Abstract
We report outcomes of an NIH-convened meeting on training for dissemination and implementation (D&I) research, focused on accelerating translation of research to healthcare practice. Participants included leaders of current trainings, center directors, and those trained in existing programs. Given the large proportion of D&I research focused on cancer control, mental health, and substance abuse, participants overwhelmingly reflected the experiences and challenges of gaining capacity in behavioral health-related D&I research. The 2-day meeting required participants to draw upon their experiences to help build a field-wide perspective for D&I research training, identify resources needed to support this perspective, and brainstorm gaps in training that needed to be filled. Questions were sent to participants in advance, and responses were synthesized and presented to discuss during the meeting. A preliminary “field-wide” perspective emerged, spanning multiple disciplines, training models, and career levels. Current programs face high demand, need for continued evolution to reflect field advances, and sustainability challenges. Current gaps include implementation practice and predoctoral training. Federal funding is key to D&I research training, be it through grants or agency-led training programs, in order to span and address specialized disease and disorder foci and career tracks.
Keywords: Dissemination, Implementation, Research capacity, Training
The long recognized, prolonged, and incomplete uptake of scientific discoveries into health practice has sparked a focus on the translation of research into practice at the National Institutes of Health (NIH) and other funding agencies in the USA and globally. In the USA, research to accelerate and improve quality improvements and evidence-based care is commonly referred to as dissemination and implementation research (e.g., http://grants.nih.gov/grants/guide/pa-files/PAR-13-055.html) or implementation science (http://cancercontrol.cancer.gov/IS/). The NIH supported five meetings to advance the science of dissemination and implementation from 2007 through 2012. During that time, registrations grew from 300 to more than 1200 and a number of recurrent themes had emerged [1]. To take stock of the field’s progress and identify priority issues for its future, the NIH convened three strategic meetings in 2013–2014 focused on training, measurement and standardized reporting, and research designs. This paper reports the process and outcomes of the meeting focused on training for dissemination and implementation research.
MEETING FORMAT, RATIONALE, AND PURPOSE
Training was the focus of one of the three meetings for several reasons. First, demand for training in dissemination and implementation research has been consistently high. At each NIH annual meeting to advance dissemination and implementation (D&I) research, preconference technical assistance programs for new investigators were heavily subscribed, attended each year by approximately 100 people. Few D&I research training programs exist, and existing programs report high applications. For example, in its first year, the NIH-supported Training Institute in Dissemination and Implementation Research in Health (TIDIRH) received 266 applications for 35 slots; similarly, the mental health-focused Implementation Research Institute (IRI) receives five applications for every available slot [2, 3]. Second, there had been no opportunity to take stock of existing D&I research training programs, which differed in focus, format, and targeted participants. Third, there was need to identify training challenges, innovations, and priorities for a rapidly advancing field of dissemination and implementation science.
The training meeting was the first of the three, held in Bethesda September 12–13, 2013. The paper authors chaired the meeting, identified participants, and formulated an agenda. Sixteen individuals from across the country, each involved in some way in training for dissemination and implementation research, participated (see Table 1). They included senior researchers leading training programs, healthcare practitioners, leaders in health services research, research center directors, those currently in or recent alumni of the established D&I research training programs, and NIH program scientists. Given the large proportion of D&I research focused on cancer, mental health, and substance abuse, participants overwhelmingly reflected the experiences and challenges of gaining capacity in behavioral health-related D&I research. This reflects the fact that within the NIH, the National Institute of Mental Health (NIMH) and the National Cancer Institute (NCI) have a longstanding D&I research agenda, dedicated research staff, scientific priorities, active funding announcements, and meetings preceding trans-NIH activities. Within the cancer domain, the D&I research training has been primarily within the area of cancer control and prevention, domains that are overwhelmingly behavioral science in nature (e.g., diet, physical activity, screening behaviors, health communications, policy impact). The growth of D&I in these specific fields may correspond to the lack of penetration in service delivery of evidence-based interventions. .
Table 1.
Attendees of the 6th Annual NIH Meeting on Advancing the Science of Dissemination and Implementation Research Training
| Name | Affiliation |
|---|---|
| Alice Ammerman, Dr. P.H., M.P.H. | The University of North Carolina at Chapel Hill |
| Martha Bruce, Ph.D., M.P.H. | Weill Cornell Medical Center |
| Alicia Bunger, Ph.D., M.S.W. | The Ohio State University |
| Melissa Davey-Rothwell, Ph.D. | Johns Hopkins University |
| Ralph Gonzales, M.D., M.P.H. | University of California, San Francisco |
| Margaret Handley, Ph.D., M.P.H. | University of California, San Francisco |
| Kimberly Hoagwood, Ph.D. | New York University |
| Amy Kilbourne, Ph.D., M.P.H. | U.S. Department of Veterans Affairs |
| Mike Ong, M.D., Ph.D. | University of California, Los Angeles |
| Thomas Patterson, Ph.D. | University of California, San Diego |
| Enola Proctor, Ph.D. | Washington University in St. Louis |
| Ken Sherr, M.D., M.P.H. | University of Washington |
| Sharon Strauss, M.D., M.Sc. | University of Toronto |
| Glenn Wagner, Ph.D. | RAND Corporation |
| David Chambers, D.Phil. | National Institute of Mental Health, NIH |
| Christopher Gordon, Ph.D. | National Institute of Mental Health, NIH |
The meeting agenda was organized around three questions: What is a field-wide vision for training investigators at multiple career stages in D&I research? What tools and resources are needed to support this vision? And what gaps need to be filled to better train future D&I scientists? Accordingly, meeting sessions focused on the following: reviewing existing D&I research training programs; capturing the range and type of funding mechanisms supporting those programs; and understanding current training challenges.
Work commenced with a review of existing programs, recognizing that not all were represented at the meeting and that meeting participants had imperfect knowledge of the broader field. This meeting, like that year’s other NIH meetings on D&I science, included a limited number of participants, albeit those most experienced about D&I research training. Prior to the meeting, participants contributed information about current training programs in D&I research. For each program they were involved in, they were asked to describe the following: program name, location, source of support, type of trainee, program aims and measures of success, and training format. This information was reviewed and synthesized in the meeting (see Table 2). While some programs listed may have ended, they are retained in the table because their format and content shaped discussion and because such programs reflect important models that have future value. This paper does not reflect new programs started after the meeting. On day 1, participants reviewed and synthesized current training, assessed strengths and limitations, and generated a field-wide perspective on training needs in an effort to improve the rigor, reach, accessibility, and sustainability of training.
Table 2.
Training in dissemination and implementation research: current opportunities
| Training opportunity | Funding source(s) | Substantive niche | Location/auspices | Duration | Training participants | Products/deliverables |
|---|---|---|---|---|---|---|
| Summer institutes | ||||||
| TIDIRH Training Institute for Dissemination and Implementation Research in Health (http://conferences.thehillgroup.com/OBSSRinstitutes/TIDIRH2015/) | NIH | NIH-wide | University host site varies each year | 1 week | Postdoctoral Junior investigators with any NIH related interest | Research proposal draft |
| IRI Implementation Research Institute (http://iristl.org) | NIMH | Mental health services | Washington University in St. Louis | 1 week immersion each summer plus mentoring for 2 years | Postdoctoral investigators new to mental health implementation research | Competitive NIH research proposal |
| MT-DIRC Mentored Training in Dissemination and Implementation Research in Cancer (http://mtdirc.org) | NCI | Cancer prevention, control, and treatment | Washington University in St. Louis | 1 week each summer, mentoring for 2 years | Postdoctoral investigators new to cancer implementation research | Competitive NIH research proposal |
| CIHR KTSI Canadian Institutes of Health Research Knowledge Translation (KT) Summer Institute (http://ktclearinghouse.ca/ktcanada/education/summerinstitute) | CIHR | International and collaborative KT efforts | Host city varies each year | 3–4 days | Graduate students, postdoctoral and clinical fellows, and junior faculty who want to advance research skills relevant to KT | Poster sessions to facilitate networking |
| Center-based training* | ||||||
| DTMI Duke Translational Medicine Institute (https://www.dtmi.duke.edu/) | NIH CTSA grant | Various | UNC | Ongoing support | Duke faculty and staff | Training opportunities: • Education database with opportunities related to translational medicine and research Funding opportunities: • Funding database • DTRI Pilot Program Funding • Coulter Award Funding • Biomarker Factory • Young Investigator Award |
| CTSI Clinical and Translational Science Institute (https://ctsi.ucsf.edu/) | NIH CTSA grant | Various | UCSF | Ongoing support | UCSF faculty at all four schools | Training opportunities: • Online education • K Scholars program • Master of Translational Medicine program • Training in Clinical Research (TICR) • Training in Implementation Science Funding opportunities: • Career Development Awards • Catalyst Awards • Strategic Opportunities Support |
| ICTS Institute of Clinical and Translational Sciences (http://icts.wustl.edu/) | NIH CTSA grant | Various | Washington University in St. Louis | Ongoing support | ICTS affiliated scholars and researchers | Training opportunities: • Clinical Research Training Center (CRTC) Funding opportunities: • ICTS Core Usage • BJHF-ICTS Funding Program • PS-QI Funding Program • SPARC Funding Program • SPIRiT Program • St. Louis Community/University Health Research Partnerships |
| CIPRS Center for Implementation Practice and Research Support (http://www.queri.research.va.gov/ciprs/) | VA’s Health Services Research and Development (HSR&D) Quality Enhancement Research Initiative (QUERI) | Provide implementation consultation for the following resources: • QUERI Implementation Guide • QI Methods Selection Tool • TDM • CFIR |
U.S. Department of Veterans Affairs | Ongoing support | VA researchers working in the field implementation research | Educational opportunities: • Available implementation science and quality improvement methods resources • Develop additional resources |
| IDEAS Center for Implementation-Dissemination of Evidence-Based Practices among States (https://www.ideas4kidsmentalhealth.org/) | Advanced Center, NIMH | Provide resources related to imply science in health and mental health. Specific areas of focus include: • Data support • Mixed methods • Engagement |
New York University (NYU) Department of Child and Adolescent Psychiatry, The Child Study Center | Ongoing support | Various other centers and practitioners | Training opportunities: • IDEAS doctoral child and adolescent psychiatry fellowships Educational opportunities: • Technical assistance for data/decision support, mixed methods, measures, and engagement with patients and providers |
| CRN Cancer Research Network (http://crn.cancer.gov/) | U24, NCI | The CRN promotes cancer research with a particular focus in 4 broad areas: • Prevention and screening • Epidemiology of prognosis and outcomes • Healthcare quality and cost • Communications and dissemination |
The 4th funding cycle of the CRN (CRN4) is composed of 9 healthcare systems and 3 affiliate sites. All are members of the HMO Research Network. | Ongoing support | Participating health plans and research center sites; CRN scholars | Training opportunities: • CRN Scholars program, a 26-month training activity for junior investigators’ development Education opportunities: • Technical assistance for data resources and informatics as well as providing connections between communities |
| Electronic training resources | ||||||
| Advanced Topics in Implementation Science Webinar Series (https://cyberseminar.cancercontrolplanet.org/implementationscience/) | NCI’s Division of Cancer Control and Population Sciences | Topics related to IR tools, design, training, funding and grant writing Specific topics related to NIH D&I workgroups |
NCI | 1 h (30 min for presentation and 30 min for discussion and Q&A) Monthly |
New and seasoned D&I investigators | Products: archived recording with relevant references |
| QUERI Cyberseminars (coming January 2015) (http://www.queri.research.va.gov/ciprs/education.cfm) | CIPRS | QUERI research | VA | TBD | VA and non-VA audiences | Products: disseminate findings and impacts of QUERI research; share and make accessible innovative IS and QI research methods; facilitate cross-QUERI collaboration |
| VA HSR&D Cyberseminars (http://www.hsrd.research.va.gov/cyberseminars/) | CIPRS | Special series include: • HERC • QUERI • VIReC |
VA | 1 h Usually 2–3 times per week |
VA and non-VA audiences | Products: archived transcripts and recordings from previous sessions along with relevant handouts and readings |
| Implementation Network e-Newsletter (http://www.implementationnetwork.com/) | N/A | Resource and announcement portals, especially for funding, conferences, jobs, and training opportunities | Wynne Norton (formerly of the U of Alabama at Birmingham School of Public Health) | Monthly | D&I investigators, trainers, and trainees Purposely broad in membership and scope |
Products: collection of D&I publications, reports, conferences, meetings, program announcements, funding opportunities; Also: subscription and suggestion requests |
| Graduate and doctoral programs | ||||||
| Master’s in Clinical Research | Training in Clinical Research Program (TICR), co-sponsored by UCSF’s CTSI and the Dept. of Epi and Biostats | In addition to implementation and dissemination science (IDS) required courses, students can select a specialized IDS track with additional IDS-specific electives, career mentoring, and research feedback. | UCSF, CTSI | 2 years | Program intended for advanced predoctoral fellows and faculty members who wish to master clinical research methods and pursue independent research careers | Program expectations: • Master broad set of clinical research methods • Plan and implement 1+ clinical research projects • Present research at national meetings • Write comprehensive literature review and publish 1+ first-authored peer-reviewed original research papers • Obtain experience in designing, implementing and evaluating programs and interventions • Obtain experience developing funding proposals |
| Certificate Program in Implementation Science | TICR—participants in the certificate program will receive a discount of 15 % over individual course prices | This program offers material related to developing more effective interventions to translate specific evidence-based findings into everyday practice. | UCSF, CTSI | 1 year (part-time) | Program designed for a broad range of professional roles, including clinical and public health researchers, quality improvement officers, community-based clinic staff, public health and public policy practitioners, and clinicians | Program expectations: • Obtain experience designing and implementing more effective interventions • Obtain experience designing more comprehensive evaluations of interventions • Obtain experience developing better grant proposals |
| PhD program in Epidemiology and Translational Science | Students funded by various sources | 11 areas of concentration: • Aging • Bioinformatics • Biostatistics • Cancer, clinical, environmental, occupational, genetic, and social EPI • Global health • Infectious disease epidemiology • Screening and early detection |
Dept. of Epi and Biostats, UCSF School of Medicine, CTSI Primarily within UCSF’s School of Medicine, UC Berkeley and Stanford |
3–4 years | Individuals who wish to pursue independent research careers in epidemiology and translational science and who have already completed training at the master’s level in epidemiology, public health or related fields. | Program expectations: • complete two quarters of research team rotations; one quarter in both analytic and non-analytic rotations • Complete and pass combined written and oral qualifying exam • Conduct original research with publishable results • Submit a dissertation (single dissertation or 3+ publishable first-authored articles based on research) • Present dissertation findings in monthly seminar settings |
| Postdoctoral child and adolescent psychiatry fellowships | Advanced Center, NIMH | 15 ongoing projects at IDEAS. Most are focused on meeting EBP implementation challenges. | IDEAS at NYU Department of Child and Adolescent Psychiatry | N/A | Child and adolescent psychiatry fellows | Paired with senior researcher within IDEAS Center to work on research project tailored to their interests; access to academic and research interests including Grant Rounds, trainings, seminars, and conferences |
| PhD program in Global Health | Various Dept. of Global Health Programs | Area of emphasis: implementation science | WU, School of Medicine and School of Public Health | 4–5 years | Bachelor’s degree minimum with master-level training preferred | Program expectations: • Preliminary written examination • General examinations • Research and dissertation • Defense of research |
This paper presents three of the meeting’s products: (1) an assessment of current training opportunities, lessons, and challenges; (2) an initial visualization of a “field-wide framework” for training in dissemination and implementation research; and (3) recommendations for advancing D&I research training. We define “field-wide” as spanning the varied disciplines that contribute to D&I research, as comprehensive of different training models, and as responsive to investigators at different career levels. In addition, while the initial intent was to develop a vision for training, the discussions suggested that this process would require more than one meeting to accomplish. We therefore use the term “perspective” which we think better represents the current status of this work.
CURRENT TRAINING
Existing programs
D&I research training occurs through summer training institutes, graduate courses, and masters and Ph.D. degree programs. Training also occurs through Clinical and Translational Science Award (CTSA) programs and research centers’ faculty development activities and webinars and through online repositories of training materials and implementation research toolkits. Training programs have varying durations, including one-time lectures (as in a webinar), day- or week-long “immersion” workshops, semester-long courses, and 1- and 2-year institutes and use small group and one-on-one mentoring.
Funding types and sources include NIH R25 grants, NIH- or foundation-supported career development awards, and university-based grant-supported research centers. Some academic institutions provide formal training to Ph.D., M.D., and masters’ students, but most programs focus on postdoctoral, early career investigators, and experienced investigators moving into D&I from related fields. Few US-based programs seem to focus on implementers in actual practice or policy makers.
Training aims also vary, as described by meeting participants: “building a national infrastructure for training,” “developing a specialized pool of D&I researchers,” and “supporting the use of D&I practice in community settings.” Aims related to individual career development include “increasing the likelihood of independently supported science,” “promoting scholars’ development and leadership potential,” increasing knowledge, promoting collaborative relationships, and “advancing the individual’s research career.” Accordingly, training “deliverables” include knowledge, research skills, career development, competitive grant proposals, degrees, and certificates. Markers of training success ranged widely. Most programs target funded NIH grants (R01s) and peer-reviewed journal articles in D&I. Broader goals included “growth of the field,” “preparation of a new cohort of skilled investigators,” trainee-community partnerships with impact on policy or clinical care, and training the next generation of leaders.
Finally, programs varied in the extent to which they focused on a specific field or discipline. While the TIDIRH program trains researchers across the span of specialties within the NIH, others target a specific field, such as mental health, cancer, geriatrics, child health, and obesity.
Current training challenges
Participants identified 15 challenges in D&I research training (summarized in Table 3), a number of which we briefly discuss here. First, it is challenging to train for a rapidly advancing and still evolving field. In one decade, implementation science has experienced an “explosion” of progress in both quality and quantity [4]. The first compendium or text in the field—Dissemination and Implementation Research in Health—was only recently published [5]. Priority research questions and methods continue to evolve rapidly. Hence, training directors agree that curriculum content must be continually revised and methods taught in one year often need updating. Moreover, competencies required for D&I research are only beginning to be addressed.
Table 3.
Field-wide training in dissemination and implementation research summary of recommendations
| Recommendations | Responsive to identified challenges |
|---|---|
| Scale of training | |
| Increase funding for D&I training | High demand for current slots budget limits of current training grants |
| Establish centralized, accessible web sites with training materials and courses | Limited training scale trainees’ need for continued learning |
| Leverage training opportunities in centers and CTSA programs | Despite CTSA emphasis on translation, few programs offer D&I |
| Train for continuum of career levels | Limited masters’ and predoctoral training |
| Train for range of stakeholders (research, practice, policy) | Little training for D&I policy and practice |
| Training format and content | |
| Train through intense immersion programs | Depth and breadth of field |
| Increase duration of training | |
| Continual review and updating of training content | Rapid growth in field |
| Employ train the trainer models | Program sustainability |
| Emphasize generalizable content | D&I spans conditions, disorders, disciplines |
| Train participants for leadership to the D&I field | Limited D&I expertise in most universities |
| Provide tracks or programs for specialized fields | Unique needs and demands of individual fields |
| Training infrastructure | |
| Support and strengthen D&I scientific meeting(s) | Investigators need a “home base” given transdisciplinary nature of D&I |
| Build and support networks for alumni of training programs | Limited number of D&I colleagues at most institutions |
A second and closely related challenge is the breadth of the D&I field, coupled with the depth of knowledge and skill required for D&I science. The D&I field has a multitude of conceptual models and frameworks [6]. D&I research requires distinct design, measures, analytic methods, and challenges for the protection of human participants in research. With few exceptions, new publications appear in a wide and scattered range of journals and disciplines. As a recent NIH-sponsored report on implementation science research for HIV/AIDS prevention and treatment succinctly stated, “no one owns implementation science… (and) implementation science necessitates interdisciplinary collaboration” [7]. Transdisciplinarity has characterized the NIH Annual Conference on the Science of Dissemination and Implementation, the NIH-wide TIDIRH program, implementation research training in university-based CTSAs, and IRI [1–3, 7, 8]. New implementation researchers must now keep pace with not only new knowledge in their specialized areas but also the broader field.
Training programs respond to these challenges in various ways. First, most training programs provide “immersion experiences,” in which trainees must devote a solid block of time to the training programs. The IRI and the Mentored Training for Dissemination and Implementation Research in Cancer (MT-DIRC) require two full years of participation, with regular mentoring between summer institutes. Shorter programs acknowledge that only introductory exposure is possible. Across programs, trainees reported that the abundance of material in a limited timeframe sometimes felt akin to trying to drink from a fire hose.
The limited number of slots in most programs means that only a fraction of applicants can be accepted. Demand is high for international training, currently available through one Ph.D. program and occasional slots in other programs focusing largely on domestic issues. High selectivity limits training. Some programs respond to high demand by securing supplemental funding: the IRI is funded primarily by NIMH but receives supplemental funding from NIDA and the VA. Few universities have enough faculty with D&I research expertise to provide in-depth training. Among the 60+ NIH CTSAs, only a handful train in D&I research and few degree programs nationwide focus on this field.
Heterogeneity among trainees presents a fourth challenge. Trainees typically differ in their grant writing experience and success, familiarity with implementation science, and interests in different evidence-based interventions and practice settings. Accordingly, faculty must calibrate training to participants with different learning styles and levels of preparedness. Many programs leverage this heterogeneity through group mentoring. Networking sessions, using innovative formats, provide trainees with individualized faculty expertise.
Fifth, programs acknowledge that training programs demand high levels of faculty effort. NIH training grant mechanisms have low, highly structured budgets with limited indirect costs to offset institutions’ burdens in hosting programs and capped salary support for training leaders and faculty. While faculty mentoring is key to quality training [3, 9], only those willing to donate time and resources can take on such training. Given budget limitations for the NIH-supported TIDIRH, participants must pay for own travel costs. Funding constraints reduce the pool of institutions able to host training and limit trainees to those with independent sources of support.
A sixth identified challenge is the high expectations for alumni. Often returning to environments with little infrastructure support for and few colleagues in implementation science, many alumni report that they are expected to serve as D&I experts, mentoring others. Explicit expectations to secure NIH R01 grants is daunting for many trainees, especially given the limited grant support for D&I research, relative to basic and clinical science.
A final and universal challenge is sustaining training programs. Most training grants end after one or two funding cycles. To extend training capacity, many programs use a “train the trainer” approach. TIDIRH routinely posts slides from the summer institute, extending training capacity to a wider pool through web resources.
Toward a field-wide framework for D&I research training
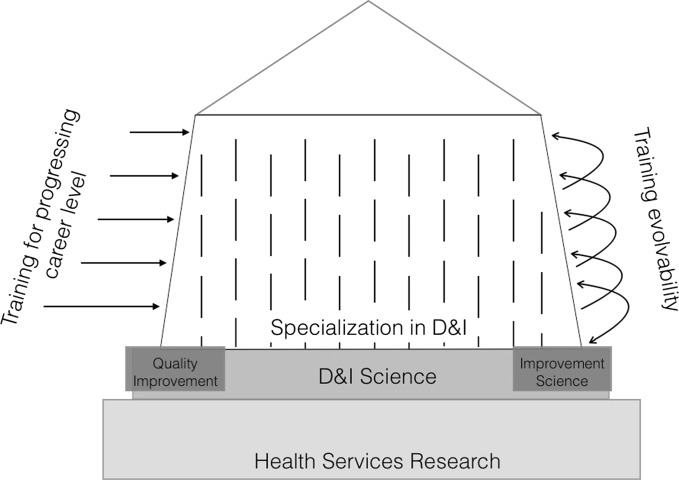
Meeting participants worked to shape a field-wide training framework that would capitalize on strengths and limitations of current training and reflect needs of the broader field in order to improve the rigor, reach, accessibility, and sustainability of D&I research training. The framework would identify a number of crosscutting training issues—across different substantive fields and educational/experience levels—and inform future training. Figure 1 depicts an initial visualization of the framework that emphasizes the need to account for the dynamism of the field, the location of D&I research within a broad scientific area of health service research, and recognition of the variability of training needs at different levels of one’s career. Recommendations for achieving this vision are summarized in Table 3.
Fig 1.
The “house” model of D&I training identifies the framework necessary to inform and sustain future training in the field of dissemination and implementation science. The boundaries of the D&I field—the walls of the house—must first be established. Broad, cross-field training is needed in addition to specialized training
Field definition, boundaries, and defined connections
Training requires a widely understood conception and definition of dissemination and implementation science as a field. Increasingly, D&I research is viewed as a distinct area of health services, delivery system science, and system redesign. Over the past decade, the field has become more clearly defined, due in part to establishment of an NIH-wide standing review committee, regular annual meetings, dedicated journal, Implementation Science, and a foundational textbook. The field is transcending the “taxonomic turmoil” that affects all new fields.
Any field-wide training framework must reflect the knowledge and skills for addressing distinctly D&I issues and employing its unique methods. Conversely, field-wide training must distinguish D&I from related research areas, while equipping trainees how and when to draw on them—areas such as industry, delivery system science, healthcare improvement, human factor engineering, patient safety research, and quality improvement science. As reflected in Fig. 1, the boundaries of the D&I field—the walls of the “house”—must be established.
Comprehensive training
The D&I field transcends traditional disease, disorder, and institute silos, and so must its training. Currently, D&I researchers focused on mental health may have little or no connections to those working on cancer-related D&I. Disciplinary or disease silos often obscure the research questions and methodologies that are distinctly D&I but common to the field. Figure 1 depicts training as spanning the breadth of the field, as broader than any one specialization.
Scaling up training
Field-wide training requires expansion on several fronts. First, training supply needs to meet demand, which existing programs cannot. Second, training should be available to investigators at all levels; more training is needed especially at the predoctoral level and for investigators who work at earlier stages of translational science, such as treatment developers. Third, training should be available for people in implementation roles, be they policy makers, administrators, supervisors, practice improvement facilitators, or front line providers. Few, if any, programs currently train for D&I practice. More and more varied D&I courses are needed to advance the field. Finally, NIH Institutes and Centers should support their own training programs to better cultivate the pipeline of investigators in specialized areas of D&I research.
Training at scale requires more adequate funding to enable training at more institutions. It also requires leveraging CTSA programs, Institute for Health Improvement initiatives, training opportunities at scientific meetings, and externally funded predoctoral and postdoctoral training programs. Scale can also be enhanced through innovative extensions of training programs. Some extenders can follow participants after they have completed a training program, providing continued career development to those returning to home institutions with little D&I research infrastructure. Also needed are web repositories of training materials (slide decks, bibliographies of key readings), electronic platforms for D&I research tools, and strong social networks that continue or span training programs. Web sites for training materials need to be assembled, catalogued, and disseminated. Libraries can warehouse webinars, conference presentation videos, and sharable syllabi, presuming resolution of intellectual property issues. Massive online open courses (MOOCs) can extend training to those remote geographically and requiring flexible training times. Training can also be provided through D&I special interest groups at scientific meetings, such as already established at the Society for Social Work Research and Practice, and through provider Practice-Based Research Networks. Figure 2 portrays the complementary roles that funding agencies, healthcare and social systems, research institutions, and professional societies could play—all contributing to enhanced D&I research capacity.
Fig 2.
Diagram of players in D&I research capacity building efforts. Research capacity is composed of healthcare and social systems, funders, research (both academic and stand-alone) institutions, and professional societies. Each of these entities interacts with one another and plays complementary roles in enhancing D&I research capacity
Specialization
A maturing field demands more specialized training programs, both in terms of fields and education levels. Thus, a fully developed framework will reflect D&I research training in a broader array of NIH institutes, beyond the current two in mental health and cancer. Moreover, tracks will be needed for trainees at different educational and experience levels and in different roles (researcher, policy maker, or administrator). Fully developed, a field-wide framework would map the training continuum for different career stages.
Continual updating of content
Given the continued and rapid advances in D&I research, a field-wide framework must be constantly assessed for content currency and flexible curriculum structures in order to accommodate updates in theoretical and methodological content. Programs should experiment with session formats and instructional styles. All D&I research training programs should be characterized by “evolvability” (K. C. Stange, oral communication, 2007), which refers to the constant updating and advancement of content to capture new developments in the field. Publication of a D&I Annual Review series and conference sessions on methodology innovations would support the evolution of cutting-edge training.
Sustainability
Successful training programs need to be sustainable. While institutional training grants can apply for competitive renewal based on strong outcomes and demonstrated need, mechanisms supporting many D&I programs allow only one renewal period. Funding constraints contribute to pent-up demand and applicant backlogs. Individual trainees need sustained training beyond short-term programs to support their leadership development. Train the trainer approaches help participants to build local communities of D&I scholars.
Implications and recommendations
The primary goal of D&I research training is to enhance and expand the research workforce that is actively advancing the knowledge base around dissemination and implementation. The proximal outcome of training is the advancement of relevant methodological expertise, increased quality and quantity of D&I research applications, and an improved empirical base to support D&I research and practice. The secondary goal is the increased dissemination and implementation of effective health interventions, and while D&I research training is primarily focused on the proximal, participants generally found the latter goal to shape the content of their research as well as the content of training on the interface between the two. These goals are essential if scientific discoveries are to improve delivery of health care.
Demand for dissemination and implementation research training significantly outweighs supply. All current training programs struggle to sustain their existence and impact after grant funding ends. D&I research continues to lack a stable home discipline or have a strong presence in most universities.
This paper’s efforts to advance a field-wide framework for D&I research training reflect the strengths and challenges of current training. The paper demonstrates the key role of federal funding in supporting training at scale for varied career paths and levels and NIH-wide disease foci and calls for a broader set of funding sources to help achieve the vision reflected here.
Shaping, developing, and delivering a field-wide vision for D&I research training will require strategic planning, vision, coordinated effort, and resources. We argue that, given the crucial role of D&I research in realizing the ultimate benefits of basic and clinical work, the NIH and other federal agencies have critical roles to play. NIH mechanisms may be uniquely positioned to help move D&I research training to scale, ensuring comprehensive training to all who enter the field, regardless of training level, field, and research orientation. Federal funding is critical in supporting D&I research training, whether through institutionally based training, individual career development grants, or special research training programs. Support is needed for training that spans the institute’s disease and disorder foci, such as the TIDIRH, as well as for disease-specific training. More individual investigators need to be supported through career development awards that are focused on dissemination and implementation research.
Equally important, the future of D&I research training requires a diverse set of stakeholders to be at the table to reflect the team-based reality of D&I research. Practitioners, health systems, patients and families, healthcare payers, community organizations, and other stakeholders all have historically been crucial to paving the way for successful dissemination and implementation of evidence-based interventions, and most are present in many of our funded research studies. This is already reflected in the transformation of the annual D&I Science conference which began as a joint effort between NIH and the VA and now involves multiple agencies, foundations, and organizations across research, practice, and policy.
The public health benefits of basic and clinical research depend on translating intervention discoveries into real world settings. The D&I research field is dedicated to fostering such translation, but training is key to the field’s development and long-term realization of benefit. Training dissemination and implementation researchers is a critical investment in improving the delivery of evidence-based healthcare, so that a pool of well-trained researchers will be prepared to test and discover strategies for increasing the reach of evidence-based interventions and their clinical effectiveness. While existing programs reflect significant progress, we assert the need for increased funding, the development of additional innovative programs, and greater synergy across initiatives. New initiatives to better meet demand and ensure the scale and depth required for training in the rapidly advancing and complex field of D&I research are key to realizing the vision reflected in the field-wide perspective presented here.
Acknowledgments
The authors wish to thank the meeting participants for their contributions to the content of this manuscript as well as the many participants in D&I research training for the many lessons we have learned working with them. Enola Proctor’s work is supported by the Center for Mental Health Services Research and the Institute for Public Health, Washington University in St. Louis, and grants 5 R25 MH080916 and 2 UL1 TR000448.
Compliance with ethical standards
Funding/support
This project was supported by the National Institutes of Health.
Notes regarding additional funding have been removed for purposes of blinding the paper.
Other disclosures
None.
Ethical approval
Not applicable
Disclaimer
None
Previous presentations
Notes regarding previous presentation of materials have been removed for purposes of blinding the paper.
Footnotes
Implications
Researchers: Amidst a growing number of D&I research programs, this paper gives a broader context for which to consider the optimization of these initiatives to ensure sufficient research capacity.
Practitioners: D&I research requires the engagement of practitioners to ensure that studies are as informative to practice audiences as possible; this paper considers how training programs can better align with practice expertise.
Policymakers: The ability to ensure that policy directives are implemented effectively requires a scientific workforce expert in the complexity of research and policy interface; this paper seeks to create such a workforce.
References
- 1.Glasgow RE, Vinson C, Chambers D, Khoury MJ, Kaplan RM, Hunter C. National Institutes of Health approaches to dissemination and implementation science: current and future directions. Am J Public Health. 2012;102(7):1274–1281. doi: 10.2105/AJPH.2012.300755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meissner HI, Glasgow RE, Vinson CA, Chambers D, Brownson RC, Green LW, Ammerman AS, Weiner BJ, Mittman B. The U.S. training institute for dissemination and implementation research in health. Implement Sci. 2012;8(12). doi: 10.1186/1748-5908-8-12 [DOI] [PMC free article] [PubMed]
- 3.Proctor EK, Landsverk J, Baumann AA, Mittman BS, Aarons GA, Brownson RC, Glisson C, Chambers D. The Implementation Research Institute: Training Mental Health Implementation Researchers in the United States. ImplementSci. 2013;8(105). doi:10.1186/1748-5908-8-105. [DOI] [PMC free article] [PubMed]
- 4.Chambers D. Forward. In: Brownson RC, Colditz GA, Proctor EK, editors. Dissemination and implementation research in health: translating science to practice. Oxford: Oxford University Press; 2012. [Google Scholar]
- 5.Brownson RC, Colditz GA, Proctor EK, editors. Dissemination and implementation research in health: translating science to practice. Oxford: Oxford University Press; 2012. [Google Scholar]
- 6.Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med. 2012;43(3):337–350. doi: 10.1016/j.amepre.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pangea Global AIDS Foundation. Report from: The expert consultation on implementation science research; July 23–24, 2009; Cape Town, South Africa. (http://pgaf.org/news-and-events/publications/75-report-from-the-expert-consultation-on-implementation-science-research).
- 8.Gonzales R, Handley MA, Ackerman S, O’Sullivan PS. A framework for training health professionals in implementation and dissemination science. Acad Med. 2012;87(3):271–278. doi: 10.1097/ACM.0b013e3182449d33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stamatakis KA, Norton WE, Stirman SW, Melvin C, Brownson RC. Developing the next generation of dissemination and implementation researchers: insights from initial trainees. Implement Sci. 2013;8(29). doi: 10.1186/1748-5908-8-29 [DOI] [PMC free article] [PubMed]