Abstract
Purpose
More than 6,500 megavoltage teletherapy units are needed worldwide, many in low-resource settings. Cobalt-60 units or linear accelerators (linacs) can fill this need. We have evaluated machine performance on the basis of patient throughput to provide insight into machine viability under various conditions in such a way that conclusions can be generalized to a vast array of clinical scenarios.
Materials and Methods
Data from patient treatment plans, peer-reviewed studies, and international organizations were combined to assess the relative patient throughput of linacs and cobalt-60 units that deliver radiotherapy with standard techniques under various power and maintenance support conditions. Data concerning the frequency and duration of power outages and downtime characteristics of the machines were used to model teletherapy operation in low-resource settings.
Results
Modeled average daily throughput was decreased for linacs because of lack of power infrastructure and for cobalt-60 units because of limited and decaying source strength. For conformal radiotherapy delivered with multileaf collimators, average daily patient throughput over 8 years of operation was equal for cobalt-60 units and linacs when an average of 1.83 hours of power outage occurred per 10-hour working day. Relative to conformal treatments delivered with multileaf collimators on the respective machines, the use of advanced techniques on linacs decreased throughput between 20% and 32% and, for cobalt machines, the need to manually place blocks reduced throughput up to 37%.
Conclusion
Our patient throughput data indicate that cobalt-60 units are generally best suited for implementation when machine operation might be 70% or less of total operable time because of power outages or mechanical repair. However, each implementation scenario is unique and requires consideration of all variables affecting implementation.
INTRODUCTION
There is a great deficit and disparity in the number of teletherapy units across the world. Only four of 139 low- and middle-income countries (LMICs) are currently equipped with an adequate number of machines, and more than 9,000 machines will be needed by 2020.1 Linear accelerators (linacs) and cobalt-60 units can be used to meet this demand for teletherapy services, although the advantages of each machine are widely debated in the literature.2-6 Both machines have proved to be clinically acceptable and have a long history of successfully treating, curing, and palliating patients with cancer. Cobalt-60 units are cited as being more robust to the challenges of resource requirements, machine downtime, and operator demands, which allows for continued treatment in areas with relatively scarce resources. However, cobalt-60 units require radioactive material for which safety is a concern. Treatments delivered by using cobalt-60 units are hindered by lower dose rates than linacs, leading to longer treatments. In addition, under some circumstances and without the implementation of advanced technologies, cobalt-60 therapies have been shown to be dosimetrically unfavorable. In contrast, linacs feature higher dose rates, no radioactive material safety concerns, and treatments that can be delivered at higher energies. In addition, technological advances in radiotherapy delivery have led to the use of intensity-modulated radiation therapy (IMRT) and volumetric-modulated arc therapy (VMAT), as well as conformal radiotherapy with linacs. But the stringent power requirements and relatively long machine downtime needed for linacs call into question the viability of machine operation when infrastructure is limited, denoted herein as “low resource.”
In choosing the appropriate teletherapy machine for a particular region, it is important to investigate projected machine performance considering patient treatment needs, machine capabilities, and the framework of local infrastructure. As a first step, we have quantified the relative daily patient throughput of cobalt-60 units and linacs that deliver a range of treatment techniques under various infrastructure conditions in an effort to add quantitative data to the discussion of teletherapy machine implementation.
MATERIALS AND METHODS
Relative average daily patient throughput was modeled for six treatment scenarios (linac delivering conformal radiotherapy, step-and-shoot IMRT, dynamic IMRT, VMAT, and cobalt-60 unit delivering conformal radiotherapy with and without multileaf collimators [MLCs]) under three power outage conditions. Data from international organizations, peer-reviewed studies, clinical observations, and patient treatment plans were used to model daily operational time of the teletherapy units and patient treatment time. Machine availability for each scenario was calculated as the total number of working hours per day in which a power supply was available and the machine was otherwise in operable condition. Patient treatment time was calculated as described under Modeled Patient Population.
Machine Operability
Power outage scenarios.
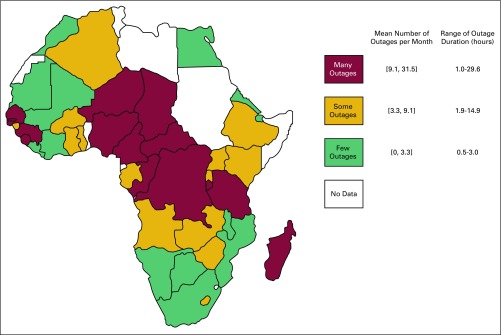
For the purpose of our study, it was assumed that although cobalt-60 units are functional during a power outage via generator-supplied power, linacs are inoperable during power outages. Using data from World Bank Enterprise Surveys, we recorded power outage frequency and duration in all 44 African countries for which data were available. African countries were used for this study because of the availability of data and the concentrated need for teletherapy.7 Data for multiple years for a single country were averaged, and the 44 data points were divided into three subgroups on the basis of frequency of outages. This discretization allowed for sampling of three power outage scenarios: many outages (an average of 9.1 to 31.5 outages per month), some outages (3.3 to 9.1 outages per month), and few outages (0 to 3.3 outages; Fig 1). Outage durations were sampled from the corresponding distribution of outage duration. The data were scaled from reported outages per month to daily values for power outages. In addition, each power outage was extended by 20 minutes to account for the time it takes to bring the machine back online after a power outage.
Fig 1.
Forty-four African countries with available power infrastructure data were divided into three groups on the basis of the number of outages experienced in a typical month.
Machine downtime.
To estimate machine downtime, we recorded fractional downtime in-house for 15 machines at The University of Texas MD Anderson Cancer Center over 16 months of operation, and daily machine downtimes were sampled from this distribution. To more closely reflect the machine operation and downtime characteristics of LMICs and low-resource settings in which onsite engineers and machine support staff may not be available, we created a second machine downtime distribution by scaling the collected data to reflect an average machine downtime of 8%, as reported for 30 linacs across 10 countries by van der Giessen et al.8 Data on cobalt-60 machine downtime were not available at our institution, nor were comprehensive analyses available in the literature. Those experienced with cobalt-60 machines suggested a downtime percentage of 1 week per 2 years of operation (1%); this value also reflects that reported in van der Giessen et al.8
Modeled Patient Population
In general, the treatment time needed per patient per fraction varies by type of machine, site of disease, prescribed dose, and delivery technique. Our modeled population included patients assigned a cancer site, radiation prescription, and treatment modality on the basis of cancer incidence and standard radiation prescriptions. Treatment time was then calculated (see Patient treatment time).
Cancer incidence and radiation prescription.
The vast diversity in cancer incidence among regions and countries indicates that teletherapy implementation should be undertaken with the projected patient population in mind. To reflect cancer incidence in the regions of power outage considered, we used published data on cancer incidence in eight African countries from Cancer Incidence in Five Continents, Volume X, from the International Agency for Research on Cancer.9 Nine cancer sites (breast, cervix, esophagus, head and neck, liver, lung, lymph node, prostate, and rectum) were identified, representing 40% to 80% of cancer incidence in each country. These percentages were averaged, normalized, and multiplied by the optimal fraction of patients receiving radiotherapy, as reported by Barton et al.10 Radiation prescriptions were assigned per site on the basis of current curative clinical schemes.
Patient treatment time.
Patient treatment time was calculated as the sum of setup, image guidance (optional), and beam delivery times.
It was assumed that the time needed for image guidance and setup was independent of the treatment machine, treatment technique, and cancer site. The distribution of patient setup times was acquired from clinical observations of 37 patient procedures. Image guidance time (2D-2D match), which was optional in patient treatment, was assumed to be 140 seconds,11 and this was verified with 31 clinical observations. Beam delivery time comprised beam-on and mechanical motion components.
Mechanical motion time included the time during which beam definition (field shape or beam angle) occurs. Beam-on time was calculated as the product of the prescribed dose (Gy), a percent depth dose correction factor (PDDC) which is applied for cobalt treatment only and scales the prescribed dose on the basis of the difference in percent depth dose characteristics of 6-MV linacs and cobalt-60 (PDDC, for cobalt-60 treatments only), a beam modulation factor (monitor units [MU]/Gy) which relates the number of monitor units needed to deliver the desired dose on the basis of treatment site and treatment technique, and the inverse dose rate (minutes/MU).
Treatment modality and cancer site-specific distributions of beam modulation factor (all modalities) and mechanical motion times (step-and-shoot IMRT) were acquired from more than 1,000 patient plans. Mechanical motion times for other modalities were approximated by using the required machine parameters. Mechanical motion time for step-and-shoot IMRT was calculated as the sum of the time for MLC definition over each beam segment (acquired by using a treatment planning script on 126 patient plans treated on Varian machines that incorporated segment order and leaf speed); it was assumed that gantry rotation time occurs simultaneously with MLC definition. For dynamic IMRT and conformal radiotherapy, mechanical motion time was set at 1 minute, under the assumption that beam angles span the full gantry extent and that gantry rotation occurs at one revolution per minute. For VMAT treatments, mechanical motion time was assumed to be 30 seconds, accounting for the collimator rotation between gantry arcs. Furthermore, total beam-on time for VMAT treatments was assumed to be at least 2 minutes or two arcs per treatment.
In addition, we considered two cobalt-60 treatment scenarios in which no MLCs were available, indicating the need for a therapist to add or change blocks. Through clinical observations, we estimated the time needed for one or three block changes per patient per fraction. One block change added 1 minute to the treatment time, and three block changes added 3.5 minutes to the treatment time.
For each treatment scenario, beam modulation factors and mechanical motion times were sampled from the distributions of treatment modality and cancer site incidence. If cobalt-60 was used, the prescribed dose was multiplied by a percent depth dose correction factor equal to 1.095, the average of the ratio of 6-MV and cobalt-60 depth doses under reference conditions from 1.5-cm to 10-cm depth. Finally, the inverse dose rate was used to calculate the beam-on time for each patient. The cobalt-60 dose rate decayed throughout the model duration, with an initial dose rate of 250 MU/minute corresponding to 100 MU/Gy under reference conditions. The linac dose rate was 600 MU/minute under reference conditions.
Daily patient throughput analysis.
For each modeled day, power outage and machine downtime values were sampled from the corresponding distributions. Patients with various treatment times according to treatment technique and cancer site were assumed to be treated until daily machine operation time had expired. Average daily patient throughput values were recorded for each of the treatment scenarios.
RESULTS
Patient Treatment Time
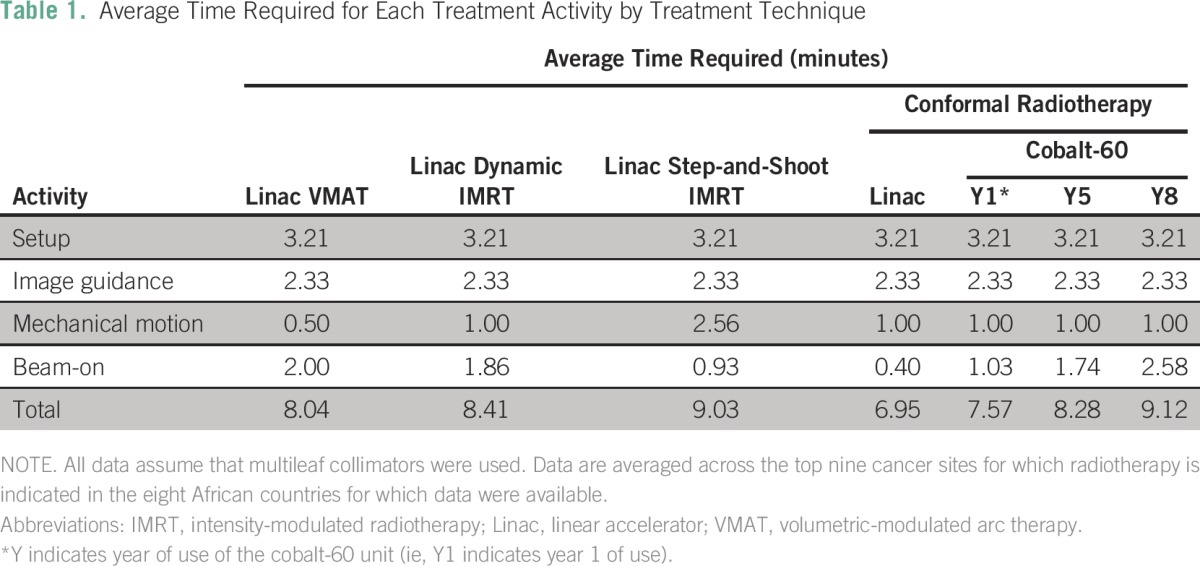
For each of the treatment scenarios, we determined the average time spent per treatment activity comprising the total average patient treatment time for each treatment scenario (Table 1). Shown are cobalt-60 units with MLCs during years 1, 5, and 8 of operation, in an effort to underscore the effect of source decay. Conformal radiotherapy during year 8 of cobalt-60 operation represented the longest average total treatment time, and step-and-shoot IMRT represented the second longest average total treatment time, largely because step-and-shoot IMRT required the longest average mechanical motion time (2.56 minutes).
Table 1.
Average Time Required for Each Treatment Activity by Treatment Technique
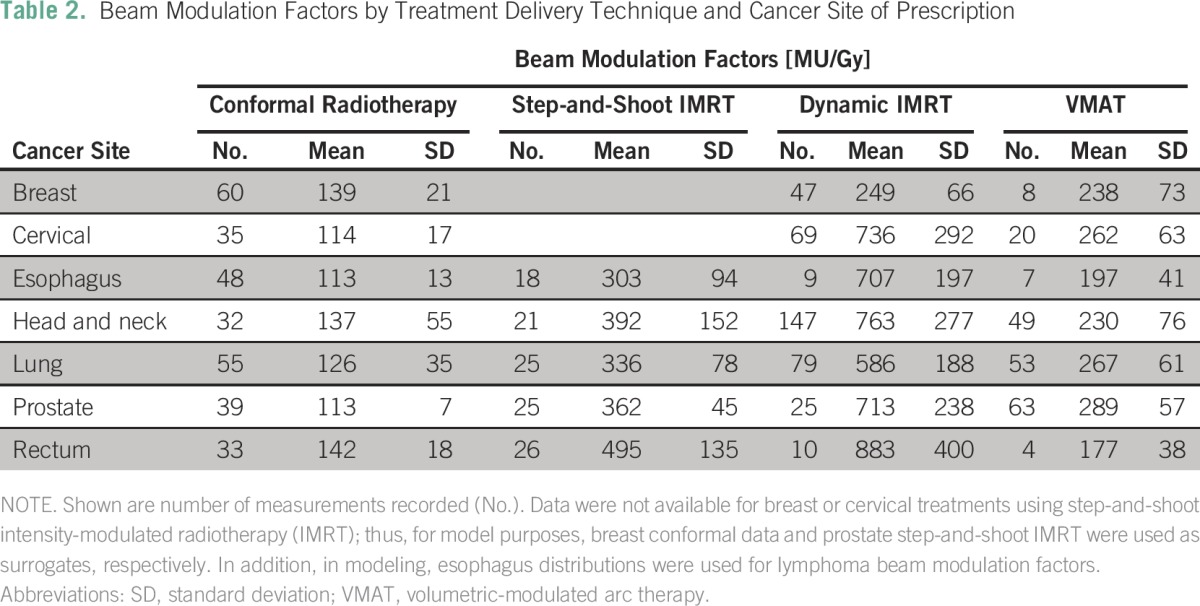
Beam modulation factors which, for each treatment technique and site, indicate the number of monitor units needed to deliver the prescribed dose, were collected from over 1,000 patient treatment plans. In Table 2, beam modulation factors for each treatment site for each of the four treatment techniques are shown the mean and standard deviation of the distributions recorded.
Table 2.
Beam Modulation Factors by Treatment Delivery Technique and Cancer Site of Prescription
Patient Throughput and Power Outage Conditions
Each of the treatment scenarios was considered under the three power outage conditions (many, some, or few power outages), assuming an average linac downtime distribution of 8%. The normalized daily patient throughput results are provided in Table 3. The average duration of daily power outages for each power outage condition is also reported.
Table 3.
Relative Daily Patient Throughput
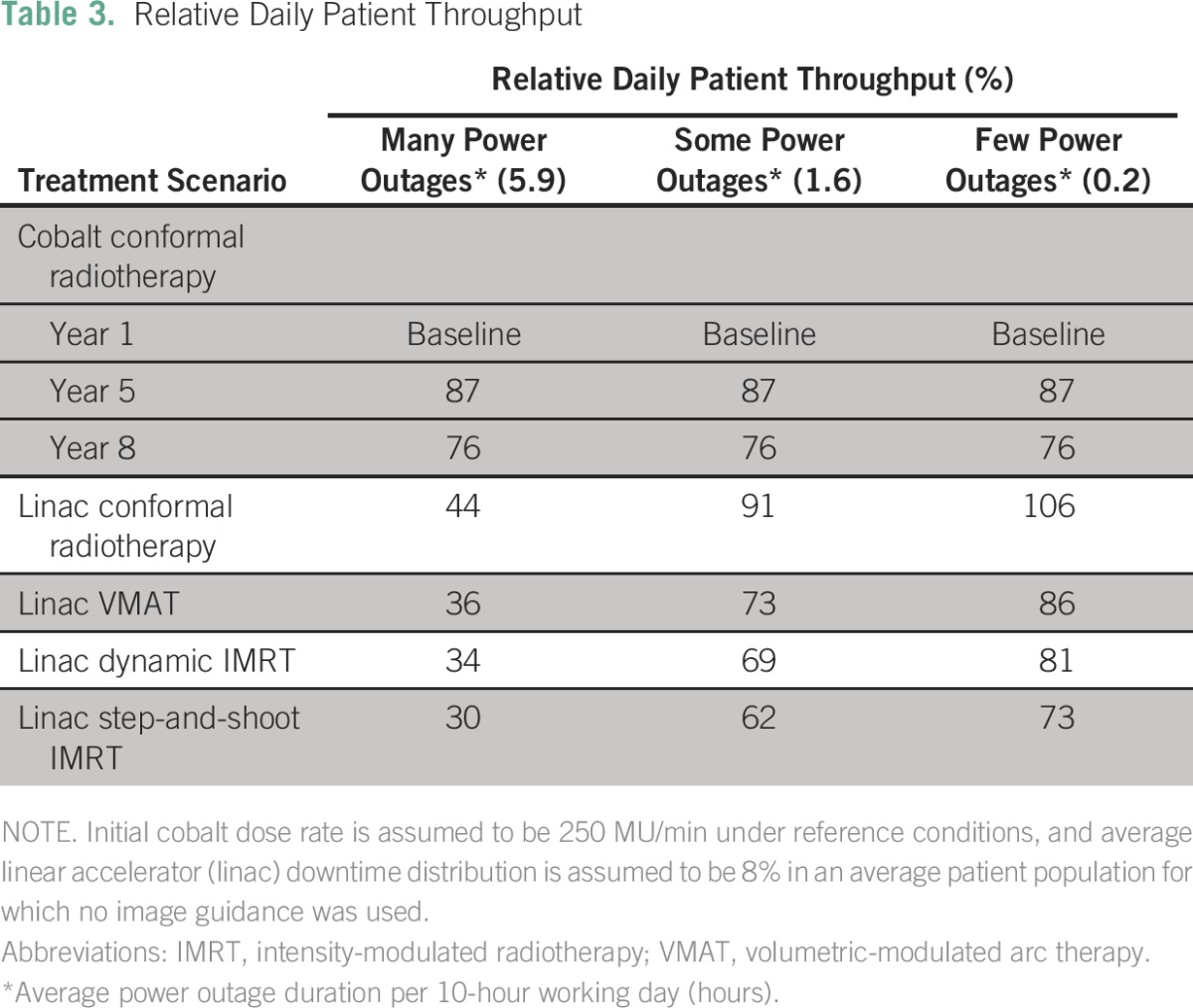
Through 5 years of cobalt-60 operation, after which dose rate is 130 MU/minute under reference conditions, daily patient throughput was 94% relative to year 1. For cobalt-60 operation through 8 years, (87 MU/minute), relative throughput was 88%. Linacs delivering conformal radiotherapy with few power outages showed the highest relative daily patient throughput, and linacs delivering step-and-shoot IMRT with many power outages showed the lowest throughput.
When linac downtime percentages were sampled from the distribution of data collected at The University of Texas MD Anderson Cancer Center (average 1.7%), linac throughput across all treatment schemes increased by an average of 4%, but relative performance at or above baseline did not change.
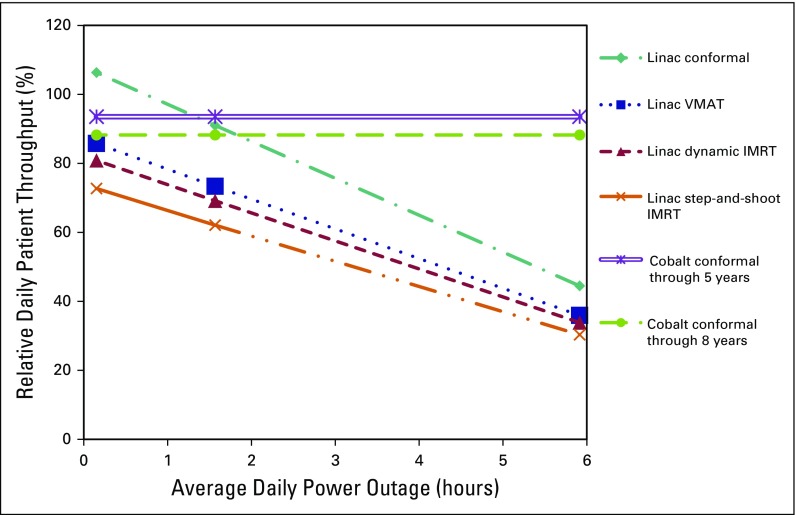
Power outages affected daily patient throughput more dramatically than did treatment scenarios. Figure 2 shows patient throughput for linacs delivering each of the four treatment types and cobalt-60 units through 5 and 8 years of operation by average daily power outage duration. Daily throughput for linac conformal radiotherapy was found to be equal to that of cobalt-60 units through 5 years of operation with average daily power outages of 1.34 hours and equal to that of cobalt-60 units through 8 years of operation with average daily power outages of 1.83 hours, assuming an average linac downtime of 8%. When the average linac downtime was assumed to be 1.7%, equal average daily patient throughput for conformal radiotherapy on linac and cobalt-60 machines through 5 and 8 years of operation was achieved at 1.88 and 2.34 average daily hours of power outage, respectively. In addition, equal throughput was observed for linac VMAT and cobalt-60 units through 8 years of operation with an average of 0.49 hours of daily power outage.
Fig 2.
Average daily patient throughput relative to cobalt-60 performance in year 1 of operation for four linear accelerator (linac) treatment techniques and for cobalt-60 units delivering conformal radiotherapy through 5 and 8 years of operation. Intersections represent the average daily duration of power outages for which the corresponding treatment machines and techniques are expected to have equal patient throughput. IMRT, intensity-modulated radiotherapy; VMAT, volumetric-modulated arc therapy.
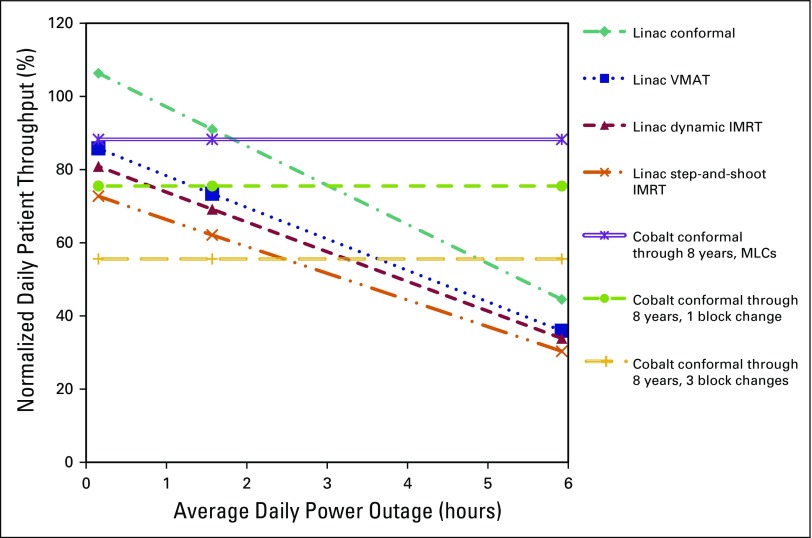
Finally, when considering the availability of MLCs, daily throughput decreased dramatically when block changes were required. In Figure 3, daily patient throughput for cobalt-60 units through 8 years of operation requiring one block change and three block changes per patient per fraction are shown. Relative to cobalt-60 units through 8 years of operation using MLCs, the need for one block change reduced the throughput to 86% and the need for three block changes reduced the throughput to 63%. The relative reduction in throughput observed when three block changes were required for cobalt-60 units made the throughput equal to that of the linac step-and-shoot IMRT modality (which had the lowest relative throughput) with an average of 2.47 hours of daily power outages per 10-hour working day.
Fig 3.
Average daily patient throughput relative to cobalt-60 performance in year 1 of operation for four linear accelerator (linac) treatment techniques and for cobalt-60 units operated over 8 years with multileaf collimators (MLCs), one block change, or three block changes per patient per fraction. Intersections represent the average daily duration of power outages for which the corresponding treatment machines and techniques are expected to have equal patient throughput. Linac downtime is sampled from the 8% average distribution. IMRT, intensity-modulated radiotherapy; VMAT, volumetric-modulated arc therapy.
DISCUSSION
Thousands of teletherapy units are needed in LMICs and in low-resource settings. The choice of teletherapy unit is an important one, especially considering the cost (both upfront and continuing) and lifetime of teletherapy units.12,13 Furthermore, the technologies associated with and the uses and capabilities of a treatment machine, while presumably dynamic over time, can have an impact on the number of patients able to receive possibly lifesaving radiotherapy services. We have quantitatively explored the relative daily patient throughput characteristics of linac and cobalt-60 teletherapy units operating with many treatment techniques and under various infrastructure scenarios. Our results underscore and re-emphasize the importance of power infrastructure characteristics at the site of implementation. It is clear that a complete understanding of the power availability in the region of projected implementation is, without doubt, critical in estimating potential machine performance. Under scenarios of moderate power outages (fewer than 1.6 average hours of power outage per 10-hour working day), conformal treatment techniques delivered with MLCs on cobalt-60 units or linacs can be expected to achieve similar patient throughput. It is our hope that the results of this study can inform the reader who also has a knowledge of their individual clinic regarding the impact of machine type and treatment choices.
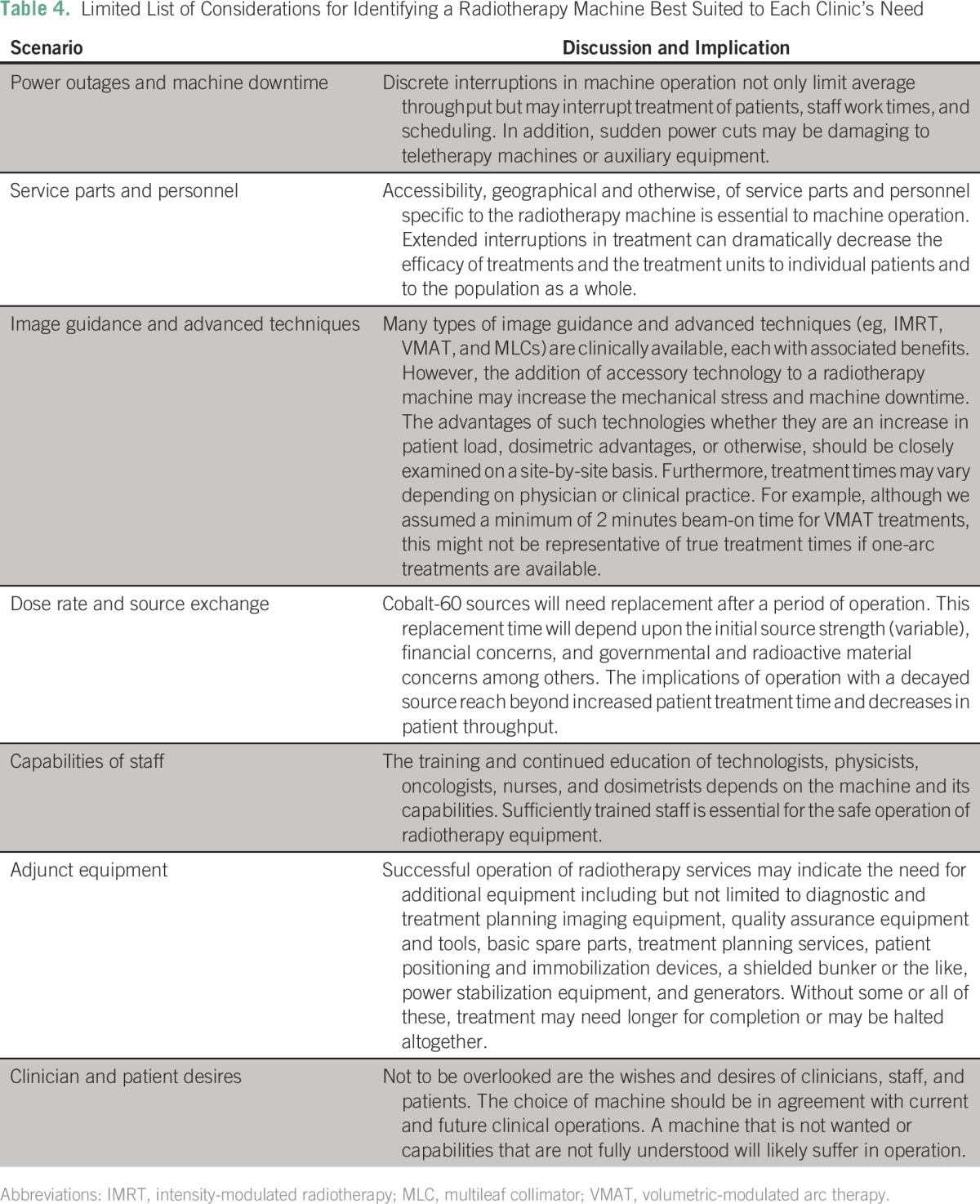
Machine implementation is a multifaceted and highly complex issue. It is impractical, and likely impossible, to completely model the projected machine performance over an extended period of time while considering all variables and scenarios that are likely to arise. As a partial acknowledgment of additional considerations, Table 4 discusses scenarios of note and their implications. Our work mainly focuses on the effect of power outages and machine downtime on relative machine performance. This is a simple first step in an effort to clearly elucidate projected machine performance.
Table 4.
Limited List of Considerations for Identifying a Radiotherapy Machine Best Suited to Each Clinic’s Need
A relative average daily throughput analysis was conducted according to data availability. Day-to-day variation in patient throughput may have impacts beyond patient throughput, including interruptions in treatment, staffing resources, and machine performance.
Considering treatment time, advanced treatment techniques, with the exception of MLCs, reduce patient throughput because of increased mechanical motion or beam-on times. Although it is beyond the scope of this investigation, the indication for implementation of these advanced techniques is debated.14,15 When considering cobalt-60 teletherapy units and the availability of MLCs, if physical block changes are needed, a substantial reduction in patient throughput is seen. If three block changes are needed per patient per fraction, throughput is decreased 37%, relative to operation with MLCs. Although block changes may not be indicated in all treatment regimens, as assumed here, our results indicate the critical role automatic beam shaping devices can play in maximizing patient throughput, but we do not consider the burden this may place on machine downtime. In addition, although a scenario of operation without MLCs was considered only for cobalt-60 units, linacs will also be subject to throughput decreases if MLCs are not used.
Often cited as a disadvantage of cobalt-60 teletherapy is the limited source strength available.2,4 We have shown that source decay (initial source strength 2.5 Gy/min at 80 cm) over 8 years represents an increase in patient treatment time of 1.5 minutes per treatment (or 20%). Although with lower initial source strengths and less frequent cobalt-60 source exchanges, patient treatment time can become prohibitively long as a result of increased beam-on time. Thus, the projected availability of cobalt-60 sources must be considered upon machine implementation.
Although the circumstances surrounding each scenario of machine implementation are unique, our analysis quantitatively compared the projected performance of cobalt-60 machines and linacs in low-resource settings. Power infrastructure is implicated as a key factor in the choice of teletherapy machine, but cobalt-60 source availability as well as the use of advanced treatment techniques, including IMRT, VMAT, and MLCs, must also be considered.
AUTHOR CONTRIBUTIONS
Conception and design: Rachel McCarroll, Bassem Youssef, Beth Beadle, Geoffrey Ibbott, Christoph Trauernicht, Peter Balter, Laurence Court
Financial support: Rachel McCarroll, Geoffrey Ibbott, Laurence Court
Administrative support: Rachel McCarroll, David Followill, Geoffrey Ibbott, Laurence Court
Provision of study materials or patients: All authors
Collection and assembly of data: Rachel McCarroll, Bassem Youssef, Beth Beadle, Rex Cardan, Robin Famiglietti, David Followill, Peter Balter, Laurence Court
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/site/ifc.
Rachel McCarroll
No relationship to disclose
Bassem Youssef
Travel, Accommodations, Expenses: Merck
Beth Beadle
No relationship to disclose
Maureen Bojador
No relationship to disclose
Rex Cardan
Honoraria: Varian Medical Systems
Consulting or Advisory Role: Varian Medical Systems
Research Funding: Varian Medical Systems
Patents, Royalties, Other Intellectual Property: Collision avoidance systems for radiotherapy
Travel, Accommodations, Expenses: Varian Medical Systems
Robin Famiglietti
No relationship to disclose
David Followill
No relationship to disclose
Geoffrey Ibbott
Stock or Other Ownership: Accuray (I)
Research Funding: Varian Medical Systems (Inst), Elekta (Inst)
Travel, Accommodations, Expenses: Elekta
Anuja Jhingran
No relationship to disclose
Christoph Trauernicht
No relationship to disclose
Peter Balter
Employment: University of Texas MD Anderson Cancer Center, University of Texas School of Dentistry (I)
Honoraria: Sun Nuclear Corporation, International Atomic Energy Agency
Speakers’ Bureau: Varian Medical Systems
Research Funding: Varian Medical Systems
Travel, Accommodations, Expenses: Sun Nuclear Corporation
Laurence Court
No relationship to disclose
REFERENCES
- 1.Datta NR, Samiei M, Bodis S. Radiation therapy infrastructure and human resources in low- and middle-income countries: Present status and projections for 2020. Int J Radiat Oncol Biol Phys. 2014;89:448–457. doi: 10.1016/j.ijrobp.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Ravichandran R. Has the time come for doing away with Cobalt-60 teletherapy for cancer treatments. J Med Phys. 2009;34:63–65. doi: 10.4103/0971-6203.51931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Dyk J, Battista JJ Cobalt-60: An old modality, a renewed challenge. Curr Oncol. 1996;3:8–17. [Google Scholar]
- 4.Page BR, Hudson AD, Brown DW, et al. Cobalt, linac, or other: What is the best solution for radiation therapy in developing countries? Int J Radiat Oncol Biol Phys. 2014;89:476–480. doi: 10.1016/j.ijrobp.2013.12.022. [DOI] [PubMed] [Google Scholar]
- 5.Adams EJ, Warrington AP. A comparison between cobalt and linear accelerator-based treatment plans for conformal and intensity-modulated radiotherapy. Br J Radiol. 2008;81:304–310. doi: 10.1259/bjr/77023750. [DOI] [PubMed] [Google Scholar]
- 6.Warrington J, Adams L: Cobalt 60 teletherapy for cancer: A revived treatment modality for the 21st century. Presented at the Appropriate Medical Technology for Developing Countries (Ref. No. 2002/057) IEE Seminar, 2002.
- 7.Abdel-Wahab M, Bourque JM, Pynda Y, et al. Status of radiotherapy resources in Africa: An International Atomic Energy Agency analysis. Lancet Oncol. 2013;14:e168–e175. doi: 10.1016/S1470-2045(12)70532-6. [DOI] [PubMed] [Google Scholar]
- 8. van der Giessen PH, Alert J, Badri C, et al: Multinational assessment of some operational costs of teletherapy. Radiother Oncol 71:347-355, 2004 . [DOI] [PubMed]
- 9.Forman D, Bray F, Brewster DH, et al (eds): Cancer Incidence in Five Continents, Vol. X. Lyon, France, International Agency for Research on Cancer, IARC Scientific Publications No. 164, 2014. [Google Scholar]
- 10.Barton MB, Jacob S, Shafiq J, et al. Estimating the demand for radiotherapy from the evidence: A review of changes from 2003 to 2012. Radiother Oncol. 2014;112:140–144. doi: 10.1016/j.radonc.2014.03.024. [DOI] [PubMed] [Google Scholar]
- 11. doi: 10.6009/jjrt.2012_jsrt_68.10.1327. Takenaga E, Nakaguchi Y, Maruyama M, et al: Comparison of various image guided radiation therapy systems; image-guided localization accuracy and patient throughput [in Japanese]. Nihon Hoshasen Gijutsu Gakkai Zasshi 68:1327-1332, 2012. [DOI] [PubMed] [Google Scholar]
- 12. Samiei M: Challenges of making radiotherapy accessible in developing countries. Cancer Control 85-96, 2013. [Google Scholar]
- 13.Datta NR, Heuser M, Samiei M, et al. Teleradiotherapy network: Applications and feasibility for providing cost-effective comprehensive radiotherapy care in low- and middle-income group countries for cancer patients. Telemed J E Health. 2015;21:523–532. doi: 10.1089/tmj.2014.0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salminen EK, Kiel K, Ibbott GS, et al. International Conference on Advances in Radiation Oncology (ICARO): Outcomes of an IAEA meeting. Radiat Oncol. 2011;6:11. doi: 10.1186/1748-717X-6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vikram B, Coleman CN, Deye JA. Current status and future potential of advanced technologies in radiation oncology. Part 1. Challenges and resources. Oncology (Williston Park) 2009;23:279–283. [PubMed] [Google Scholar]