Sugar-Sweetened Beverages and Childhood Obesity: The Evidence Calls for Policy Interventions (Responsible Authors: Janne C. de Ruyter, Jacob C. Seidell)
A Case for Reducing Sugar-Sweetened Beverage Consumption in Infants and Toddlers
The easy access to an abundance of sugar-sweetened beverages (SSB) is of major concern now that compelling evidence has linked high intakes of these drinks to childhood obesity. Recently, two independent trials showed increased weight in children consuming SSB compared with a control group who received water or drinks with artificial sweeteners [1,2]. Therefore, the high availability and intense marketing of SSB combined with the high rates of childhood obesity worldwide should raise concern among public health professionals as well as politicians [3,4]. In this article, we elaborate on the evidence for the association between SSB and adverse health effects, and propose a multiple-setting behavioral intervention in the community that promotes water and discourages SSB after breast and/or bottle feeding in children between the ages of 0 and 4 years.
The Rise in Consumption of Sugar-Sweetened Beverages
SSB include all sodas, fruit drinks, sport drinks, and other beverages with added sugar [5]. Over the last several decades, the total consumption of SSB has increased worldwide – in some countries such as Mexico and the USA by almost 100% [6]. In Dutch children, the intake of SSB is now one of the highest in Europe [7]. This may be rooted in a tradition of giving children SSB when they are still very young: 36% of Dutch children consume SSB as their first drink after breast and/or bottle feeding [8], and at most day care centers children consume at least two SSB per day [9]. In 2009, of all liquids consumed by Dutch children aged 2-6 years, only 24% or 263 ml/day was water [10,11]. This is lower than in other countries such as France where the intake of water in children aged 6-11 years was 44% or 549 ml/day [11,12]. Although methodological issues may explain some of these differences, we believe that intake of water in groups of Dutch children indeed is relatively low.
Sugar-Sweetened Beverages and Excess Weight
Both observational and experimental studies have been performed to investigate the association between SSB intake and weight gain. Observational studies however should be interpreted with caution due to bias resulting from potentially confounding variables. They do therefore not permit inferences about temporal relationships. Experimental studies provide better insight into the cause-and-effect relationship between SSB and body weight gain. To investigate the effect of SSB on body weight thoroughly, we performed a double-blind experiment that was designed to answer the question whether SSB lead to cause weight gain [1]. In this study, 641 normal-weight primary school children aged 4-12 years were assigned to one of two groups. The intervention group received 220 ml of SSB each day; the control group received 220 ml of non-caloric artificially sweetened drink. After 18 months of intervention the children consuming the SSB had gained about 1 kg more weight, compared with those drinking the non-caloric drinks. They also accumulated more body fat. An experimental study of Ebbeling et al. [2] in adolescents yielded similar results. They performed an experiment in 224 overweight and obese teenagers who at baseline consumed up to two SSB daily. In this study, the intervention group received bottled water and diet drinks to discourage intake of SSB in the home. The control group continued drinking beverages as they used to. After 1 year, teenagers in the intervention group gained less weight than those in the control group. This effect was most pronounced in Hispanic teenagers. Thus, both trials have confirmed that SSB indeed lead to cause more weight gain than sugar-free drinks. Also, a recent systematic review and meta-analysis of prospective cohort studies and randomized clinical trials provided evidence that SSB consumption promotes weight gain in children and adults [13]. In the past, studies also reported no significant association between SSB and body weight [14,15,16]. Interestingly, these studies were all either written by employees of the SSB industry or by authors who were paid by the industry to do the research.
The physiological pathway responsible for the association between SSB and excess weight remains unclear. One of the possible explanations is the poor satiety value of sugar in liquid form. In one of our studies we found that SSB and sugar-free beverages produced similar satiety [17]. Therefore, when children are substituting sugar-free drinks for SSB they will probably not compensate for missed calories by eating more food later. This may, at least partly, explain our previous observation that the children in the sugar-free group accumulated less body fat than those in the sugar group [1].
Sugar-Sweetened Beverages and Dental Problems
Apart from the effects on body weight gain, consumption of SSB also contributes to the development of dental erosion and caries. Dental erosion is the irreversible loss of tooth structure due to chemical dissolution by acids. Consequently, acidic foods and drinks are thought to play a role in triggering dental erosion [18]. The acidity levels (pH) and buffer capacity of food products determine its erosive potential. Numerous in vitro studies have shown an association between dental erosion and the consumption of soft drinks, fruit drinks, fruit juices, and artificially sweetened beverages [19,20,21,22]. Dental erosion has become a major health problem in most industrialized countries. In the Netherlands, the prevalence of dental erosion in children has increased dramatically over the last decades [23]. Approximately one third of Dutch children now suffer from dental erosion [24].
Apart from dental erosion, dental caries is another public health problem that affects 60-90% of school-aged children and the vast majority of adults worldwide [25]. In the Netherlands, at least one third of children aged 5 years have sustained dental caries [26]. Dental caries is caused by bacterial infection that causes demineralization and destruction of the hard tissues of the teeth. Over the past 20 years, a decline in caries has been observed in most industrialized countries. This pattern was the result of a number of public health measures [27]. However, it must be emphasized that the problem of caries has not been eradicated but only controlled to a certain degree [28]. The consumption of SSB has been associated with the onset of dental caries [29].
Public Health Measures in Early Life
In conclusion, there is now substantial evidence that justifies public health measures to reduce the consumption of SSB and promote replacement of these by sugar-free beverages, preferably water. Although recent trials [1,2] were mainly performed with artificially sweetened beverages, one may assume that water would be as effective. Public health measures for children may be in the form of regulations on advertising and marketing to children, restricted availability in schools, and/or soda taxes to discourage consumption. Strategies such as taxes and restricted availability have worked for tobacco [30], and many argue that similar steps are needed for SSB. In addition, such strategies may be particularly relevant for children aged 0-4 years. Children of this age group are important to focus on for a number of reasons. First, dietary preferences are initially established between the ages 0 and 4 years, laying the foundation for eating habits later in life [31,32]. Birch et al. [32] have shown that when children are used to consuming water at a young age, they are more likely to drink water later in life. Second, excess weight, dental erosion, and caries in childhood have been associated with health risks in childhood itself [33] – but also later in life [34,35,36].
A Multiple-Setting Behavioral Intervention in the Community
Many studies suggest that the physical, sociocultural, and economic environment of children plays a crucial role in the onset of obesity in both distal and proximal ways [37]. Distally, the physical, sociocultural, and economic environment determine the general demand, availability, and pricing of foods. Proximally, neighborhood as well as school and home environments determine the availability of foods. Changing the environment may therefore be an effective strategy to prevent obesity in children [38]. There have been successful initiatives to implement such environmental based approach. The French EPODE program (Ensemble, Prevenons l'Obésité des Enfants which means ‘Together, let's prevent obesity in children’) is an example of a community-based intervention initiated in two small towns in France in 2000 [39]. This approach turned out to be effective, and is now being extended to many other countries in Europe.
The EPODE program provides a valuable framework that can be used on how to set up an environmental approach to prevent weight gain in children [40]. This, in combination with the rising belief that obesity prevention should start at an early age and convincing evidence that SSB are fattening, sets the stage for a multiple-setting behavioral intervention in the community. We will therefore develop, implement, and evaluate an intervention that promotes the consumption of water and discourages the consumption of SSB in children aged 0-4 years living in Amsterdam. We will focus on disadvantaged and poor populations because they are at the highest risk of developing both obesity [41] and dental problems [42]. The aim of the intervention is to increase water intake of children and reduce SSB intake. We will therefore educate caregivers of young children, i.e. parents, personnel of day care centers and preschools, and health care professionals, about the health benefits of water. With the use of the Triple P Parenting program we will also provide caregivers with pedagogical tools to persuade children to drink water [43]. Research showed that parents have a key influence on the development and maintenance of children's behaviors [44]. Moreover, especially caregivers of young children appear willing to modify their behavior if this benefits their children [45].
We will collaborate with the municipal youth health care service because of their prominent role in the health education of the caregivers. We will also involve day care centers and preschools to contribute to a continuous health promoting environment for children [46]. Studies in children aged 0-4 years on the effects of behavioral interventions that promote water are scarce [47]. Studies in primary and secondary schools that improved water access showed inconsistent outcomes [48,49]. Overall, the outcomes suggest that intake of water is added to regular liquid intake and that water does not replace intake of SSB. An intervention should therefore not only promote water but also discourage SSB intake.
The outcomes of this project can be translated into strategies that municipal youth health care services, day care centers, and preschools can use when teaching healthy drinking habits to children and their caregivers. We will put our findings together in the so called ‘Infant Toddler Water Toolkit’ that municipalities can use when designing a healthy drinking policy for 0- to 4-year-old children in a city.
Conclusion
There is compelling evidence that SSB increase childhood obesity. ‘Reduce sugary drinks, drink water instead’, is a simple message that can be distributed among young children and their caregivers. SSB are devoid of essential nutrients and one can therefore easily do without them. One may speculate that there is no other single food product whose elimination could contribute more to prevent excessive weight gain.
The goal of the proposed community-based intervention is to establish a healthier environment where water – and not SSB – are widely accessible. In the long run, this may improve health behaviors and health outcomes such as overweight as well as dental erosion and caries in both children and their caregivers.
EPODE, a Multi-Stakeholder Approach to Prevent Childhood Obesity (Responsible Authors: J.-M. Borys, E. Levy, J. Vinck, J. Mayer, H. Finch, H. Ruault du Plessis, P. Richard, P. Harper)
Introduction
The prevalence of overweight and obesity has increased worldwide over the last 30 years [50,51,52,53,54], and forecasts suggest that the majority of the world's adults will be overweight or obese by 2030. Not only does overweight and obesity have a negative impact on health and wellbeing, the related economic costs represent a significant burden to public health systems across the globe.
Evidence suggests that once obesity is established, it is difficult to reverse [55], strengthening the case for primary prevention. Prevention is widely recognized to be the most efficient and cost-effective way to tackle the obesity pandemic.
The environment determines, to a large extent, both eating and physical activity habits, and, as such, determinants of overweight and obesity lie not only with the individual [56,57,58,59,60] but with the community at large. It is therefore essential that, to ensure primary prevention of overweight and obesity, a multifaceted strategy is developed that targets the whole community to step-by-step change the environment, policies, social norms, and the behaviors elicited by these environmental variables. Thus modifying unhealthy habits requires changing perceptions, the micro-environment (e.g. schools, homes, neighborhoods), and the macro-environment (e.g. the urban setting, education and health systems, governments, the food industry, the media, and society's attitudes and beliefs) so that healthy behaviors prevail [60].
The aim of this article is to discuss the EPODE (the French acronym for ‘Ensemble Prévenons l'Obésité Des Enfants’ – ‘Together We Can Prevent Childhood Obesity’) multi-stakeholder approach and to demonstrate its effectiveness in ensuring primary prevention of overweight and obesity.
The EPODE vision statement is that childhood obesity will be prevented by creating healthy local environments, family norms and childhood settings, all being strongly supportive of children and their families enjoying healthy eating, active play, and recreation.
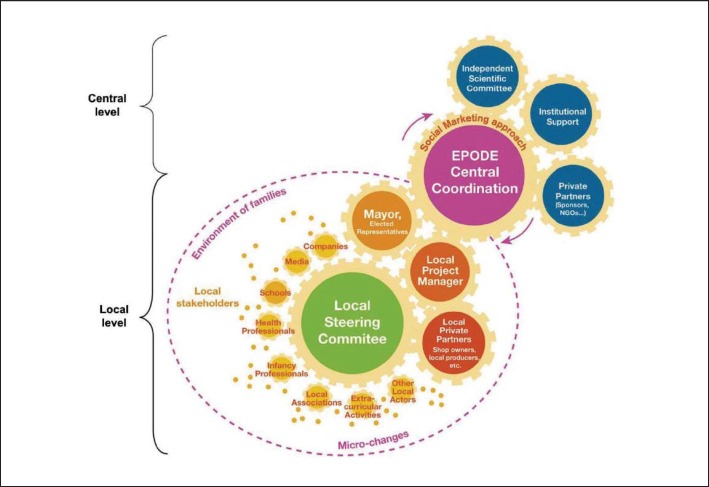
EPODE is a community capacity-building approach to implement sustainable strategies aimed at promoting healthier lifestyles and preventing childhood obesity and non-communicable diseases. The model consists of concrete initiatives, at both national and local levels, that encourage better and more balanced eating habits and increased levels of physical activity (fig. 1).
Fig. 1.
EPODE stakeholders at central and local levels. NGO = Non-governmental organization.
EPODE programs target communities at different levels, affecting groups of children aged 0-12 years. Local stakeholders who influence childhood settings, food and physical activity environments, and sociocultural norms are automatically included.
Origins of the Methodology
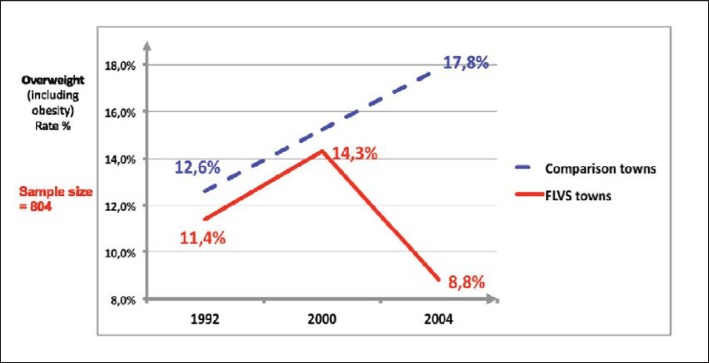
The EPODE methodology is the result of the FLVS study that began in 1992 in two towns in Northern France (Fleurbaix and Laventie) [61]. This study was a long-term school-based intervention that took place between 1992 and 1998 and evolved into a community-based program that was active from 1998 to 2004. Actions that were implemented during this intervention aimed at improving eating and physical activity habits among children. Initial data obtained from this study showed that interventions solely targeting schools were not sufficient to significantly reduce the prevalence of obesity and overweight (fig. 2) [62].
Fig. 2.
Downward trends in the prevalence of childhood overweight in the setting of 12-year school- and community-based programs.
Improved results were obtained through a subsequent community-based intervention (1998-2004) [62] that involved many local stakeholders. The FLVS study also demonstrated that this prevention program was efficient across all socioeconomic levels [63]. Evaluation of the results of this study led to the identification of the main factors of success that formed the four pillars of the EPODE methodology [63,64]:
Political commitment: formal commitment is sought from political representatives from the local community to the state and federal level.
Scientific evaluation and dissemination: using evidence from a wide variety of sources to guide the implementation of EPODE interventions and to evaluate impact and outcomes of the EPODE program.
Public-private partnership at all levels: to secure sufficient resources to fund central services, as well as contributions from local organizations to fund implementation at the community level.
Communication, including social marketing methods: planning, coordinating actions and providing the social marketing and support services at community level.
Implementation
‘EPODE’ was first launched in 2004 in ten French pilot communities. Since then, the EPODE methodology has been implemented across the world in countries such as Belgium, Greece, Spain, The Netherlands, Romania, South Australia, and Mexico.
The implementation of the EPODE methodology takes place on two levels. It is firstly important to address the central level, which can be represented by a public body (e.g. Ministry of Health) or a private organization such as a Communication Agency. The central level has the primary role of coordinating the multiple stakeholders involved in the program (institutions, scientific expertise, and corporate sector). The central level also has the responsibility for training and coaching the actors involved at the local level and proposing regular campaigns.
At the local level, a local leader, such as the mayor, within each community involved in the program, plays a key role in nominating and hiring a local project manager to implement the concrete actions on the ground.
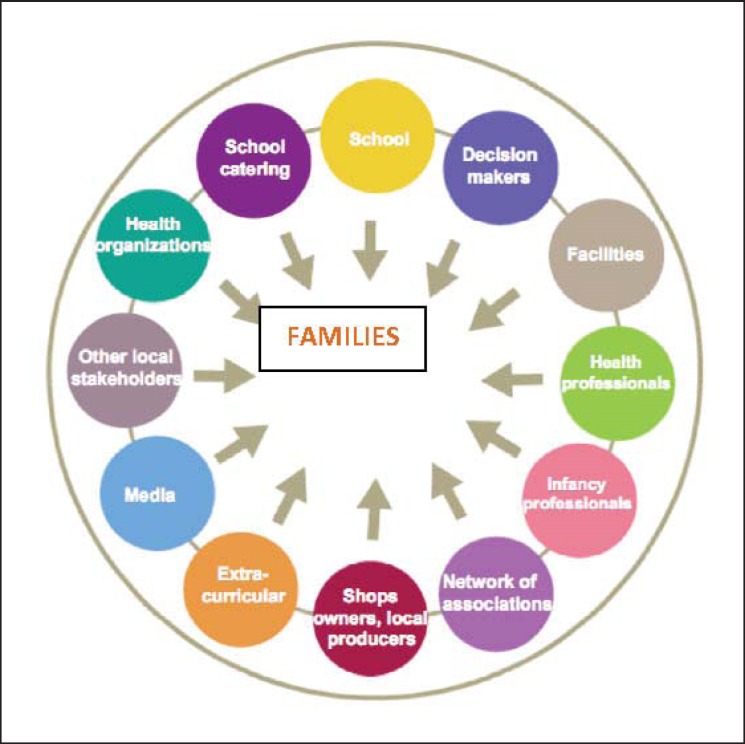
The role of the local project manager is to mobilize a wide diversity of local stakeholders, especially in schools, preschools, extracurricular organizations, and any social network of associations (fig. 3). These are all key settings in which to implement activities involving children and families in order to change their local behavioral context. For this purpose, the local project manager coordinates a multifaceted local steering committee of local representatives from various fields. This committee meets on a regular basis to make key decisions, foster the implementation of activities and actions, and generate peer-to-peer dynamics (see table 1 for the number and type of actions implemented in two towns that are part of the VIASANO program, based on the EPODE methodology, as an example).
Fig. 3.
Local stakeholders mobilized at local level.
Table 1.
Number of actions in the two pilot towns per target group and per theme, VIASANO
| Target group | Theme | |||
|---|---|---|---|---|
| food | physical activity | food and physical activity | general health | |
| Children and adolescents | 36 | 11 | 29 | 4 |
| Children and families | 20 | 4 | 13 | 2 |
| Health care professionals | 2 | / | 3 | 1 |
| General public | 45 | 15 | 37 | 14 |
| Others (schools, local business community, disabled, …) | 4 | 1 | 4 | 1 |
Actions targeting the community can be diverse and often use local media to change social norms and influence policy. Some examples of actions targeting the local population include distribution of healthy snacks during a public walking activity for families in the town; an educational and activity game for families or the elderly to promote physical activity; a conference for seniors about food, physical activity, and other health-related issues; healthy lunches for employees; stands promoting healthy food and physical activity during events; redesigning school playing area to encourage physical activity; and embellishing public green spaces.
The community-based interventions based on the EPODE methodology are evaluated according to their four levels of implementation: central and local organization levels, setting level, and child level [63,64]. Evaluation includes both process and outcome indicator monitoring. The heights and weights of children from the age of 5 to 12 years are measured, and BMI is calculated and recorded. Although the accuracy of BMI in diagnosing obesity is limited [65,66], it allows international comparisons and is therefore preferred among other adiposity markers in children. Changes in food and physical activity habits are assessed by specific questionnaires administered in schools or other settings (e.g. local health centers).
The evaluation framework of each program is designed by the central coordination team, with the expertise of a scientific committee and feedback from local stakeholders. Evaluation is crucial to the success of an EPODE program as it is a key-driver for political engagement and fosters mobilization of stakeholders in a sustainable way.
Results
Impact on Overweight and Obesity Prevalence
In eight French towns where the EPODE methodology was implemented, children aged 5-12 years (n = 23,205) were weighed and measured each year between 2005 and 2009 by school health professionals. While national data available in France indicated an overall stabilization in the prevalence of childhood overweight and obesity, results from the eight French EPODE pilot towns showed a significant decrease of 9.12% (p < 0.0001) in overweight and obesity between 2005 and 2009. It is also noteworthy that children who attended schools in deprived areas showed a downward trend of 2% (NS: p = 0.38) in the prevalence of childhood overweight (including obesity), compared with an increase in the prevalence of overweight and obesity in children from disadvantaged households at national level [67]. The VIASANO program, based on the EPODE methodology, was launched in 2007 in several towns in Belgium. In two of these towns, we collected BMI data on children in 2007 and 2010. In 2007, children aged 3-4 years (first-year preschool) and 5-6 years (third-year preschool) (n = 1,300) were weighed and measured by the School Health Prevention Services as well as 1,484 children in 2010 in the VIASANO towns and in a control population (the entire French Community). The prevalence of overweight showed a decrease of 22% (p < 0.05) in VIASANO towns in comparison with the control population.
Transferability
Following a European project granted by the European Commission (DG SANCO), i.e. the Epode European Project (www.epode-european-network.com), the EPODE methodology was implemented in over 500 communities in 8 countries across the world, involving over 11 million people and demonstrating the transferability of the EPODE methodology to culturally diverse settings [68,69].
Conclusions
As a result of the EPODE experience and with the aim of supporting EPODE community-based programs and other EPODE-like programs, the EPODE International Network (EIN) was created in 2011. In 2014, the EIN supports community-based obesity prevention programs through capacity building and best practice sharing, connecting over 30 international programs and involving 150 million people.
Furthermore, the EPHE (‘EPODE for the Promotion of Health Equity’) project is also an outcome of the EPODE experience and is a collaborative project with the European Commission (DG Health and Consumers) that aims to ensure health equity across Europe. EPHE seeks to understand whether the implementation of an adapted EPODE methodology can reduce socioeconomic inequalities in health-related diet and physical activity behaviors of families with children aged 6-12 years, living in 7 different European countries.
The theory behind the EPODE methodology reflects the importance of a multifactorial approach in the prevention of childhood obesity. The four pillars show the core components of the approach and help to explain why EPODE has had an impact on overweight prevalence in the towns of implementation as early evaluation suggests encouraging results from several EPODE programs [70].
Further important lessons are to be learned from more detailed evaluations of EPODE.
Childhood obesity prevention programs, which aspire to have a wide reach, may benefit from the insights into the EPODE methodology. EPODE already is referenced in several national and international reports, position papers, and conferences as an innovative example of a community-based program aimed at promoting healthy active behaviors in children [71,72,73,74,75,76,77,78,79,80,81,82,83,84,85].
Disclosure Statement
JCdR, JCS, and JV declare no conflict of interest. JMB and EL did not provide a disclosure statement.
HF, JM, HRdP, PH, and PR: The EPHE Project is a Pan-European project (2012-2015) co-funded by the DG SanCO. Other partners in EPHE include universities, WHO Regional Office for Europe and Community-Based Programmes across 7 European member states. The EPHE Project is also co-funded by its historical private partners: Ferrero, Mars, Orangina-Schweppes together with Danone. All of EPHE private partners have directly or indirectly committed to the EU platform on diet, physical activity and health. Please visit the EU website to see their commitments: http://ec.europa.eu/health/nutrition_physical_activity/platform/index_en.htm. For more information, please visit the website: www.epheproject.eu.
References
- 1.De Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar-free or sugar-sweetened beverages and body weight in children. N Engl J Med. 2012;367:1397–1406. doi: 10.1056/NEJMoa1203034. [DOI] [PubMed] [Google Scholar]
- 2.Ebbeling CB, Feldman HA, Chomitz VR, Antonelli TA, Gortmaker SL, Osganian SK, Ludwig DS. A randomized trial of sugar-sweetened beverages and adolescent body weight. N Engl J Med. 2012;367:1407–1416. doi: 10.1056/NEJMoa1203388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schonbeck Y, Talma H, van Dommelen P, Bakker B, Buitendijk SE, Hirasing RA, van Buuren S. Increase in prevalence of overweight in Dutch children and adolescents: a comparison of nationwide growth studies in 1980, 1997 and 2009. PLoS One. 2011;6:e27608. doi: 10.1371/journal.pone.0027608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988-2004. Pediatrics. 2008;121:1604–1614. doi: 10.1542/peds.2007-2834. [DOI] [PubMed] [Google Scholar]
- 6.Brownell KD, Farley T, Willett WC, Popkin BM, Chaloupka FJ, Thompson JW, Ludwig DS. The public health and economic benefits of taxing sugar-sweetened beverages. N Engl J Med. 2009;361:1599–1605. doi: 10.1056/NEJMhpr0905723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brug J, van Stralen MM, Te Velde SJ, Chinapaw MJ, De Bourdeaudhuij I, Lien N, Bere E, Maskini V, Singh AS, Maes L, Moreno L, Jan N, Kovacs E, Lobstein T, Manios Y. Differences in weight status and energy-balance related behaviors among schoolchildren across Europe: the ENERGY-project. PLoS One. 2012;7:e34742. doi: 10.1371/journal.pone.0034742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Boerboom H, Hengstz K. DRINK water JOGG. Report by Motivaction Research and Strategy, Amsterdam, 2013.
- 9. De Ruyter JC, Vogel A. The drinkWATERstudy: replacing sugar-sweetened beverages with water in day care centers: a pilot study. In preparation, 2014.
- 10. Ocke MC, Van Rossum CTM, Fransen HP, Buurma EM, de Boer EJ, Brants HAM, Niekerk EM, van der Laan JD, Drijvers JJMM, Ghameshlou Z. Dutch National Food Consumption Survey – young children 2005/2006. Report by RIVM, Bilthoven, 2009. www.rivm.nl/bibliotheek/rapporten/350070001.pdf (last accessed February 24, 2014).
- 11. Voedingscentrum (English translation Netherlands Nutrition Center). Vocht inname. (English translation: liquid intake). www.voedingscentrum.nl/encyclopedie/trefwoord/vocht (last accessed January 6, 2014).
- 12.Bellisle F, Thornton SN, Hebel P, Denizeau M, Tahiri M. A study of fluid intake from beverages in a sample of healthy French children, adolescents and adults. Eur J Clin Nutr. 2010;64:350–355. doi: 10.1038/ejcn.2010.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr. 2013;98:1084–1102. doi: 10.3945/ajcn.113.058362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Forshee RA, Anderson PA, Storey ML. The role of beverage consumption, physical activity, sedentary behavior, and demographics on body mass index of adolescents. Int J Food Sci Nutr. 2004;55:463–478. doi: 10.1080/09637480400015729. [DOI] [PubMed] [Google Scholar]
- 15.Forshee RA, Storey ML. Total beverage consumption and beverage choices among children and adolescents. Int J Food Sci Nutr. 2003;54:297–307. doi: 10.1080/09637480120092143. [DOI] [PubMed] [Google Scholar]
- 16.Valente H, Teixeira V, Padrao P, Bessa M, Cordeiro T, Moreira A, Mitchell V, Lopes C, Mota J, Moreira P. Sugar-sweetened beverage intake and overweight in children from a Mediterranean country. Public Health Nutr. 2011;14:127–132. doi: 10.1017/S1368980010002533. [DOI] [PubMed] [Google Scholar]
- 17.De Ruyter JC, Katan MB, Kuijper LDJ, Liem DG, Olthof MR. The effect of sugar-free versus sugar-sweetened beverages on satiety, liking and wanting: an 18 month randomized double-blind trial in children. PLoS One. 2013;8:e78039. doi: 10.1371/journal.pone.0078039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lussi A, Jaeggi T, Zero D. The role of diet in the aetiology of dental erosion. Caries Res. 2004;38(suppl 1):34–44. doi: 10.1159/000074360. [DOI] [PubMed] [Google Scholar]
- 19.Attin T, Weiss K, Becker K, Buchalla W, Wiegand A. Impact of modified acidic soft drinks on enamel erosion. Oral Dis. 2005;11:7–12. doi: 10.1111/j.1601-0825.2004.01056.x. [DOI] [PubMed] [Google Scholar]
- 20.De Carvalho Sales-Peres SH, Magalhaes AC, de Andrade Moreira Machado MA, Buzalaf MA. Evaluation of the erosive potential of soft drinks. Eur J Dent. 2007;1:10–13. [PMC free article] [PubMed] [Google Scholar]
- 21.Kitchens M, Owens BM. Effect of carbonated beverages, coffee, sports and high energy drinks, and bottled water on the in vitro erosion characteristics of dental enamel. J Clin Pediatr Dent. 2007;31:153–159. doi: 10.17796/jcpd.31.3.1157l653t8206100. [DOI] [PubMed] [Google Scholar]
- 22.Owens BM, Kitchens M. The erosive potential of soft drinks on enamel surface substrate: an in vitro scanning electron microscopy investigation. J Contemp Dent Pract. 2007;8:11–20. [PubMed] [Google Scholar]
- 23.Gambon DL, Brand HS, Veerman EC. Dental erosion in the 21st century: what is happening to nutritional habits and lifestyle in our society? Br Dent J. 2012;213:55–57. doi: 10.1038/sj.bdj.2012.613. [DOI] [PubMed] [Google Scholar]
- 24.El Aidi H, Bronkhorst EM, Huysmans MC, Truin GJ. Dynamics of tooth erosion in adolescents: a 3-year longitudinal study. J Dent. 2010;38:131–137. doi: 10.1016/j.jdent.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 25. World Health Organization What is the burden of oral disease? www.who.int/oral_health/disease_burden/global/en/ (last accessed January 6, 2014).
- 26. Abbink EJAA, den Dekker J. Signalement Mondzorg 2013 – Mondgezondheid en preventief tandheelkundig gedrag van jeugdige verzekerden (English translation: Oral care 2013:Oral health and preventive dental behavior of insured youth). Report by Committee of Health Insurers, Diemen, 2013.
- 27.Caballero BL, Allen L, Prentice A. Encyclopedia of Human Nutrition. Waltham: Academic Press; 2006. [Google Scholar]
- 28. World Health Organization The global burden of oral diseases and risks to oral health. www.who.int/bulletin/volumes/83/9/petersen0905abstract/en/ (last accessed January 6, 2014). [PMC free article] [PubMed]
- 29.Ruottinen S, Karjalainen S, Pienihakkinen K, Lagstrom H, Niinikoski H, Salminen M, Ronnemaa T, Simell O. Sucrose intake since infancy and dental health in 10-year-old children. Caries Res. 2004;38:142–148. doi: 10.1159/000075938. [DOI] [PubMed] [Google Scholar]
- 30.Chaloupka FJ, Straif K, Leon ME. Effectiveness of tax and price policies in tobacco control. Tob Control. 2011;20:235–238. doi: 10.1136/tc.2010.039982. [DOI] [PubMed] [Google Scholar]
- 31.Birch L, Savage JS, Ventura A. Influences on the development of children's eating behaviours: from infancy to adolescence. Can J Diet Pract Res. 2007;68:s1–s56. [PMC free article] [PubMed] [Google Scholar]
- 32.Birch LL. Development of food preferences. Annu Rev Nutr. 1999;19:41–62. doi: 10.1146/annurev.nutr.19.1.41. [DOI] [PubMed] [Google Scholar]
- 33.Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, Allen K, Lopes M, Savoye M, Morrison J, Sherwin RS, Caprio S. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350:2362–2374. doi: 10.1056/NEJMoa031049. [DOI] [PubMed] [Google Scholar]
- 34.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–493. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hannon TS, Rao G, Arslanian SA. Childhood obesity and type 2 diabetes mellitus. Pediatrics. 2005;116:473–480. doi: 10.1542/peds.2004-2536. [DOI] [PubMed] [Google Scholar]
- 36.Najafipour H, Malek Mohammadi T, Rahim F, Haghdoost AA, Shadkam M, Afshari M. Association of oral health and cardiovascular disease risk factors ‘results from a community based study on 5900 adult subjects’. ISRN Cardiol. 2013;78:21–26. doi: 10.1155/2013/782126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, Armstrong R, Prosser L, Summerbell CD. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011 doi: 10.1002/14651858.CD001871.pub3. CD001871. [DOI] [PubMed] [Google Scholar]
- 38.Swinburn B, Egger G, Raza F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med. 1999;29:563–570. doi: 10.1006/pmed.1999.0585. [DOI] [PubMed] [Google Scholar]
- 39.Borys JM, Le Bodo Y, Jebb SA, Seidell JC, Summerbell C, Richard D, De Henauw S, Moreno LA, Romon M, Visscher TL, Raffin S, Swinburn B. EPODE approach for childhood obesity prevention: methods, progress and international development. Obes Rev. 2012;13:299–315. doi: 10.1111/j.1467-789X.2011.00950.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Van Koperen TM, Jebb SA, Summerbell CD, Visscher TL, Romon M, Borys JM, Seidell JC. Characterizing the EPODE logic model: unravelling the past and informing the future. Obes Rev. 2013;14:162–170. doi: 10.1111/j.1467-789X.2012.01057.x. [DOI] [PubMed] [Google Scholar]
- 41.Wang Y, Lim H. The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int Rev Psychiatry. 2012;24:176–188. doi: 10.3109/09540261.2012.688195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tanaka K, Miyake Y, Sasaki S, Hirota Y. Socioeconomic status and risk of dental caries in Japanese preschool children: the Osaka Maternal and Child Health Study. J Public Health Dent. 2013;73:217–223. doi: 10.1111/jphd.12016. [DOI] [PubMed] [Google Scholar]
- 43.Sanders MR. Development, evaluation, and multinational dissemination of the triple P-Positive Parenting Program. Annu Rev Clin Psychol. 2012;8:345–379. doi: 10.1146/annurev-clinpsy-032511-143104. [DOI] [PubMed] [Google Scholar]
- 44.Brotman LM, Dawson-McClure S, Huang KY, Theise R, Kamboukos D, Wang J, Petkova E, Ogedegbe G. Early childhood family intervention and long-term obesity prevention among high-risk minority youth. Pediatrics. 2012;129:e621–628. doi: 10.1542/peds.2011-1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gillman MW, Ludwig DS. How early should obesity prevention start? N Engl J Med. 2013;369:2173–2175. doi: 10.1056/NEJMp1310577. [DOI] [PubMed] [Google Scholar]
- 46.Schwarz DF. The Philadelphia experience: actionable strategies for childhood obesity prevention. Child Obes. 2013;9:282–285. doi: 10.1089/chi.2013.9401. [DOI] [PubMed] [Google Scholar]
- 47.Larson N, Ward DS, Neelon SB, Story M. What role can child-care settings play in obesity prevention? a review of the evidence and call for research efforts. J Am Diet Assoc. 2011;111:1343–1362. doi: 10.1016/j.jada.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 48.Muckelbauer R, Libuda L, Clausen K, Toschke AM, Reinehr T, Kersting M. Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled cluster trial. Pediatrics. 2009;123:e661–667. doi: 10.1542/peds.2008-2186. [DOI] [PubMed] [Google Scholar]
- 49.Patel AI, Bogart LM, Elliott MN, Lamb S, Uyeda KE, Hawes-Dawson J, Klein DJ, Schuster MA. Increasing the availability and consumption of drinking water in middle schools: a pilot study. Prev Chronic Dis. 2011;8:A60. [PMC free article] [PubMed] [Google Scholar]
- 50.Lissau I, Overpeck MD, Ruan WJ, Due P, Holstein BE, Hediger ML, Health Behaviour in School-Aged Children Obesity Working Group Body mass index and overweight in adolescents in 13 European countries, Israel, and the United States. Arch Pediatr Adolesc Med. 2004;158:27–33. doi: 10.1001/archpedi.158.1.27. [DOI] [PubMed] [Google Scholar]
- 51.Spurgeon D. Childhood obesity in Canada has tripled in past 20 years. BMJ. 2002;324:1416. doi: 10.1136/bmj.324.7351.1416/f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kalies H, Lenz J, von Kries R. Prevalence of overweight and obesity and trends in body mass index in German pre-school children, 1982-1997. Int J Obes Relat Metab Disord. 2002;26:1211–1217. doi: 10.1038/sj.ijo.0802013. [DOI] [PubMed] [Google Scholar]
- 53.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1:11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- 54.Lobstein T, Frelut ML. Prevalence of overweight among children in Europe. Obes Rev. 2003;4:195–200. doi: 10.1046/j.1467-789x.2003.00116.x. [DOI] [PubMed] [Google Scholar]
- 55.Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, Armstrong R, Prosser L, Summerbell CD. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 3 doi: 10.1002/14651858.CD001871.pub3. CD001871. [DOI] [PubMed] [Google Scholar]
- 56.Swinburn B, Egger G, Raza F. (). Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med. 1999;29:563–570. doi: 10.1006/pmed.1999.0585. [DOI] [PubMed] [Google Scholar]
- 57.Davison KK, Birch ll. Childhood overweight: a contextual model and recommendations for future research. Obes Rev. 2001;2:159–171. doi: 10.1046/j.1467-789x.2001.00036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kremers SPJ, De Bruijn G-J, Visscher TLS, Van Mechelen W, De Vries NK, Brug J. Environmental influences on energy balance-related behaviors: a dual-process view. Int J Behav Nutr Phys Act. 2006;3:9. doi: 10.1186/1479-5868-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vandenbroeck IP, Goossens J, Clemens M. Foresight Tackling Obesities: Future Choices-Building the Obesity System Map. UK Government's Foresight Programme. UK Government Office for Science; 2007. [Google Scholar]
- 60.Cohen DA, Babey SH. Contextual influences on eating behaviours: heuristic processing and dietary choices. Obes Rev. 2012;13:766–779. doi: 10.1111/j.1467-789X.2012.01001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bemelmans WJE, Verschuuren M, van Dale D, Savelkoul M, Wendel-Vos GCW, van Raaij J. An EU-Wide Overview of Community-Based Initiatives to Reduce Childhood Obesity. Bilthoven: RIVM; 2011. [Google Scholar]
- 62.Romon M, Lommez A, Tafflet M, Basdevant A, Oppert JM, Bresson JL, Ducimetière P, Charles MA, Borys JM. Downward trends in the prevalence of childhood overweight in the setting of 12-year school- and community-based programmes. Public Health Nutr. 2009;12:1735–1742. doi: 10.1017/S1368980008004278. [DOI] [PubMed] [Google Scholar]
- 63. Borys J-M, Le Bodo Y, De Henauw S, Moreno LA, Romon M, Seidell JC, Visscher TLS. Preventing Childhood Obesity. EPODE European Network Recommendations. 2011. www.epode-international-network.com/sites/default/files/EEN_BOOK.pdf (last accessed February 24, 2014).
- 64.Borys J-M, Le Bodo Y, Jebb SA, Seidell JC, Summerbell C, Richard D, De Henauw S, Moreno LA, Romon M, Visscher TLS, Raffin S, Swinburn B. EPODE approach for childhood obesity prevention: methods, progress and international development. Obes Rev. 2012;13:299–315. doi: 10.1111/j.1467-789X.2011.00950.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, Allison TG, Batsis JA, Sert-Kuniyoshi FH, Lopez-Jimenez F. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond) 2008;32:959–966. doi: 10.1038/ijo.2008.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Borys J-M, Valdeyron L, Levy E, Vinck J, Edell D, Walter L, Ruault du Plessis H, Harper P, Richard P, Barriguette A. EPODE – a model for reducing the incidence of obesity and weight-related comorbidities. US Endocrinology. 2013;9:32–36. doi: 10.17925/EE.2013.09.02.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Commission of the European Communities White Paper on a Strategy for Europe on Nutrition, Overweight and Obesity Related Health Issues. Brussels, May 30, 2007, COM(2007) 279 final. http://ec.europa.eu/health/ph_determinants/life_style/nutrition/documents/nutrition_wp_en.pdf (lasst accessed February 25, 2014).
- 68.Romon M, Duhamel A, Salleron J, Lommez A, Meyer J, Borys J. Évolution de la prévalence du surpoids et de l'obésité chez les enfants de 4 à 11 ans entre 2005 et 2010 dans les villes «EPODE». Nutr Clin Metab. 2010;24((suppl 1)):58. [Google Scholar]
- 69. Borys J-M. Encouraging results in French EPODE Pilot towns, EEN Newsletter N°5 September 2010.
- 70. Preventing childhood obesity involving local stakeholders in a sustainable way: the VIASANO programme. ECOG Congress abstract, 2010.
- 71. EEN EEN press release: 22% fewer overweight children in nursery schools in Belgium thanks to the VIASANO programme. 2012. www.epode-international-network.com/sites/default/files/EIN_Viasano_PressRelease.pdf(last accessed February 25, 2014).
- 72. Directorate General for Health and Consumers of the European Commission EPODE European Network Project. Grant Agreement 2007327, DGSANCO. 2007.
- 73.Cross-Government Obesity Unit, Department of Health and Department of Children, Schools and Families . Healthy weight, healthy lives: a cross-government strategy for England. UK Department of Health; 2008. [Google Scholar]
- 74.Dutch Covenant on Overweight and Obesity . In search of the X Factor: energy in balance. La Haye: Dutch Covenant on Overweight and Obesity; 2008. [Google Scholar]
- 75.Levi J, Segal LM, Juliano C. Prevention for a healthier America: investments in disease prevention yield significant savings, stronger communities. Trust for America's Health, TFAH: February 2009. [Google Scholar]
- 76.Boyer V. Parliamentary Information Report – Conclusion of the Obesity Prevention Mission. 2008.
- 77.Falling Walls. Future breakthroughs in science and society. Berlin: Falling Walls Conference; 2009. [Google Scholar]
- 78.World Health Organization . Population-based prevention strategies for childhood obesity. Geneva: World Health Organization; 2009. [Google Scholar]
- 79. De Danne A. Committee for obesity prevention and treatment. Report to the President of the French Republic. 2009.
- 80.Etienne J, Bout B. Research perspectives on obesity prevention and treatment. French Parliament; 2009. [Google Scholar]
- 81. Public Health Agency of Canada Achieving healthier weights in Canada's communities. Call for proposals. May 2010.
- 82.Levi J, Vinter S, St. Laurent R, Segal LM. F as in Fat: how obesity threatens America's future. Trust for America's Health; 2010. [Google Scholar]
- 83. OPAL by EPODE programme South Australia Health, SA Health. 2010. www.opal.sa.gov.au (last accessed February 25, 2014).
- 84. EPODE-5 Pasos programme (Mexico) 2010. www.5pasos.mx (last accessed February 25, 2014).
- 85.Basdevant A, Bas-Theron F, Combris P, et al. Obesity: review and evaluation of obesity prevention and treatment programmes. INSERM; 2006. [Google Scholar]