Abstract
Objective
To determine the prevalence of comorbid mild traumatic brain injury (mTBI), PTSD, and depression, termed the deployment trauma phenotype (DTP), and its constituent diagnoses' impact on unemployment status in a national cohort of veterans.
Setting
Retrospective analysis of the comprehensive TBI evaluation, a VA-wide protocol for assessing TBI, employment status, and psychiatric impressions.
Participants
The final dataset consisted of 48,821 veterans.
Main Outcomes and Measures
Frequency of mTBI, PTSD, and depression in isolation and combinations and their association with unemployment status.
Results
Age- and education- adjusted risk ratios showed that the mTBI-only group was the least likely to be unemployed, RR = 0.65 [0.59, 0.71]. By contrast, the greatest likelihood of unemployment was associated with membership in the DTP group, RR =1.45 [1.36, 1.56] and the comorbid PTSD and Depression group, RR = 1.39 [1.27, 1.52]. Furthermore, the DTP was nearly three times more prevalent (16.4%) in this sample compared to comorbid PTSD and Depression (5.7%) indicating that the DTP conveys risk for unemployment to a significantly greater number of individuals.
Conclusions and Relevance
The co-morbid and interactive conditions of PTSD, depression, and mTBI, rather than mTBI in isolation, were linked to significant risk for unemployment in this veteran cohort. These findings suggest that multi-faceted assessments and interventions to improve post-deployment reintegration are needed.
Introduction
Military personnel from Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OEF), and Operation New Dawn (OND) face significant challenges re-entering civilian life after structured military careers. The functional consequences of psychiatric conditions co-occurring with mild traumatic brain injury (mTBI) among active military personnel, veterans, and, in turn, their family members and society are becoming increasingly recognized. Recent investigations examining the prevalence and types of community reintegration problems among returning veterans identified difficulties in social functioning, including family and marital discord, as well as unemployment and underemployment1-5.
Psychiatric disorders comorbid with history of military-related mTBI are believed to drive this interference with successful reintegration. Mild TBI has emerged as a common deployment related conditions 7 and in national news, mTBI is popularly identified as the “signature wound” of the veterans who have served during OEF/OIF/OND. However, data have emerged since the publication of the seminal “Invisible Wounds” Rand Report6 suggesting that a more complex amalgam of interactive, co-morbid physical and psychiatric conditions may underlie the functional deficits experienced in this cohort, rather than mTBI alone. Hoge7, while affirming the alarming prevalence of mTBI sounded by the Rand report, warned that the source of distress in these veterans is due to the co-occurrence of posttraumatic stress disorder (PTSD) and depression, rather than mTBI alone. Therefore, mTBI on its own may not lead to poor outcomes, but instead, it may serve as a marker for the occurrence of other deployment-related comorbidities that in combination are the likely cause of reintegration difficulty8.
Our previous work supports the hypothesis that comorbid conditions, in addition to mTBI, account for reintegration difficulties. 9 Employing a well-characterized sample of OEF/OIF/OND veterans recruited at the Translational Research Center for TBI and Stress Disorders (TRACTS), a Veterans Affairs (VA) TBI National Network Research Center, we identified empirically-derived clusters of diagnoses and found that most veterans were burdened by multiple psychiatric and mTBI diagnoses that could be grouped into four distinct factors. One such factor, consisting of co-occurring PTSD, depression and military mTBI, which we termed the Deployment Trauma Phenotype (DTP), characterized 16.9% of the sample and was strongly and uniquely linked to disability, as measured by the World Health Organization's Disability Assessment Schedule (WHODAS-2). The overall level of disability in the DTP group was higher than 80% of that in the general international public10. Individuals with the DTP not only had significantly higher levels of reported disability relative to individuals who were burdened by the diagnoses comprising any of the other three factors, but they also accounted for approximately 70% of the sample who were determined to be “substantially disabled.”9 The DTP was associated with the most severe levels of disability relative to any other psychiatric condition or mTBI diagnosis, either in isolation or in any other combination of prevalent diagnoses in the sample.
The clinical characterization that participants undergo as part of their participation in TRACTS is unique because psychiatric conditions and head injuries are diagnosed using extensive semi-structured clinical interviews conducted by doctoral level psychologists and confirmed via consensus9. A significant limitation of our previous findings, the data were based on a relatively small convenience sample of volunteers drawn from the Boston Metropolitan area. The question therefore remains: does the DTP occur at similar rates within the general population of veterans currently under the care of the Department of Veterans Affairs and, if so, does it confer the same liability for functional disability, indexed by unemployment status, in a larger epidemiological sample?
Though veterans burdened with the DTP reported the most disability across each of the six domains assessed by the WHODAS-2, it does not tell us directly about the impact on an individual's employment status, which is potentially one of the most important markers of disability for younger individuals. Employment status has been shown to be broadly predictive of socio-economic stability and of outcomes in a variety of social domains12. Further, employment status is a central aspect of reintegration to civilian life13, and OEF/OIF/OND veterans have greater rates of unemployment relative to their civilian counterparts14. Psychiatric conditions in the general population are associated with three to five times higher rates of unemployment15 and a recent epidemiological study demonstrated that suspected psychiatric conditions were significantly associated with unemployment status in this Veteran population16. Although most OEF/OIF/OND Veterans are relatively young and at a developmental stage with emphasis on careers and professional achievement, too many are unemployed with psychiatric diagnoses that could further interfere with engagement in the workforce17.
The goal of the current study was to examine the prevalence of the DTP and its constituent diagnoses in a large national sample of OEF/OIF veterans, and to explore the relationship of these mental health conditions and mTBI history to unemployment status. Specifically, these data are derived from a sample of 86,140 OEF/OIF veterans who had been evaluated for possible history of military service-related TBI at the VA healthcare facilities. The VA mandated and nationally administered Comprehensive TBI Evaluation (CTBIE) collects detailed information about exposure to potential concussive events and their sequela for the purpose of assessing the presence or absence of a TBI. Additionally, the CTBIE assesses the presence of other co-occurring psychiatric conditions, employment status, and persisting post concussive symptoms (via the Neurobehavioral Symptom Inventory, NSI). Importantly, recent research has identified NSI response patterns that can be used to identify individuals who may not have represented their current functioning accurately18,19. The assessment of response validity is rarely done in population-based studies of mTBI, but is important because of the evidence of increased levels of non-credible symptom reporting among some veterans undergoing the CTBIE18,20. In the current study, we excluded all individuals whose pattern of NSI responding on the items comprising the proposed validity subscale exceeded criterion values suggested to be indicative of non-credible representations of their current symptom severity.
This is the first population-based study to examine the interactive impact of comorbid deployment-related conditions upon unemployment status. It is also the first epidemiological study to exclude individuals with non-credible responding patterns, increasing the reliability of the findings. We hypothesized that individuals with the DTP would demonstrate greater levels of unemployment relative to its constituent diagnoses of depression, PTSD, or mTBI, occurring in isolation or in any of the possible two-way combinations of these conditions. Since unemployment status within this cohort is impacted by age16,21 we also examined the interaction of age and diagnosis configuration with regard to the outcome measure of unemployment.
Methods
Design
This study was a retrospective cross-sectional analysis of data from the VA comprehensive TBI evaluation (CTBIE) administered between the 4th fiscal quarter of 2009 through the 4th quarter of 2013. The VA Boston Healthcare System's Committee for Human Subjects Research approved all procedures.
Data Sources
Beginning in April 2007, the VA mandated TBI screening for all OEF/OIF veterans (later including OND veterans). All individuals who screen positive for possible history of TBI are then referred for the CTBIE22. The CTBIE database was obtained from VA Patient Care Services and initially included records for 86,140 individuals. From the initial sample of 86,140, a total of 37,319 were excluded for a number of reasons. First, 20,083 individuals were excluded because their record lacked complete data for all of the relevant CTBIE and VA/DoD criteria that was needed to judge presence/absence and severity of TBI23. Severity of the TBI was necessary to obtain in order to exclude those with a history of moderate to severe TBI. Second, 673 individuals were excluded because the CTBIE did not indicate if a TBI had occurred. Third, 9,630 were excluded because of inconsistency between the CTBIE and VA/DoD criteria that was required to confirm TBI severity. Finally, 9 individuals were excluded because their record did not contain NSI data (necessary because we used the Validity-10 scale from the NSI to exclude individuals with non-credible symptom reporting). Lastly, 7,194 individuals were excluded because their data on the Validity-10 scale suggested that their responses were not a valid representation of their symptoms. This resulted in a final analytic dataset of 48,821 (see Figure 1). Within that group, an additional 1,058 veterans were missing employment status data. The final data set (n=48,821) and those excluded from the study for incomplete CTBIE data (n=20,083) were comparable in terms of age, gender, education, NSI symptom severity, and prevalence of PTSD and Depression. Comparison of the clinical characteristics and demographics between the final data set and those who failed the NSI Validity-10 scale revealed that the two groups are comparable to each other in terms of demographics, though the non-credible symptom reporting group had significantly higher NSI symptom severity scores. These higher NSI scores were not surprising as the Validity-10, embedded within the NSI, was developed to identify possible symptom exaggeration. Thus, we would expect inflated NSI total scores observed in the subgroup who failed the Validity-10 measure compared to our final sample. In terms of clinical characteristics, the non-credible symptom reporting group relative to the final sample also had a lower prevalence of mTBI-only diagnoses and a higher prevalence of the DTP. Due to non-credible responding, it was expected that there would be differences in the excluded group relative to the final dataset.
Figure 1.
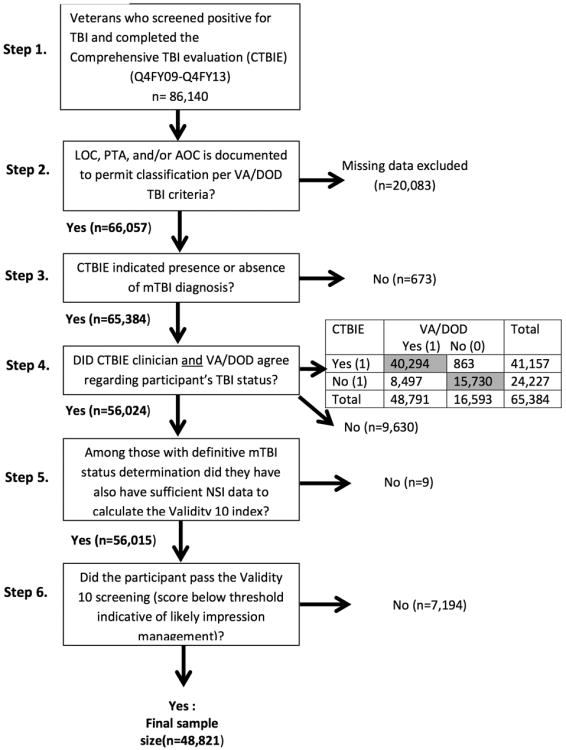
Flow chart of the 6 steps undertaken to arrive at the final sample size. Steps 1-4 ensure the validity and reliability of a TBI diagnosis. Steps 5-6 ruled out individuals with possible poor effort on the assessment (based on an embedded measure of impression management on the NSI-22).
Comprehensive TBI Evaluation (CTBIE)
All OEF/OIF Veterans are screened for a TBI, and individuals who screen positive for possible history of TBI are then referred for the CTBIE22. Importantly, while many individuals screen positive for TBI and are referred for the CTBIE, not all are ultimately determined to have sustained a TBI after this more comprehensive assessment.
The CTBIE is a semi-structured, retrospective clinical interview administered by a clinician trained in TBI assessment. The CTBIE assesses the presence/absence and duration of any symptoms of a TBI (loss of consciousness (LOC), post traumatic amnesia (PTA), and alteration of consciousness (AOC)) that might have occurred in the immediate aftermath an exposure to a blast or a blow/jolt to the head. Ultimately, the CTBIE clinician renders a judgment as to whether a TBI occurred, and whether or not that TBI and/or another psychiatric condition most likely underlies the current reported symptom patterns and functioning.
Given that the CTBIE database includes the raw data regarding duration of LOC, PTA, and AOC, it is also possible to generate an algorithm to apply VA/DoD criteria, and thereby, classify cases directly with regard to the presence/absence of a TBI and its severity.24 Taking a conservative approach to maximize the likelihood of an accurate diagnosis, we required concordance between the results of our algorithm based on VA/DoD criterion and the CTIBE clinician's judgment regarding the presence of mTBI in order to include a case in the present study. Individuals with a history of moderate to severe TBI were excluded (n=3,705).
Clinicians administering the CTBIE are also asked to identify suspected clinically significant psychiatric conditions. There is not a standard method for the assessment of these psychiatric conditions, and these judgments are made based on the clinician's impressions,. The prevalence of PTSD and depression as reported on the CTBIE were examined in this study. The CTBIE also documents veterans' employment status in seven categories: unemployed/not looking for work, unemployed/looking for work, homemaker, volunteer, student, working part-time, and working full-time. The primary outcome measure for this study was the unemployed/not looking (UNL) for work category, which enabled us to examine the association between DTP and the worst of possible employment outcomes (i.e., those who have given up the possibility of current or future employment).
Neurobehavioral Symptom Inventory (NSI)
The 22-item Neurobehavioral Symptom Inventory (NSI-22), a self-report measure of post concussive symptom severity following exposure to a possible TBI, is administered as part of the CTBIE. Importantly, the Validity-10 scale has been developed as a measure of internal validity18,19,25. The Validity-10 scale is comprised of ten NSI items that are infrequently endorsed and/or related to atypical symptom report (e.g., endorsing persisting problems with dizziness, balance, coordination, nausea, vision, hearing, noise sensitivity, taste/smell, decision making, and slow thinking). Scores on the Validity-10 scale range from 0 to 40. A cut score of 22 is used to determine non-credible responding18,19,25. The Validity-10 scale has been validated with the Personality Assessment Inventory, substantiating its use for the detection of invalid responding on the NSI-2226. As depicted in Figure 1 (step 6), 12.8% of the sample was excluded secondary to non-credible responding on the Validity-10 scale.
Statistical Analysis
Eight diagnostic groups were derived by classifying participants by the presence/absence of mTBI, PTSD, and depression. The No diagnoses (reference) group was comprised of individuals with no relevant diagnoses (no mTBI; no PTSD; no Depression). Pateint groups were comprised of individuals with single diagnosis (mTBI only; PTSD only; Depression only), two diagnoses (mTBI and PTSD; mTBI and Depression; PTSD and Depression) and the three way, DTP, diagnoses (mTBI and PTSD and Depression). Descriptive statistics for demographics and clinical characteristics were calculated. One-way ANOVAs were performed to examine possible differences in the selected pairwise comparisons (see Table 1).
Table 1. Veteran Demographic and Clinical Characterization.
| Prevalence | Age (years) Mean (SD) | Gender (% males) | Education Level a (%) | NSI Symptom Severity Mean (SD) b | |
|---|---|---|---|---|---|
| Total | N/A | 33.97 (8.56) | 94.25% | HS: 62.57% | 34.21 (14.26) |
| HS+: 31.87% | |||||
| BA: 5.56% | |||||
| No mTBI, PTSD, or Depression | 18.72% | 34.56 (9.39) | 93.7% | HS: 60.6% | 30.21 (15.57) |
| HS+: 32.4% | |||||
| BA: 7.0% | |||||
| mTBI only | 16.60% | 32.87 (8.30) | 95.0% | HS: 61.0% | 27.91 (13.61) |
| HS+: 32.7% | |||||
| BA: 6.3% | |||||
| PTSD-only | 8.72% | 35.37 (8.74) | 94.0% | HS: 62.7% | 33.04 (13.73) |
| HS+: 31.6% | |||||
| BA: 5.7% | |||||
| Depression- Only | 4.08% | 36.30 (9.74) | 88.1% | HS: 59.2% | 33.95 (13.59) |
| HS+: 33.5% | |||||
| BA: 7.3% | |||||
| mTBI and PTSD | 24.25% | 33.07 (7.66) | 96.6% | HS: 63.9% | 36.52 (12.92) |
| HS+: 31.7% | |||||
| BA: 4.4% | |||||
| mTBI and Depression | 5.57% | 34.11 (8.95) | 92.5% | HS: 63.3% | 35.89 (12.81) |
| HS+: 31.4% | |||||
| BA: 5.3% | |||||
| PTSD and Depression | 5.68% | 35.84 (8.95) | 89.9% | HS: 62.2% | 37.94 (13.33) |
| HS+: 32.6% | |||||
| BA: 5.2% | |||||
| DTP | 16.37% | 33.69 (8.03) | 94.5% | HS: 65.2% | 40.58 (12.32) |
| HS+: 30.3% | |||||
| BA: 4.4% |
HS = High School or GED, HS+ = Some post High School education, BA = BA or more education
The selected pairwise comparisons for the NSI (mTBI-only vs. No mTBI, PTSD or Depression; PTSD and Depression vs. No mTBI, PTSD or Depression; mTBI, PTSD and Depression vs. No mTBI, PTSD or Depression; and mTBI, PTSD and Depression vs. PTSD and Depression) were all significant with p < 0.0001
The primary analyses assessed prevalence of UNL by diagnostic group. Crude, age-and education-, and age-, education-, and NSI- adjusted risk ratios (RR) and 95% confidence intervals (CI) were calculated using log-binomial regression (proc genmod in SAS), with no mTBI, PTSD or Depression as the reference group. The prevalence of unemployment and crude risk ratio (95% CI) were calculated within each age stratum, with no mTBI, PTSD or Depression as the reference group. To examine the statistical difference between risk ratios for specific groups of interest (e.g., DTP vs. PTSD and Depression), we conducted age- and education- adjusted log-binomial regressions for a subset of a priori pairwise comparisons.
Another set of analyses were conducted to examine the impact of NSI symptom severity and diagnostic group upon risk for UNL. NSI symptom severity was collapsed into tertiles. Then the prevalence and crude risk ratio (95% CI) using log-binomial regression were calculated for each tertile with no mTBI, PTSD or Depression as the reference group.
SAS (version 9.3) software was used for all analyses. The statistical tests were two-sided, with a p-value of <.05 used as the cutoff for reporting statistically significant results.
Results
Demographics and Clinical Characterization
Participants had a mean age of 33.97 (8.56 SD), the majority were male (94.3%), married (49.9%), and had at least a high school education or GED (62.6%). Examination of the prevalence of mTBI, PTSD, and depression in isolation or combination revealed that the DTP was the fourth most common constellation of clinical diagnoses, occurring in 16.4% of the sample, following comorbid mTBI and PTSD (24.3%), no diagnoses (18.7%), and mTBI only (16.6%); see Table 1. NSI symptom severity scores were the lowest among individuals with a diagnosis of mTBI only, followed by the No diagnoses group (no mTBI, PTSD, or Depression). In general, with increasing number of psychiatric conditions, NSI symptom severity scores also increased with the DTP demonstrating the most severe NSI symptoms (See Table 1).
Clinical Diagnoses and Employment Status
Unadjusted risk ratios demonstrated that the DTP group and the PTSD and Depression group had the greatest risk for UNL (RR = 1.44 for both) relative to the No diagnoses (reference) group, whereas, the mTBI-only group had the lowest risk of UNL (RR = 0.63) relative to the No diagnoses group. Risk for UNL was relatively comparable amongst all other diagnoses in isolation or combination. In contrast to the crude risk ratios, age- and education-adjusted risk ratios demonstrated that relative to the reference group, the DTP group conveyed the greatest risk for UNL (RR= 1.45), followed by the PTSD and Depression group (RR= 1.39). However, an additional a priori analysis revealed that the adjusted risk ratio comparing the DTP group to the PTSD and Depression group was not statistically significant (RR = 1.05; 95% CI [0.96-1.15]). The mTBI-only group continued to have the lowest risk of UNL (RR= 0.65), and all other diagnostic groupings conveyed similar risk for UNL compared to the reference group (RRs = 0.95-1.08). Risk ratios adjusted for NSI scores, as well as age and education, demonstrated the same pattern of findings. That is, the mTBI group showed the lowest risk for UNL (RR= 0.69) compared to the No diagnoses group and the DTP group (RR= 1.16). Additionally, the PTSD and Depression groups (RR=1.17) demonstrated significantly greater risk for UNL relative to the No diagnoses group.
Since age-adjusted risk ratios revealed differing risk for UNL relative to the crude risk ratios, we examined the DTP and all constituent diagnoses' impact upon UNL rate stratifying by age (see Table 3). Risk ratios indicated that of all groups considered, the DTP group conveyed greatest risk for UNL in the 18-29, 30-39 and 40-49 year-old age cohorts. Comorbid PTSD and Depression conveyed the greatest risk for UNL only among the oldest age cohort (50+). The differences in risk for unemployment, however, did not reach statistical significance when the DTP and comorbid PTSD and Depression groups were compared for each age cohort.
Table 3. Risk ratios of unemployment status within the diagnostic groups stratified by age.
| Diagnostic Group | Age (years) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 18-29 | 30-39 | 40-49 | 50+ | |||||||||
| N | %a | Crude Risk Ratio (95% CI) | N | %a | Crude Risk Ratio (95% CI) | N | %a | Crude Risk Ratio (95% CI) | N | %a | Crude Risk Ratio (95% CI) | |
| mTBI, PTSD and Depression | 2,835 | 16.5 | 1.29 (1.14, 1.46)*** | 3,507 | 20.2 | 1.52 (1.36, 1.69)*** | 1,274 | 24.3 | 1.73 (1.48, 2.03)*** | 362 | 27.6 | 1.37 (1.10, 1.72)** |
| PTSD and Depression | 742 | 16.4 | 1.28 (1.06, 1.55)** | 1,202 | 17.9 | 1.35 (1.16, 1.56)*** | 585 | 22.3 | 1.59 (1.30, 1.94)*** | 243 | 33.6 | 1.67 (1.32, 2.12)*** |
| mTBI and Depression | 1,000 | 12.0 | 0.94 (0.78, 1.14) | 1,080 | 12.4 | 0.93 (0.78, 1.12) | 445 | 13.5 | 0.96 (0.73, 1.25) | 186 | 22.2 | 1.11 (0.81, 1.51) |
| mTBI and PTSD | 4,617 | 11.4 | 0.87 (0.77, 0.98)* | 5,036 | 14.4 | 1.08 (0.97, 1.21) | 1,692 | 17.4 | 1.24 (1.05, 1.46)* | 469 | 21.5 | 1.07 (0.85, 1.35) |
| Depression-only | 554 | 13.6 | 1.07 (0.85, 1.35) | 788 | 13.9 | 1.05 (0.86, 1.27) | 417 | 17.3 | 1.23 (0.96, 1.58) | 230 | 21.2 | 1.06 (0.78, 1.42) |
| PTSD-only | 1,222 | 13.1 | 1.03 (0.86, 1.22) | 1,826 | 12.7 | 0.95 (0.82, 1.11) | 862 | 17.4 | 1.24 (1.02, 1.50)* | 339 | 25.0 | 1.24 (0.98, 1.59) |
| mTBI-only | 3,588 | 7.8 | 0.61 (0.53, 0.71)*** | 2,898 | 8.7 | 0.65 (0.56, 0.76)*** | 1,201 | 8.6 | 0.61 (0.49, 0.77)*** | 405 | 15.1 | 0.75 (0.57, 0.99)* |
| No mTBI, PTSD or Depression | 3,315 | 12.8 | REFERENCEb | 3,492 | 13.3 | REFERENCEb | 1,589 | 14.1 | REFERENCEb | 709 | 20.1 | REFERENCEb |
Percent unemployed/not looking for work.
p < 0.001.
p < .05
p < .01
p < .00
As seen in Table 1, NSI symptom severity differed between diagnostic groups. In order to examine the relative contribution of NSI symptom severity upon UNL, we examined the DTP and all constituent diagnoses stratifying by NSI symptom severity (Table 4). Again the DTP and the comorbid PTSD and Depression groups conveyed the greatest risk for UNL and the mTBI only group conveyed the lowest risk for UNL. It is notable, that risk for UNL in both of these groups was greatest among those who endorsed the least severe NSI symptoms (lowest tertile).
Table 4. Risk ratios of unemployment status within the diagnostic groups stratified by NSI total score tertiles.
| Diagnostic Group | NSI Total Score Tertiles | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Tertile 1 (0-26) | Tertile 2 (27-40) | Tertile 3 (41+) | |||||||
| N | %a | Crude Risk Ratio (95% CI) | N | %a | Crude Risk Ratio (95% CI) | N | %a | Crude Risk Ratio (95% CI) | |
| mTBI, PTSD and Depression | 1,183 | 13.1 | 1.53 (1.28, 1.84)*** | 2,602 | 15.8 | 1.13 (0.99, 1.29) | 4,207 | 24.3 | 1.14 (1.04, 1.25)** |
| PTSD and Depression | 597 | 14.7% | 1.72 (1.38, 2.15)*** | 899 | 15.5 | 1.11 (0.93, 1.33) | 1,280 | 25.3 | 1.19 (1.05, 1.34)** |
| mTBI and Depression | 676 | 7.5 | 0.88 (0.66, 1.18) | 1,012 | 12.4 | 0.89 (0.73, 1.07) | 1,033 | 17.5 | 0.82 (0.70, 0.96)* |
| mTBI and PTSD | 2,814 | 8.6 | 1.00 (0.85, 1.18) | 4,262 | 11.7 | 0.83 (0.73, 0.95) | 4,764 | 18.9 | 0.89 (0.80, 0.97)* |
| Depression-only | 609 | 10.3 | 1.21 (0.94, 1.57) | 732 | 14.7 | 1.05 (0.86, 1.29) | 652 | 21.2 | 0.99 (0.84, 1.17) |
| PTSD-only | 1,463 | 9.2 | 1.08 (0.89, 1.31) | 1,447 | 14.2 | 1.02 (0.86, 1.20) | 1,348 | 21.2 | 0.99 (0.87, 1.13) |
| mTBI-only | 3994 | 6.4% | 0.75 (0.64, 0.88)b | 2,504 | 9.4 | 0.67 (0.57, 0.78)*** | 1,606 | 13.1 | 0.61 (0.53, 0.71)*** |
| No mTBI, PTSD or Depression | 3,933 | 8.5 | REFERENCEb | 2,532 | 14.0 | REFERENCEb | 2,672 | 21.3 | REFERENCEb |
Percent unemployed/not looking for work.
The no diagnosis group was used as a reference group.
p < .05
p < .01
p < .001
Discussion
Prevalence of DTP
The results of the current study replicate and extend our prior findings that the co-occurrence of mTBI, PTSD, and depression is a relatively common pattern of co-morbidity among OEF/OIF veterans, and that it is associated with significant consequences for unemployment status beyond what would be predicted by any of these three diagnoses occurring in isolation. We have previously suggested that this pattern of co-morbid diagnoses represents a specific clinical phenotype, we have termed the Deployment Trauma Phenotype9 (DTP), that arises as a result of combat-related trauma having both physical and psychiatric causes and consequences. It is noteworthy that the prevalence of DTP (16.4%) observed in this large nationally based sample is nearly identical to the prevalence (16.9%) that we reported in our previous study9 using a laboratory based convenience sample (n=255).
Clinical Diagnosis and Unemployment Status
Crude and age- and education- adjusted risk ratios of unemployment among the eight diagnostic groups showed that with the exception of the DTP group and the PTSD and Depression group, all had risk ratios similar to the no diagnosis (reference) group, suggesting that the risk for unemployment for those with a single diagnosis or combined mTBI with depression or PTSD was roughly equivalent. By contrast, the DTP group and the PTSD and Depression group both had elevated risk of unemployment, with the former showing a tendency for conveying the greatest risk when strictly looking at the age-and education-adjusted risk ratios.
With increasing number of diagnoses, NSI symptom severity scores increased. This raised the possibility that it is not a specific constellation of psychiatric diagnoses that determines risk for UNL but rather, global distress as measured by the NSI. However, risk ratios adjusted for the NSI, as well as age and education did not change the overall findings. The mTBI only group showed the lowest risk for UNL, and the DTP and PTSD and Depression diagnoses conveyed the greatest risk for UNL. Analyses stratified by NSI symptom severity also demonstrated the same pattern of findings, with greatest risk for UNL among the DTP and PTSD and Depression groups and lowest risk among the mTBI only group. Strikingly, it was also observed that greatest risk for UNL among the DTP and PTSD and Depression groups was within the first tertile, those who reported the least severe NSI symptoms. With increasing NSI symptom severity (second and third tertiles), risk for UNL generally declined. This was seen despite the fact that there are many more individuals in the third tertile for both of these groups. These findings demonstrate that NSI symptom severity does not mediate the association between diagnostic group and UNL. While higher NSI scores are associated with increasing number of diagnoses these symptoms do not appear to be a strong determinant of UNL risk. In sum, it appears that comorbid PTSD, Depression, and mTBI and not overall NSI symptom severity have significant implications for negative functional outcomes post-deployment (e.g., UNL).
Consistent with other data indicating that age has a significant impact on unemployment status within this cohort of veterans, 16,21 we observed that the effect of DTP on unemployment was influenced by age, with a tendency for the greatest risk of unemployment among those with the DTP between ages 18-49, contrasting with a tendency for the greatest risk of unemployment among those with PTSD and Depression in the oldest age stratum. Further, our data indicated that DTP conveys that risk to a greater number of individuals, as DTP was nearly three times more prevalent than co-morbid PTSD and Depression. Thus, we contend that the DTP conveys risk for unemployment for the highest percentage of OEF/OIF veterans, those under the age of 50.
Military mTBI without co-occurring conditions
Using this national sample, we again found that a history of military mTBI in isolation is not associated with functional disability10, assessed here as unemployed and not seeking work. Specifically, individuals with a diagnosis of mTBI only had the lowest rate of unemployment/not seeking work (8.6%). This rate was even lower than individuals without a diagnosis of mTBI, PTSD, or depression (13.8%), as well as a population based survey of OEF/OIF/OND veterans without disability (14.1%) of the same time period27. In fact, the unemployment rate of the mTBI-only group is comparable to the civilian population rate of unemployment from this time period28. It is possible that the mTBI-only group represents a resilient subgroup of OEF/OIF veterans who deployed to a war zone and were exposed to events leading to mTBI (i.e., blasts) but were not susceptible to the psychological effects of those events in ways similar to the other groups. It has been shown that mTBI, relative to other orthopedic injuries, is often comorbid with other psychiatric diagnoses7. Furthermore, diagnosis of mTBI-only appears to result in better functional outcomes relative to the diagnosis of PTSD or Depression in isolation15 or combination11. Critically, our findings suggest that it is only when mTBI co-occurs with deployment-related PTSD and Depression, that it is associated with negative functional consequences including leaving the workforce.
Our data raise the possibility that DTP may reflect a unique pathophysiology that is not simply a sum of its constituent parts. This situation may be analogous to other syndromic presentations of symptoms or conditions. For example, metabolic syndrome is defined as the presence of three or more of the following conditions: obesity, dyslipidemia, hypertension, and/or diabetes, and is associated with much greater cerebrovascular risk relative to any of its constituent diagnoses in isolation and may be caused by a common underlying pathophysiological mechanism29. Future studies are needed to determine whether there are individuals who are simply more vulnerable to developing DTP because of pre-existing psychological and/or biological circumstances, or whether DTP itself is a consequence of exposure to specific circumstances in combat that impart both physical and psychological trauma.
Secondary observations and policy implications
Although it was not a primary focus of this analysis, it also appeared that Veterans in the DTP group endorsed the greatest number of “post-concussive” symptoms on the NSI compared to any other group, including those with Depression and PTSD alone. Furthermore, participants in the mTBI-only group reported significantly fewer “post-concussive” symptoms than any other group, including those with no confirmed secondary diagnoses. This observation is consistent with Seal and colleagues, and may provide a clue to the functional issues faced by those in the DTP group. The fact that mTBI alone was not associated with elevated symptoms, suggests that the attribution of such symptoms to the neuropathological effects of concussion itself needs careful scrutiny. It is only in the presence of psychiatric co-morbidities that the mTBI was associated with increased reports of such symptomology.
Clinical Implications
The present findings have significant implications with regard to diagnosis and treatment of PTSD, depression and mTBI. First, we suggest that the co-occurrence of certain diagnoses should be considered a definable clinical phenotype requiring treatment(s) encompassing the broad range of psychiatric and physical symptoms likely to be extant in a single patient. This approach would be different than the silo approach most commonly occurring in current medical practice, where such problems are typically diagnosed and treated independently. A consequence of this purely problem-centered silo approach, which requires a heavy burden of clinical visits with little communication across various clinical services, is poor medical compliance, high therapeutic dropout rates, and poor outcome17. In other medically complex populations, such as older adults, integrative or person-centered approaches that consider the high prevalence of multiple conditions have led to superior outcomes29. Second, just as the evidence supports integrative treatment, it also suggests that assessment be comprehensive and multidisciplinary in this younger cohort to create individually tailored treatment targets. Currently, at least within the Veteran's Health Administration, patients are screened for conditions independently. The identification of high-risk phenotypes, such as the DTP, as well as the prevalence of multiple co-occurring behavioral and psychiatric conditions in returning veterans, would suggest that certain individuals receive comprehensive assessments for affective, cognitive and physical issues to guide multidisciplinary treatments.
Limitations
Although this study employed a large sample of OEF/OIF veterans, some limits to the generalizability of these findings should be noted. Specifically, every veteran in this sample screened positive for a military mTBI. While our approach was appropriate for purposes of assessing the prevalence of the DTP, it might not be a full representation of the true prevalence of the DTP constituent diagnoses in isolation and in combination in this cohort. Further, the CTBIE data did not include information on possible confounding causes of unemployment such as retirement or functional disability due to physical injury. This is important because individuals in our unemployed/not looking for work group might have left the work force for reasons other than psychiatric issues. We hypothesize that a high rate of unemployment within the PTSD and Depression group, driven by the oldest age stratum, may have included a higher proportion of retired individuals. However, the data needed to test this hypothesis were not available. Finally, it must be noted that while the current study revealed a virtually identical prevalence of DTP to the findings within the TRACTS TBI National Network Research Center that were based on semi-structured clinical interviews to diagnosis PTSD, depression, and TBI, it is unclear how clinicians performing the CTBIE arrived at their diagnostic impressions. While the CTBIE does require clinicians to determine if another psychiatric disorder could be contributing to the clinical presentation, there is no consistent structured practice for determining the presence of psychiatric conditions required by the CTBIE. Thus, future epidemiological studies must validate the CTBIE clinical impressions with the veterans' general medical record. It must be recognized that not all active duty service members transition their healthcare to the VA upon separation from the military, which could also limit generalizability of our findings30. Consideration of military experiences (e.g., combat exposure, number and length of deployments, rank, and service branch), which could impact psychiatric, TBI, and unemployment status, is also needed. Additionally, at the population level, a comparison of the negative functional outcomes associated with other deployment-related comorbid conditions, such as pain, sleep disorder, and substance abuse, is necessary.
Conclusion
In an epidemiologic, nationally-representative sample that excluded individuals with non-credible responding patterns, the prevalence of the DTP was virtually identical to that observed by the TRACTS TBI National Network Research Center's intensively evaluated convenience sample. The co-occurring and interactive conditions of PTSD, depression and mTBI, rather than any one or two co-occurring conditions, were linked to extremely poor functional outcome (unemployment and not looking for work) in this veteran cohort. Our replication and confirmation of the existence of this clinical phenotype and its accompanying significant risk for unemployment has clear clinical implications, emphasizing the need for integrated, multidisciplinary healthcare services.
Table 2. Crude and age-, education- and NSI-adjusted risk ratios of unemployment by diagnostic group.
| Diagnostic Group | Unemployed | Crude risk ratio (95% CI) | Age- and education-adjusted risk ratio (95% CI) | Age-, education-, and NSI-adjusted risk ratio (95% CI) |
|---|---|---|---|---|
| mTBI, PTSD, and depression | 19.85% | 1.44 (1.34-1.54)a | 1.45 (1.36-1.56)a | 1.16 (1.08-1.24)a |
| PTSD and depression | 19.85% | 1.44 (1.31-1.58)a | 1.39 (1.27-1.52)a | 1.17 (1.06-1.28)b |
| mTBI and depression | 13.11% | 0.95 (0.85-1.06) | 0.95 (0.85-1.07) | 0.85 (0.76-0.94)b |
| mTBI and PTSD | 13.82% | 1.00 (0.94-1.07) | 1.03 (0.96-1.11) | 0.89 (0.83-0.96)b |
| Depression only | 15.46% | 1.12 (1.00-1.26) | 1.08 (0.96-1.21) | 0.99 (0.88-1.11) |
| PTSD only | 14.71% | 1.07 (0.97-1.17) | 1.05 (0.96-1.14) | 0.99 (0.91-1.08) |
| mTBI only | 8.62% | 0.63 (0.57-0.68)a | 0.65 (0.59-0.71)a | 0.69 (0.63-0.75)a |
| No mTBI, PTSD, or depression | 13.79% | Referenced | Referenced | Referenced |
Abbreviations: CI, confidence interval; mTBI, mild traumatic injury; NSI, Neurobehavioral Symptom Inventory; PTSD, posttraumatic stress disorder.
p<.001.
p < .01.
The no diagnosis group was used as a reference group.
Acknowledgments
Funding/Support: This study was supported in part by the Translational Research Center for TBI and Stress Disorders (TRACTS) VA Rehabilitation Research and Development Traumatic Brain Injury National Network Research Center (B9254-C, McGlinchey); NIH NIA K23AG034258 (Fortier); VA CSR&D Merit Review Award (McGlinchey); and VA HSR&D IIR 11-358 (Meterko).
Footnotes
Potential Conflict of Interest Disclosures: None reported
To be noted, a portion of these findings were presented as part of a plenary talk at the recent International Neuropsychological Society's annual meeting (February 5, 2016, Boston, MA) but have not been included in any published journal articles or book chapters.
References
- 1.Erbes CR, Kaler ME, Schult T, Polusny MA, Arbisi PA. Mental health diagnosis and occupational functioning in National Guard/Reserve veterans returning from Iraq. Journal of rehabilitation research and development. 2011;48:1159–70. doi: 10.1682/jrrd.2010.11.0212. [DOI] [PubMed] [Google Scholar]
- 2.Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Southwick SM. Perceived stigma and barriers to mental health care utilization among OEF-OIF veterans. Psychiatric services. 2009;60:1118–22. doi: 10.1176/ps.2009.60.8.1118. [DOI] [PubMed] [Google Scholar]
- 3.Pittman JO, Goldsmith AA, Lemmer JA, Kilmer MT, Baker DG. Post-traumatic stress disorder, depression, and health-related quality of life in OEF/OIF veterans. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2012;21:99–103. doi: 10.1007/s11136-011-9918-3. [DOI] [PubMed] [Google Scholar]
- 4.Schnurr PP, Lunney CA, Bovin MJ, Marx BP. Posttraumatic stress disorder and quality of life: extension of findings to veterans of the wars in Iraq and Afghanistan. Clinical psychology review. 2009;29:727–35. doi: 10.1016/j.cpr.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 5.Cassidy JD, Cancelliere C, Carroll LJ, et al. Systematic review of self-reported prognosis in adults after mild traumatic brain injury: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Archives of physical medicine and rehabilitation. 2014;95:S132–51. doi: 10.1016/j.apmr.2013.08.299. [DOI] [PubMed] [Google Scholar]
- 6.Tanielian T, J L. Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. RAND; Santa Monica: 2008. [Google Scholar]
- 7.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. Soldiers returning from Iraq. The New England journal of medicine. 2008;358:453–63. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- 8.Storzbach D, O'Neil ME, Roost SM, et al. Comparing the Neuropsychological Test Performance of Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans with and without Blast Exposure, Mild Traumatic Brain Injury, and Posttraumatic Stress Symptoms. Journal of the International Neuropsychological Society : JINS. 2015;21:353–63. doi: 10.1017/S1355617715000326. [DOI] [PubMed] [Google Scholar]
- 9.Lippa SM, Fonda JR, Fortier CB, et al. Deployment-related psychiatric and behavioral conditions and their association with functional disability in OEF/OIF/OND veterans. Journal of traumatic stress. 2015;28:25–33. doi: 10.1002/jts.21979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.(WHOSIS) WHOSIS. World Health Statistics. 2010 http://www.who.int/whosis/en/
- 11.Seal KH, Bertenthal D, Samuelson K, Maguen S, Kumar S, Vasterling JJ. Association between mild traumatic brain injury and mental health problems and self-reported cognitive dysfunction in Iraq and Afghanistan Veterans. Journal of rehabilitation research and development. 2016;53:185–98. doi: 10.1682/JRRD.2014.12.0301. [DOI] [PubMed] [Google Scholar]
- 12.Atkinson T, Liem R, Liem JH. The social costs of unemployment: implications for social support. Journal of health and social behavior. 1986;27:317–31. [PubMed] [Google Scholar]
- 13.Sayer NA, Noorbaloochi S, Frazier P, Carlson K, Gravely A, Murdoch M. Reintegration problems and treatment interests among Iraq and Afghanistan combat veterans receiving VA medical care. Psychiatric services. 2010;61:589–97. doi: 10.1176/ps.2010.61.6.589. [DOI] [PubMed] [Google Scholar]
- 14.Kleykamp M. Unemployment, earnings and enrollment among post 9/11 veterans. Social science research. 2013;42:836–51. doi: 10.1016/j.ssresearch.2012.12.017. [DOI] [PubMed] [Google Scholar]
- 15.Sturm RGC, Pacula RL, Wells KB. Datapoints: labor force participation by persons with mental illness. Psychiatric services. 1999;50:1407. doi: 10.1176/ps.50.11.1407. [DOI] [PubMed] [Google Scholar]
- 16.Pogoda TK, Stolzmann KL, Iverson KM, et al. Associations Between Traumatic Brain Injury, Suspected Psychiatric Conditions, and Unemployment in Operation Enduring Freedom/Operation Iraqi Freedom Veterans. The Journal of head trauma rehabilitation. 2016;31:191–203. doi: 10.1097/HTR.0000000000000092. [DOI] [PubMed] [Google Scholar]
- 17.Twamley EWBD, Norman SB, Pittman JO, Lohr JB, Resnick SG. Veterans Health Administration vocational services for Operation Iraqi Freedom/Operation Enduring Freedom Veterans with psychiatric conditions. Journal of rehabilitation research and development. 2013;50:663–70. doi: 10.1682/jrrd.2012.08.0137. [DOI] [PubMed] [Google Scholar]
- 18.Armistead-Jehle P, Cooper DB, Vanderploeg RD. The role of performance validity tests in the assessment of cognitive functioning after military concussion: A replication and extension. Applied neuropsychology Adult. 2016;23:264–73. doi: 10.1080/23279095.2015.1055564. [DOI] [PubMed] [Google Scholar]
- 19.Vanderploeg RD, Cooper DB, Belanger HG, et al. Screening for postdeployment conditions: development and cross-validation of an embedded validity scale in the neurobehavioral symptom inventory. The Journal of head trauma rehabilitation. 2014;29:1–10. doi: 10.1097/HTR.0b013e318281966e. [DOI] [PubMed] [Google Scholar]
- 20.Clark AL, Amick MM, Fortier C, Milberg WP, McGlinchey RE. Poor performance validity predicts clinical characteristics and cognitive test performance of OEF/OIF/OND Veterans in a research setting. The Clinical neuropsychologist. 2014;28:802–25. doi: 10.1080/13854046.2014.904928. [DOI] [PubMed] [Google Scholar]
- 21.Cohen SI, Suri P, Amick MM, Yan K. Clinical and demographic factors associated with employment status in US military veterans returning from Iraq and Afghanistan. Work. 2013;44:213–9. doi: 10.3233/WOR-2012-1417. [DOI] [PubMed] [Google Scholar]
- 22.Hendricks AMAJ, Baker E, Charns MP, Gardner JA, Iverson KM, Kimerling R, Krengel M, Meterko M, Pogoda TK, Stolzmann KL, Lew HL. Screening for mild traumatic brain injury in OEF-OIF deployed US military: an empirical assessment of VHA's experience. Brain Inj. 2013;27:125–34. doi: 10.3109/02699052.2012.729284. [DOI] [PubMed] [Google Scholar]
- 23.Defense. DoVAaDo. VA/DoD Clinical Practice Guideline for Management of Concussion/Mild Traumatic Brain Injury. Washington, DC: Department of Veterans Affairs and Department of Defense; 2009. [Google Scholar]
- 24.Belanger HG, Vanderploeg RD, Sayer N. Screening for Remote History of Mild Traumatic Brain Injury in VHA: A Critical Literature Review. The Journal of head trauma rehabilitation. 2016;31:204–14. doi: 10.1097/HTR.0000000000000168. [DOI] [PubMed] [Google Scholar]
- 25.Jurick SM, Twamley EW, Crocker LD, et al. Postconcussive symptom overreporting in Iraq/Afghanistan Veterans with mild traumatic brain injury. Journal of rehabilitation research and development. 2016;53:571–84. doi: 10.1682/JRRD.2015.05.0094. [DOI] [PubMed] [Google Scholar]
- 26.Lange RT, Brickell TA, Lippa SM, French LM. Clinical utility of the Neurobehavioral Symptom Inventory validity scales to screen for symptom exaggeration following traumatic brain injury. Journal of clinical and experimental neuropsychology. 2015;37:853–62. doi: 10.1080/13803395.2015.1064864. [DOI] [PubMed] [Google Scholar]
- 27.Statistics BoL. Employment status of veterans by age, race, Hispanic or Latino ethnicity, sex, and presence and degree of disability. Current Population Survey. 2009-2013 [Google Scholar]
- 28.Statistics BoL. Employment status of the civilian noninstitutional population: 1943 to date, 2013. Current Population Survey [Google Scholar]
- 29.eatohbcia Epod. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 30.Vanneman ME, Harris AH, Chen C, et al. Army Active Duty Members' Linkage to Veterans Health Administration Services After Deployments to Iraq or Afghanistan and Following Separation. Military medicine. 2015;180:1052–8. doi: 10.7205/MILMED-D-14-00682. [DOI] [PMC free article] [PubMed] [Google Scholar]


