study setting. Public health practitioners and policymakers need to consider how sociocultural and religious factors unique to specific local contexts may promote or hinder uptake of available HIV/AIDS prevention and care interventions.
Keywords: HIV testing, determinants of HIV testing, prevention of mother-to-child transmission, PEN-3 cultural model, sub-Saharan Africa, HIV or AIDS
Introduction
Although mother-to-child transmission (MTCT) of HIV has almost been eliminated in many high-income countries, MTCT remains an important source of new HIV infections in sub-Saharan Africa.1 According to the 2014 report of the Joint United Nations Program on HIV/AIDS, sub-Saharan Africa accounted for 87% of the 1.5 million pregnant women living with HIV and 91% of children living with HIV worldwide. 1 Despite improved effort and the availability of simple, relatively inexpensive, and highly effective antiretroviral therapy for preventing mother-to-child transmission of HIV (PMTCT), 32% of these pregnant women did not receive services for PMTCT, resulting in an estimated 210,000 new infections in children.1
Nigeria has an estimated population of 180 million people, of which 3.2 million are living with HIV, representing 9% of the global HIV burden.2 Awareness of HIV/AIDS is almost universal among women and men in both urban and rural areas of Nigeria.3 However, according to the Nigerian National Agency for the Control of AIDS, 40% of these people do not know their HIV status and may continue to infect others unknowingly.4 Findings from the 2013 Nigerian Demographic Health Survey reported that, although 60% of women and 71% of men knew where to get an HIV test, 70% of women and 78% of men had never been tested.3 Furthermore, only 10% of the men and women who had been tested in 2013 received their test results.3 Previous studies conducted in Nigeria, Kenya, South Africa, and other African countries have reported that lack of access to testing, fear of discovery, not knowing where to test, and lack of access to treatment are key reasons for not getting tested.5–7 A lack of resources for HIV testing and counseling at convenient locations and hours of operation have been reported as factors leading to ambivalence about HIV testing.7–10
The Healthy Beginning Initiative (HBI) funded by the National Institutes of Health was designed to address barriers to HIV testing for pregnant women and their male partners.11 Working with priests and trained church health advisors, HBI employed prayer sessions held each Sunday in 20 intervention churches in Enugu, southeast Nigeria, to recruit pregnant women and their partners. Baby showers held one Sunday each month for the participating pregnant women were used to deliver the intervention (education in PMTCT), and free, on-site and integrated testing (HIV, sickle cell genotype, and hepatitis B) rather than HIV-only testing (aimed at reducing access barriers and cost and at addressing stigma).12 Culturally appropriate baby receptions integrated into traditional family and community celebrations of child birth were used to encourage postdelivery follow-up and care. HBI in intervention churches was led by lay church health advisors. Pregnant women and their male partners in 20 control churches received usual care (i.e., referral to a health facility). 11 An analysis of HBI data showed that HIV testing rate among pregnant women in the intervention group was 91.92% compared to 54.61% in the control group. Compared to the national HIV testing rate of 20% among pregnant women,11 HBI was a remarkable success, underscoring the need to identify strategies for sustaining and increasing this initiative. However, while results are encouraging, discerning why some pregnant women and their male partners availed themselves of available, free testing and linkage to PMTCT care services while others did not, is crucial. The objective of this study was to understand the underlying factors that might explain why people do or do not test for HIV, even in the supportive context of HBI. Using the PEN-3 cultural model (described later) as a guide, we sought to understand these factors in a subset of HBI participants. Our major research question was “What were the specific reasons why pregnant women in Nigeria and their male partners tested or did not test for HIV?”
Theoretical Framework
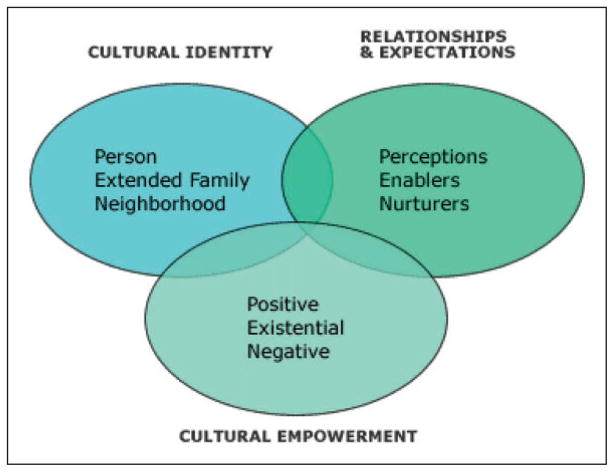
Using the PEN-3 cultural model as our theoretical foundation (Figure 1), we explored local perceptions on why men and women tested or did not test for HIV. Developed by Airhihenbuwa and his colleagues,13–15 the PEN-3 model emphasizes and examines cultural beliefs and practices which influence health behaviors that should be acknowledged, encouraged or discouraged.15 It consists of three domains: (a) cultural identity, (b) relations and expectations, and (c) cultural empowerment.14,16 Cultural Identity challenges the assumption that all interventions should be focused on the individual, broadening the intervention focus to incorporate immediate and extended family members and community contexts.17 Relationships and Expectations posits that health-behavior interpretations are based on people’s perceptions of behaviors, resources and institutional forces that enable or hinder these behaviors; and the influence of family, kin, friends, and culture that nurture these behaviors.14,15,17 Within the Cultural Empowerment domain, factors that are critical to health-behavior change are evaluated for attributes that are positive, existential, and negative.14,17 While positive factors include values and relationships that promote the health behavior of interest, existential factors include cultural health beliefs and practices that are unique or indigenous to a group.14 Finally, negative aspects include health beliefs and actions that are harmful.14 Of particular interest to this study is the cultural empowerment domain, which we used to identify factors behind choosing whether to test for HIV.
Figure 1.
Illustration of the PEN-3 model.
Design and Methods
Data for this study were derived using focus group sessions with a purposive sample of HBI participants to explore their perceptions around barriers to and enablers of, HIV testing among pregnant women and their partners. Focus groups facilitated open discussions18,19 and provided the opportunity to elaborate on comments made by other group members. It also helped to achieve a deeper understanding of the role of culture in couple’s uptake of prenatal HIV screening. The focus group sessions were gender sensitive (i.e., separate male and female). This approach reduced the fear of repercussions from the opposite sex. Participants were recruited and interviewed by trained HBI staff. All of those who were approached to participate agreed and provided written and verbal consent. The same staff, with the aid of the lead authors, conducted the focus group discussions. Focus group sessions varied in size from 8 to 12 participants, and eight sessions were conducted— four male and four female. Participants were probed on their own HIV testing experiences, including factors they perceived to be enablers or barriers. The study was approved by the Institutional Review Board of the University of Nevada, Reno and the Nigerian National Health Research Ethics Committee.
Setting
The study was conducted in Enugu, southeast Nigeria, which is inhabited predominantly by the Igbo ethnic group. Although language and culture appear to be the main unifying factors among the Igbos, there is widespread practice of Christianity, with church attendance approaching 90%.11 In addition, marriage is vastly important to the Igbos, perceived as ensuring the continuation of already existing links,20–22 generally monogamous, and involving parents and kin centrally in traditional marriage negotiations.20 Church weddings, which affix a Christian stamp to a union, are common and coexist with traditional Igbo marriage practices. 20 These key characteristics were central in the development of HBI.
Participants
A purposive sampling approach was used to recruit participants in the intervention and control arm of HBI and to ensure a heterogeneous participant population. Using this approach, we recruited participants of varying sociodemographic backgrounds (e.g., age, occupation, education, income, urban vs. rural residence, primigravidas vs. multiparous women, etc.).
Development of the Focus Group Guide
The questions for the focus group discussions were developed using the three domains and nine constructs of the PEN-3 cultural model (see Table 1). The questions were designed to be open ended and included items that incorporated cultural identity (i.e., factors at the individual, family or community level that influenced HIV testing), relationships and expectations (perceptions about HIV testing in general, including the role of family or health-care setting in influencing HIV testing), and cultural empowerment (i.e., the role of the church-based HBI in influencing HIV testing). The questions explored beliefs and attitudinal variables that promote or hinder HIV testing. Overall, these questions where designed to allow participants to explore individual, family, community, and structural factors that influence HIV testing while encouraging discussions of how culture may influence HIV testing behavior.
Table 1.
Focus Group Guide.
| Perceptions of HIV test focus group topics and sample questions guided by PEN-3 |
|---|
Cultural identity (person, extended family, neighbor-community (church) context)
|
Focus Group Procedure
The focus groups sessions were conducted between March and April, 2015. Informed consent was obtained prior to conducting the focus group sessions. During informed consent, the rationale for the study was explained to potential respondents (in the local language, Igbo), and their voluntary participation was sought. All respondents were informed that their participation was voluntary, and that if they chose not to participate, they would not lose any benefits from their health facility. They were also informed of their right to withdraw from the study at any time. Those who volunteered to participate in the study were asked to sign the inform consent form. Participants who could not read or write were asked to give their thumbprint as a confirmation of their consent. Thus, participation in the study was entirely voluntary, and no incentives were provided to respondents. Respondents were assured of confidentiality, and only study unique identification numbers were used. Each focus group session lasted about 2 hours. The group sessions were digitally recorded with the participants’ consent. Two staff members from the HBI trial (one for male participants, one for female participants) who were experienced in facilitating focus groups sessions moderated the sessions. Moderators followed the focus group guide and used additional probing questions as necessary. The group sessions were conducted in a private conference room of the HBI initiative.
Data Analysis
The focus groups in Igbo were transcribed and translated into English by native speakers prior to data analysis. We followed the analytic process as outlined by Strauss, Corbin, and Kendall23–25 for open, axial, and selective coding. All the data from the focus group discussions were analyzed manually, first using open line-by-line coding of the textual data (i.e., focus group transcripts). This involved each author reading and rereading all the focus group transcripts independently, then meeting to discuss them, noting any patterns and sharing reflections. This enabled us to establish initial descriptive codes while highlighting emerging relationships across transcripts.26 Next, we performed axial coding, in which we combined similar codes into higher order categories. We merged all higher codes and grouped and arranged them based on parallels and connections across the transcripts. Then by systematically relating the high-order categories next to each other, selective coding was used to explain patterns in the data and to identify a core category, which in this analysis was identified as a core theoretical variable. Theoretical saturation in data analysis was reached by consensus when the core theoretical variable was explained, and data no longer yielded new information pertinent to the generation of the theory.23 We used several techniques to maintain quality and rigor. First, two researchers independently completed both open and axial coding before meeting with the group for discussions and modification or additions where necessary. Next, we maintained a detailed audit trail that included memos and notes from the focus group discussions, meeting notes, and field notes throughout the data collection and analysis process. Member checks were used to enhance the reliability, while data confirmability by multiple researchers and researcher consensus of the similarities and differences in data coding through open dialog ensured trustworthiness of the data.27
Findings
A total of 83 individuals participated in the study—38 males (45%) and 45 females (54%). Mean age of the participants was 35.6 years (SD=9.09); 25 participants (38%) had primary school education, 38 (45%) had secondary education, and 20 (24%) completed tertiary level education. The majority of the participants (53; 63%) lived in a rural region. Data are presented below for the themes generated from the focus groups which together illustrate how participants perceived multiple factors (both positive and negative) influence HIV testing behaviors in Nigeria (Table 2).
Table 2.
Themes Generated Using PEN-3 Cultural Model as a Guide.
| Positive | Negative | |
|---|---|---|
| Perceptions |
|
|
| Enablers |
|
|
| Nurturers |
|
|
Positive Perceptions
The need to know one’s status
In the focus group discussions, one of the factors that widely facilitated HIV testing as noted by participants is the need for one to know one’s sero-status. Majority of our participants perceived HIV testing as a good thing, stating that it enabled them to know firsthand “whether they were positive or negative.” One female respondent stated that “you may not know you have it till you test.” A male participant stated that “it is good to test for HIV, as it helps you to know your status. Some may be positive without knowing it.” Another male participant stated that “the virus has killed many people in any village, many people thought they were poisoned, but now, testing has helped to discover and treat the virus.”
The need to start antiretroviral treatment if positive was salient among participants with influencing decisions to know one’s status. Indeed, there was a general consensus that having knowledge of one’s status was beneficial even if the test was positive because of the availability of treatment. One woman stated that “knowledge of status enables one to start treatment early if positive.” The same sentiment was echoed by a male participant who stated the following: “It is good that everyone does HIV testing because without this test, many people would have died. Testing helps to know when to start treatment.” We found similar perceptions with knowledge of HIV status in cases where test results may be negative. One female participant noted that awareness of HIV status was also important particularly for people whose test results were negative as it “enables one to be careful . . . so as to avoid occasions and things that would lead one to contract HIV.” Another female participant stated that it “allowed people to be confident in themselves because they are free from HIV.” One female participant was of the opinion that “if one tested negative, it will enable them to try to maintain their healthy status, but if positive, it will enable them to start taking their medication, in order to prolong life.” Another reason why knowledge of status was important as elaborated by a male participant was that “by knowing your status, the spread of HIV can be controlled and not transmitted to others.”
The role of prenatal testing
HIV testing was important as noted by participants not only for knowledge of status but also in the case of pregnant women, to prevent transmission of HIV to unborn children. Because Nigeria has the highest number of MTCT of HIV in sub-Saharan Africa,1 many participants stated that HIV testing has become a part of routine prenatal care in the country. One woman noted that “the test is required for all pregnant women.” Another woman stated that “the reason why I tested was to protect my unborn baby.” Participants’ perceptions also echoed language that mirrors what they may have heard in the clinic or radio in reference to HIV testing. For example, one female participant stated that testing for HIV facilitated having a HIV-free baby. Another female participant stated that it ensures that “pregnant women will know when to begin to treat baby in the womb early if HIV positive.” Male participants were of the opinion that “routine HIV testing during prenatal care mattered not only for healthy babies but also to ensure that these babies were born without any challenges.” One woman shared that “a pregnant woman [I knew] was sick, after testing, she found out that she had the virus, got into care and had a healthy baby.” Many participants knew that HIV could be transmitted from mother to child during pregnancy and understood that prenatal HIV testing and uptake of treatment could prevent transmission. Women also recognized that even if they did test positive, they could still have healthy children if they followed through with the appropriate medical care.
Negative Perceptions
The role of fear of HIV testing
Majority of our participants were of the opinion that the primary reasons why people do not test for HIV was fear, particularly fear of the unknown, fear of HIV positive results, fear of needles, and collection of blood samples in some cases. In terms of fear of the unknown, one female participant stated the following: “People are afraid to test because they believe that when they contract the disease they will die, so they will rather not know their status.” There was an overall perception from female participants that “fear is a result of thinking that all hope is lost and if one discovers that they are positive they think they will die today or tomorrow.” One female participant stated that “people are afraid to test because they don’t want to die.” Also, another explained that “people do not want to test because rather than hearing they are HIV positive, they would prefer to die and not know their status.” Yet, another female participant indicated that “fear comes to mind because people are preoccupied with thoughts on what will happen if they are positive?” A similar sentiment was echoed by another female participant who stated that “fear of knowledge of status is enough reason not to want to perform the test.” While another participant stated that “the fear that one may already be infected influences decision to not want to know their status.”
Male participants shared the same views in reference to not testing as a result of fear of death if status is positive. One male participant indicated that “a positive result may force some to kill themselves, so they would rather not test.” Coupled with general fear of losing hope in life as a result of HIV testing, another reason why some people are afraid of testing is because of the risky behaviors they engage in. One male participant noted that “out of phobia (fear) some people refuse to test for HIV because of their lifestyle and fear of past risky behaviors.” Another stated that this fear also is a result of the costs associated with treatment. However a general perception shared by participants was the fear of the HIV test itself, particularly the needle used for the test and objections toward collection of blood samples. One female participant stated that “people do not test out of fear of contracting HIV through infected needles.”
The role of shame and HIV testing
In addition to fear and stigma, perceptions of shame were cited as a common reason why people choose not to test for HIV. Participants suggested that because HIV remains so stigmatized, it was not uncommon for people to feel ashamed of being seen as a HIV carrier. One female participant noted that “some men and women do not want to test out of shame because people may use them as caricature.” The “shame associated with being positive” and the potential for “perceived laughter due to a sero-positive status” are among the negative consequences cited for refusal to test for HIV. Available evidence has also shown that HIV/AIDS in sub-Saharan Africa has grown to become an epidemic that affects the family as a functioning system, threatening its supportive capacity, and redefining the manner of coping and adapting to the burden of a disease.28 Nowhere is this more evident than in decisions to participate in routine testing for HIV. One male participant noted that “people do not test because they want to avoid putting their family to shame if the result is positive. In fact, they would prefer to die rather than bring their family to disrepute.” Another male participant noted that “people would feel embarrassed if they tested positive for HIV, and know that it may lead to divorce or separation of the family, and so they would choose not to test.”
Conspiratorial beliefs about HIV testing
A male participant was of the opinion that “many people in the rural villages do not test because they do not know the final destination of their blood sample.” Another explained: “People are suspicious of what people are trying to do with their blood hence their fear of participating in routine testing for HIV.” A female participant stated that “the fear of depletion of their blood, even fear on whether their blood is being sold and thoughts regarding whether it is being used for rituals are among the reasons why people do not test for HIV.”
Positive Enablers
The role of the church in HIV testing
With church attendance among people in Enugu close to 90%, it is not surprising that the church plays an important role in influencing HIV testing. One male participant noted that “the church demands HIV test before wedding/marriage.” A female participant stated that “people test for the sake of marriage within the church.” Another stated that it is because of “encouragement from the priest.” Discussions on these mandatory requirements from the church for HIV testing prior to wedding or marriage resulted in the following response by a male participant: “Our people are happy about it, and they have no problem with it because they all know that it is the right thing to do and they must do it to get married in the church.” Another male participant stated that “our ministers and priests should be encouraged to even include the HIV counseling in their sermons.” Another stated that:
“people should contact their priests, because they are unbiased and would tell the truth; part of their call to duty is to save lives. If they have the opportunity to save lives by encouraging HIV testing, it’s part of their duty”.
One male participant, in explaining why people test for HIV, stated the following: “It’s because of marriage counseling and advice from the church. It enables couples to receive guidance on how they can have HIV-free children.”
Personal rapport with health-care workers
In elaborating the benefits of HIV testing as it relates to facilitating knowledge of one’s status, one male participant mentioned that he actually asked a doctor friend of his indirectly about HIV prior to testing. He stated the following: “The doctor explained everything about HIV to me, including information on medicines that one can take if positive. The way he explained it all to me helped me decide to go for the test.” Thus, presenting information and options in accessible ways through trusted health-care providers could potentially facilitate testing.
Negative Enabler
Lack of confidentiality
The uptake of HIV testing is not without barriers as some participant mentioned. One in particular was the lack of confidentiality in handling results of HIV tests. One female participant noted that “in some cases you may know the person administering the test and so decide not to go for the test for fear that they will disclose your results.” Another female participant shared the following: “I know a lady who tested positive in a clinic, and one of the staff from that clinic came to the lady’s office and told people. So, lack of confidentiality makes people not to test for HIV.” Especially due to the noted “shame associated with being positive,” lack of confidentiality and the idea that healthcare providers could share results with other community members is a strong deterrent against testing.
Positive Nurturer
The role of marriage in HIV testing
In describing why men and women participated in routine testing for HIV, our findings highlight the significance of marriage. One female participant stated the following: “Testing enables a woman to know her spouse’s status before accepting a marriage proposal.” Another stated that “testing is necessary for knowing your and your husband’s HIV status before marriage.” Women who tested for HIV discussed marriage as a key motivation for learning their status. A male participant stated that “new couples should test to know their status to save each other in case one of them is positive.” While another man discussed how his wife influenced him to undergo testing: “It helps the couple to know early, the effects of HIV infection. I and my wife were happy to learn that we do not have the virus. It was my wife who encouraged me to do the test.” Several participants stated that testing before marriage was beneficial to the overall health of the couple. Participants shared that testing could save lives and prevent transmission to a partner.
While marriage can be an individual affair in other contexts, among the Igbos, it is a family and community affair that also influenced uptake of HIV testing as shared by participants. 20 Thus, it was not uncommon for the family and extended family to play a role in decisions to test for HIV prior to marriage as stated by one female participant: “I didn’t want to do the test before marriage because when I looked at my spouse I believed he was negative, but his family and siblings encouraged us to go for the test.” A male participant stated the following:
“If anyone wants to come for Igba Nkwu (wine presentation ceremony as part of the Igbo traditional marriage rites), they must test for HIV. It is in our constitution now. In fact, in some cases, we even refer couples to where they should take the test as we trust the results coming from particular places. We have embedded it in our constitution that our prospective in-laws must be tested for HIV”.
When asked if this requirement has evoked any feelings from anyone in the community, the participant stated the following:
“if you really want to marry someone that you really love, nothing anyone tells you to do as regards testing will stand in the way. It is not mandatory they perform the test where we tell them to do, so we give them option. The key thing is that they get tested prior to marriage because we don’t want anything that will break up their relationship in the future particularly when it comes to sickness like HIV. We believe that HIV testing should be a precondition for marriage in our town”.
Negative Nurturer
The role of HIV-related stigma within family and community systems
In addition to fear, participants mentioned that stigma associated with HIV is a prime reason why people do not test for HIV. For example, one female participant stated that “rejection from friends and family members as a result of a positive status is a reason why some people decide not to test for HIV.” A male participant stated that in the beginning: “if you heard anyone was HIV positive, you will not come close to them or allow them to touch you and so people did not want to test because of it.” The overall perception shared by participants is that “if others know they are positive, they will be stigmatized.” One female participant noted that “the attitude towards people living with HIV, particularly in instances where they are treated as outcasts in the society, influences people’s decisions not to test for HIV.” Another shared that “my sister-in-law was positive and pregnant and was stigmatized because of her condition, and was sent back to her family after she lost the baby.” A male participant stated that “isolation from friends and relatives resulting in social stigmatization are major reasons why people do not test for HIV.” Another male participant told a story of how her own sister who tested positive for HIV and later developed AIDS was left to die in a goat shed. For some, being ostracized by family and the community due to a positive test is worse than actually having the virus, which leads them to take no action to test, treat, or even prevent further transmission if positive.
Discussion
The objective of this study was to qualitatively explore the barriers to, and facilitators of HIV testing among pregnant women and their male partners residing in southeast Nigeria. A number of important themes emerged from the focus group data that have implications for the improvement in the delivery of HIV testing interventions for individuals living in Nigeria. First, in using the PEN-3 cultural model as a guide,13,29,30 our findings highlight not only the perceptions, enablers, and nurturing factors but also the positive and negative factors that may play a role in influencing pregnant women and their male partners’ decision to test for HIV. The need to know one’s status, the role of prenatal care, the influence of the church, and the role of marriage were among the positive perceptions, enabling and nurturing factors identified to influence HIV testing. On the other hand, fear, particularly in relation to fear associated with a positive test result, feelings of shame, conspiratorial beliefs about HIV testing, lack of confidentiality, and the possibility of HIV-related stigma were cited as factors that may deter testing for HIV. The results support the importance of actively engaging individuals in open dialogs on HIV testing so as to incorporate their input into the development, implementation, or dissemination of a culturally tailored HIV testing health promotion intervention that would increase uptake of HIV testing among pregnant women and their male partners.
Second, the formal role of religion and the church and the general role of culture as it pertains to marriage were instrumental in influencing HIV testing behaviors among participants. For example, participants revealed how the church remains a significant aspect of life and played a key role in fostering decisions to test for HIV, particularly as part of requirements for exchange of marital vows. Consistent with previous research,31,32 our findings illustrate how community-based HIV programs at religious faith-based organization may potentially be an effective way to increase HIV screening among disproportionately affected populations, marginalized from mainstream health-care system. Thus, the church can be an important partner in reaching people at highest risk for HIV. Our findings illustrated how the dedication and belief systems of the church had an impact in promoting couples’ voluntary counseling and testing. As an accessible, malefriendly setting, the church can also be an important venue for addressing male partner participation in PMTCT interventions. Since churches are familiar community-based institutions, more thorough collaborations between researchers and religious faith-based organizations can contribute to increasing HIV testing among pregnant women and their male partners in Nigeria and similar low-income settings with high rates of HIV incidence and MTCT of HIV.
Participants also noted how culture as it pertains to marriage was important in influencing decisions to test for HIV. Our findings echo previous literature on the role of culture in influencing HIV testing in southeastern Nigeria.33 The influence of marriage within the Igbo culture was a positive nurturer that promoted HIV testing among couples so much so that participants indicated that HIV testing allowed couples to know their status and take appropriate measures to protect themselves. Overall, attitudes toward HIV testing were largely favorable whether for its importance within prenatal testing or for marriage. However, many participants shared how fear, conspiratorial beliefs, and stigma may deter uptake of HIV testing. These findings are consistent with previous studies conducted in other parts of sub-Saharan Africa.34 For example, in a systematic review by Musheke and colleagues,34 the authors found that maternal obligation to protect unborn child from HIV influenced uptake of HIV testing among many pregnant women in sub-Saharan Africa.
On the other hand, HIV-related stigma, the fear of social exclusion and losing social support, as well as conspiratorial beliefs about blood collection were barriers to HIV testing as noted in the systematic review.34 Other studies have shown that the fear of a positive HIV testing, or simply knowing one’s status is enough to deter pregnant women from testing for HIV.35,36 Additionally, fear of male partners’ response as well as the fear of potential stigma and violence faced at the hands of community and family members served as a deterrent. 37,38 The current study revealed examples of HIV positive individuals being isolated from their family and friends as a result of their status. Participants also discussed the role of stigmatization and fear of being treated as an outcast by the community as barriers to knowing one’s status. Such statements from participants in this study support the need for further research on the role stigma and fear may play with influencing decisions to test for HIV. A focus on elucidating the role of HIV stigma in decision making surrounding HIV testing among pregnant women and their male partners is a valuable direction for future research.
Implications for Practice
At the individual level, because HIV testing is key to improving health outcomes, there is a need to minimize or reduce the fear that individuals may have toward HIV testing using culturally appropriate frameworks that encourage open discussions. To do so requires engaging in dialog with individuals by listening to the taken-for-granted assumptions people may have about HIV testing – whether positive or negative, or whether these perceptions are influenced by health-care systems or family systems. Central to the premise of the PEN-3 cultural model is the idea of listening13,30 which in this study, offered the opportunity to help clarify individual perceptions or conspiratorial beliefs participants may have about HIV testing. Dialogs like our focus group sessions also encouraged openness as researchers and individuals in the course of discussions worked together to displace the taken for-granted assumptions about HIV including assuaging the perceptions of fear that individuals may have with HIV testing.
In settings where there is perceived lack of confidentiality regarding HIV testing or multiple beliefs about testing in general, there is a need to scale up and sustain hybrid models of integrated laboratory testing (that includes, e.g., HIV counseling and testing with rapid oral swab tests, malaria, hepatitis, blood pressure screening, diabetes testing, etc.) in community-based settings.39 These multidisease health campaigns may provide the opportunity to test as many people who might not have perceived themselves to be at risk for HIV, increase the rate at which people test and receive their results, while providing the opportunity to link those who test positive to care or provide HIV prevention education for those who tested negative.39 They also allow flexibility at the community and individual level to help reach testing coverage goals.39
At the structural level, and as a positive enabling structure, the influence of the church is significant in a setting where church attendance is high. Efforts should be made to work with faith-based organizations to integrate multidisease health campaigns that include HIV counseling and testing, into their existing health platform of churches. Particularly, this study has implications for developing faith-based HIV testing and treatment initiatives, as participants expressed support for involvement of the church in health promotion activities. Given the significance of faith-based organizations in Nigeria, it is possible that the church may be a valuable partner in promotion of HIV testing and linkage to care among pregnant women, thus contributing to reduction in rates of pediatric HIV in Nigeria.
Limitations
This study is not without limitations. First, the findings are limited due to selection bias.40 We sought to include a purposive sample of HBI participants, but due in part to feasibility and scheduling issues, other potentially relevant HBI participants with key perceptions on why people test or do not test for HIV may not have been adequately represented in this study. Furthermore, social desirability bias41 may be present in data collection due to the sensitive nature of the topic with participants giving answers they think are socially accepted rather than being strictly honest. However, in an attempt to minimize this bias, we used multiple sources of data collection tools and probed participants where necessary to elaborate on the perceptions shared. Finally, our small sample size with participants comprising people that belong to the Igbo ethnic group of Nigeria means that our findings may not be generalizable to other settings. Despite these limitations, our use of the PEN-3 cultural model provides a valuable starting point for understanding the factors, including the role culture may play in influencing HIV testing. Our findings are also starting point for development of interventions to promote churches’ involvement in HIV testing and linkage to care. The focus-group process guided by the PEN-3 model may be useful to other researchers interested in engaging in cultural-centered dialogs on the factors influencing HIV testing.
Conclusion
Given the need to increase uptake of HIV testing in high-risk settings like Nigeria, the issue is not whether HIV testing is important, but how to encourage people to increase their intent, and subsequently undertake HIV testing. Our results represent an important step toward filling this gap and highlight the importance of engaging in dialogs that use cultural framework. This approach allows not only discussions of cultural beliefs and practices that are beneficial and should be encouraged (e.g., need to know one’s status, influence of marriage) but also factors that are harmful (e.g., conspiratorial beliefs about blood, HIV-related stigma) and may undermine uptake of HIV testing. In this way, future interventions and policies should be as much about promoting positive factors that influence HIV testing as changing negative ones.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was co-funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Institute of Mental Health (NIMH), the President’s Emergency Plan for AIDS Relief (PEPFAR) under award number R01HD075050 (Ezeanolue, PI). The funding agencies played no role in the study conception, design, data collection, data analysis, data interpretation or writing of this report.
Biographies
John E. Ehiri is a professor of Public Health and the chair of the Department of Health Promotion Sciences at the University of Arizona, Tucson.
Juliet Iwelunmor is an assistant professor in the Department of Kinesiology and Community Health, College of Applied Health Sciences, University of Illinois at Urbana-Champaign, IL, USA. Her research explores social, cultural, behavioral, and policy factors that influence the health of individuals, families, and communities across the lifespan. She is particularly interested in global health issues, having previously worked as the Culture Sector coordinator for the United Nations Educational, Scientific and Cultural Organization (UNESCO) Intersectoral Platform on HIV and AIDS. Dr. Iwelunmor completed her PhD in Biobehavioral Health and Demography at The Pennsylvania State University, from which she also received her undergraduate degree in Human Development and Family Studies.
Theddeus Iheanacho is an assistant professor of Psychiatry at Yale University School of Medicine, and medical director, CTI/HUD-VASH Program, at VA Connecticut Health Care System.
Sarah Blackstone is a PhD Candidate in Community Health at the University of Illinois Urbana-Champaign. Her interests are in dissemination and implementation science, specifically designing and implementing effective and sustainable interventions targeting maternal and child health, sexual and reproductive health, and chronic diseases in low-resource settings.
Michael C. Obiefune is the executive medical director of PeTR-Global Solutions, a local Non-Governmental Organization that implements The US President’s Emergency Plan for AIDS Relief (PEPFAR) in Enugu State, Nigeria.
Amaka G. Ogidi is a staff of of PeTR-Global Solutions, a local Non-Governmental Organization that implements The US President’s Emergency Plan for AIDS Relief (PEPFAR) in Enugu State, Nigeria.
Frances U. Ahunanya is a staff of of PeTR-Global Solutions, a local Non-Governmental Organization that implements The US President’s Emergency Plan for AIDS Relief (PEPFAR) in Enugu State, Nigeria.
Donatus Nnadi is a staff of PeTR-Global Solutions, a local Non-Governmental Organization that implements The US President’s Emergency Plan for AIDS Relief (PEPFAR) in Enugu State, Nigeria.
Dina Patel is a staff of Global Health and Implementation Research Initiatives, School of Community Health Sciences, University of Nevada, Las Vegas, USA. She is also a staff of HealthySunrise Foundation, Las Vegas, USA.
Aaron T. Hunt is a staff of Global Health and Implementation Research Initiatives, School of Community Health Sciences, University of Nevada, Las Vegas, USA. He is also a staff of HealthySunrise Foundation, Las Vegas, USA.
Echezona E. Ezeanolue is a professor of Pediatrics and Public Health and the director of Global Health and Implementation Research Initiatives, School of Community Health Sciences, University of Nevada, Las Vegas.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.UNAIDS. Progress report on the global plan. 2014. [Google Scholar]
- 2.NACA. Federal republic of Nigeria, global AIDS report: country progress report. 2015. [Google Scholar]
- 3.NDHS. National population commission; Nigerian demographic and health survey reports. 2013. [Google Scholar]
- 4.NACA. National agency for the control of AIDS; Nigeria global AIDS response, county progress report. 2012. [Google Scholar]
- 5.Cherutich P, et al. Lack of knowledge of HIV status a major barrier to HIV prevention, care and treatment efforts in Kenya: results from a nationally representative study. PLoS One. 2012;7:e36797. doi: 10.1371/journal.pone.0036797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cherutich P, Bunnell R, Mermin J. HIV testing: current practice and future directions. Curr HIV/AIDS Rep. 2013;10:134–141. doi: 10.1007/s11904-013-0158-8. [DOI] [PubMed] [Google Scholar]
- 7.Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape Town, South Africa. Sex Transm Infect. 2003;79:442–447. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmed S, et al. HIV counseling and testing and access-to-care needs of populations most-at-risk for HIV in Nigeria. AIDS Care. 2013;25:85–94. doi: 10.1080/09540121.2012.686597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morin SF, et al. Removing barriers to knowing HIV status: same-day mobile HIV testing in Zimbabwe. JAIDS. 2006;41:218–224. doi: 10.1097/01.qai.0000179455.01068.ab. [DOI] [PubMed] [Google Scholar]
- 10.Negin J, et al. Feasibility, acceptability and cost of home-based HIV testing in rural Kenya. Trop Med Int Health. 2009;14:849–855. doi: 10.1111/j.1365-3156.2009.02304.x. [DOI] [PubMed] [Google Scholar]
- 11.Ezeanolue EE, et al. Comparative effectiveness of congregation-versus clinic-based approach to prevention of mother-to-child HIV transmission: study protocol for a cluster randomized controlled trial. Implement Sci. 2013;8:62. doi: 10.1186/1748-5908-8-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ezeanolue E, et al. The baby shower initiative: a framework for interventions to promote birth outcomes. Ann Glob Health. 2014;80:227. [Google Scholar]
- 13.Airhihenbuwa CO. Health and culture: beyond the Western paradigm. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- 14.Airhihenbuwa CO, Webster JD. Culture and African contexts of HIV/AIDS prevention, care and support. SAHARA-J. 2004;1:4–13. doi: 10.1080/17290376.2004.9724822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Airhihenbuwa C, et al. Stigma, culture, and HIV and AIDS in the western cape, South Africa: an application of the PEN-3 cultural model for community-based research. J Black Psychol. 2009;35:407–432. doi: 10.1177/0095798408329941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iwelunmor J, Newsome V, Airhihenbuwa CO. Framing the impact of culture on health: a systematic review of the PEN-3 cultural model and its application in public health research and interventions. Ethnicity & Health. 2014;19:20–46. doi: 10.1080/13557858.2013.857768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Airhihenbuwa C. On being comfortable with being uncomfortable: centering an Africanist vision in our gateway to global health. Health Educ Behav. 2007;34:31–42. doi: 10.1177/1090198106291377. [DOI] [PubMed] [Google Scholar]
- 18.Krueger RA, Casey MA. Focus groups: a practical guide for applied research. Thousand Oaks, CA: Sage; 2009. [Google Scholar]
- 19.Iwelunmor J, Zungu N. Rethinking HIV/AIDS disclosure among women within the context of motherhood in South Africa. Am J Public Health. 2010;100:1393. doi: 10.2105/AJPH.2009.168989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Okonjo K. Aspects of continuity and change in mate-selection among the Igbo West of the River Niger. J Comp Fam Stud. 1992;23:339–360. [Google Scholar]
- 21.Smith DJ. Contradictions in Nigeria’s fertility transition: the burdens and benefits of having people. Popul Dev Rev. 2004;30:221–238. [Google Scholar]
- 22.Isiugo-Abanihe UC. The socio-cultural context of high fertility among Igbo women. Int Sociol. 1994;9:237–258. doi: 10.1177/026858094009002008. [DOI] [PubMed] [Google Scholar]
- 23.Strauss A, Corbin J. Basics of qualitative research. Vol. 15. Newbury Park, CA: Sage; 1990. [Google Scholar]
- 24.Kendall J. Axial coding and the grounded theory controversy. West J Nurs Res. 1999;21:743–757. doi: 10.1177/019394599902100603. [DOI] [PubMed] [Google Scholar]
- 25.Corbin JM, Strauss A. Grounded theory research: procedures, canons, and evaluative criteria. Qual Soc. 1990;13:3–21. [Google Scholar]
- 26.Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 27.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–112. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 28.Iwelunmor J, et al. Family systems and HIV/AIDS in South Africa. Int Q Community Health Educ. 2008;27:321–335. doi: 10.2190/IQ.27.4.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Iwelunmor J, et al. Socio-cultural factors influencing the prevention of mother-to-child transmission of HIV in Nigeria: a synthesis of the literature. BMC Public Health. 2014;14:1. doi: 10.1186/1471-2458-14-771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Airhihenbuwa CO. Healing our differences: the crisis of global health and the politics of identity. Lanham, MD: Rowman & Littlefield; 2007. [Google Scholar]
- 31.Campbell MK, et al. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213–234. doi: 10.1146/annurev.publhealth.28.021406.144016. [DOI] [PubMed] [Google Scholar]
- 32.Wingood GM, et al. Design of a faith-based HIV intervention: successful collaboration between a university and a church. Health Promot Pract. 2011;12:823–831. doi: 10.1177/1524839910372039. [DOI] [PubMed] [Google Scholar]
- 33.Winskell K, et al. Making sense of HIV in southeastern Nigeria. Med Anthropol Q. 2013;27:193–214. doi: 10.1111/maq.12023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Musheke M, et al. A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in Sub-Saharan Africa. BMC Public Health. 2013;13:1. doi: 10.1186/1471-2458-13-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nyondo A, Chimwaza A, Muula A. Stakeholders’ perceptions on factors influencing male involvement in prevention of mother to child transmission of HIV services in Blantyre, Malawi. BMC Public Health. 2014;14:691. doi: 10.1186/1471-2458-14-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sprague C, Chersich MF, Black V. Health system weaknesses constrain access to PMTCT and maternal HIV services in South Africa: a qualitative enquiry. AIDS Res Ther. 2011;8:10. doi: 10.1186/1742-6405-8-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Medley AM, Mugerwa GW, Kennedy C, et al. Ugandan men’s attitudes toward their partner’s participation in antenatal HIV testing. Health Care Women Int. 2012;34:359–374. doi: 10.1080/07399332.2012.655392. [DOI] [PubMed] [Google Scholar]
- 38.Turan JM, et al. HIV/AIDS stigma and refusal of HIV testing among pregnant women in rural Kenya: results from the MAMAS study. AIDS Behav. 2011;15:1111–1120. doi: 10.1007/s10461-010-9798-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chamie G, et al. A hybrid mobile approach for population-wide HIV testing in rural east Africa: an observational study. Lancet HIV. 2016;3:e111–e119. doi: 10.1016/S2352-3018(15)00251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barbour RS. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog? BMJ. 2001;322:1115–1117. doi: 10.1136/bmj.322.7294.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fisher RJ. Social desirability bias and the validity of indirect questioning. J Cons Res. 1993;20:303–315. [Google Scholar]