Abstract
AIM
To reduce readmissions and improve patient outcomes in cirrhotic patients through better understanding of readmission predictors.
METHODS
We performed a single-center retrospective study of patients admitted with decompensated cirrhosis from January 1, 2011 to December 31, 2013 (n = 222). Primary outcomes were time to first readmission and 30-d readmission rate due to complications of cirrhosis. Clinical and demographic data were collected to help describe predictors of readmission, along with care coordination measures such as post-discharge status and outpatient follow-up. Univariate and multivariate analyses were performed to describe variables associated with readmission.
RESULTS
One hundred thirty-two patients (59.4%) were readmitted at least once during the study period. Median time to first and second readmissions were 54 and 93 d, respectively. Thirty and 90-d readmission rates were 20.7 and 30.1 percent, respectively. Predictors of 30-d readmission included education level, hepatic encephalopathy at index, ALT more than upper normal limit and Medicare coverage. There were no statistically significant differences in readmission rates when stratified by discharge disposition, outpatient follow-up provider or time to first outpatient visit.
CONCLUSION
Readmissions are challenging aspect of care for cirrhotic patients and risk continues beyond 30 d. More initiatives are needed to develop enhanced, longitudinal post-discharge systems.
Keywords: Chronic disease, Re-hospitalizations, Liver disease, Readmissions, Cirrhosis, Chronic care
Core tip: To reduce readmissions and improve patient outcomes, we conducted a retrospective cohort study of 222 decompensated cirrhotics admitted to a single institution and followed longitudinally for readmission. Nearly 60% were readmitted during the study, with hepatic encephalopathy as the most common cause of readmission, with social factors, education level and insurance, also affecting readmission rates. We also found that readmission risk in this population continues well beyond 30 d, with 30% of patients being readmitted at 90 d, calling for continued, coordinated care after hospitalization.
INTRODUCTION
Cirrhosis is the second most common digestive disease cause of death and 12th overall cause of death in the United States[1]. Cirrhosis and complications of cirrhosis account for around 40000 deaths in the United States annually, similar to diabetes and slightly more than kidney diseases, with a mortality rate of 25.7 deaths per 100000 people[2,3]. In addition to high mortality, cirrhosis and its complications are the cause of many high-cost hospitalizations. One study in 2002 showed that cirrhosis accounts for 150000 hospitalizations in the US, with an estimated single hospital admission cost of $15000 and a total estimated cost of $4 billion annually[2]. A more recent study found that 37% of patients with decompensated cirrhosis were readmitted within one month of discharge at a cost of roughly $20000 per admission[4]. The additional burdens of disease, including lost days of work, diminished quality of life, and health care costs are difficult to measure.
In the current value-based healthcare landscape, hospitals will be increasingly held financially accountable for readmissions under value-based care programs. Moreover, no evidence-based systems have been developed to reduce readmission rates in most chronic disease conditions. Providers and health systems face challenges, as the current body of literature lacks data on effective chronic disease care management for cirrhosis, and our current episodic system of health care delivery is insufficient to tackle this issue. Factors associated with readmissions in decompensated cirrhosis in previous works include Model for End-Stage Liver Disease (MELD), diabetes, nosocomial infections, BMI and hepatic encephalopathy[5-7].
Our institution has sought to improve the continuity of care for high-risk patients through post-discharge phone calls, as well as through care management programs for chronic conditions such as heart disease and diabetes. We hope to extend such programs to patients with cirrhosis to improve clinical outcomes and reduce readmissions[8]. We performed this study to better understand and define the predictors of readmission, as well as time to first readmission, in a cohort of patients with decompensated cirrhosis, to better target future programs aimed at reducing readmissions and improving patient outcomes.
MATERIALS AND METHODS
Selection of cohort
We utilized an internal research patient data registry (RPDR), which is a database consisting of 1 billion records encompassing 4.5 million patients from 1988 to the present, to identify our cohort. Data come from multiple sources within 5 major Boston area hospitals, including billing registries and electronic medical records, and contain patient encounters, laboratory test results, imaging, and other clinical data. We searched this database to identify potential subjects by any of the International Classification of Diseases 9 (ICD-9) diagnosis groups or common procedure terminology codes associated with cirrhosis and complications of cirrhosis (Table 1).
Table 1.
ICD-9 codes used to identify patients
| Bleeding from esophageal varices | 456 |
| Esophageal varices in diseases classified elsewhere | 456.2 |
| Spontaneous bacterial peritonitis | 567.23 |
| Alcoholic fatty liver | 571 |
| Alcoholic cirrhosis of liver | 571.2 |
| Laennec's cirrhosis | 571.2 |
| Cirrhosis of liver nos | 571.5 |
| Cirrhosis of liver without mention of alcohol | 571.5 |
| Macro nodular cirrhosis | 571.5 |
| Micro nodular cirrhosis | 571.5 |
| Portal cirrhosis NOS | 571.5 |
| Posthepatitic cirrhosis | 571.5 |
| Post necrotic cirrhosis | 571.5 |
| Cholangitic cirrhosis | 571.6 |
| Cholestatic cirrhosis | 571.6 |
| Hepatic encephalopathy | 572.2 |
| Portal hypertension | 572.3 |
| Hepatorenal syndrome | 572.4 |
| Other sequelae of chronic liver disease | 572.8 |
| Hepatopulmonary syndrome | 573.5 |
| Ascites | 789.5 |
Patients over the age of 18 who were hospitalized due to one of the complications of cirrhosis between January 1, 2011 - December 31, 2013 were included in the initial study cohort. Complications of cirrhosis from Table 1 were grouped into the following categories for analysis: (1) Hepatic encephalopathy (HE), defined as altered mental status due to chronic liver disease and improved after treatment with lactulose; (2) Gastrointestinal bleeding (GIB), defined as a clinically significant bleeding and varices, gastric antral vascular ectasia and portal hypertensive gastropathy seen on endoscopy; (3) Spontaneous bacterial peritonitis (SBP), defined as infection of preexisting ascitic fluid and more than 250 polymorphonuclear cells per high power field and/or monomicrobial culture in the ascitic fluid without evidence for an intra-abdominal secondary source such as a perforated viscus; (4) Volume related, defined as ascites or hepatic hydrothorax requiring paracentesis during the hospitalization. Acute renal failure or hyponatremia was also included in this category; and (5) Other complications defined as hepatorenal syndrome, hepatopulmonary syndrome, hepatocellular carcinoma (HCC) and portal vein thrombosis.
Emergency Department (ED) visits or hospitalizations due to any diagnosis other than complications of cirrhosis were not considered as a readmission. We did not include alcohol-related admissions, such as alcohol withdrawal, as admissions due to complications of cirrhosis. Also, in our institution many patients receive regular large volume paracentesis for ascites in ED visits. These brief encounters were not considered an elective readmission due to decompensation.
Exclusion criteria were advanced extrahepatic malignancy, end stage renal failure, end stage heart failure, patients with prior liver transplant, patients who had no further encounters within our health care system, and patients who died or were placed on hospice within one month from the index hospitalization.
Institutional structure
This study was conducted at a single academic transplant center. Our outpatient liver program includes 7 hepatologists, 31 gastroenterologists not specifically trained in hepatology, and 2 nurse practitioners, as well as an advanced liver fellow. Inpatients patients with liver disease can be admitted to our dedicated liver service but are most often admitted to a general medicine hospitalist service with hepatology or gastroenterology consultation. A majority of our patients are local and live within an hour’s drive or less from the hospital, though patients on the transplant list may come from other parts of New England, such as Maine and New Hampshire, and are seen more regularly as outpatients by local primary care physicians (PCPs) and gastroenterologists.
Collection of baseline data
Medical records for patients meeting the above inclusion criteria were individually reviewed. Baseline variables collected from chart review and RPDR data included age, gender, race, education, health insurance, marital status, MELD scores, laboratory test results, co-morbidities, medications, date of index and subsequent admissions, date of follow-up visits by a PCP or a gastroenterologist, post-discharge setting, smoking history and alcohol use. Admission and discharge MELD scores were calculated based on Mayo Clinic MELD calculator, using creatinine, total bilirubin, and international normalized ratio (INR) extracted closest to the admission and discharge time, respectively[9]. The Charlson Co-morbidity Index (CCI) was also calculated for each patient at index admission[10].
Follow-up time and study outcomes
Patients were followed from the index admission until readmission, death, discharge with hospice care, liver transplantation, loss to follow-up or December 31, 2013, whichever came first. All patients were followed post-discharge for a minimum of 90 d and all readmissions were reviewed. The primary outcomes were time to first readmission and 30-d readmission rate for cirrhosis or a complication of cirrhosis. The secondary outcome was the 90-d readmission rate.
Statistical analysis
Univariate analyses were performed using chi-square or proportional hazard ratio to find predictors of 30-d readmission and time to first readmission. Clinically relevant candidate variables with P < 0.15 were used in Cox proportional hazards regression (for time to first readmission) and logistic regression (for 30 and 90 d readmission rates) models. Due to co-linearity between reason for index admission and medications at discharge, medications at discharge was excluded from the final models. Two-sided P values ≤ 0.05 were considered significant. All statistical analyses were performed using SAS v.9.3. The statistical methods and results of this study were reviewed by biostatistician Han Lee, PhD of Massachusetts General Hospital and Harvard Medical School.
RESULTS
From January 1, 2011 to December 31, 2013, 222 patients were admitted to our center due to one of the complications of cirrhosis and did not meet any of the exclusion criteria. The median time from hospital discharge to end of the study period was 273 d. Baseline characteristics of the study population are presented in Table 2.
Table 2.
Baseline characteristics of cohort (n = 222) n (%)
| Demographics | Number of patients |
| Male | 149 (67.2) |
| White | 168 (76) |
| Married | 82 (36.9) |
| Age | mean ± SD: 56.7 (11.7) |
| Insurance | |
| Private insurance | 81 (36.5) |
| Medicaid or mass health | 74 (33.3) |
| Medicare | 62 (27.9) |
| No Insurance (self-pay/free care) | 5 (2.3) |
| Education | |
| High school/equivalent or less | 127 (57.2) |
| Some college and above | 60 (27) |
| Not recorded | 35 (15.8) |
| Clinical History | |
| Alcohol use | |
| Former heavy use | 110 (49.5) |
| No significant history | 65 (29.3) |
| Current heavy use | 47 (21.2) |
| Smoking | |
| Never smoked | 82 (36.7) |
| Former smoker | 77 (34.7) |
| Current smoker | 63 (28.4) |
| Etiology of cirrhosis | |
| Alcohol | 83 (37.4) |
| HCV or HBV (HCV, n = 46) | 49 (22.1) |
| Combination of etiologies (mainly HCV + alcohol) | 40 (18) |
| NASH | 29 (13) |
| Cryptogenic or other etiologies | 21 (9.5) |
| Co-morbidities (Top 5) | |
| Mental health (Depression or bipolar disorder) | 68 (30.2) |
| Diabetes mellitus | 65 (29.8) |
| Coronary artery disease | 27 (12) |
| Chronic kidney disease | 27 (12) |
| Hepatocellular carcinoma | 24 (10.6) |
HCV: Hepatitis C virus; HBV: Hepatitis B virus.
One hundred thirty-two of these 222 patients (59.4%) were readmitted at least once during the study period. The median time to first readmission, our primary outcome, was 54 d. Thirty and 90-d readmission rates were 20.7 and 30.1 percent, respectively. The most common cause of index admission was one of the volume related conditions (28.8%) while the most common cause of readmission was hepatic encephalopathy (35.5%) (Table 3). The average length of stay for the index hospitalization was 7.2 d, and 88 patients (49.4%) were readmitted with the same complication of cirrhosis.
Table 3.
Hospitalization characteristics n (%)
| Index hospitalization | |
| Complication of cirrhosis at index admission | Number of patients |
| Volume-related | 64 (28.8) |
| Hepatic encephalopathy | 61 (27.5) |
| Variceal bleeding | 54 (24.3) |
| Spontaneous bacterial peritonitis | 27 (12.2) |
| Other or > 1 complication | 16 (7.2) |
| mean ± SD | |
| Length of stay | 7.2 (7.8) |
| MELD at admission | 13.3 (7.7) |
| MELD at discharge | 12.2 (7.5) |
| Readmissions | Number of patients |
| Readmitted with the same complication | 88 (49.4) |
| Readmitted in one month | 46 (20.7) |
| Cause of readmission | |
| Hepatic encephalopathy | 49 (35.5) |
| Volume-related | 38 (27.5) |
| Variceal bleeding | 31 (22.5) |
| Other or > 1 complication | 12 (8.7) |
| Spontaneous bacterial peritonitis | 8 (5.8) |
MELD: Model for end-stage liver disease.
Post-discharge conditions are summarized in Table 4 based on the post-discharge care setting. Patients discharged to a skilled nursing facility, those who left the hospital against medical advice, and homeless patients who were discharged to shelters had more 30-d readmissions but the results were not statistically significant (P < 0.12).
Table 4.
Post-discharge follow-up n (%)
| Number of patients | 30-d readmissions | P value | |
| Post-discharge status | |||
| Home | 120 (54.3) | 19 (15.9) | P < 0.12 |
| VNA | 60 (27.2) | 14 (23.3) | |
| SNF/rehab or LTAC | 30 (13.5) | 8 (26.7) | |
| Eloped | 5 (2.3) | 0 | |
| Shelter | 5 (2.3) | 0 | |
| Mental Institute | 1 (0.4) | 1(100) | |
| Follow-up outpatient visits | |||
| Gastroenterologist | 83 (37.4) | 10 (12.1) | P = 0.9 |
| PCP | 22 (9.9) | 2 (9.1) | |
| Both | 31 (14) | 4 (12.9) | |
| Readmitted before visit | 29 (13.1) | 29 (100) | |
| Total | 165 (74.3) | 45 (27.3) | |
| First post-discharge outpatient follow-up (PCP and/or GI) | |||
| < 2 d | 35 (21.2) | 31 (60.0) | P = 0.1 |
| 2-14 d | 66 (40.0) | 13 (19.7) | |
| > 14 d | 64 (38.8) | 3 (4.7) | |
| Time to visit (d) | Mean ± SD | ||
| Time to first visit by GI | 22.6 (43.7) | ||
| Time to first visit by PCP | 31.9 (35) | ||
| Time to first visit by PCP or GI | 24.7 (33.8) | ||
PCP: Primary care physician; GI: Gastrointestinal.
One hundred sixty five patients out of the 222 index patients (74.3 %) had a follow-up outpatient visit in our institution at some point after index admission (Table 4). The rest of the patients were not seen at our center after discharge and may have had local follow-up. Of those 165 patients seen at our institution, 83 (37.4%) were seen only by a gastroenterologist, 22 (9.9%) only by a PCP and 31 (14%) both by a gastroenterologist and a PCP. The remaining 29 patients had an outpatient visit scheduled post-discharge but were readmitted before the scheduled visit. Among the patients who had a post-discharge follow-up visit at our institution, there was no significant difference in 30-d readmission rates based on the visit by a PCP versus a gastroenterologist or both (P = 0.9).
We further analyzed 30 d readmission rates stratified by time until first post-discharge follow-up visit: < 2 d, 2-14 d, and > 14 d. Thirty five patients (21%) were seen in an office visit within two days after index discharge, 66 (40%) between 2 and 14 d, and 64 (38.8%) after 14 d, but there was no statistically significant difference in the rate of readmission amongst these groups (P = 0.1). The average time between discharge and the first outpatient follow-up appointment was also calculated at 22.6 d for patients seen by a GI specialist, 31.9 d for those who saw a PCP and 24.7 d for those who saw both.
In the univariate time-to-event analysis, the following covariates were associated with time to readmission (P < 0.05): education level, etiology of cirrhosis, MELD score, diagnosis of HE at index admission, history of HCC, and history of depression or bipolar disorder (Table 5). In the multivariate analysis, lower education level, any cirrhosis etiology other than alcohol, higher MELD score, HE at index admission and history of HCC were associated with shorter time to readmission (Table 5). Kaplan-Meier curves for time to readmission stratified by MELD score and etiology of cirrhosis are shown in Figures 1 and 2, respectively. In both the univariate and multivariate analysis of predictors for 30-d readmissions, patients with lower education, HE at index, ALT more than upper limit of normal (ULN) and Medicare patients had higher 30-d readmission rates (P < 0.05) (Table 6). The c-statistic for this test was 0.75.
Table 5.
Predictors of time to readmission
| Variable |
Univariate analysis |
Multivariate analysis |
|||
| HR | P value | HR | P value | ||
| (95%CI) | (95%CI) | ||||
| Education level (ref = Some college and above)1 | 1.00 | 0.02 | 1.00 | ||
| Finished high school and less | 1.64 (1.02-2.46) | 0.02 | 1.56 (0.98-2.46) | 0.05 | |
| MELD category (ref = MELD < 15 ) | 1.00 | 0.007 | 1.00 | ||
| 15 ≤ MELD < 25 | 1.45 (0.97-2.15) | 0.06 | 1.52 (1.00-2.31) | 0.04 | |
| MELD ≥ 25 | 2.51 (1.33-4.75) | 0.004 | 2.51 (1.24-5.11) | 0.01 | |
| Etiology of CLD (ref = Alcohol) | 1.00 | 0.03 | 1.00 | ||
| HCV | 1.74 (1.10-2.76) | 0.03 | 1.73 (1.06-2.82) | 0.02 | |
| NASH/Cryptogenic | 1.25 (0.76-2.05) | 0.36 | 1.81 (1.02-3.18) | 0.04 | |
| Other/Combination of etiologies | 1.94 (1.20-3.11) | 0.006 | 2.02 (1.24-3.29) | 0.004 | |
| History of HCC | 1.85 (1.10-3.08) | 0.01 | 1.67 (0.95-2.93) | 0.07 | |
| HE | 1.51 (1.04-2.16) | 0.01 | 1.61 (1.11-2.40) | 0.01 | |
Education variable was adjusted for unknown status. HCC: Hepatocellular carcinoma; MELD: Model for End-Stage Liver Disease; HCV: Hepatitis C virus.
Figure 1.
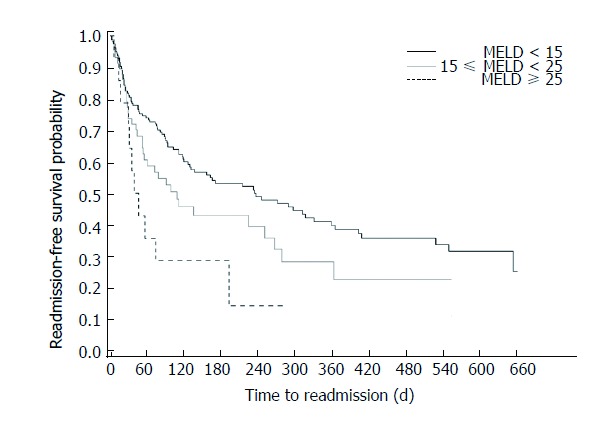
Kaplan-Meier curve for time to readmission stratified by MELD score.
Figure 2.
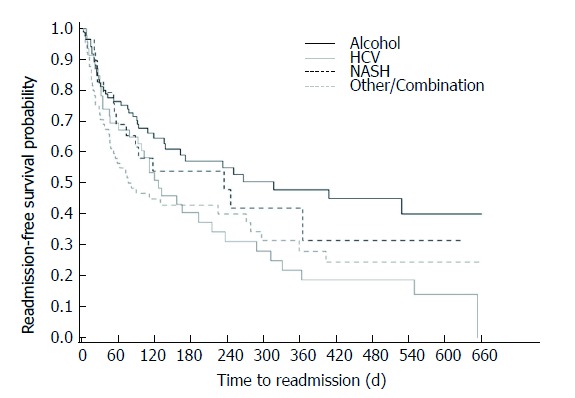
Kaplan-Meier curve for time to readmission stratified by etiology of cirrhosis.
Table 6.
Predictors of 30-d readmission
| Variable |
Univariate analysis |
Multivariate analysis |
||
| OR | P value | OR | P value | |
| (95%CI) | (95%CI) | |||
| Insurance (ref =Medicaid/No insurance) | 1 | 1 | ||
| Medicare1 | 1.8 (1.00 -3.94) | 0.05 | 3.42 (1.3-9.00) | 0.01 |
| Education (ref = Some college and above) | 1.00 | 1 | ||
| Finished high school and less2 | 3.56 (1.40-9.00) | 0.002 | 2.62 (1.01-7.12) | 0.05 |
| ALT > ULN at discharge | 2.52 (1.29-4.89) | 0.006 | 2.29 (1.09-5.11) | 0.03 |
| Hepatic encephalopathy | 2.17 (1.10-4.29) | 0.01 | 2.34 (1.09-4.80) | 0.03 |
Insurance variable was adjusted for patients with private insurance;
Education variable was adjusted for unknown status. ULN: Upper limit of normal.
DISCUSSION
Hospital readmissions are costly and represent opportunities for improvements in quality of care, communication, and coordination. Readmissions are viewed as potentially avoidable and the large payers, such as the United States Department of Health and Human Services Center for Medicare and Medicaid Services Readmission Prevention Program penalizes hospitals for higher than expected readmissions for heart failure, myocardial infarction and pneumonia. As healthcare moves towards value-based payment methods, primary care and specialists alike must prepare to better organize care for the highest risk and highest cost patients. Understanding the attributes of patients and causes for readmission is the foundation for designing strategies to mitigate the economic losses and prevent clinical morbidity. Additionally, while the current 30-d readmission threshold is appropriate for discrete admission events, such as surgery, applying this model to a chronic disease population may not capture true readmission risk or opportunity for improvement. By studying our patients longitudinally, we showed that about 20% of our patients were readmitted within 30 d, but that rate rose to 30% at 90 d. We also found that lower education level, MELD score ≥ 15, chronic liver disease due to more than one etiology, HE at index admission, and history of HCC are associated with shorter time to readmission with the median time to first readmission of 54 d.
Our data is consistent with previous studies which have shown similar 30-d and 90-d readmission results[4,7,11-13]. We also found that Medicare patients, patients with lower education levels, higher ALT levels at discharge, and HE at the time of presentation are associated with higher 30-d admission rates. We also found that MELD score, which is a measure of hepatic and renal function combined, is associated with more 30-d readmission and shorter time to first readmission rates. Prior studies have also demonstrated that patients with higher MELD score are more prone to 30-d readmission[4,11] or more first hospital admission in patients who had not been admitted the previous year[14].
As seen in other recent studies, hepatic encephalopathy was a predictor for readmission, based on both 30-d and time to readmission analyses[7,15,16]. The one-year mortality for cirrhotic patients with hepatic encephalopathy is very high, approaching 60%-80% in recent studies[17,18]. HE is an expensive disease, costing approximately $63000 per case and is responsible for approximately 7.2 billion dollars in direct costs annually[19,20]. Thirty-four out of 62 (54.9%) of our patients who presented first with hepatic encephalopathy were readmitted at least once with the same diagnosis in one year. HE is not simply a marker of disease severity; forty four (71%) of our index patients who presented with HE had MELD score below 15. This is an opportunity for focused management, as we hypothesize that HE patients are more prone to readmission due to the functional impact of encephalopathy.
Careful discharge planning and expedited outpatient follow-up may help prevent readmissions, though further study is needed for cirrhosis patients. In our study, patients discharged to skilled nursing facility, those who left the hospital against medical advice and homeless patients who were discharged to shelters had higher 30-d readmission rates, but the results were not statistically significant. While not statistically significant, it is worth noting that the majority of our patients (54.3%) were discharged home without any support services, and only 27.2% of our patient cohort had VNA services after their index admission, pointing to an opportunity for further outreach once the patient leaves the hospital. As many cirrhotic patients have HE, compromising their decision making, coordinating medications and returning to their outpatient clinics for follow-up more challenging. As health systems design interventions for these complex patients, the role of home health care should be considered, with home visits for patients in our catchment area from nurses and/or allied health professionals who help patients organize their care once they’ve left the hospital.
Early outpatient follow-up by primary care and/or specialists may be another opportunity to improve outcomes but not necessarily reduce readmissions. A recent study conducted by the VA found that early (within 7 d of discharge) outpatient follow-up in patients with cirrhosis slightly increased the rate of 30-d readmissions, but significantly lowered the risk of mortality[21]. A study in Denmark showed that one-hour rehabilitation clinic within 1-3 wk after discharge from HE, reduced alcohol consumption and improved survival, but did not diminish the subsequent hospital admissions[22]. While our own numbers on outpatient follow-up were small, we did not show that relatively early medical follow-up (14 d or less) prevented readmissions. Follow up in two or three weeks for cirrhotics may not be sufficient. As the average time to a post-discharge visit ranged from 22.6-31.9 d, and 29 patients were readmitted before they had an outpatient visit, there is clearly room to improve access to post-discharge care, potentially harnessing alternate care models such as home health services, RN-led clinics and virtual visits.
Due to our use of clinical records, rather than insurance claims data, we were not able to directly gather data about hospitalizations outside our health care system. Also, our inclusion criteria only searched for admissions due to complications of cirrhosis, although (many) patients were hospitalized electively or non-electively for existing co-morbidities other than complications of cirrhosis. Our study is subject to selection bias given that patients followed at tertiary care centers tend to be more medically complex.
In summary, we showed that readmission risk for patients with cirrhosis continues well beyond 30 d and may be attributable to serious chronic disease and compromised coping skills. We found that lower education level, MELD score ≥ 15, chronic liver disease due to more than one etiology, HE at index admission, and history of HCC are associated with shorter time to readmission with the median time to first readmission of 54 d. As health systems and insurers increasingly support the adoption of value-based payment methods and patient-centered care, providers and health systems leaders must work proactively to identify high-cost and high-risk patient populations that may benefit from integrated care systems to help proactively manage chronically ill patients[23,24]. We believe that patients with cirrhosis are a population that will benefit by a systematic multidisciplinary outreach program which has the potential for preventing readmissions, improving care and saving money. Future studies should explore systems of care to define post-discharge best practices for continued care once the patient leaves the hospital environment.
COMMENTS
Background
Hospital readmissions are gaining increasing scrutiny as a measure of value-based health care as they directly impact both quality and cost of care. Cirrhosis and complications of cirrhosis account for around 40000 deaths in the United States annually and also account for 150000 hospitalizations in the US, with an estimated total estimated cost of $4 billion annually. A recent study found that 37% of patients with decompensated cirrhosis were readmitted within one month of discharge at a cost of roughly $20000 per admission.
Research frontiers
In the current value-based healthcare landscape, hospitals will be increasingly held financially accountable for readmissions under value-based care programs. Moreover, no evidence-based systems have been developed to reduce readmission rates in most chronic disease conditions, such as cirrhosis.
Innovations and breakthroughs
Factors associated with readmissions in decompensated cirrhosis in previous works include MELD, diabetes, nosocomial infections, BMI and hepatic encephalopathy. Early outpatient follow-up by primary care and/or specialists may be another opportunity to improve outcomes but not necessarily reduce readmissions. A recent study found that early (within 7 d of discharge) outpatient follow-up in patients with cirrhosis slightly increased the rate of 30-d readmissions, but significantly lowered the risk of mortality. While our own numbers on outpatient follow-up were small, we did not show that relatively early medical follow-up (14 d or less) prevented readmissions. Follow up in two or three weeks for cirrhotics may not be sufficient, as the average time to a post-discharge visit ranged from 22.6-31.9 d, and 29 patients were readmitted before they had an outpatient visit; there is clearly room to improve access to post-discharge care, potentially harnessing alternate care models such as home health services, RN-led clinics and virtual visits.
Applications
Authors’ institution has sought to improve the continuity of care for high-risk patients through post-discharge phone calls, as well as through care management programs for chronic conditions such as heart disease and diabetes, and they hope to extend such programs to patients with cirrhosis to improve clinical outcomes and reduce readmissions. Authors performed this study to better understand and define the predictors of readmission, as well as time to first readmission, in a cohort of patients with decompensated cirrhosis, to better target future programs aimed at reducing readmissions and improving patient outcomes.
Terminology
Value-based payments are a strategy increasingly adopted by payers with the goal of shifting from volume-based payment, e.g., “fee-for service” payments, to those based on improved clinical outcomes.
Peer-review
For chronic disease populations, current 30-d readmission thresholds may not capture true readmission risk or opportunities for improvement. This paper found that lower education level, MELD score ≥ 15, chronic liver disease due to more than one etiology, HE at index admission and history of HCC are associated with shorter time to readmission with the median time to first readmission of 54 d. Designing post-admission continuity of care interventions with these factors in mind would improve clinical practice and patient outcomes.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Institutional review board statement: The study was reviewed and approved by the Partners Human Research Committee Institutional Review Board.
Informed consent statement: This study received an informed consent waiver from our Institutional Review Board due to minimal risk to study subjects.
Conflict-of-interest statement: All the Authors have no conflict of interest related to the manuscript.
Data sharing statement: No additional data available.
Peer-review started: November 29, 2016
First decision: February 9, 2017
Article in press: March 31, 2017
P- Reviewer: Liu R S- Editor: Yu J L- Editor: A E- Editor: Huang Y
Contributor Information
Siamak M Seraj, Massachusetts General Hospital, Division of Gastroenterology, Boston, MA 02114, United States.
Emily J Campbell, Massachusetts General Hospital, Division of Gastroenterology, Boston, MA 02114, United States.
Sarah K Argyropoulos, Massachusetts General Hospital, Division of Gastroenterology, Boston, MA 02114, United States.
Kara Wegermann, Duke University Hospital, Department of Medicine, Durham, NC 27710, United States.
Raymond T Chung, Massachusetts General Hospital, Division of Gastroenterology, Boston, MA 02114, United States; Harvard Medical School, Boston, MA 02115, United States.
James M Richter, Massachusetts General Hospital, Division of Gastroenterology, Boston, MA 02114, United States; Harvard Medical School, Boston, MA 02115, United States. jrichter@mgh.harvard.edu.
References
- 1.Centers for Disease Control and Prevention (CDC) In: Kirch W (Ed.) Encyclopedia of Public Health. Netherlands: Springer. 2008:105. [Google Scholar]
- 2.Kim WR, Brown RS Jr, Terrault NA, El-Serag H. Burden of liver disease in the United States: summary of a workshop. Hepatology. 2002;36:227–242. doi: 10.1053/jhep.2002.34734. [DOI] [PubMed] [Google Scholar]
- 3.Asrani SK, Larson JJ, Yawn B, Therneau TM, Kim WR. Underestimation of liver-related mortality in the United States. Gastroenterology. 2013;145:375–382.e1-2. doi: 10.1053/j.gastro.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Volk ML, Tocco RS, Bazick J, Rakoski MO, Lok AS. Hospital readmissions among patients with decompensated cirrhosis. Am J Gastroenterol. 2012;107:247–252. doi: 10.1038/ajg.2011.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agrawal K, Kumar P, Markert R, Agrawal S. Risk Factors for 30-Day Readmissions of Individuals with Decompensated Cirrhosis. South Med J. 2015;108:682–687. doi: 10.14423/SMJ.0000000000000371. [DOI] [PubMed] [Google Scholar]
- 6.Tapper EB, Finkelstein D, Mittleman MA, Piatkowski G, Chang M, Lai M. A Quality Improvement Initiative Reduces 30-Day Rate of Readmission for Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2016;14:753–759. doi: 10.1016/j.cgh.2015.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bajaj JS, Reddy KR, Tandon P, Wong F, Kamath PS, Garcia-Tsao G, Maliakkal B, Biggins SW, Thuluvath PJ, Fallon MB, et al. The 3-month readmission rate remains unacceptably high in a large North American cohort of patients with cirrhosis. Hepatology. 2016;64:200–208. doi: 10.1002/hep.28414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Runyon B, Mitroi L. Do Automated Telephone Systems Decrease Hospital Readmissions Among Patients with Cirrhosis? Dig Dis Sci. 2015;60:3502–3503. doi: 10.1007/s10620-015-3883-6. [DOI] [PubMed] [Google Scholar]
- 9.Kamath PS, Kim WR; Advanced Liver Disease Study Group. The model for end-stage liver disease (MELD) Hepatology. 2007;45:797–805. doi: 10.1002/hep.21563. [DOI] [PubMed] [Google Scholar]
- 10.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 11.Berman K, Tandra S, Forssell K, Vuppalanchi R, Burton JR Jr, Nguyen J, Mullis D, Kwo P, Chalasani N. Incidence and predictors of 30-day readmission among patients hospitalized for advanced liver disease. Clin Gastroenterol Hepatol. 2011;9:254–259. doi: 10.1016/j.cgh.2010.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bini EJ, Weinshel EH, Generoso R, Salman L, Dahr G, Pena-Sing I, Komorowski T. Impact of gastroenterology consultation on the outcomes of patients admitted to the hospital with decompensated cirrhosis. Hepatology. 2001;34:1089–1095. doi: 10.1053/jhep.2001.29204. [DOI] [PubMed] [Google Scholar]
- 13.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 14.Johnson KB, Campbell EJ, Chi H, Zheng H, King LY, Wu Y, Delemos A, Hurairah A, Corey K, Richter JM, et al. Advanced disease, diuretic use, and marital status predict hospital admissions in an ambulatory cirrhosis cohort. Dig Dis Sci. 2014;59:174–182. doi: 10.1007/s10620-013-2832-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tapper EB, Halbert B, Mellinger J. Rates of and Reasons for Hospital Readmissions in Patients With Cirrhosis: A Multistate Population-based Cohort Study. Clin Gastroenterol Hepatol. 2016;14:1181–1188.e2. doi: 10.1016/j.cgh.2016.04.009. [DOI] [PubMed] [Google Scholar]
- 16.Saab S. Evaluation of the impact of rehospitalization in the management of hepatic encephalopathy. Int J Gen Med. 2015;8:165–173. doi: 10.2147/IJGM.S81878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jepsen P, Ott P, Andersen PK, Sørensen HT, Vilstrup H. Clinical course of alcoholic liver cirrhosis: a Danish population-based cohort study. Hepatology. 2010;51:1675–1682. doi: 10.1002/hep.23500. [DOI] [PubMed] [Google Scholar]
- 18.Stewart CA, Malinchoc M, Kim WR, Kamath PS. Hepatic encephalopathy as a predictor of survival in patients with end-stage liver disease. Liver Transpl. 2007;13:1366–1371. doi: 10.1002/lt.21129. [DOI] [PubMed] [Google Scholar]
- 19.Stepanova M, Mishra A, Venkatesan C, Younossi ZM. In-hospital mortality and economic burden associated with hepatic encephalopathy in the United States from 2005 to 2009. Clin Gastroenterol Hepatol. 2012;10:1034–1041.e1. doi: 10.1016/j.cgh.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 20.Courson A, Jones GM, Twilla JD. Treatment of Acute Hepatic Encephalopathy: Comparing the Effects of Adding Rifaximin to Lactulose on Patient Outcomes. J Pharm Pract. 2016;29:212–217. doi: 10.1177/0897190014566312. [DOI] [PubMed] [Google Scholar]
- 21.Kanwal F, Asch SM, Kramer JR, Cao Y, Asrani S, El-Serag HB. Early outpatient follow-up and 30-day outcomes in patients hospitalized with cirrhosis. Hepatology. 2016;64:569–581. doi: 10.1002/hep.28558. [DOI] [PubMed] [Google Scholar]
- 22.Andersen MM, Aunt S, Jensen NM, Homann C, Manniche J, Svendsen S, Christensen E, Reher-Langberg A, Schiødt FV. Rehabilitation for cirrhotic patients discharged after hepatic encephalopathy improves survival. Dan Med J. 2013;60:A4683. [PubMed] [Google Scholar]
- 23.Fisher ES. Building a medical neighborhood for the medical home. N Engl J Med. 2008;359:1202–1205. doi: 10.1056/NEJMp0806233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Butcher L. Building a medical neighborhood. Hosp Health Netw. 2011;85:31–34. [PubMed] [Google Scholar]


