Abstract
We aimed to determine whether the administration of statins to type 2 diabetics without preexisting CHD reduced the incidence of CHD and their effects on cholesterol and CRP levels. All the participants were carefully interviewed, clinically examined, and laboratory tested to exclude conditions likely to provoke an inflammatory response that was an exclusion criterion. Exclusion criteria: Serious heart, liver or kidney problems, history of renal transplant, recent history of drug or alcohol abuse, HbA1c>10%, blood pressure >140/90mmHg, BMI >35 kg/m2, triglycerides >3,0mmol/dm1. 95 obese diabetics (mean age 60,9 years and BMI=31,59 kg/m2, diabetes duration more than 10 years) without pre-existing CHD, were included in the analysis and were randomized to simvastatin (25 female and 20 male used 40 mg simvastatin daily) or placebo (30 female and 20 male) group. After six months, simvastatin significantly lowered CRP levels by 19%, (p<0,01), cholesterol levels by 18%, TG levels by 8%, LDL levels by 20% and VLDL levels by 17%, whereas there was no change with placebo. After one year the difference sustained between groups. Coronary events were rarely in the simvastatin group (6,6%) than in the placebo group (14%). Coronary revascularizations were 4 in the placebo group and 1 in the simvastatin group. Rate of stroke was more often in the placebo group (18%) than in the simvastatin group (8,8%). So, reduction of acute CHD events is for 7,4% in the simvastatin group. Positive correlation was between CRP and CVD (r=0,29). Statin therapy reduced the risk of coronary hearth disease in diabetics without CHD.
Keywords: statin, diabetes mellitus type 2, coronary heart disease, CRP, cholesterol, primary prevention
INTRODUCTION
Diabetes mellitus type 2 is resulting from the interaction of obesity, inflammation, and hyperglycaemia. Activated immunity and cytokine production lead to insulin resistance and other components of the metabolic syndrome, establishing the link between diabetes and atherosclerosis. Hyperglycaemia-induced endothelial dysfunction is mediated by increased oxidative stress, a promoter of adventitial inflammation and vasa vasorum neovas-cularisation in experimental models of diabetic atherosclerosis. Recent studies have documented increased inflammation, neovascularisation, and intraplaque haemorrhage in human diabetic atherosclerosis (1). This inflammatory microangiopathic process is independently associated with plaque rupture, leading to coronary thrombosis. Tissue factor, the most potent trigger of the coagulation cascade, is increased in diabetic patients with poor glycemic control. Circulating tissue factor micro particles are also associated with apoptosis of plaque macrophages, closing the link among inflammation, plaque rupture, and blood thrombogenicity. High-density lipoproteins, responsible for free cholesterol removal, are reduced in patients with insulin resistance and diabetes. High-density lipoprotein therapy leads to a significant decrease in plaque macrophages and increase in smooth-muscle cells. These beneficial effects may be responsible for coronary plaque stabilization in patients treated with recombinant Apolipoprotein A-I Milano/ phospholipid complex. Finally, peroxisomal proliferators-activated receptors (PPARs) are now considered the nuclear transcriptional regulators of atherosclerosis. Three subfamilies, including PPAR-alpha, -delta, and -gamma, have been identified with crucial roles in lipid metabolism, plaque inflammation, expression of adhesion molecules and cytokines, and regulation of matrix metalloproteinase’s. Multiple experimental studies have documented plaque stabilization with PPAR-gamma agonists, a group of medications holding great promise in the treatment of diabetes atherosclerosis. Elevated circulating inflammatory markers such as C-reactive protein (2) and interleukin-6 predict the development of type 2 diabetes, and several drugs with anti-inflammatory properties lower both acute-phase reactants and glycaemia (aspirin and thiazolidinediones) and possibly decrease the risk of developing type 2 diabetes (statin). Cardiovascular disease is the most important cause of morbidity and mortality in patients with type 2 diabetes. Statin therapy restores endothelial function in hyperlipidemic patients. Fluvastatin, simvastatin, lovastatin, atorvastatin, and cerivastatin, but not pravastatin, dose-dependently decrease smooth muscle cell (SMC) migration and proliferation. Moreover, statins are able to reduce cholesterol accumulation in macrophages in vitro by blocking cholesterol esterification and endocytosis of modified lipoproteins and matrix-degrading enzyme secretion (3). In 2004, the NCEP ATP III update recognized that not all patients with diabetes have a >20% 10-year risk for CHD; some patients with diabetes may have a moderate rather than a high risk for the disease (4). The American Diabetes Association (ADA) guidelines recommend statin therapy in the majority of patients with diabetes (5). Four large studies (which included a significant number of patients with diabetes and no history of CHD) have affected treatment guidelines, despite various flaws in their designs and some no significant results (6). While the authors of the Collaborative Atorvastatin Diabetes Study (CARDS) rationalized that statins are indicated for the primary prevention in the majority of patients with type 2 diabetes mellitus, they proposed that the debate should focus on determining if any patients with diabetes are at sufficiently low risk to withhold statin therapy (7). The authors of the Atorvastatin Study for Prevention of Coronary Heart Disease Endpoints in Non-Insulin-Dependent Diabetes Mellitus (ASPEN) suggested that a lower-risk primary prevention cohort would be expected to show less benefit from statin therapy (8).
We aimed to determine whether the administration of statins to type 2 diabetics without pre-existing coronary heart disease reduced the incidence of coronary heart disease and their effects on cholesterol and CRP levels.
PATIENTS AND METHODS
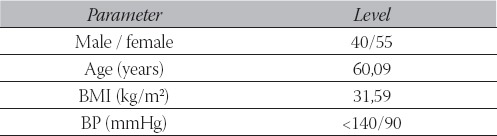
All the participants were carefully interviewed, clinically examined, and laboratory tested to exclude conditions likely to provoke an inflammatory response that was an exclusion criterion. Exclusion criteria: Serious heart, liver or kidney problems, history of renal transplant, recent history of drug or alcohol abuse, HbA1c >10%, blood pressure higher than 140/90mmHg, BMI >35 kg/m2, triglycerides >3,0mmol/dm3. In line with accepted guidelines, the LDL cholesterol level was used as a criterion for entry into the study. Ninety-five obese patients with type 2 diabetes mellitus (mean age 60,9 years and mean BMI=31,59 kg/m2, diabetes duration more than 10 years) without pre-existing coronary heart disease, were included in the analysis of data and were randomized to simvastatin (n=45, 25 female and 20 male used 40 mg simvastatin daily) or placebo (n=50, 30 female and 20 male) group (Table 1).
TABLE 1.
Baseline characteristics
All the subjects were matched for age, sex, body mass index, blood pressure, and smoking habits. Laboratory measurements were checked every three months and that included serum levels of TC, TG, HDL-C, LDL-C, VLDL-C, plasma CRP level, HbA1c and basal C-pep- tide. Vascular disease was considered to be present if there was evidence of angina, intermittent claudication, stroke, transient ischemic attack, and ECG abnormalities according to the Minnesota code. We evaluated incidence of acute coronary heart disease events, coronary revascularisation, or stroke in both group during one year period. The Centres for Disease Control and Prevention and AHA recommended using CRP as marker for primary prevention of major cardiovascular events. As proposal of that association, level of CRP classified to three categories: 1) < 1 mg/cm3 = low risk; 2) 1-3 mg/cm3 = mild risk; 3) > 3 mg/cm3 high risk. Coronary screening clinics were established in Clinic for endocrinology, diabetes and metabolism diseases and in Heart Centre. The subjects were seen at every three-month intervals, and dietary advice was reinforced on each occasion. A fasting lipoprotein profile and CRP was obtained every three months, and an ECG was recorded annually or as required clinically. All ECG results were verified by visual inspection. All laboratory analyses were conducted at the Central Laboratory at the University of Sarajevo Clinics Centre. Student’s T-test, percentile and correlation was performed in statistical analysis.
RESULTS
In the beginning of study lipoproteins profile and CRP level [5,73 ± 2,02 vs. 5,29 ± 2,05 mg/dm3; p>0,05] were similar in both group. Mean CRP-levels were 5,66 mg/ cm3. More than 66% subjects had CRP > 3 mg/cm3, which those classified across AHA in category with high risk for atherosclerosis. Thirty four percent of diabetics had medium risk for atherosclerosis with CRP from 1 to 3 mg/cm3. In investigated groups no any subjects with CRP <1 mg/cm3/low risk for atherosclerosis. No significant difference among two groups pro basal C-peptide as well, (1232±115 pmol/dm3 vs. 1189 ±129 pmol/dm3, p>0,05). Mean total cholesterol was 6,29±1,17 mmol/ dm3, mean level of triglycerides was 2,59 2 ±0,62 mmol/ dm3, and HDL-cholesterol 1,0 mmol/dm3 (Table 2).
TABLE 2.
The laboratory changes in the simvastatin group
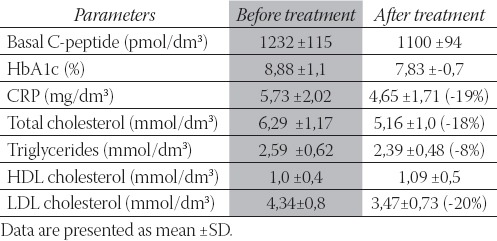
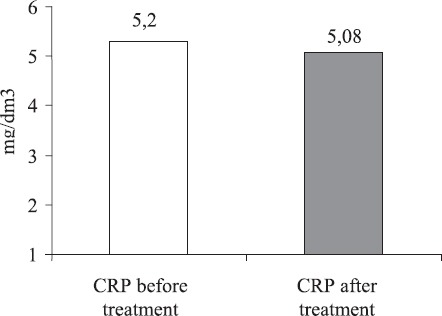
Among 64% patients have total cholesterol > 5,2 mmol/ dm3. At 63% subjects the triglycerides concentrations were >1,8 mmol/dm3, while at 71% HDL-cholesterol concentration was low. Mean HbA1c was 8,88%. Bad glucoregulation with HbA1c > 8% was in more than 60% of subjects (p<0,001). On 18% diabetics HbA1c was from 6,1 to 7,0%, and on 22% HbA1c was from 7,1 do 8,0%. After six months simvastatin significantly lowered CRP levels by 19% (Figure 1), (p<0,01), cholesterol levels by 18%, TG levels by 8%, LDL levels by 20% and VLDL levels by 17%, whereas there was no change with placebo (Table 3 and Figure 2).
FIGURE 1.
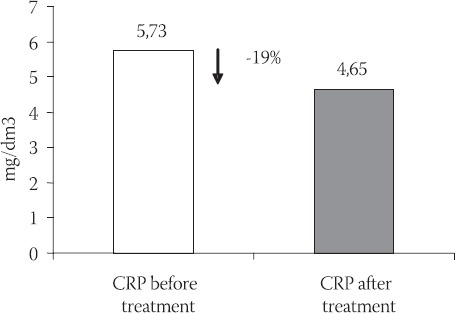
CRP reduction in simvastatin group (-19%)
TABLE 3.
The laboratory changes in the placebo group
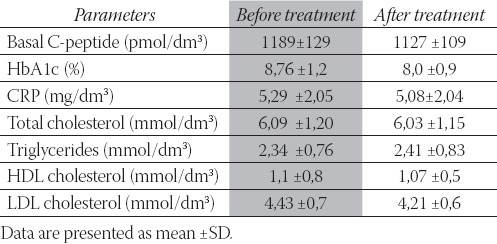
FIGURE 2.
CRP reduction in placebo group
After one year the difference sustained between groups. At diabetics who have the highest level of CRP and fasting insulin cardiovascular diseases were frequently. Coronary events were rarer in the simvastatin group (n=3; 6,6%) than in the placebo group (n=7; 14%) (Figure 3).
FIGURE 3.
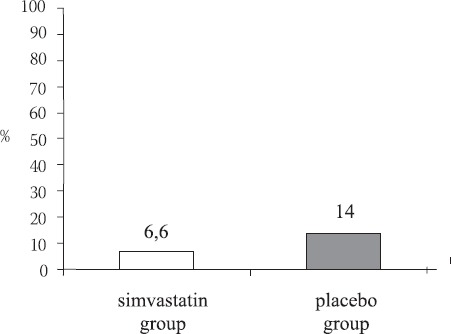
Frequency of coronary events
Coronary revascularizations were 4 (8%) in the placebo group and 1 (2,2%) in the simvastatin group (n=1; 2,2%). Rate of stroke were often in the placebo group (n=9; 18%) than in the simvastatin group (n=4; 8,8%). So, reduction of acute coronary heart disease events is for 7,4% and rate of stroke for 9,2% in the simvaststin group. We found positive correlation between CRP and total cholesterol (r=0,49, P<0,05) and negative correlation between CRP and HDL levels (r=-0,39, P<0,05). CRP correlated significantly with basal C-peptide (r=0,60) and with BMI (r=0,79). Positive correlation was between elevated CRP and CVD (r=0,29). We found a significant interaction between the presence of diabetes and the effect of pre-treatment with statins on cardiovascular diseases.
DISCUSSION
The study results showed reduction of acute coronary heart disease events for 7,4% and rate of stroke for 9,2% in the simvastatin group. The Heart Protection Study (HPS) results questioned the proposal that patients with diabetes and no history of CHD have the equivalent risk for a vascular event as those with pre-existing CHD (9). In addition to significantly reducing the risk of first major vascular events by 24% in all patients and by 22% in patients with diabetes (both p<0,0001), sim-vastatin 40 mg decreased the rate of all major vascular events (first and subsequent) in these patients during the five-year follow-up. HPS investigators concluded that cholesterol lowering with statin therapy is generally efficacious in patients with diabetes, including those without CHD and with relatively low LDL-C levels (10). The results of the overall ASCOT-LLA (Anglo- Scandinavian Cardiac Outcomes Trial Lipid-Lowering Arm) demonstrated a benefit with atorvastatin therapy, but the type 2 diabetes mellitus subgroup did not demonstrate a significant benefit. While it is possible that a significant benefit in the primary endpoint could have occurred among patients with type 2 diabetes mellitus if the trial had continued for the full five years, it cannot be concluded that a benefit would have existed (11). The Collaborative Atorvastatin Diabetes Study (CARDS), a double-blind randomised placebo-controlled trial, assessed primary prevention with atorvastatin 10mg daily in 2,838 patients with type 2 diabetes and at least one additional risk factor (smoking, microalbuminuria, retinopathy or hypertension) (12). Participants were aged 40 years or above (mean age around 62 years) and had a serum LDL-C concentration of 4,14 mmol/dm3 or lower; 68% were male. The LDL-C concentration was reduced more with atorvastatin (mean reduction 1,20 mmol/dm3 greater than with placebo, 95% CI 1,17-1,23, p<0,0001). ASPEN, originally designed as a randomized, double-blind, placebo-controlled analysis that was conducted in a large patient population (n = 2410) with type 2 diabetes mellitus and a history of CHD, compared atorvastatin 10 mg daily with placebo (8). The ASPEN results were not statistically significant, demonstrating no significant difference in primary and individual end-points for all patients in either the primary or secondary prevention subgroup. In the primary prevention subgroup of patients, there was a no significant reduction of fatal CHD plus nonfatal MI and stroke (fatal or non-fatal); however, there was a trend toward increased CV mortality risk. On the basis of these findings, type 2 diabetes mellitus may not be considered a true risk equivalent to CHD. The Antihypertensive and Lipid-Lowering treatment to prevent Heart Attack Trial (ALLHAT) was a non-blinded randomised controlled trial designed to compare classes of antihypertensive drugs in patients aged 55 years or older with hypertension and at least one additional risk factor; 51% were male (13). Pravastatin reduced LDL-C concentration by 0,4 mmol/dm3 more than placebo. The German Diabetes and Dialysis Study (4D), a double-blind randomised placebo-controlled trial, assessed atorvastatin 20mg daily in 1,255 patients with type 2 diabetes and nephropathy requiring maintenance haemodialysis (a group at very high risk of developing cardiovascular disease) (14). After a mean follow-up of around 4 years, atorvastatin had lowered the LDL cholesterol concentration (by a mean of around 0,6mmol/L more than with placebo), but not the likelihood of cardiovascular death, non-fatal coronary events or stroke (the primary endpoint: 37% with atorvastatin vs. 38% on placebo; p=0,37). Currently, ADA recommends that for people over the age of 40 years without overt CVD, statin therapy should be initiated to achieve an LDL-C reduction of 30-40% regardless of baseline LDL-C levels (5). This treatment is prudent in diabetic patients with known CV risk factors or markedly increased LDL-C concentrations (>130 mg/100cm3), regardless of the presence of CVD; however, the question still remains as to whether statin therapy should be initiated in all patients with diabetes in the absence of other CV risk factors and an LDL-C concentration of <130 mg/100cm3. The National Institute for Health and Clinical Excellence (NICE) recommends statin therapy for primary prevention of cardiovascular disease in people with type 2 diabetes in whom, clinically, the cardiovascular disease risk has been estimated to be at least 20% over 10 years.
The cardiovascular diseases were often in aged diabetics. The mean age of patients was 60,9 years. The 85,5% of participants have high body weight. More than 60% of subjects have bad glucoregulation with HbA1c > 8% (p<0,001). Among 64% patients have total cholesterol > 5,2 mmol/dm3. At 63% subjects the triglycerides concentrations were >1,8 mmol/dm3, while at 71% HDL-C concentration was low. More than 66% subjects had CRP > 3 mg/cm3, which those classified across AHA in category with high risk for atherosclerosis. CRP concentrations statistical significantly correlated with coronary diseases (r=0,29; p<0,05), with HbA1c (r=0,34), and with total cholesterol (r=0,49), as well. Results showed negative correlation between CRP and HDL-cholesterol (r =-0,39). Similar results showed moreover study (15). Except cholesterol concentrations and CRP levels may helped to choice patients for statins treatment. Force/ Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS), investigated relationship between LDL-cholesterol and CRP (16). That explained as 50% patients with acute coronary syndrome in USA have normal LDL-cholesterol and high CRP. Therefore, CRP determination needs to be in the patients with middle coronary risk (10-20% during 10 years).
CONCLUSION
Treatment with statins reduced the risk of coronary events in diabetics without CHD. The frequency of the need for coronary angiography and revascularization procedures was significantly lower in the simvastatin group than in the placebo group. Except cholesterol concentrations and CRP levels may helped to choice patients for statins treatment. Elevated CRP in association with high insulin is a significant cardiovascular risk in type 2 diabetics. CRP determination needs to be in the patients with middle coronary risk.
List of Abbreviations
AHA - American Heart Association
BMI - Body Mass Index
BP - Blood Pressure
CHD - Coronary Heart Disease
CVD - Cardiovascular Disease
CRP - C - reactive protein
HDL-C - High-Density Lipoprotein Cholesterol
LDL-C - Low-Density Lipoprotein Cholesterol
PPAR - Peroxisomal proliferators-activated receptors
TC - Total Cholesterol
TG - Triglycerides
VLDL - Very Low-Density Lipoprotein Cholesterol
REFERENCES
- 1.Ross R. Atherosclerosis-an inflammatory disease. N. Engl. J. Med. 1999;340(2):115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 2.Ridker P.M, Rifai N, Rose L, et al. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N. Engl. J. Med. 2002;347:1557–1565. doi: 10.1056/NEJMoa021993. [DOI] [PubMed] [Google Scholar]
- 3.Bellosta S, Ferri N, Arnaboldi L, Bernini F, Paoletti R, Corsini A. Pleiotropic effects of statins in atherosclerosis and diabetes. Diabetes-Care. 2000;23(Suppl 2):lB72–78. [PubMed] [Google Scholar]
- 4.Grundy S.M, Cleeman J.I, Bairey Merz C.N, Brewer B, Jr, Clark L.T, Hunninghake D.B, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–239. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association. Standards of medical care for patients with diabetes mellitus (position statement) Diabetes Care. 2006;29:S4–42. [PubMed] [Google Scholar]
- 6.Riche D.M, McClendon K.S. Role of statins for the primary prevention of cardiovascular disease in patients with Type 2 diabetes mellitus. Am. J. Health-Syst. Pharm. 2007;64(15):1603–1610. doi: 10.2146/ajhp060397. [DOI] [PubMed] [Google Scholar]
- 7.Colhoun H.M, Betteridge D.J, Durrington P.N, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet. 2004;364:685–696. doi: 10.1016/S0140-6736(04)16895-5. [DOI] [PubMed] [Google Scholar]
- 8.Knopp R.H, D’Emden M, Smilde J.G, et al. Efficacy and safety of atorvastatin in the prevention of cardiovascular end points in subjects with type 2 diabetes: the Atorvastatin Study for Prevention of Coronary Heart Disease Endpoints in Non-Insulin-Dependent Diabetes Mellitus (ASPEN) Diabetes Care. 2006;29:1478–1485. doi: 10.2337/dc05-2415. [DOI] [PubMed] [Google Scholar]
- 9.Wood D. Heart Protection Study, Lancet 2002; 360. 7-22. J Hypertens. 1998;16:1407–1414. [Google Scholar]
- 10.Law M.R, Wald N.J, Rudnicka A.R. Quantifying effect of statins on low density lipoprotein cholesterol, ischemic heart disease, and stroke: systematic review and metaanalysis. B.M.J. 2003;326:1423. doi: 10.1136/bmj.326.7404.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sever P.S. Reduction in cardiovascular events with atorvastatin in 2,532 patients with type 2 diabetes. Anglo-Scandinavian Cardiac Outcomes Trial-Lipid-Lowering Arm (ASCOT-LLA) Diabetes Care. 2005;28:1151–1157. doi: 10.2337/diacare.28.5.1151. [DOI] [PubMed] [Google Scholar]
- 12.Colhoun H.M, Betteridge D.J, Durrington P.N, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorva-statin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet. 2004;364:685–696. doi: 10.1016/S0140-6736(04)16895-5. [DOI] [PubMed] [Google Scholar]
- 13.ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in moderately hypercho-lesterolemic, hypertensive patients randomized to pravastatin vs. usual care: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT-LLT) J.A.M.A. 2002;288:2998–3007. doi: 10.1001/jama.288.23.2998. [DOI] [PubMed] [Google Scholar]
- 14.Wanner C. Atorvastatin in patients with type 2 diabetes mellitus undergoing haemodialysis. N. Engl. J. Med. 2005;353:238–248. doi: 10.1056/NEJMoa043545. [DOI] [PubMed] [Google Scholar]
- 15.Ridker P.M. Rosuvastatin in the primary prevention of cardiovascular disease among patients with low levels of low-density lipoprotein cholesterol and elevated high-sensitivity C-reactive protein: rationale and design of the JUPITER trial. Circulation. 2003;108:2292–2297. doi: 10.1161/01.CIR.0000100688.17280.E6. [DOI] [PubMed] [Google Scholar]
- 16.Gotto A.M, Jr, Whitney E, Stein E.A, Shapiro D.R, Clearfield M, Weis S, et al. Relation between baseline and on-treatment lipid parameters and first acute major coronary events in the Air Force/Texas Coronary Atherosclerosis Prevention Study (AF-CAPS/TexCAPS) Circulation. 2000;101:477–484. doi: 10.1161/01.cir.101.5.477. [DOI] [PubMed] [Google Scholar]


