Abstract
Primary skin melanoma and skin cancers have been more prevalent in the previous decades and therefore have become a very significant public health problem. Dermatologists of the Skin and Venereal Diseases Clinic of the University of Sarajevo Clinics Centre initiated the first public preventive action called “Days of Fighting Melanoma” in May 2008. The objective of the campaign was to provide free dermatological examinations to all volunteers and to inform, through the media, wider population on early signs and recognition of skin cancer and the importance of sun protection. The total of 325 citizens were examined clinically and with dermatoscope in the period between 5 and 31 May 2008. The examination also included histological diagnoses: 7 patients with confirmed melanoma, 30 with basal cell carcinoma and 2 with spinocellular carcinoma. The results suggested a need for the expansion of the campaign to other towns in our country in order to demonstrate the importance of early detection of the disease and treatment options.
Keywords: melanoma, skin cancer, screening, prevention
INTRODUCTION
Prevalence of malignant skin tumours constantly increases whereas malignant melanoma is the most prevalent in comparison with other types. Incidence of malignant melanoma in Europe fluctuates in the range 4-14 patients per 100 000 inhabitants (1). Eti-olopathogenesis involves several factors; however, sun rays have been established as the most important external etiological causes of initiation, stimulation and ultimate development of skin tumours (2). Over the last couple of years an increase in the numbers of patients has been noted among our population (3), thus a need for initiation of a public health preventive action aimed at early detection of skin cancers and melanoma arose. The aim of this massive preventive campaign was to inform, make aware and warn wider public of Bosnia and Herzegovina on risks of detrimental effects of sun rays and consequences that are evident as an increase of frequency of patients with skin cancers (basal cell and squamous cell carcinoma). Amongst those, malignant melanoma is the most malignant of all.
MATERIALS AND METHODS
Within the public health preventive action “Days of Fighting Melanoma” free preventive dermatological examinations of citizens were organized and advertised in the media one month in advance. The examinations were conducted at the Clinic for Skin and Venereal Diseases of the University of Sarajevo Clinics Centre in the period between 5th and 31st May. Firstly, all the volunteers were physically examined (inspection of entire skin surface, skin adnexa, visible mucosa and semimucosa as well as palpation of lymph nodes). Suspicious lesions were examined with a dermatoscope, thereafter the patients were referred to further treatment. The screening included a photo-type of patients, type and abundance of moles, actinic keratosis, keratoa- canthoma, basal cell and squamous cell carcinoma, melanoma and other malignant skin tumours. Surgically removed and histologically verified tumours were retrospectively analyzed as shown in the Results below.
Over the period between 5th and 31st May 2008 the total of 325 citizens were examined. Almost two thirds of the examined patients were women. The age of patients ranged from 4-88, whereas the average age was 49,5 years. Majority of patients subjected to the screening belonged to the working age group of citizens, however almost 90% of patients conducted their work in an enclosed space.
RESULTS
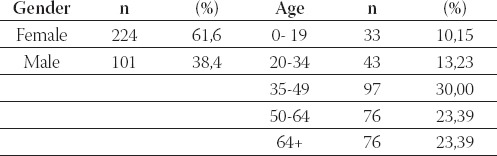
The results of our study are given in the following tables. Table 1. illustrates demographic structure of the examined group. In the period between 5th and 31st May 2008 a total of 325 citizens were examined. Almost two thirds of the examined patients were women, 224 cases. The age of subjects ranged from 4-88, whereas the average age was 49,5 years. Majority of patients involved in the screening were of the working age group of inhabitants, however almost 90% of performed their work in an enclosed space.
TABLE 1.
Demographic distribution of the screened population
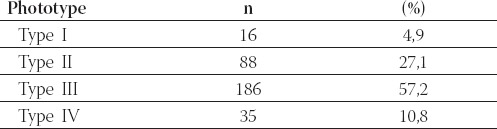
As presented in Table 2., the dominant skin type was type III, i.e. more than one half of the examined patients had light brown or brown hair, fair complexion, and they rarely sustained sun burns and almost always acquired suntan after exposure to sun. Most of them have never or only occasionally used protective creams or lotions and a half of them have sustained two to three episodes of sun burns by the age of 20. Majority of the examined patients sustained serious sun burn at least once in their life, according to anamneses.
TABLE 2.
Respective prototypes
Physical and subsequent dermatoscopic examination and pathohistologic report verified 30 cases of basal cell carcinoma (18,3%) and 2 spinocellular (0,6%) carcinoma. Majority of patients with skin cancer were male (M:F=1,6:1) aged between 70 and 80 years, whereas none of the patients was younger than 43. Three patients had a positive anamnesis for previously treated skin cancer. Four patients with average age of 76 years (1,2%) (three men and a woman) had histologically verified keratoacanthoma whereas 5 patients (1,5 %) had actinic keratosis. Following the physical examination 52 patients (16%) were found with one or more dysplastic nevi and Atypical Mole Syndrome, based on anamnesis and clinical examination, was found in 5 patients only (1,5%).
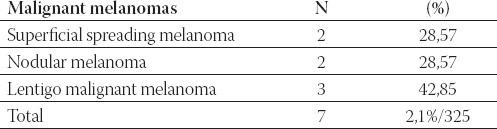
Table 3. shows the total number of histologically verified melanoma and their histological subtypes. Patients with histologically verified melanoma were older than 60 and their average age was 68,8 years. Five patients were female and two male, i.e. ratio M:F=1:2,5. Average tumour thickness (Breslow’s Index ranged from 0,1-5 mm) was 2,52 millimetres. Anatomic localization in both cases of nodular melanoma was trunk, in cases of superficial spreading melanoma the localization was in lower legs, whereas the face was the melanoma site in malignant lentigo.
TABLE 3.
Histological subtypes of melanomas within the histologi-cally verified group
DISCUSSION
According to the “Euro Melanoma Day” model, dermatologists working at the Clinic for Skin and Venereal Diseases of the University of Sarajevo Clinics Centre, initiated the first preventive public health campaign titled “Days of Fighting Melanoma” using a slogan “Pay more attention to sun protection”. Malignant melanoma etiopathogenesis involves several factors. Intermittent sunbathing is connected with the occurrence of sun burns in childhood (particularly before the age of 14) and adolescence and it plays a very important role in the development of melanoma, as in that life period almost 80% of UV radiation is absorbed (4,5). Skin types 1 and 2 according to Braun-Falco, and individual genetic predisposition are important endogenic factors (2).
Malignant melanoma has the highest incidence as compared to all other skin cancers and in some parts of the world it exhibits certain characteristics of an epidemic. Around 8,000 people develop malignant melanoma in Great Britain with fourfold increase of incidence in men and threefold in women over the period 1975 - 2001, mostly among Caucasians. An increase in incidence has been noted in Europe in the age group 25-49 and amounts to 2%-3% in the North and up to 8% in the South Europe every year (6).
An average age (mean) for the development of melanoma was 68,8 years. Mean age for the malignant melanoma development indicated in the references is 53 (8), which is almost identical to the result of a study covering the ten-year period (1996-2006) in the area of Zenica-Doboj Canton (3). In a study conducted by Nola et al. it was 57 years (8), and according to the results of a similar campaign from Greece for the period 2000-2004 the mean age was 54 (9). The average age of the subjects examined within this study is 49,5, which is comparable with the results of similar campaigns conducted in Croatia and Greece (9,10). Breslow’s Index, i.e. average thickness of melanoma was 2,5 mm (medium thick and thick melanoma), with moderately bad and bad prognostic index. There were also cases of melanoma in situ, and so called thin melanoma. In similar campaigns tumours were mainly of the so called thin melanoma type (Breslow’s Index less or equal to 1.5 mm), whereas the most prevalent histological type was superficially spreading melanoma (10,11).
Basal cell and spinocellular skin cancers are among the most frequent non-melanoma tumours in white people and they make 19% of all the malignant tumours in men and 11% in women (12). In the last decade a continuous increase in the incidence has been noted, particularly of basal cell cancer in white people, which scientists connect with the depletion of Ozone layer and partly with changed life style and habits. More than 90% of skin cancers are caused by UV radiation emitted by the Sun and they are located in the regions of skin exposed to sun (13). The results of this preventive action have shown that basal cell carcinoma is the most prevalent skin cancer in white people and confirmed the fact that they most frequently occur after the age of 40. The most frequent histological type was the solid type followed by equally prevalent ulcerous and pigmented basalioma. The frequency of spinocel-lular carcinoma (0,5%-1%) was almost equal to the one found in other similar campaigns (9,10). The results related to skin precancers were also similar (9,10,11).
Primary skin cancer prevention includes identification, prevention and removal of risk factors whenever possible. The most important external factor is ultraviolet radiation emitted by the Sun with wavelength 250 nm to 350 nm, i.e. so called UVA and UVB rays (2). The following primary preventive measures are recommended: avoid intentional sunbathing and recreational activities in open space in the period between 10 and 16 hours, apply physical sun protection wearing appropriate clothes and protect skin by protective SP factor 15 or higher, depending on the photo-type, 15 minutes before leaving into an open space.
Secondary skin cancer prevention involves, as in other malignant diseases, the application of appropriate screening method(s) for identification of potential patients (14). All the volunteers had an opportunity to undertake dermatoscopic examination, a non-invasive diagnostic procedure for early detection of tumours, and/or identification and screening of suspicious pigmented and non-pigmented lesions in order to conduct prophylactic or diagnostic and surgical procedures or other therapeutic procedures.
CONCLUSION
The results of the first preventive public health action “Days of Fighting Melanoma” have undoubtedly indicated a need for continuous education of a wider population through the media and by printing appropriate educational brochures in order to emphasize a possibility of early detection and treatment of the disease.
The American Cancer Society recommends self-examination of skin once a month and, for those with increased risk, skin examination should be a part of regular general examinations.
REFERENCES
- 1.Pašić A, Maligni melanom U. Lipozenčić J. i sur. Dermatovener-ologija. Zagreb: Medicinska naklada; 2005. pp. 493–494. [Google Scholar]
- 2.Braun-Falco O, Plewing G, Wolff HH, Winkelmann RK. In: Malignant melanoma. Dermatology. Braun-Falko O, Plewing G, Wolff HH, Win-kelman RK, editors. Berlin: Springer-Verlag; 2000. pp. 1531–1548. [Google Scholar]
- 3.Drljević I. Influence of detrimental radiation of sunrays on an increase in malignant melanoma and non-melanoma malign skin tumours. Sarajevo: University of Sarajevo; 2006. Master Thesis. [Google Scholar]
- 4.Stanec S, Šitum M, Epidemiologija melanoma U, Stanec S, Šitum M. i sur. Melanom-protokol liječenja. Zagreb: Znanje; 2003. p. 9. [Google Scholar]
- 5.Walter S.D, Marrett L.D. Association of cutaneous malignant melanoma with intermittent exposure to ultraviolet radiation: results of a case-control study in Ontario, Canada. Int. J. Epidemiol. 1999;199:418–427. doi: 10.1093/ije/28.3.418. [DOI] [PubMed] [Google Scholar]
- 6.Cancer-Research UK. UK Malignant melanoma statistics. 2006. [accessed: 23.08.2008]. http://info.Cancer researchuk.org/cancerstats/types/melanoma/
- 7.Swatter S. Malignant Melanoma. Emedicine. 2005. [accessed: 28.09.2008]. http://www.emedicine.com/derm/topic257.htm .
- 8.Nola I, Krušlin B, Muller D, Oremović L, Belicza M. The rise in the melanoma incidence in Croatia. Acta Dermatovenerol. Croat. 2002;10:3–7. [PubMed] [Google Scholar]
- 9.Stratigos A, Nikolaou V, Kedicoglou S, Antoniou C, et al. Melanoma/skin cancer screening in a Mediterranean country: results of the Euromelanoma Screening Day Campaign in Greece. J Eur. Acad. Dermatol. Venerol. 2006;21(1):56–62. doi: 10.1111/j.1468-3083.2006.01865.x. [DOI] [PubMed] [Google Scholar]
- 10.Rezultati javno-zdravstvene oreventivne akcije: “Dani borbe protiv melanoma”-Oktal Pharma. 2008. [accessed: 04.11.2008]. http://www.oktal-pharma.hr/hr/content/display/177 .
- 11.Landi M.T, Baccarelli A, Calista D, et al. Combined risk factors for cutaneous melanoma in a Mediterranean population. Br. J. Cancer. 2001;85:1304–1310. doi: 10.1054/bjoc.2001.2029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Obralić N, Tumori kože U, Mušanović M, Obralić N. Onkologija. Sarajevo: Bošnjački institut; 2001. pp. 175–180. [Google Scholar]
- 13.Kitchner S. Epidemilogy of melanoma. In: Soyer H.P, editor. Colour Atlas of Melanocytic Lesions of the Skin. Berlin: Springer-Verlag; 2007. pp. 185–195. [Google Scholar]
- 14.Ebling Z. Sekundarna prevencija raka. U: Šamija M. i sur., ur Onkologija. Zagreb: Medicinska naklada; 2000. pp. 449–455. [Google Scholar]


