Abstract
Poor balance and balance impairments are major predictors of falls. The purpose of the current study was to determine the clinical validity of baseline quantitative static trunk sway measurements in predicting incident falls in a cohort of 287 community-dwelling non-demented older Americans (mean age 76.14±6.82 years; 54% female). Trunk sway was measured using the SwayStar™ device, and quantified as angular displacement in degrees in anterior-posterior (pitch) and medio-lateral (roll) planes. Over a one-year follow-up period, 66 elders (23%) reported incident falls. Anterior-posterior angular displacement was a strong predictor of incident falls in older adults in Cox proportional hazards models (hazard ratio adjusted for age, gender, education, RBANS total score, medical comorbidities, geriatric depression scale score, sensory impairments, gait speed, and history of fall in the past 1 year ((aHR) =1.59; p = .033) whereas, angular displacement in the medio-lateral plane was not predictive of falls (aHR=1.35; p = .276). Our results reveal the significance of quantitative trunk sway, specifically anterior-posterior angular displacement, in predicting incident falls in older adults.
Keywords: Static Balance, Trunk Sway, Falls, Older Adults, Aging
1. Introduction
Balance or the ability to distribute one’s weight in an effort to remain upright and steady is a complex and multifaceted construct involving successful integration of sensory, motor, and musculo-skeletal systems, which are all impacted by increasing age [1, 2]. Static balance or the ability to sustain the body in equilibrium within its base of support [3] is typically measured during bipedal standing. Since the body is never really motionless during standing, body sway can be measured in two planes: 1) anterior-posterior (forward-backward movement) and 2) medio-lateral (left-right movement). Much of the research is in agreement that medio-lateral control of balance occurs mainly at the hips and trunk, while anterior-posterior control of balance occurs mainly at the ankles [4].
Postural sway during standing has been linked to falls in the elderly using mainly force plate technology with and without sensory disturbances [5–8]; however, these investigations have yielded inconsistent findings in regards to fall prediction being associated with either medio-lateral or anterior-posterior trunk sway (see [9] for review). Innovative technology now provides advanced reliable and valid quantitative assessments of multi-directional static balance performance [i.e., trunk sway; 10, 11, 12], but its clinical utility in predicting incident falls in older adults is unknown. The main objective of the current study was to establish the clinical validity of quantitative trunk sway performance during undisturbed standing with eyes open in medio-lateral and anterior-posterior directions in predicting incident falls over a one-year follow-up period in 287 community-dwelling older Americans using the SwayStar™ system. Given the fact that over three-fourths of older Americans have balance problems and are consequently more likely to fall[13], we surmised that baseline trunk sway could be a marker of ‘steadiness’ to predict incident falls. Herein, we set out to test our hypothesis that individuals at risk for future falls would demonstrate significantly increased angular displacement at baseline compared to elders without a fall.
2. Materials and Methods
2.1. Participants
Older adults recruited for the Central Control of Mobility in Aging (CCMA) study at the Albert Einstein College of Medicine (AECOM) in Bronx, NY with available trunk sway data and one year of standardized follow-up fall interviews (see Section 2.3 below) were included. CCMA study procedures have been described elsewhere [14, 15]. In brief, potential community-dwelling participants ages 65 years and older and English speaking were identified from a population list of lower Westchester County, NY. Exclusion criteria included presence of dementia, significant loss of vision or hearing, inability to ambulate independently even by using a walking device, and current or past history of neurological or psychiatric disorders or medical procedures that may affect mobility. For the purposes of the current study, individuals with Parkinson’s disease were excluded. All participants provided written informed consent to the experimental procedures, which were approved by AECOM’s institutional review board and were in accordance with the Declaration of Helsinki.
Participants were deemed non-demented using validated cut scores from the AD8 Dementia Screening Interview [cutoff score ≥2; 16] and the Memory Impairment Screen [MIS; cutoff score < 5; 17], and later confirmed using consensus clinical case conference procedures [see 18] where the presence of mild cognitive impairment syndrome (MCI) was also determined. Global cognitive status was assessed with the Repeatable Battery for Assessment of Neuropsychological Status (RBANS) and depressive symptomology was characterized using the Geriatric Depression Scale (GDS-30 item).
Medical comorbidity index scores (range 0–9) were obtained from dichotomous rating (presence or absence) of physician diagnosed diabetes, chronic heart failure, arthritis, hypertension, depression, stroke, chronic obstructive pulmonary disease, angina, and myocardial infarction [see also 18, 19]. This scale typically includes ratings for Parkinson’s disease (PD), but as previously mentioned PD was an exclusion criterion.
All participants were required to successfully complete a visual and sensory screening exam. Visual acuity was reported as the lowest (i.e., worst) monocular value on the Snellen eye chart in decimal notation (from 0.20 (or 20/100) to 1.00 (or 20/20)), and participants with acuity < .20 were excluded. Sensation in the lower extremities was measured at the big toe using a 128Hz tuning fork by the study clinician, and rated as either normal or impaired with normal performance defined as the ability to feel the tuning fork struck moderately hard for 10 seconds or longer; while sensation was used as a covariate in our statistical models, it was not used as exclusion criteria.
2.2. Trunk Sway Measurements
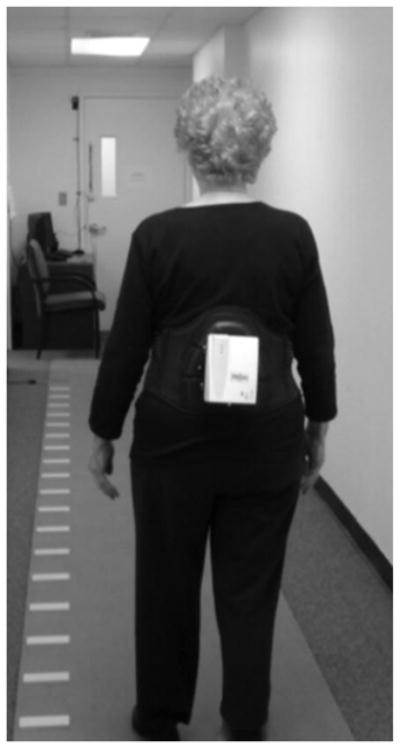
Trunk sway was measured using the SwayStar™ device system (Balance International Innovations GMBH, Switzerland) that contains sensors to record angular deviations of the trunk in both the medio-lateral (roll) and anterior-posterior (pitch) planes at a sampling frequency of 100 Hz [10, 12]. The SwayStar system includes a lightweight device (750 grams) that is mounted on an adjustable belt and sits securely near the center of mass on the participant’s lower back (L3-5 vertebral body; see Figure 1). Participants were asked to wear the Swaystar device and keep their eyes open while standing still with feet shoulder width apart on a firm flat surface for a period of 10 seconds. Quantitative trunk sway measurements were simultaneously recorded. Participants were not required to be tethered with cables as wireless Bluetooth communication was employed between the SwayStar device and the recording computer.
Figure 1.
Peak-to-peak measures of angular displacement in both planes were measured and bias was removed using a 90% range of excursion values as described in the Swaystar manual (see [20]). The peak-to-peak range of the participant’s excursions was divided into 40 bins. Each 10 ms sample was assigned to one of these bins depending on its amplitude. With all samples binned, a histogram was created and the lower 5% and upper 95% limits were removed to minimize effects of outlying values. The SwayStar system has been reported to have good test-retest reliability [r=.69 and r=.81 for roll and pitch respectively; see 12].
2.3. Fall Interviews
Falls data was ascertained via structured telephone interviews and at yearly in-house visits. Falls were operationalized as unintentionally coming down to the floor or to a lower level not due to a major intrinsic or extrinsic event [21]. Participants were asked a baseline visit whether they experienced a fall during the past one year, of which 45 elders endorsed a fall. Trained research assistants contacted participants by telephone every 2–3 months and asked a series of questions, using a standardized form to reduce inter-tester-variability. Falls were ascertained by the question: “Have you fallen since we last spoke?” If the participant endorsed a fall, further information regarding the location of the fall and whether an injury was sustained from each fall was also collected. In order to be included in the current study, participants were required to partake in systematic falls interviews over a one-year period. As it is not feasible for every participant to be contacted at exactly 365 days post-baseline visit, we allowed the time-window for the one-year fall interview to extend up to 30 days post-baseline visit. The one-year follow-up interval was selected, as this was a clinically relevant period for over which clinicians could make prognostications and that would inform patients about their fall risk over a relatively short period of time. Sixty-six individuals reported a fall during the 12-month follow-up period, of which only twelve participants reported a previous fall at baseline.
2.4. Statistical Approach
Data were inspected descriptively and graphically and the normality of model assumptions was formally tested. Angular displacements for both pitch and roll planes had skewed distributions and were log transformed to achieve normality. Descriptive statistics (mean and standard deviation (SD)) were calculated for continuous variables, including demographics and trunk sway. Separate Cox proportional hazards models were used to compute hazard ratios (HR) with 95% confidence intervals (CI) to predict incident falls based on trunk sway angular displacement for both the pitch and roll planes. In terms of the time scale, if the participant reported a fall at any time during the one-year period, then their time to fall was recorded in days from baseline to date of the interview at which the fall was reported. It should be noted that the ‘time-to-fall’ variable is based on the date of the interview when a fall was endorsed, and does not represent the actual date of the fall. If the participant did not report a fall during this one-year period, then the time to censor was recorded as the number of days from baseline to the last date of contact. Cox models were run unadjusted and then fully-adjusted for age, gender, education, RBANS total score, medical comorbidity index score, Geriatric Depression Scale Score, visual acuity, presence of somatosensory impairments, gait speed and history of falls during the one-year time interval prior to the baseline visit. The covariates were selected based on associations with falls reported in our previous studies [see 22]. Proportional hazards assumptions of all models were tested graphically and analytically, and were adequately met. All statistical analyses were run using IBM’s Statistical Package for the Social Sciences (SPSS) version 21.
3. Results
3.1. Demographics
Two hundred and eighty-seven older adults (mean age 76.14±6.82 years; 54% female) with Swaystar data collected between June 2011 and March 2013 and one- year of follow-up falls interviews participated in the current study. None of the participants met criteria for dementia [18]. All participants were deemed relatively healthy given the low number of endorsed medical comorbidities [see also 18, 19]. Table 1 delineates additional demographic information and average angular displacement values for pitch and roll planes. Over a mean study follow-up period of 316.04 days, 66 participants (23%) reported an incident fall with the mean time to fall equal to 224.56 days (range 42 – 383). Compared to the 221 older adults who did not report an incident fall, the 66 elders who reported a fall were significantly older (77.92 vs. 75.61 years; p = .02), had worse global health scale scores (1.91 vs. 1.52; p = .02) and manifested significantly slower gait speeds (92.32 vs. 103.72 cm/sec; p < .01); otherwise, fallers and non-fallers were not materially different on any of the other specified covariates.
Table 1.
Demographic and clinical characteristics of study sample (n=287)
| Variable | Value* | Range |
|---|---|---|
| Age (years) | 76.14 ± 6.82 | 65–95 |
| Female (%) | 155 (54) | |
| Ethnicity, White (%) | 251 (88) | |
| Education (years) | 14.43 ± 2.81 | 5–21 |
| RBANS Total Score (55–145) | 91.66 ± 12.22 | 62–137 |
| Geriatric Depression Scale (GDS) Score (0–30) | 4.75 ± 3.83 | 0–20 |
| Medical Comorbidity Index Score (0–9) | 1.61 ± 1.14 | 0–5 |
| Visual Acuity (decimal notation) | 0.45 ± 0.18 | 0.20–1.00 |
| Sensory Impairment (%) | 43 (15) | |
| Gait Velocity (cm/sec) | 101.10 ± 22.32 | 36–170 |
| Study follow-up period (days) | 316.04 ± 77.31 | 42–390 |
| Prevalent Falls (%; 1 year prior to study commencement) | 45 (16) | |
| Incident Falls (%) | 66 (23) | |
| Time to fall (days) | 224.56 ± 106.51 | 42–383 |
| Pitch angle displacement during standing (°) | 1.69 ± 1.33 | 0.36–9.67 |
| Roll angle displacement during standing (°) | 1.06 ± 0.55 | 0.11–4.97 |
Values are presented as mean ± SD for continuous variables and n (%) for dichotomous variables.
3.2. Trunk Sway & Falls
In adjusted models, anterior-posterior angular displacement (HR 1.64, p = .033) at baseline predicted incident falls in older adults (see Table 2), with fallers demonstrating significantly larger anterior-posterior angular displacements than non-fallers (p = .034). However, medio-lateral angular displacements between fallers and non-fallers were similar and not predictive of incident falls (HR 1.35, p = .276). Receiver-operating-characteristic (ROC) curve analysis was used to estimate accuracy of classifying older adults into those who fell during a one-year period using anterior-posterior angular displacement as a predictor. Sensitivity (true-positive proportion) was plotted vs. 1-specificity (false-positive proportion) with classification accuracy indicated by area under the ROC curve (AUC). Anterior-posterior angular displacement was found to be a significant predictor (AUC = .60, p = .01, 95% CI [.53 – .68]. Based on a cut-off value of 1.88° displacement in the anterior-posterior plane, the sensitivity and specificity for detecting incident falls was 31.8% and 77.4% respectively.
Table 2.
Trunk Sway and Fall Risk: Cox Model Results
| Factors# | Unadjusted Model | Fully Adjusted Model^ | ||
|---|---|---|---|---|
| HR (95% CI) | p-value | aHR (95% CI) | p-value | |
| Pitch Angle Displacement | 1.64 (1.10–2.46) | .016 | 1.59 (1.04–2.42) | .033 |
| Roll Angle Displacement | 1.51 (0.90–2.52) | .118 | 1.31 (0.78–2.20) | .315 |
Pitch and Roll values were log-transformed
Adjusted for Age, Gender, Education, RBANS Total Score, Global Health Score, Geriatric Depression Scale Score, Somatosensory Impairment, Visual Acuity, Gait Velocity, & History of a Fall in past 1 year.
4. Discussion
Using innovative quantitative trunk sway measures, we demonstrate that angular displacement in the anterior-posterior, but not medio-lateral plane, at baseline was associated with a 64% increased risk of incident falls over a one-year study period in a relatively large cohort of non-demented community-dwelling seniors. These findings remained significant even after controlling for critical covariates. The high specificity of anterior-posterior angular displacement indicates that this process is important for predicting falls, while the low sensitivity is expected given that this assessment should be considered in the context of a multifactorial fall risk evaluation.
4.1. Trunk Sway in Aging
With aging comes increased variability in mobility, including both balance and gait processes and such systemic changes are likely the result of less automated postural control mechanisms that increase the likelihood of elders having a fall [2]. While aging has been associated with increased trunk sway across both planes [23, 24], the clinical utility of quantitative trunk sway in predicting falls in healthy community-dwelling older adults has not been thoroughly investigated. Our results are in line with findings from Maki and colleagues [6], where prospective fallers demonstrated significantly increased anterior-posterior sway on a force-plate compared to non-fallers during an eyes-open test of spontaneous sway. In the same spontaneous sway test, Maki et al. also reported increased mediolateral sway for fallers vs. non-fallers, however this only occurred when participants were blindfolded which highlights the importance of vision during anterior-posterior sway.
Balance control during bipedal standing relies on both ankle and hip strategies, depending on whether leg and trunk segments are moving in or out of phase [25]. As previously mentioned, medio-lateral control of balance occurs mainly at the hips and trunk (i.e., core), while anterior-posterior control of balance occurs mainly at the ankles (i.e., lower extremities) [4]. The current study reveals that anterior-posterior trunk sway is a significant predictor of falls with 60% classification accuracy for older adults. Perhaps one explanation for this significant finding is that older adults that are more likely to experience an incident fall actually manifest weaker lower-extremity muscle strength [2, 24] which has been identified as a strong independent predictor of functional impairments [26]. A more comprehensive investigation of the association of lower-extremity muscle strength with anterior-posterior sway in future studies is warranted. Nevertheless, these results reveal the clinical validity of anterior-posterior trunk sway in predicting incident falls.
4.2. Future Directions
Successful balance requires efficient interaction of musculo-skeletal and sensory systems (namely visual, somatosensory, and vestibular) to control biomechanical and peripersonal movements in three-dimensional space [4]. Our previous research provide clues regarding the consequences of inefficient visual-somatosensory integration and its link to worse static balance (measured using the unipedal test) and history of falls in older adults [27]. It would be critical for future studies to discern whether inefficient visual-somatosensory integration and trunk sway in older adults rely on overlapping functional neural circuitry, as both have been associated with falls in older adults. Identification of such shared neural networks could prove useful in the development of future sensorimotor interventions aimed at increasing sensory, motor, and balance processes while reducing falls for older adults.
4.3. Study Strengths and Limitations
This study has a number of strengths including use of a relatively large sample enrolled in a longitudinal study, use of reliable and valid trunk sway procedures, as well as standardized falls ascertainment methods, and the prospective design. Nevertheless, no study is without its limitations. To improve the reliability of our measures and safety of participants, we did not include individuals with disability or dementia. Thus, the generalizability of our data is limited by the fact that our study sample was relatively healthy, ambulatory, and free of dementia. Many studies investigating trunk sway rely on force-plate technology for postural balance measurements and yet the results have been inconsistent. Our main objective was to establish the validity of predicting incident falls using innovative quantitative trunk sway. The protocol implemented at our institution contained a 10-second standing paradigm. While we can appreciate that 10 seconds seems like a relatively short duration for capturing sway, we previously reported on the role of prefrontal cortical activation during postural control in older adults with and without Parkinsonian syndrome using a 10-second epoch.[28] There, we examined concurrent functional brain activity using functional near-infrared spectroscopy (fNIRS) and actual postural control using center of pressure measures from an electronic gait pad with embedded pressure sensors. Other studies have implemented longer sampling durations [9, 29–31] and have reported that as the sample duration increases, so does the reliability of the data. [29–31] Future studies should employ a longer sample duration to increase reliability, allow for more detailed time-series analysis, and afford more detailed comparisons with other studies using similar sway measures.
4.4. Conclusions
In conclusion, our results reveal the significance of quantitative trunk sway, specifically anterior-posterior angular displacement, in predicting incident falls over a one-year period. Given the multifactorial nature of falls in older adults, static balance testing should be considered in the context of a multifactorial fall risk assessment, especially over relatively short follow-up intervals. Given the ubiquity of balance impairments in seniors and the fact that such impairments are likely amenable to interventions, our data provide support for implementation of balance training programs that predominately focus on enhancing anterior-posterior balance control mechanisms.
Highlights.
1) Poor balance and balance impairments are major predictors of falls.
2) Quantitative balance tests are free of subjective assessments of equilibrium control.
3) Increased trunk sway in the pitch plane was a significant predictor of falls.
4) Elders with incident falls manifested significantly reduced lower-extremity strength.
5) Such findings will prove useful in development of interventions aimed at reducing falls.
Acknowledgments
Research was supported by funding from the National Institute on Aging (R01AG036921-01A1 & R01AG044007-01A1) and the Resnick Gerontology Center at the Albert Einstein College of Medicine. We express our gratitude to the CCMA participants and research assistants for their assistance with data collection.
Footnotes
Author Contributions
JRM and JV developed and implemented the project. MO collected and cleaned the data. MO & JV supervised the project. EA provided significant contribution to the statistical approach. JRM analyzed the data and created the figures and tables. All authors contributed extensively to the work presented in this paper, commented on the manuscript throughout the editorial process, and approved the final submitted version.
Conflict of Interest Statement
This research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Vision, Hearing, Balance, and Sensory Impairment in Americans Aged 70 Years and Over: United States, 1999–2006. Center for Disease Control; http://www.cdc.gov/nchs/products/databriefs/db31.htm. [PubMed] [Google Scholar]
- 2.Lord S, Sherrington C, Menz H, Close JC. Falls in Older People: Risk factors and strategies for prevention. Cambridge: Cambridge University Press; 2007. [Google Scholar]
- 3.Goldie PA, Bach TM, Evans OM. Force platform measures for evaluating postural control: reliability and validity. Archives of physical medicine and rehabilitation. 1989;70:510–7. [PubMed] [Google Scholar]
- 4.Shumway-Cook A, Woollacott M. Motor Control. 4. Lippincott, Williams, & Wilkins; 2012. [Google Scholar]
- 5.Lord SR, Clark RD. Simple physiological and clinical tests for the accurate prediction of falling in older people. Gerontology. 1996;42:199–203. doi: 10.1159/000213793. [DOI] [PubMed] [Google Scholar]
- 6.Maki BE, Holliday PJ, Topper AK. A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. Journal of gerontology. 1994;49:M72–84. doi: 10.1093/geronj/49.2.m72. [DOI] [PubMed] [Google Scholar]
- 7.Stel VS, Smit JH, Pluijm SM, Lips P. Balance and mobility performance as treatable risk factors for recurrent falling in older persons. Journal of clinical epidemiology. 2003;56:659–68. doi: 10.1016/s0895-4356(03)00082-9. [DOI] [PubMed] [Google Scholar]
- 8.Thapa PB, Gideon P, Brockman KG, Fought RL, Ray WA. Clinical and biomechanical measures of balance as fall predictors in ambulatory nursing home residents. The journals of gerontology Series A, Biological sciences and medical sciences. 1996;51:M239–46. doi: 10.1093/gerona/51a.5.m239. [DOI] [PubMed] [Google Scholar]
- 9.Piirtola M, Era P. Force platform measurements as predictors of falls among older people - a review. Gerontology. 2006;52:1–16. doi: 10.1159/000089820. [DOI] [PubMed] [Google Scholar]
- 10.Gill J, Allum JH, Carpenter MG, Held-Ziolkowska M, Adkin AL, Honegger F, et al. Trunk sway measures of postural stability during clinical balance tests: effects of age. The journals of gerontology Series A, Biological sciences and medical sciences. 2001;56:M438–47. doi: 10.1093/gerona/56.7.m438. [DOI] [PubMed] [Google Scholar]
- 11.Allum JH, Adkin AL, Carpenter MG, Held-Ziolkowska M, Honegger F, Pierchala K. Trunk sway measures of postural stability during clinical balance tests: effects of a unilateral vestibular deficit. Gait & posture. 2001;14:227–37. doi: 10.1016/s0966-6362(01)00132-1. [DOI] [PubMed] [Google Scholar]
- 12.Lee SW, Verghese J, Holtzer R, Mahoney JR, Oh-Park M. Trunk sway during walking among older adults: norms and correlation with gait velocity. Gait & posture. 2014;40:676–81. doi: 10.1016/j.gaitpost.2014.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.http://nihseniorhealth.gov/falls/causesandriskfactors/01.html. NIH: internet.
- 14.Holtzer R, Mahoney J, Verghese J. Intraindividual variability in executive functions but not speed of processing or conflict resolution predicts performance differences in gait speed in older adults. The journals of gerontology Series A, Biological sciences and medical sciences. 2014;69:980–6. doi: 10.1093/gerona/glt180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holtzer R, Wang C, Verghese J. Performance variance on walking while talking tasks: theory, findings, and clinical implications. Age. 2014;36:373–81. doi: 10.1007/s11357-013-9570-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Galvin JE, Roe CM, Xiong C, Morris JC. Validity and reliability of the AD8 informant interview in dementia. Neurology. 2006;67:1942–8. doi: 10.1212/01.wnl.0000247042.15547.eb. [DOI] [PubMed] [Google Scholar]
- 17.Buschke H, Kuslansky G, Katz M, Stewart WF, Sliwinski MJ, Eckholdt HM, et al. Screening for dementia with the memory impairment screen. Neurology. 1999;52:231–8. doi: 10.1212/wnl.52.2.231. [DOI] [PubMed] [Google Scholar]
- 18.Holtzer R, Verghese J, Wang C, Hall CB, Lipton RB. Within-person across-neuropsychological test variability and incident dementia. JAMA. 2008;300:823–30. doi: 10.1001/jama.300.7.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verghese J, Wang C, Lipton RB, Holtzer R, Xue X. Quantitative gait dysfunction and risk of cognitive decline and dementia. Journal of neurology, neurosurgery, and psychiatry. 2007;78:929–35. doi: 10.1136/jnnp.2006.106914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.http://www.b2i.info/web/index.htm.
- 21.Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. The New England journal of medicine. 1994;331:821–7. doi: 10.1056/NEJM199409293311301. [DOI] [PubMed] [Google Scholar]
- 22.Allali G, Ayers E, Holtzer R, Verghese J. The role of postural instability/gait difficulty and fear of falling in predicting falls in non-demented older adults. Arch Geriatr Geronto. 2016 doi: 10.1016/j.archger.2016.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goutier KM, Jansen SL, Horlings CG, Kung UM, Allum JH. The influence of walking speed and gender on trunk sway for the healthy young and older adults. Age and ageing. 2010;39:647–50. doi: 10.1093/ageing/afq066. [DOI] [PubMed] [Google Scholar]
- 24.Lord SR, Clark RD, Webster IW. Physiological factors associated with falls in an elderly population. J Am Geriatr Soc. 1991;39:1194–200. doi: 10.1111/j.1532-5415.1991.tb03574.x. [DOI] [PubMed] [Google Scholar]
- 25.Creath R, Kiemel T, Horak F, Peterka R, Jeka J. A unified view of quiet and perturbed stance: simultaneous co-existing excitable modes. Neuroscience letters. 2005;377:75–80. doi: 10.1016/j.neulet.2004.11.071. [DOI] [PubMed] [Google Scholar]
- 26.Reid KF, Naumova EN, Carabello RJ, Phillips EM, Fielding RA. Lower extremity muscle mass predicts functional performance in mobility-limited elders. The journal of nutrition, health & aging. 2008;12:493–8. doi: 10.1007/BF02982711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahoney JR, Holtzer R, Verghese J. Visual-somatosensory integration and balance: evidence for psychophysical integrative differences in aging. Multisens Res. 2014;27:17–42. doi: 10.1163/22134808-00002444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mahoney JR, Holtzer R, Izzetoglu M, Zemon V, Verghese J, Allali G. The role of prefrontal cortex during postural control in Parkinsonian syndromes a functional near-infrared spectroscopy study. Brain research. 2015 doi: 10.1016/j.brainres.2015.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Le Clair K, Riach C. Postural stability measures: what to measure and for how long. Clinical biomechanics (Bristol, Avon) 1996;11:176–8. doi: 10.1016/0268-0033(95)00027-5. [DOI] [PubMed] [Google Scholar]
- 30.Carpenter MG, Frank JS, Winter DA, Peysar GW. Sampling duration effects on centre of pressure summary measures. Gait & posture. 2001;13:35–40. doi: 10.1016/s0966-6362(00)00093-x. [DOI] [PubMed] [Google Scholar]
- 31.van der Kooij H, Campbell AD, Carpenter MG. Sampling duration effects on centre of pressure descriptive measures. Gait & posture. 2011;34:19–24. doi: 10.1016/j.gaitpost.2011.02.025. [DOI] [PubMed] [Google Scholar]


