ABSTRACT
Purpose:
Vascular inflammation and leakage in sepsis is mediated by Angiopoietin-1 (Ang-1) and Angiopoietin-2 (Ang-2) and their phosphorylation of the endothelial Tie-2 receptor. This study investigates levels of Ang-1 and Ang-2 in newborns to gain insight in the vascular pathophysiology of early onset sepsis (EOS) within 72 h after birth.
Methods:
A prospective cohort study was performed among 71 Surinamese newborns treated with antibiotics for suspected EOS and 20 control newborns. Newborns with suspected EOS were divided in two groups: blood culture negative and positive EOS. Ang-1 and Ang-2 levels were measured in serum obtained at the start of antibiotic treatment and at re-evaluation after 48 to 72 h.
Results:
In this cohort 8.5% of newborns had a positive blood culture. At the start of antibiotic treatment Ang-1 serum levels were lower (P < 0.01), and Ang-2 and Ang-2/Ang-1 serum protein ratios were higher (P < 0.01 and P < 0.01, respectively) in newborns with blood culture positive EOS than in controls. These levels were not dependent on timing of first blood draw after birth. After 48 to 72 h levels of Ang-1 further decreased in blood culture positive EOS, while in the other groups no change was observed.
Conclusions:
Our findings support the hypothesis that a disbalance in the Angiopoietins plays a role in the vascular pathophysiology of EOS.
Keywords: Angiopoietins, early onset sepsis, newborn, Suriname
Abbreviations: Ang-1, angiopoietin-1, Ang-2, angiopoietin-2, EOS, early onset sepsis, Tie-2, TEK tyrosine kinase endothelial-2 receptor
INTRODUCTION
Sepsis is a syndrome with physiologic, pathological, and biochemical changes induced by an infection, and occurs in all age groups (1). Early onset sepsis (EOS) in newborns, defined as onset of sepsis within 72 h after birth, remains a clinical diagnostic and therapeutic challenge due to its nonspecific clinical presentation. This is associated with late discovery and undertreatment of septic newborns or overtreatment with antibiotics of uninfected ones (2–4). These diagnostic and therapeutic problems arise because the pathophysiology of EOS is not completely understood (3–5).
One of the pathological changes in septic patients is microvascular dysfunction leading to increased vascular inflammation and leakage (6). Vascular endothelial cells control these changes through the Angiopoietin/Receptor Tyrosine Kinase (Tie)-2 endothelial receptor system, which is severely disturbed in sepsis (6–9). The system consists of the ligands Angiopoietin-1 (Ang-1) and Angiopoietin-2 (Ang-2) (9). In health, Ang-1-Tie2 binding promotes intracellular Tie-2 phosphorylation, which prevents the occurrence of vascular inflammation and vascular leakage (10). During sepsis, Ang-2 dose dependently competes with Ang-1, which inhibits Tie-2 phosphorylation and induces destabilizing vascular inflammation and leakage (11, 12). In sepsis in children and adults, higher Ang-2 levels and Ang-2/Ang-1 ratios in blood are associated with presence, severity, and outcome of sepsis, while changes in Ang-1 levels are less uniformly present (13–17). To date, there is insufficient knowledge if disturbances in the Angiopoietin/Tie2 system also reflect the activation state of the endothelium during EOS in newborns (18). Furthermore, no data exists on the Angiopoietins during EOS from non-Western countries, such as Suriname.
Therefore, we studied the levels and behavior of Ang-1 and Ang-2 at the start of antibiotic treatment and at re-evaluation between 48 to 72 h in Surinamese newborns with suspected EOS. We hypothesized that lower Ang-1 and higher Ang-2 and Ang-2/Ang-1 protein ratio were associated with blood culture positive EOS.
PATIENTS AND METHODS
Study design and subjects
A prospective observational cohort study was performed at the neonatal care facility of the Academic Pediatric Center Suriname at the Academic Hospital Paramaribo. Patients were included in a 14-month period between April 1, 2015 and May 31, 2016. Newborns with a gestational age equal to or above 34 weeks in whom antibiotics were started within the first 72 h of life for suspected EOS were included. Excluded were neonates of whom no serum was obtained or not enough information was available after the study period to confirm outcomes. Written informed consent was obtained from at least one parent for the use of residual serum and clinical information. The study protocol was approved by the Surinamese Medical-Ethical Board (VG-021-14A) and was made available on clinicaltrials.gov (Trial registration: NCT02486783 registered 27/6/2015).
Clinical protocol
For all newborns, the standard local protocol for the management of suspected EOS was followed. This included the start of antibiotics after blood collection for culture and serial laboratory testing of infectious parameters (t = 0). Intravenous ampicillin (50–75 mg/kg/day) and gentamycin (5 mg/kg/day) were started based on the presence of maternal risk factors for infection (i.e., positive group B streptococcus culture, (premature) prolonged rupture of membranes, intrapartum fever or intrapartum antibiotics) and/or clinical signs of infection of the newborn. Controls were newborns without signs of infection receiving blood draws for hyperbilirubinemia. In these controls, no antibiotics were started. Newborns in whom antibiotics were started were divided into two groups based on blood culture result: blood culture negative EOS and blood culture positive EOS.
Data collection
For all newborns maternal information (i.e., history, pregnancy complications (i.e., presence of diabetes mellitus, pregnancy-induced hypertension or preeclampsia) and maternal risk factors for infection) was recorded, along with gestational age (if unknown according to Ballard), Apgar scores, birth weight, gender, ethnicity, results from laboratory testing (white blood cell counts and C-reactive protein (CRP) levels), duration of antibiotic treatment, blood culture results, hospital course, and mortality.
Sample collection, preparation, and analysis
Blood samples were collected in serum microtainers using standard blood collection during the insertion of a venous cannula. This time point was labeled t = 0. After 48 to 72 h of treatment with antibiotics a second blood sample was obtained using capillary collection. This time point was labeled t = 48 to 72. CRP and hematological parameters were determined routinely at the clinical laboratory of the Academic Hospital Paramaribo. Blood was allowed to clot at room temperature and serum was separated by centrifugation at 2,300×g for 8 min, the serum was harvested and residual sample was stored at −80°C until further analysis. Frozen samples were transported on dry ice from Suriname to the Netherlands. For analysis, the samples were thawed on ice and immediately analyzed. Measurement of levels of Ang-1 and Ang-2 was performed using the Human Luminex Screening Assay LXSAH (R&D Systems, Minneapolis, Minn) according to the manufacturer's instructions. We determined interassay coefficients of variation (CV) and accepted a maximum of 20%. Median inter-assay CV ranged from 7.3% to 10.5% for Ang-1 and 4.6% to 10.3% for Ang-2, respectively.
Statistical analysis
Categorical variables were presented as numbers and percentages with 95% CI and compared with chi-square. Continuous variables were presented as median and interquartile range (IQR) Due to the nonparametric nature of the data a Mann–Whitney or Kruskal–Wallis test with Dunn correction for multiple comparisons was used for the analysis of continuous variables. Spearman rho was used to assess bivariable associations between CRP levels and Ang-1 and Ang-2 levels, respectively. P values < 0.05 were considered statistically significant. All the analyses were performed using Prism version 7.0a (Graphpad Software Inc, San Diego, Calif).
RESULTS
Demographics
Of 101 eligible newborns eight newborns were excluded for incomplete clinical information and two for insufficient serum. For the 91 included newborns demographics are given in Table 1. Birth weight, age at presentation, Apgar score, and clinical course at t = 48 to 72 h were distributed unevenly among the three groups. Six (8.5%; 95% CI 3.9–17.2) newborns receiving antibiotic treatment had a positive blood culture (all gram-negative bacteria, Klebsiella pneumoniae (n = 2), Enterobacter cloacae (n = 2) and Escherichia coli (n = 2)). Newborns with EOS received respiratory and circulatory support more often than controls (P < 0.001). A total of five newborns with EOS died. White blood cell, neutrophil and trombocyte counts, and CRP levels were not different between groups (Table 2).
Table 1.
Descriptive statistics of the study group (n = 91)
| Early onset sepsis | ||||
| Controls (n = 20) | Blood culture negative (n = 65) | Blood culture positive (n = 6) | P value | |
| Pregnancy, n (%) | ||||
| Complications* | 3 (15) | 16 (25) | 1 (17) | 0.63 |
| Chorioamnionitis† | 0 | 18 (28) | 0 | |
| Mode of delivery, n (%) | ||||
| Vaginal | 12 (60) | 46 (75) | 4 (67) | 0.54 |
| Caesarean | 8 (40) | 19 (25) | 2 (33) | |
| Sex, n (%) | ||||
| Male | 9 (45) | 29 (45) | 5 (83) | 0.19 |
| Female | 11 (55) | 36 (55) | 1 (17) | |
| Ethnicity, n (%) | ||||
| Maroon and Creole | 12 (60) | 44 (68) | 4 (67) | |
| Hindo-Surinamese | 3 (15) | 14 (21) | 1 (17) | 0.61 |
| Other‡ | 5 (25) | 7 (11) | 1 (17) | |
| Gestational age, n (%) (weeks) | ||||
| 34–37 | 1 (5) | 22 (34) | 0 | |
| 37–40 | 14 (70) | 30 (46) | 4 (67) | 0.06 |
| ≥40 | 5 (25) | 13 (20) | 2 (33) | |
| Apgar score, n (%) | ||||
| <5 | 0 | 5 (8) | 2 (33) | 0.03 |
| Birth weight, median (IQR) (g) | 3,130 (700) | 2,840 (835) | 3,500 (906) | 0.02 |
| Age at presentation, n (%) (h) | ||||
| <24 | 4 (20) | 43 (66) | 2 (33) | |
| 24–48 | 7 (35) | 13 (20) | 1 (17) | <0.01 |
| 48–72 | 9 (45) | 9 (14) | 3 (50) | |
| Clinical course (at 48–72 h), n (%) | ||||
| CPAP | 0 | 9 (14) | 0 | |
| Mechanical ventilation | 0 | 7 (11) | 2 (33) | |
| Cardiotonics | 0 | 5 (8) | 1 (17) | <0.001 |
| Mortality | 0 | 3 (5) | 2 (33) | |
*Presence of pregnancy-induced hypertension, preeclampsia, or diabetes mellitus.
†Defined as intrapartum fever or administration of antibiotics.
‡Includes: Javanese, Chinese, Caucasian, and Amerindian.
CPAP indicates continuous positive airway pressure; IQR, interquartile range; N/A, not applicable.
Table 2.
Infection biomarkers in baseline controls and newborns with suspected and blood culture positive early onset sepsis
| Early onset sepsis | ||||||
| Time point | n (%) | Controls | Blood culture negative | Blood culture positive | P value* | |
| White blood cells (×109/L) | t = 0 | 88 (97) | 15.3 (8.2) | 17.5 (9.7) | 21.9 (82.4) | 0.68 |
| Neutrophils (×109/L) | t = 0 | 72 (79) | 7.1 (8.5) | 9.2 (7.9) | 10.2 (34.1) | 0.57 |
| Platelets (×109/L) | t = 0 | 83 (91) | 235 (82) | 239 (60) | 74 (164.5) | 0.07 |
| C-reactive protein (mg/dL) | t = 0t = 48–72 hDelta | 75 (82)44 (48)44 (48) | <0.5 (0)N/AN/A | <0.5 (0.7)0.7 (1.8)0.1 (1.3) | 0.7 (4.8)1.4 (16.3)1.7 (3.4) | 0.340.810.46 |
| Angiopoietin-1 (ng/mL) | t = 0t = 48–72 h | 91 (100)49 (54) | 77.4 (65.2)68.9 (44.5) | 82.2 (45.7)73.6 (67.3) | 28.3 (28.0)1.3 (16.1) | <0.010.02 |
| Angiopoietin-2 (ng/mL) | t = 0t = 48–72 h | 91 (100)49 (54) | 10.2 (1.9)9.9 (1.5) | 11.2 (6.9)11.8 (4.7) | 21.1 (13.3)19.0 (18.9) | <0.010.07 |
Data presented as median (IQR).
*Data analyzed with a Kruskal-Wallis test between all groups or with a Mann-Whitney test between blood culture negative and positive groups.
EOS indicates early onset sepsis; IQR, interquartile range; N/A, not applicable.
Levels of angiopoietins
At t = 0, median levels of Ang-1 were significantly lower in blood culture positive EOS (28.3 (28.0) ng/mL) versus controls (77.4 (65.2) ng/mL), P < 0.01 (Table 2) (Fig. 1A). Median Ang-2 levels were higher in blood culture EOS (21.1 (13.3) ng/mL) versus controls (10.2 (1.9) ng/mL), P < 0.001, respectively (Fig. 1B). The Ang-2/Ang-1 protein ratio was higher in blood culture positive EOS (median (IQR) 0.77 (0.77) versus controls (median (IQR) 0.13 (0.13) (P < 0.01) (Fig. 1C)). There was no difference in median levels of Ang-1, Ang-2, and Ang-2/Ang-1 protein ratio between blood culture negative EOS and controls.
Fig. 1.
Serum levels of Angiopoietin-1 and Angiopoietin-2 of controls and newborns with blood culture negative and positive early onset sepsis (EOS).
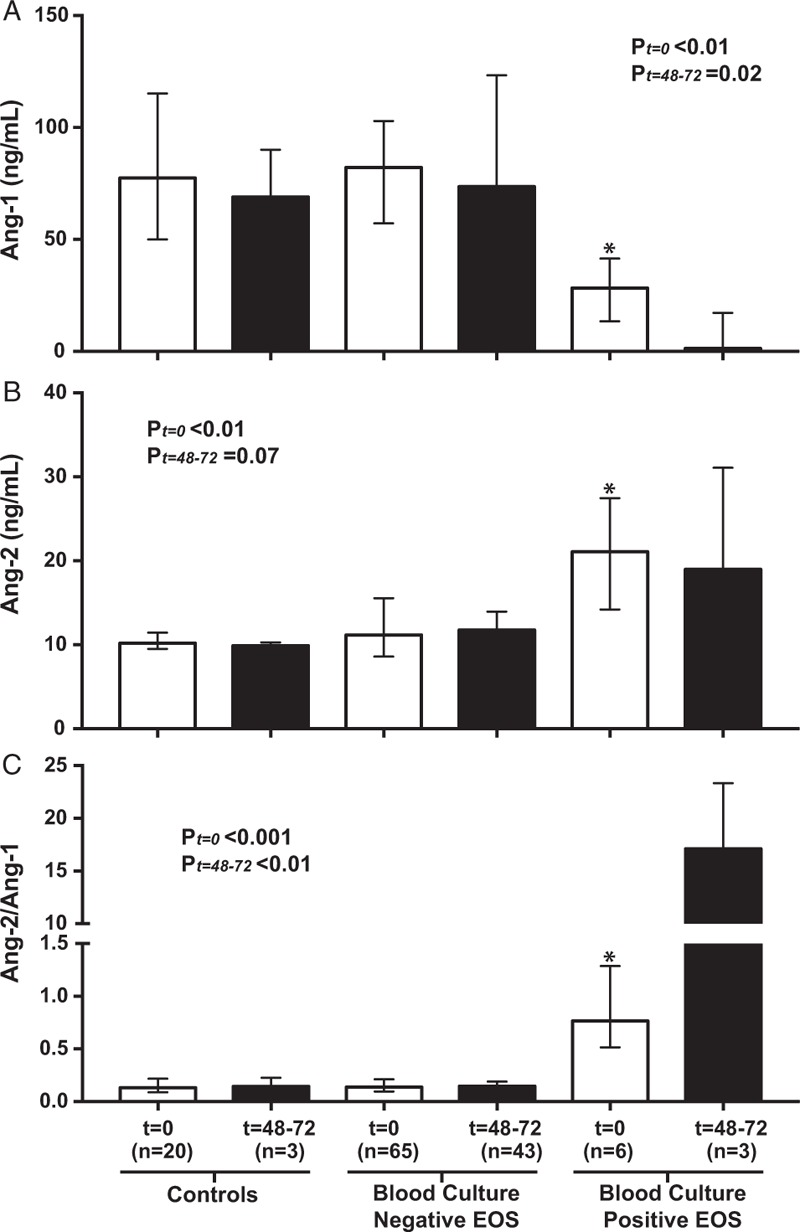
A, Angiopoietin-1 (Ang-1). B, Angiopoietin-2 (Ang-2). C, Ang-2/Ang-1protein ratio. Data represent levels in serum sampled at t = 0 (white bars) and t = 48 to 72 h (black bars) and are analyzed with a Kruskal–Wallis test with Dunn correction for multiple comparisons between all groups at t = 0 (Pt=0) and at t = 48–72 (Pt=48–72). ∗P < 0.05 when groups are separately compared with controls. Bars represent median values and error bars interquartile range.
At t = 48 to 72 h, median Ang-1 levels had decreased 21-fold in blood culture positive EOS from levels at t = 0 (P = 0.10), while median Ang-2 levels remained high (P = 0.99) (Table 2) (Fig. 1, A and B). Median levels of Ang-1, Ang-2, and Ang-2/Ang-1 protein ratio were not different when comparing blood culture positive or blood culture negative EOS with controls.
Levels of Ang-1 and Ang-2 were tested for dependency on timing of first blood draw (t = 0) after birth. For controls and EOS (blood culture negative plus blood culture positive EOS) median levels at t = 0 were not different between newborns if t = 0 was before 24 h or between 24 to 72 h after birth (Fig. 2, A and B).
Fig. 2.
Serum levels of Angiopoietin-1 and Angiopoietin-2 at inclusion in newborns included before and after the first 24 h of life.
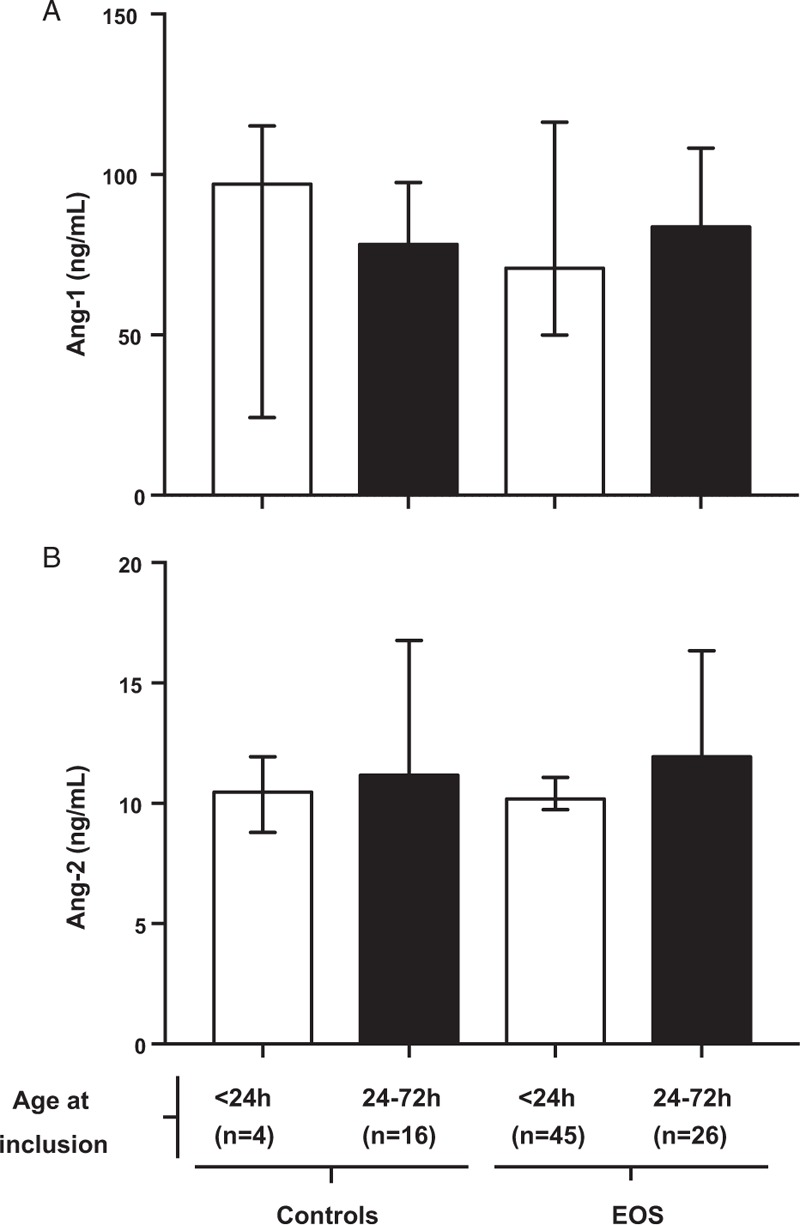
A, Angiopoietin-1 (Ang-1). B, Angiopoietin-2 (Ang-2). Data represent pooled levels at t = 0 from newborns considered uninfected (controls) and from newborns considered infected (blood culture negative and positive EOS), included before 24 h (white bars) versus 24 to 72 h (black bars) after birth. Data was analyzed with a Mann–Whitney test. Bars represent median values and error bars interquartile range.
Because CRP levels at t = 48 to 72 h increased from levels at t = 0 in blood culture negative and positive EOS (Table 2), correlation of Ang-1 and Ang-2 with CRP was assessed among 44 newborns with blood culture negative (n = 42) and positive (n = 2) EOS in whom all data had been recorded (Fig. 3, A and B). Lower median Ang-1 (rho −0.46; 95% CI −0.67 to −0.19), but not higher Ang-2, correlated with higher CRP at t = 48 to 72 h.
Fig. 3.
Correlations of serum levels of Angiopoietin-1 and Angiopoietin-2 with serum levels of C-reactive protein in newborns with blood culture negative or positive early onset sepsis (EOS).
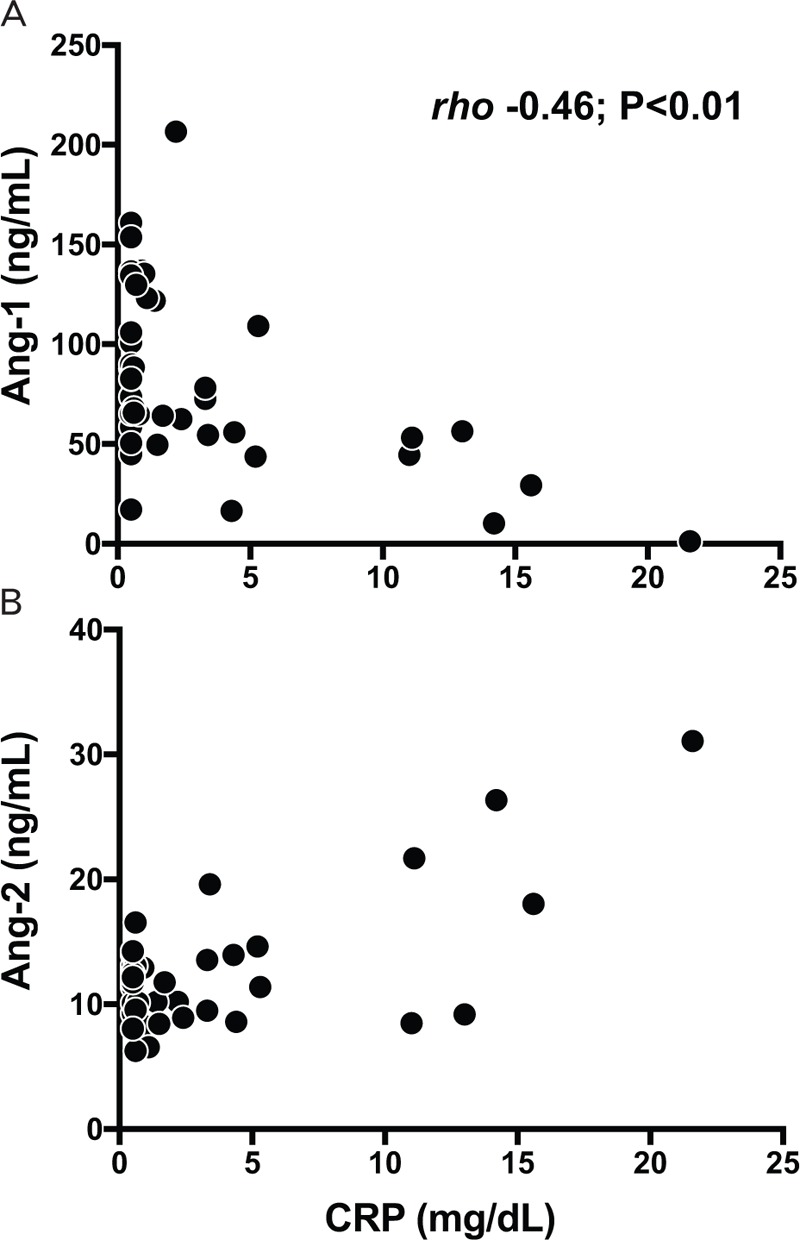
Correlations of CRP with (A) Angiopoietin-1 (Ang-1); (B) Angiopoietin-2 (Ang-2). Data represent levels of Ang-1, Ang-2, and CRP in serum sampled at t = 48 to 72 h from newborns (in whom data on levels was universally available) with blood culture negative (n = 42) and positive (n = 2) EOS. Spearman rho was used to assess correlations. Correlation (rho) is given when significant. CRP indicates C-reactive protein.
DISCUSSION
In this study, we investigated the serum levels of Ang-1 and Ang-2 to better understand the vascular pathophysiology in near-term and term Surinamese newborns treated for EOS. Lower levels of Ang-1, higher Ang-2, and a higher Ang-2/Ang-1 protein ratio in serum of newborns were associated with blood culture positive EOS at the start of antibiotic treatment. Levels of Ang-1 further decreased over time in newborns with blood culture positive EOS and correlated negatively with higher levels of CRP. These results indicate a role for the Angiopoietins in vascular inflammation during EOS in Suriname. An estimated 5% to 10% of total EOS data is from non-Western countries such as Suriname, while there is strong indication that over 90% of global deaths due to EOS occur in these settings (2, 19, 20). Thus, our data add critical basic and clinical knowledge on the true global impact of EOS.
Our results of Ang-1 levels are in line with other studies that reported reduced Ang-1 levels in children associated with septic shock and death (21, 22). The mechanism for low Ang-1 remains poorly understood. While Ang-1 levels are low, the levels of its soluble ligand sTie-2 are higher in the blood of septic patients. Soluble Tie 2 may act as a decoy receptor binding Ang-1 with high affinity, thereby decreasing its circulating levels. On the other hand, increasing Ang-1 levels, thereby increasing endothelial Tie-2 receptor phosphorylation, may help to inhibit vascular inflammation and leakage. In a clinically relevant murine model, intravenous recombinant Ang-1 treatment was sufficient to improve sepsis-associated organ dysfunctions and survival time, most likely by preserving endothelial barrier function (23).
Higher levels of Ang-2 may be reflective of vascular inflammation and vascular leakage. Intravenous lipopolysaccharide injection in human volunteers, adult human sepsis, and secondary infection in critically ill patients causes higher levels of circulating Ang-2 and higher Ang-2/Ang-1 ratios (24–28). As intracellular Tie-2 phosphorylation cannot be assessed in patients, an increased Ang-2/Ang-1 ratio might be predictive for reduced endothelial Tie-2 receptor phosphorylation with subsequent vascular inflammation and leakage.
EOS can occur following colonization of the newborn with bacterial pathogens following intrauterine infection or in the birth canal during labor (4). Two studies found higher maternal and amniotic fluid levels of Ang-2 in cases of intrauterine infection in at term and preterm birth (29, 30). To our knowledge, placental Ang-2 crossing has not been described. The presence of intrauterine infection may result in EOS and cause subsequent suppression of neonatal levels of Ang-1 and release of neonatal Ang-2 from endothelial cells. Our finding that levels of Ang-1 and Ang-2 are similar between infected newborns included directly after birth and after 24 h supports this hypothesis.
A remarkable finding in our study was that levels of Ang-1 in newborns were up to a 10-fold higher, specifically in healthy newborns and those with blood culture negative EOS, than in children or adults in earlier studies (13–17, 21, 22). Placental levels of Ang-1 and Ang-2 are high during pregnancy and then quickly drop after birth (31, 32). Only one earlier study compared both antepartum and postcaesarean maternal samples with neonatal umbilical cord blood samples (32). Ang-1 concentrations were significantly higher in umbilical samples, suggesting separate Angiopoietin regulation in the newborn. Animal models of pregnancy may help elucidate the exact dynamics of Angiopoietins in newborns (33). These animal models may also be instrumental in detecting endothelial Tie-2 receptor phosphorylation in different microvascular beds.
From a clinical perspective, our findings indicate that serial measurement of Angiopoietins may predict or exclude bacteremia in newborns before blood culture results are known. High serial Ang-1 and low serial Ang2/Ang-1 ratio may be extra arguments to discontinue antibiotics, alongside serial measurement of CRP. A known limitation to CRP is its slow synthesis limiting its utility in early prediction of EOS. To overcome this issue, inflammatory mediators that precede CRP synthesis, such as interleukin (IL)-1ß, IL-6, IL-8, and tumor-necrosis factor (TNF)-α, have been of interest in EOS research (34–36). These mediators have short half-lives, which limits their clinical use and establishment of appropriate cut-off values. In our study, levels of Ang-1 remained high in healthy and low in the sickest newborns at re-evaluation 48 to 72 h after the start of antibiotics, indicating persistent association with severity of disease over time and clinical utility. Additionally, TNF-α has been shown to correlate with Ang-2 levels in adult patients with sepsis (24, 37). For these reasons it would be interesting to evaluate temporal relations of the Angiopoietins with a panel of inflammatory mediators, such as TNF-α, Il-6, and IL-1ß in EOS.
Our study has several limitations. First, our sample size was relatively small to assess relevance of the Angiopoietins as clinical biomarkers and results may have been confounded by birth weight and asphyxia, which were distributed unevenly among the groups. Second, as levels of the Angiopoietins were determined with a Luminex Screening Assay we were unable to compare levels with results from other studies measured with ELISA (21, 28), and small sample volumes acquired in neonates precluded assessment of other inflammatory mediators. Future studies will focus on eliminating these limitations to enable us to validate the current observations in newborns in Surinamese newborns.
In summary, our data show changes in the ligands of the Angiopoietin/Tie2 endothelial receptor system Ang-1 and Ang-2 in EOS and support the hypothesis that increased vascular inflammation and increased vascular leakage leads to microvascular dysfunction in the pathophysiology of EOS. The potential impact of intra-uterine-infection deserves attention in future investigations to further elucidate dynamics of Angiopoietins in newborns with and without EOS.
Acknowledgments
The authors acknowledge the efforts of all employees of the Clinical Laboratory of the Academic Hospital Paramaribo and the Central Laboratory of Suriname, Paramaribo, Suriname, for assistance with sample storage, handling, and transport.
Footnotes
REFERENCES
- 1.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016; 315 8:801–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schrag SJ, Farley MM, Petit S, Reingold A, Weston EJ, Pondo T, Hudson Jain J, Lynfield R. Epidemiology of invasive early-onset neonatal sepsis, 2005 to 2014. Pediatrics 2016; 138:pii: e20162013. [DOI] [PubMed] [Google Scholar]
- 3.van Herk W, Stocker M, van Rossum AM. Recognising early onset neonatal sepsis: an essential step in appropriate antimicrobial use. J Infect 2016; 72:S77–S82. [DOI] [PubMed] [Google Scholar]
- 4.Simonson KA, Anderson-Berry AL, Delair SF, Davies HD. Early-onset neonatal sepsis. Clin Microbiol Rev 2014; 27 1:21–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hofer N, Zacharias E, Müller W, Resch B. An update on the use of C-reactive protein in early-onset neonatal sepsis: current insights and new tasks. Neonatology 2012; 102:25–36. [DOI] [PubMed] [Google Scholar]
- 6.Aird WC. The role of the endothelium in severe sepsis and multiple organ dysfunction syndrome. Blood 2003; 101 10:3765–3777. [DOI] [PubMed] [Google Scholar]
- 7.van Meurs M, Kümpers P, Ligtenberg JJ, Meertens JH, Molema G, Zijlstra JG. Bench-to-bedside review: angiopoietin signalling in critical illness—a future target? Crit Care 2009; 13 2:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parikh SM. Dysregulation of the angiopoietin-Tie-2 axis in sepsis and ARDS. Virulence 2013; 4 6:517–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kurniati NF, Jongman RM, vom Hagen F, Spokes KC, Moser J, Regan ER, Krenning G, Moonen JR, Harmsen MC, Struys MM, et al. The flow dependency of Tie2 expression in endotoxemia. Intensive Care Med 2013; 39 7:1262–1271. [DOI] [PubMed] [Google Scholar]
- 10.Kim M, Allen B, Korhonen EA. Opposing actions of angiopoietin-2 on Tie-2 signaling and FOXO1 activation. J Clin Invest 2016; 126 9:3511–3525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yuan HT, Khankin EV, Karumanchi SA, Parikh SM. Angiopoietin 2 is a partial agonist/antagonist of Tie2 signaling in the endothelium. Mol Cell Biol 2009; 29 8:2011–2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van der Heijden M, van Nieuw Amerongen GP, van Hinsbergh VW, Groeneveld AB. The interaction of soluble Tie2 with angiopoietins and pulmonary vascular permeability in septic and nonseptic critically ill patients. Shock 2010; 33 3:263–268. [DOI] [PubMed] [Google Scholar]
- 13.Giuliano JS, Jr, Tran K, Li FY, Shabanova V, Tala JA, Bhandari V. The temporal kinetics of circulating angiopoietin levels in children with sepsis. Pediatr Crit Care Med 2014; 15 1:e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang K, Bhandari V, Giuliano JS., Jr Angiopoietin-1, angiopoietin-2 and bicarbonate as diagnostic biomarkers in children with severe sepsis. PLoS One 2014; 9 9:e108461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lymperopoulou K, Velissaris D, Kotsaki A, Antypa E, Georgiadou S, Tsaganos T, Koulenti D, Paggalou E, Damoraki G, Karagiannidis N, et al. Angiopoietin-2 associations with the underlying infection and sepsis severity. Cytokine 2015; 73 1:163–168. [DOI] [PubMed] [Google Scholar]
- 16.Ricciuto DR, dos Santos CC, Hawkes M, Toltl LJ, Conroy AL, Rajwans N, Lafferty EI, Cook DJ, Fox-Robichaud A, Kahnamoui K, et al. Angiopoietin-1 and angiopoietin-2 as clinically informative prognostic biomarkers of morbidity and mortality in severe sepsis. Crit Care Med 2011; 39 4:702–710. [DOI] [PubMed] [Google Scholar]
- 17.Fang Y, Li C, Shao R, Yu H, Zhang Q, Zhao L. Prognostic significance of the angiopoietin-2/angiopoietin-1 and angiopoietin-1/Tie-2 ratios for early sepsis in an emergency department. Crit Care 2015; 14 19:367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mussap M, Cibecchini F, Noto A, Fanos V. In search of biomarkers for diagnosing and managing neonatal sepsis: the role of angiopoietins. J Matern Fetal Neonatal Med 2013; 26 2:24–26. [DOI] [PubMed] [Google Scholar]
- 19.Edmond KM, Kortsalioudaki C, Scott S, Schrag SJ, Zaidi AK, Cousens S, Heath PT. Group B streptococcal disease in infants aged younger than 3 months: systematic review and meta-analysis. Lancet 2013; 379 9815:547–556. [DOI] [PubMed] [Google Scholar]
- 20.Lawn JE, Cousens S, Zupan J. Lancet Neonatal Survival Steering Team. 4 million neonatal deaths: when? Where? Why? Lancet 2005; 365 9462:891–900. [DOI] [PubMed] [Google Scholar]
- 21.Mankhambo LA, Banda DL, Jeffers G, White SA, Balmer P, Nkhoma S, Phiri H, Molyneux EM, Hart CA, Molyneux ME, et al. Study Group IPD. The role of angiogenic factors in predicting clinical outcome in severe bacterial infection in Malawian children. Crit Care 2010; 14 3:R91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guiliano JS, Lahni PM, Harmon K, Wong HR, Doughty LA, Carcillo JA, Zingarelli B, Sukhatme VP, Parikh SM, Wheeler DS. Admission angiopoeitin levels in children with septic shock. Shock 2007; 28 6:650–654. [PMC free article] [PubMed] [Google Scholar]
- 23.David S, Park JK, Meurs MV, Zijlstra JG, Koenecke C, Schrimpf C, Shushakova N, Gueler F, Haller H, Kümpers P. Acute administration of recombinant Angiopoietin-1 ameliorates multiple-organ dysfunction syndrome and improves survival in murine sepsis. Cytokine 2011; 55 2:251–259. [DOI] [PubMed] [Google Scholar]
- 24.Fiedler U, Reiss Y, Scharpfenecker M, Grunow V, Koidl S, Thurston G, Gale NW, Witzenrath M, Rosseau S, Suttorp N, et al. Angiopoietin-2 sensitizes endothelial cells to TNF-alpha and has a crucial role in the induction of inflammation. Nat Med 2006; 12 2:235–239. [DOI] [PubMed] [Google Scholar]
- 25.Parikh SM, Mammoto T, Schultz A, Yuan HT, Christiani D, Karumanchi SA, Sukhatme VP. Excess circulating angiopoietin-2 may contribute to pulmonary vascular leak in sepsis in humans. PLoS Med 2006; 3 3:e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kümpers P, van Meurs M, David S, Molema G, Bijzet J, Lukasz A, Biertz F, Haller H, Zijlstra JG. Time course of angiopoietin-2 release during experimental human endotoxemia and sepsis. Crit Care 2009; 13 3:R64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.David S, Mukherjee A, Ghosh CC, Yano M, Khankin EV, Wenger JB, Karumanchi SA, Shapiro NI, Parikh SM. Angiopoietin-2 may contribute to multiple organ dysfunction and death in sepsis. Crit Care Med 2012; 40 11:3034–3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Van Vught LA, Wiewel MA, Hoogendijk AJ, Frencken JF, Scicluna BP, Klein Klouwenberg PM, Zwinderman AH, Lutter R, Horn J, Schultz MJ, et al. The host response in sepsis patients developing intensive care unit-acquired secondary infections. Am J Respir Crit Care Med 2017; 196 4:458–470. [DOI] [PubMed] [Google Scholar]
- 29.Pacora P, Romero R, Chaiworapongsa T, Kusanovic JP, Erez O, Vaisbuch E, Mazaki-Tovi S, Gotsch F, Jai Kim C, Than NG, et al. Amniotic fluid angiopoietin-2 in term and preterm parturition, and intra-amniotic infection/inflammation. J Perinat Med 2009; 37 5:503–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buhimschi CS, Bhandari V, Dulay AT, Thung S, Razeq SS, Rosenberg V, Han CS, Ali UA, Zambrano E, Zhao G, et al. Amniotic fluid angiopoietin-1, angiopoietin-2, and soluble receptor tunica interna endothelial cell kinase-2 levels and regulation in normal pregnancy and intraamniotic inflammation-induced preterm birth. J Clin Endocrinol Metab 2010; 95 7:3428–3436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kappou D, Sifakis S, Konstantinidou A, Papantoniou N, Spandidos DA. Role of the angiopoietin/tie system in pregnancy. Exp Ther Med 2015; 9 4:1091–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Keikkala E, Hytinantti T, Wathén KA, Andersson S, Vuorela P. Significant decrease in maternal serum concentrations of angiopoietin-1 and -2 after delivery. Acta Obstet Gynecol Scand 2012; 91 8:917–922. [DOI] [PubMed] [Google Scholar]
- 33.Reynolds LP, Borowicz PP, Vonnahme KA, Johnson ML, Grazul-Bilska AT, Wallace JM, Caton JS, Redmer DA. Animal models of placental angiogenesis. Placenta 2005; 26 10:689–708. [DOI] [PubMed] [Google Scholar]
- 34.Machado JR, Soave DF, da Silva MV, de Menezes LB, Etchebehere RM, Monteiro ML, dos Reis MA, Corrêa RR, Celes MR. Neonatal sepsis and inflammatory mediators. Mediators Inflamm 2014; 2014:269681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khaertynov KS, Boichuk SV, Khaiboullina SF, Anokhin VA, Andreeva AA, Lombardi VC, Satrutdinov MA, Agafonova EA, Rizvanov AA. Comparative assessment of cytokine pattern in early and late onset of neonatal sepsis. J Immunol Res 2017; 2017:8601063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fattah MA, Omer AF, Asaif S, Manlulu R, Karar T, Ahmed A, Aljada A, Saleh AM, Qureshi S, Nasr A. Utility of cytokine, adhesion molecule and acute phase proteins in early diagnosis of neonatal sepsis. J Nat Sci Biol Med 2017; 8 1:32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Benest AV, Kruse K, Savant S, Thomas M, Laib AM, Loos EK, Fiedler U, Augustin HG. Angiopoietin-2 is critical for cytokine-induced vascular leakage. PLoS One 2013; 8 8:e70459. [DOI] [PMC free article] [PubMed] [Google Scholar]


