ABSTRACT
Background
Exposure to underserved areas during training may increase residents' likelihood of practice in these settings. The Marshall University Family Medicine Residency offers a supplemental continuity experience at a local free clinic to interested residents.
Objective
We assessed the association of such an experience with graduate practice choices.
Methods
We evaluated all residency graduates (N = 138) who completed our family medicine program from 1997 through 2014 and compared participants in the free clinic experience to nonparticipants. Various characteristics and outcome measures were collected retrospectively from resident records maintained for program accreditation.
Results
A total of 43 residents participated in the free clinic experience compared with 95 nonparticipants. Postgraduation practice in an area of need was seen for 56% (24 of 43) of participants compared with 31% (29 of 95) of nonparticipants (P = .005). The 53 graduates practicing in areas of need were nearly twice as likely to have taken part in the free clinic experience (45% [24 of 53] versus 22% [19 of 85], P = .005). Participants were more likely to practice in rural areas (63%, 27 of 43) than residents who did not participate (43% [41 of 95], P = .033). Board certification rates were high for both free clinic participants (98%, 42 of 43) and nonparticipants (95% [90 of 95], P = .43).
Conclusions
Resident participation in a supplemental continuity experience at a free clinic was associated with practicing in areas of need and rural communities after graduation.
What was known and gap
Resident exposure to care of underserved populations during training may increase their likelihood of practice in areas of need, but the effect of resident participation in voluntary continuity experiences in free clinics has not been studied.
What is new
A study of the association between voluntary participation in a continuity residency experience at a free clinic serving underserved patients and location of practice after graduation.
Limitations
Single site, single specialty study; high potential for selection bias.
Bottom line
Residents who participated in the free clinic experience were more likely to practice in communities of need and rural settings after graduation.
Introduction
Since its inception in 1977, the Marshall University Family Medicine Residency Program in Huntington, West Virginia, has maintained a focus on preparing primary care physicians for rural and small-town practice in underserved communities. Because the program is located in a state where a majority of counties are medically underserved,1 the training of highly qualified family physicians to serve the health care needs of West Virginia and the surrounding Appalachian region is a major tenet of its mission. Over the years, the program has developed several initiatives designed to increase the number of graduates practicing in the region's areas of need. We established West Virginia's first rural residency track in 1994 in cooperation with a community health center, which has demonstrated to be effective in graduating family physicians who practice in rural areas of West Virginia.2 In 1995, the program began to offer family medicine residents a longitudinal experience at a free clinic that serves the uninsured of the region, with the hope of encouraging and supporting interest in caring for underserved populations.
Published literature on the educational experiences provided at free clinics is limited. Most articles tend to focus on clinics run by medical students,3–10 and only a few attempt to address how student participation in these activities affects their future career choices.10 This is even more relevant for postgraduate residency education.11
We assessed the relationship between resident participation in a longitudinal free clinic educational experience and several outcomes of graduates, with particular emphasis on practice in medically underserved communities.
Methods
Setting and Participants
The free clinic, named Ebenezer Medical Outreach (EMO) Center, is located in an underserved community in Huntington, West Virginia. This medical clinic has provided free care to uninsured individuals from the surrounding region for more than 2 decades, beginning in 1989 as a joint effort between Ebenezer Methodist Church and Marshall University Department of Family and Community Health. It transitioned to a separate incorporated entity with a supervising board of directors in 2002. This clinic has grown to a fully equipped facility with 8 examination rooms, located in a newly restored historic high school building.
Services have expanded to include primary care clinics, multiple subspecialty clinics, a free pharmacy, women's preventive services, counseling, dental services, and health education. The clinic has been supported through a combination of grants, donations (from 2 local hospitals and people in the community), and volunteer efforts. Patients are eligible for care if they are uninsured and below 200% of the federal poverty level. There are no other prerequisites. Although not a requirement, all patients at the clinic are US citizens (57% female, 15% minorities). At its peak, the clinic provided care for approximately 1800 patients, averaging 7500 encounters each year. The 2013 US census data indicated that 14% of West Virginians (255 000) lacked health insurance.12 All activities at the clinic have been provided on a volunteer basis, with no cost to the clinic. The costs of resident and faculty participation have been absorbed by the family medicine department as part of its community outreach efforts.
Intervention
Beginning in 1995, Marshall Family Medicine residents have been offered the opportunity to provide longitudinal care at the clinic with scheduled patients once a week. This experience supplemented their standard continuity practice without negatively affecting work hour restrictions. Each year, rising second-year residents were informed of the clinical experience offered at the clinic, and interested residents were assigned a weekly single half-day continuity session, with supervision provided by Marshall University Department of Family and Community Health faculty. Residents were not required to participate. All other elements of the curriculum were the same. The first residents began to see patients at the free clinic in 1995 and graduated in 1997.
Outcome Measures
We evaluated all graduates (N = 138) who had completed our family medicine program from 1997 through 2014. All residents were graduates of accredited US medical schools (95% allopathic, 5% osteopathic), and 59% (81 of 138) were from West Virginia. Various characteristics and outcome measures were collected retrospectively from records maintained for program accreditation. This included information obtained at residency enrollment, during residency training, through exit interviews at graduation, and via surveys and telephone following graduation.
In addition to free clinic participation, we collected on the following topics:
Age, sex, West Virginia hometown
Medical school attended
Graduation year
Practice location in areas of need, including medically underserved areas (MUAs) as defined by the Health Resources and Services Administration (HRSA) and Health Professional Shortage Area (HPSA as defined by HRSA)13
Practice location in rural or small-town communities (small rural < 2500 population and intermediate rural 2500–10 000 population as defined by the US Department of Agriculture Economic Research Service14)
Practice type as primarily traditional primary care or non–primary care (eg, hospitalists, occupational medicine, emergency medicine)
Economically disadvantaged background (HRSA poverty guidelines15)
Certification by the American Board of Family Medicine or the American Osteopathic Board of Family Physicians
Our main study outcomes focused on graduates who practice in areas of need and in rural areas. Graduates' practice addresses were used to determine location in MUAs, HPSAs, and rural/small-town designations.
This study was approved by the Marshall University Institutional Review Board.
Analysis
We compared outcomes of graduates who were free clinic participants to those of nonparticipants from 1997 through 2014. Continuous variables were summarized using the mean, except for age, which was not normally distributed. Comparisons of study variables for participants and nonparticipants were carried out using the chi-square test (or Fisher's exact test when appropriate) for categorical variables, and Student's t test (or Wilcoxon rank sum test if non-normal) for continuous variables. All analyses were performed using Stata version 13.0 (StataCorp LP, College Station, TX).
Results
Table 1 summarizes the results of our comparison of free clinic participants (n = 43) with nonparticipants (n = 95) for 1997 through 2014. Table 2 compares characteristics of the 53 residency graduates who chose to practice in an area of need with those of the 85 graduates who did not.
Table 1.
Comparison of Free Clinic Participant Residents (EMO) and Nonparticipant Residents (Non-EMO)
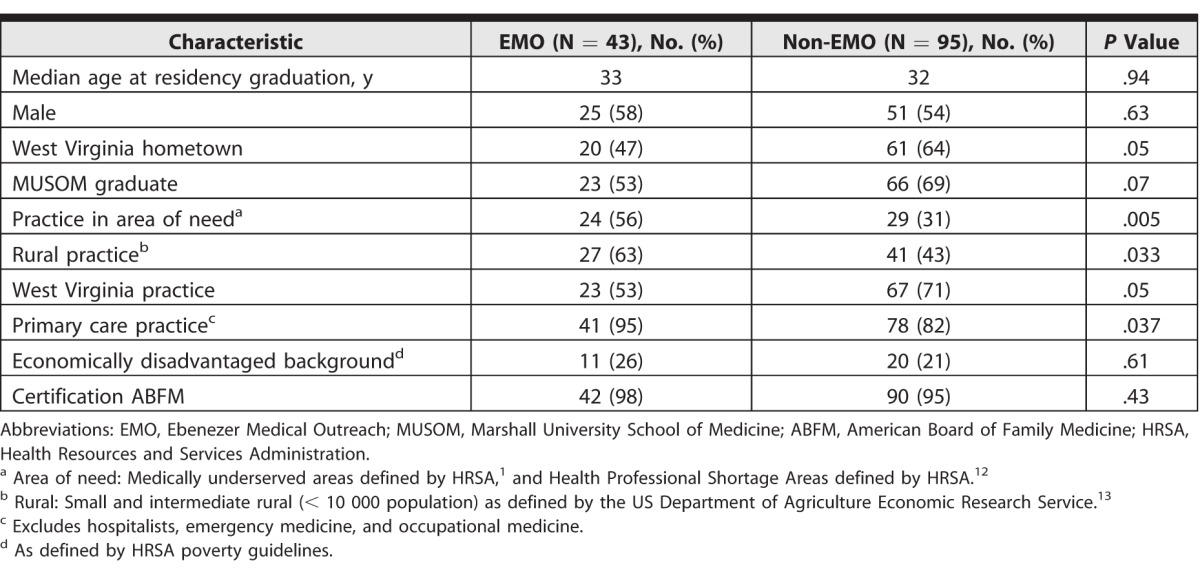
Table 2.
Comparison of Graduate Characteristics Between Practicing in an Area of Need and Practicing in Nonshortage Areas
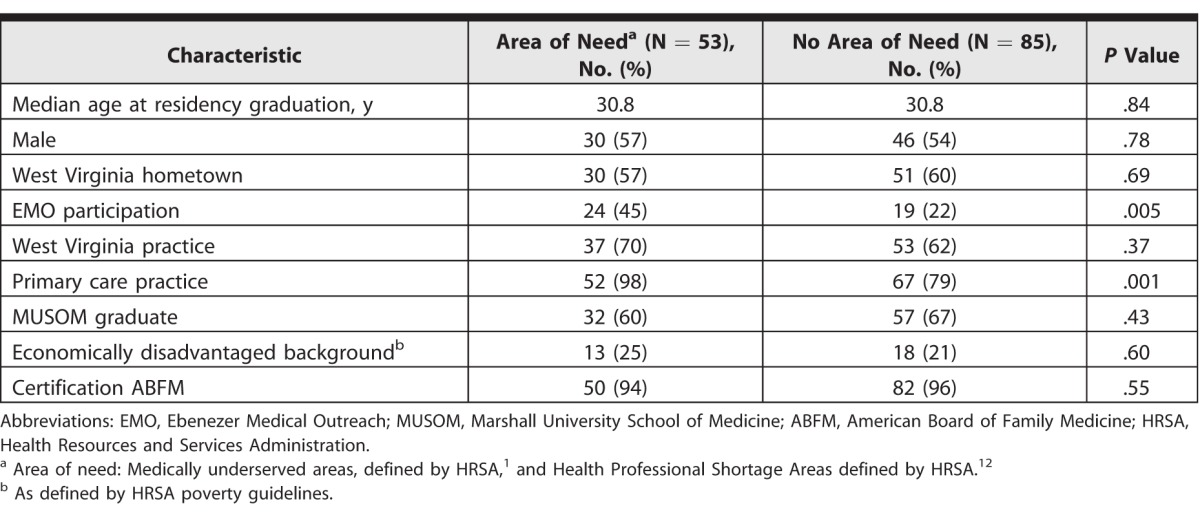
The residents who participated in the free clinic experience were more likely to practice in areas of need after graduation (56% [24 of 43]) than those who did not (31% [29 of 95], P = .005). Additionally, graduates practicing in areas of need were nearly twice as likely to have participated in the free clinic experience (45% [24 of 53] versus 22% [19 of 85], P = .005). Participants were more likely to practice in rural areas (63% [27 of 43] versus 43% [41 of 95], P = .033) and were more likely to practice traditional primary care (95% [41 of 43] versus 82% [78 of 95], P = .037).
A total of 38% (n = 53) of all Marshall family medicine graduates during the study period practiced in areas of need.
The residency program has averaged 2.5 participants in the free clinic per year during the 17-year period of the study. Nonparticipant graduates were more likely to choose alternative practice types than the participants, who were more likely to choose traditional primary care practice.
Discussion
Our findings suggest that the opportunity to provide longitudinal care in a free clinic setting may have supported the program's efforts to graduate family physicians who serve in areas of need and rural communities. Interestingly, residents from an economically disadvantaged background were no more likely to participate in the free clinic experience than other residents (Table 1) and were no more likely to practice in an area of need (Table 2).
Free clinic participating residents were more likely to practice in rural areas. The clinic is located in a small city with a population of less than 50 000 that is central to mostly rural central Appalachia. Many patients seen there are drawn from the surrounding rural areas, and the majority of regional opportunities for our graduates to work in areas of need (MUAs, HPSAs) are located in rural communities, likely contributing to our findings.
A study on the social mission of medical education ranked Marshall University School of Medicine in the top 20 (16th of 141) of American allopathic and osteopathic medical schools, and included graduates practicing primary care in shortage areas as a major ranking criteria.16 Marshall students interested in family medicine are highly recruited to our program and make up a substantial portion of the resident complement. This group of graduates may be more likely to consider future practice in medically underserved communities and West Virginia. In addition, our residency recruiting efforts include informing all applicants of the EMO opportunity to attract students who have an interest in working with underserved populations.
Our study predates the impact of the Affordable Care Act, and while the numbers of uninsured served by the free clinic have subsequently decreased in response to the full implementation of the Affordable Care Act, the clinic remains active and this learning opportunity continues, demonstrating its sustainability.
Our study has several limitations. Our sample is small and from a single residency program. We were not able to assess the impact of marital status or growing up in a medically underserved community at the time of graduation on practice choice. Some selection bias likely occurred in residents who chose to participate in the EMO continuity clinic. Both the program and the free clinic experience likely attracted residents who already have an interest in and are committed to working with the medically underserved in their future practice.
Conclusion
Family medicine residency graduates who participated in a weekly continuity practice at a free clinic were more likely to practice in areas of need, to practice in a rural setting, and to provide traditional primary care than those who did not take part in the free clinic experience.
References
- 1. . Health Resources and Services Administration (HRSA) Data Warehouse. MUA find. http://muafind.hrsa.gov/index.aspx. Accessed July 27, 2017.
- 2. . Petrany SM, Gress T. . Comparison of academic and practice outcomes of rural and traditional track graduates of a family medicine residency program. Acad Med. 2013; 88 6: 819– 823. [DOI] [PubMed] [Google Scholar]
- 3. . Butala NM, Chang H, Horwitz LI, et al. . Improving quality of preventive care at a student-run free clinic. PLoS One. 2013; 8 11: e81441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. . Zucker J, Lee J, Khokhar M, et al. . Measuring and assessing preventive medicine services in a student-run free clinic. J Health Care Poor Underserved. 2013; 24 1: 344– 358. [DOI] [PubMed] [Google Scholar]
- 5. . Wang T, Bhakta H. . A new model for interprofessional collaboration at a student-run free clinic. J Interprof Care. 2013; 27 4: 339– 340. [DOI] [PubMed] [Google Scholar]
- 6. . Smith SD, Johnson ML, Rodriguez N, et al. . Medical student perceptions of the educational value of a student-run free clinic. Fam Med. 2012; 44 9: 646– 649. [PubMed] [Google Scholar]
- 7. . Colbert CY, Ogden PE, Lowe D, et al. . Students learn systems-based care and facilitate system change as stakeholders in a free clinic experience. Adv Health Sci Educ Theory Pract. 2010; 15 4: 533– 545. [DOI] [PubMed] [Google Scholar]
- 8. . Moskowitz D, Glasco J, Johnson B, et al. . Students in the community: an interprofessional student-run free clinic. J Interprof Care. 2006; 20 3: 254– 259. [DOI] [PubMed] [Google Scholar]
- 9. . Niescierenko ML, Cadzow RB, Fox CH. . Insuring the uninsured: a student-run initiative to improve access to care in an urban community. J Natl Med Assoc. 2006; 98 6: 906– 911. [PMC free article] [PubMed] [Google Scholar]
- 10. . Campos-Outcalt DE. . Specialties chosen by medical students who participated in a student-run, community-based free clinic. Am J Prev Med. 1985; 1 4: 50– 51. [PubMed] [Google Scholar]
- 11. . Pincavage AT, Razi RR, Arora VM, et al. . Resident education in free clinics: an internal medicine continuity clinic experience. J Grad Med Educ. 2013; 5 2: 327– 331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. . Smith JC, Medalia C. . Health insurance coverage in the United States: 2013. Current population reports. September 2014. http://www.nber.org/cps/hi/2014redesign/p60-250.pdf. Accessed July 27, 2017.
- 13. . Health Resources and Services Administration (HRSA) Data Warehouse. HPSA find. http://datawarehouse.hrsa.gov/tools/analyzers/hpsafind.aspx. Accessed July 27, 2017.
- 14. . US Department of Agriculture Economic Research Service. What is rural? http://www.ers.usda.gov/topics/rural-economy-population/rural-classifications/what-is-rural.aspx. Accessed July 27, 2017.
- 15. . US Department of Health and Human Services Health Resources and Services Administration. Federal poverty guidelines. https://www.hrsa.gov/gethealthcare/affordable/hillburton/povertyguidelines.html. Accessed July 27, 2017.
- 16. . Mullan F, Chen C, Petterson S, et al. . The social mission of medical education: ranking the schools. Ann Intern Med. 2010; 152 12: 804– 811. [DOI] [PubMed] [Google Scholar]


