Introduction
Traumatic Brain Injury (TBI) is a leading cause of disability and injury-related death in the United States and worldwide.1 In 2012, it was estimated that there are approximately 1.7 million TBI-related incidents resulting in either an emergency department visit, hospitalization, or death.2 TBI carries an estimated annual financial burden of $50 billion per year in the United States alone.3 As the population of the US continues to age, and given recent increases in the number of TBIs among the elderly in the US4 and worldwide5, 6, the consequences of TBI become even more pressing. TBI is particularly concerning in the elderly population, as it is associated with relatively higher levels of impairment, and higher rates of mortality than in younger age groups.7–9 Inpatient rehabilitation after a TBI has been shown to significantly improve functional outcomes in all age groups,10 and is thought to assist in regaining function that would have otherwise been lost without early aggressive rehabilitation intervention.
Several recent studies suggest regional variation in practice patterns in the management of conditions such as splenic injury11, intussusception12, and urinary lithiasis.13 In the TBI literature, significant variation has been observed with regard to how rehabilitation is delivered14, 15, but there has not been examination of health care delivery systems on a larger scale (state, region, country, etc.). As healthcare costs continue increasing in the United States, identifying efficient health care systems that utilize rehabilitation services appropriately after a TBI has a growing importance. We recently demonstrated significant variation in pediatric TBI outcomes and showed that the state where acute care hospitalization took place was significantly associated with inpatient mortality as well as likelihood of rehabilitation after acute care hospitalization16. In the present study, we aim to examine whether similar relationships exist in adult TBI. We examine variation in adult TBI outcomes and hypothesize that there is significant state-to-state variation for inpatient mortality and discharge disposition in adult patients hospitalized with TBI in the United States.
Methods
Overview of Study Design
This retrospective cohort study was conducted to examine differences in outcomes of adult TBI patients by the state in which care was received. The Healthcare Cost and Utilization Project (HCUP) State Inpatient Database (SID) was used to identify all adult moderate and severe TBI cases hospitalized in reporting states and their subsequent outcomes. Inpatient mortality and discharge to inpatient rehabilitation among inpatients who were discharged alive served as the primary outcomes of interest. State-specific relative risks were generated using multivariable models for both outcomes. This study was not focused on ascertaining why any observed differences between states exist, but rather to determine whether significant state-to-state variation exists, and is based on the premise that, on average, TBI severity in one state is similar to that in other states. Thus, we assume that any observed differences in outcomes can be attributed to differences in the health care systems of each state. Human subjects approval by an institutional review board was not required for analysis of these publicly available datasets without identifiable information.
Data Sources
The SID is a set of hospital databases from data organizations in participating states, and contains the universe of the state inpatient discharge abstracts, translated into a uniform format to facilitate multi-state comparisons and analyses. Although only 48 states participate, the SID from these 48 states represents approximately 97% of all United States community hospital discharges. Although some states include discharges from specialty facilities, such as psychiatric facilities, 98% of the abstracts in the dataset are from community, nonrehabilitation hospitals. The rare occurrence of a hospitalization not being included in the dataset is when a hospital does not generate a bill for an inpatient stay, and for purposes of this analysis, this is assumed not to occur. The SID contains a core set of clinical and nonclinical information on all patients, regardless of payer, including persons covered by Medicare, Medicaid, private insurance, and the uninsured. A subset of 20 states from the 2010 SID was used for this analysis (AR, AZ, CA, CO, FL, IA, KY, MD, MI, MS, NC, NJ, NV, NY, OR, UT, VT, WA, WI, and WV). While there are other state SIDs available for the year 2010, these other state SIDs do not have unique hospital identifiers available, which is necessary to account for clustering by hospital in the statistical analyses. It should be noted that this database treats acute care and rehabilitation units of the same hospital as different hospitals, and thus discharge to a rehabilitation unit within the same hospital is also successfully captured.
Case Selection
We identified all adult patients (>18 years old) hospitalized with TBI (modified CDC definition of TBI using ICD-9 diagnosis codes–800.0–801.9, 800.00–801.99, 803.1–804.9, 803.02–804.99, 850.0–854.1, 850.00–854.19, excluded 950.1–950.3, 995.55, and 959.01) in 20 states during the selected year. The CDC definition was narrowed by the investigators to ensure that patients included had an actual TBI (e.g. 959.01 could refer to a simple laceration of the scalp). Patients were included if one of these codes was listed as a primary or secondary diagnosis as these are typically codes used only for an initial injury (most of these codes have an additional digit to describe the length of loss of consciousness associated with the injury). All available discharge codes were sorted into seven mutually exclusive discharge groups: home, skilled nursing facility (SNF), inpatient rehabilitation, another acute care hospital, psychiatric hospital, hospice, and death. We excluded patients with a discharge disposition “transfer to another acute care hospital” to avoid double counting. Patients discharged to hospice were counted with deaths since these patients were not considered eligible for inpatient rehabilitation. It should be noted that patients discharged home with outpatient rehabilitation or with home health care are not distinguishable from all other patients discharged home in the dataset. We excluded patients for whom any of the following variables was missing (‘N’ in parentheses): age (191), insurance status (255), sex (353), disposition (83). All together, these accounted for 632 patients, representing approximately 0.7% of the sample.
Independent variables of interest
In addition to our main independent variable of interest (state), we were also interested in the independent contributions of age (with spline cutpoints visually determined by unadjusted relationships of age and the outcome of interest), insurance status (government, private, or uninsured), and severity of TBI stratified by Abbreviated Injury Scale (AIS) Score (serious, severe, critical, and unsurvivable).17–21 Severity of TBI was categorized using the ICDPIC program implemented with Stata statistical software (Statacorp LP 14, College Station, TX) that derives AIS scores from ICD9-CM codes.11, 22–24 Patients were only included if they had a head/neck AIS of greater than or equal to 3. Given the paucity of patients in the “unsurvivable” category, these were considered in models as being in the same group as a “critical” injury.
Multivariable Regression Analyses for Binary Outcomes
Two outcomes of interest, hospital mortality rates (out of all discharges) and discharge to inpatient rehabilitation (out of total live discharges), were examined in multivariable regression analyses. State of hospitalization, insurance status, and TBI severity were treated as independent categorical variables while age was treated as a continuous variable with splines at predetermined cutpoints (post-regression linear combinations of these spline variables were used to quantify the risk of age within different ranges). Multivariable Poisson regression with robust standard error estimates and clustering by hospital was used for mortality and rehabilitation outcomes given the non-rare occurrence of our outcomes of interest. Although Poisson regression is typically used for count outcomes, robust Poisson regression is an alternative to logistic regression for non-rare outcomes (>10%) overall25 or among subgroups of interest.26 Note that California was excluded from the rehabilitation regression because of the lack of a code indicating discharge to inpatient rehabilitation. States with the highest number of patients were selected as referent states to optimize standard error calculations. All analyses were performed using Stata/SE 14 (StataCorp LP, College Station, TX).
Results
Patient Characteristics
There were 95,546 adult patients hospitalized with a TBI in the states examined (Table 1) and 68,238 patients discharged alive from the hospital (excluding California). In general, patients were male (61.1%), had a bimodal age distribution with peaks in the 19–29 year old age group and the 80–89 year old age group, an AIS score of 3 (49.5%), had government-based insurance (64.0%), and were discharged to home from the acute care hospital (57.0%).
Table 1.
Characteristics of Adults 19 Years of Age and Above Hospitalized with TBI in 20 States of the US in 2010
| Characteristic | Number | % |
|---|---|---|
| N | 95,546 | |
| Female (%) | 37,161 | 38.9 |
| Age Group | ||
| - 19–29 Years | 11,827 | 12.4 |
| - 30–39 Years | 7,286 | 7.6 |
| - 40–49 Years | 9,587 | 10.0 |
| - 50–59 Years | 12,334 | 12.9 |
| - 60–69 Years | 12,162 | 12.7 |
| - 70–79 Years | 15,290 | 16.0 |
| - 80–89 Years | 20,884 | 21.9 |
| - 90–99 Years | 5,975 | 6.3 |
| - 100+ Years | 201 | 0.2 |
| Severity of Injury | ||
| - Serious TBI | 47,278 | 49.5 |
| - Severe TBI | 45,953 | 48.1 |
| - Critical TBI | 2,242 | 2.4 |
| - Unsurvivable TBI | 73 | 0.1 |
| Insurance | ||
| - Government | 61,463 | 64.0 |
| - Private | 24,918 | 26.0 |
| - Uninsured | 9,611 | 10.0 |
| Disposition | ||
| - Home | 54,423 | 57.0 |
| - Skilled Nursing Facility | 20,590 | 21.6 |
| - Inpatient Rehabilitation | 9,198 | 9.6 |
| - Psychiatric Hospital | 369 | 0.4 |
| - Hospice | 2,091 | 2.2 |
| - Died | 8,875 | 9.3 |
Unadjusted Outcomes
There were statistically significant differences by state in inpatient mortality and the proportion of discharges to inpatient rehabilitation among live patients (Table 2 and 3). Inpatient mortality varied from 9.8% in California to 13.5% in North Carolina. Excluding those who died and patients in California, the proportion of discharges to inpatient rehabilitation varied from 5.6% in Oregon to 19.7% in Massachusetts. Inpatient mortality varied by insurance status from 9.2% in private insurance patients to 12.8% in government-based insurance patients. The proportion of alive discharges to inpatient rehabilitation also varied by insurance status from 5.1% in uninsured patients to 16.9% in private insurance patients.
Table 2.
Adjusted* Relative Risk of Inpatient Mortality** among Adult TBI Patients Hospitalized in 20 States of the US in 2010 (n=95,546)
| Inpatient Mortality | ||||
|---|---|---|---|---|
|
| ||||
| State | N | Crude % | RR | 95% CI |
| Arkansas | 1497 | 12.9 | 1.37 | [1.17, 1.61] |
| Arizona | 4675 | 10.5 | 1.17 | [1.03, 1.33] |
| California | 18107 | 9.8 | Referent | Referent |
| Colorado | 3364 | 10.0 | 1.10 | [0.96, 1.26] |
| Florida | 14078 | 13.4 | 1.35 | [1.22, 1.49] |
| Iowa | 1693 | 12.8 | 1.29 | [1.08, 1.53] |
| Kentucky | 2527 | 13.3 | 1.31 | [1.04, 1.64] |
| Massachusetts | 4013 | 10.2 | 1.05 | [0.88, 1.25] |
| Maryland | 3173 | 10.2 | 1.08 | [0.84, 1.40] |
| Michigan | 6419 | 11.1 | 1.13 | [1.02, 1.25] |
| Mississippi | 1119 | 13.2 | 1.33 | [1.03, 1.71] |
| Nevada | 1941 | 11.2 | 1.21 | [0.99, 1.47] |
| New Jersey | 5128 | 11.8 | 1.17 | [1.04, 1.32] |
| New York | 10813 | 11.0 | 1.13 | [1.02, 1.24] |
| North Carolina | 5199 | 13.5 | 1.36 | [1.21, 1.52] |
| Oregon | 1973 | 11.8 | 1.26 | [1.10, 1.44] |
| Utah | 1406 | 11.7 | 1.32 | [1.14, 1.52] |
| Vermont | 252 | 11.5 | 1.24 | [1.06, 1.46] |
| Washington | 3262 | 11.7 | 1.20 | [1.05, 1.38] |
| Wisconsin | 3180 | 12.9 | 1.30 | [1.10, 1.53] |
| West Virginia | 1727 | 12.5 | 1.31 | [1.12, 1.55] |
|
| ||||
| Severity of TBI | N | Crude % | RR | 95% CI |
|
| ||||
| Serious | 47278 | 8.1 | Referent | Referent |
| Severe | 45953 | 11.7 | 1.21 | [1.16, 1.26] |
| Critical/Unsurvivable | 2315 | 75.0 | 8.88 | [8.49, 9.29] |
|
| ||||
| Type of Insurance | N | Crude % | RR | 95% CI |
|
| ||||
| Government | 61296 | 12.8 | Referent | Referent |
| Private | 24701 | 9.2 | 1.00 | [0.94, 1.05] |
| Uninsured | 9549 | 9.3 | 1.13 | [1.04, 1.23] |
|
| ||||
| Age | Crude % | RR | 95% CI | |
|
| ||||
| Age (Per Year 19–40) | 0.996 | [0.991, 1.001] | ||
| Age (Per Year 41–65) | 1.019 | [1.011, 1.027] | ||
| Age (Per Year 66+) | 1.028 | [1.023, 1.034] | ||
Adjusted for hospital state, severity of TBI, type of insurance, and age
Inpatient Mortality includes discharge to Hospice
Table 3.
Adjusted* Relative Risk of Discharge to Inpatient Rehabilitation Among Alive Adult TBI Patients Hospitalized in 20 States of the US in 2010 (n=68,238)
| Discharge to Rehabilitation | ||||
|---|---|---|---|---|
|
| ||||
| State | N | Crude % | RR | 95% CI |
| Arkansas | 1304 | 18.3 | 1.92 | [1.50, 2.47] |
| Arizona | 4183 | 13.0 | 1.26 | [1.04, 1.52] |
| Colorado | 3029 | 13.9 | 1.36 | [1.07, 1.73] |
| Florida | 12194 | 10.0 | Referent | Referent |
| Iowa | 1476 | 16.4 | 1.57 | [1.12, 2.21] |
| Kentucky | 2190 | 15.2 | 1.54 | [1.13, 2.11] |
| Massachusetts | 3602 | 19.7 | 1.88 | [1.50, 2.36] |
| Maryland | 2854 | 18.0 | 1.77 | [0.97, 3.24] |
| Michigan | 5706 | 13.6 | 1.30 | [1.07, 1.58] |
| Mississippi | 971 | 13.7 | 1.33 | [0.98, 1.81] |
| Nevada | 1723 | 14.7 | 1.43 | [1.16, 1.76] |
| New Jersey | 4521 | 17.2 | 1.78 | [1.42, 2.21] |
| New York | 9620 | 12.8 | 1.25 | [0.99, 1.58] |
| North Carolina | 4498 | 13.7 | 1.36 | [1.08, 1.73] |
| Oregon | 1740 | 5.6 | 0.56 | [0.33, 0.97] |
| Utah | 1242 | 15.2 | 1.43 | [1.06, 1.93] |
| Vermont | 223 | 8.5 | 0.80 | [0.67, 0.96] |
| Washington | 2879 | 9.3 | 0.91 | [0.69, 1.20] |
| Wisconsin | 2771 | 16.3 | 1.59 | [1.27, 1.99] |
| West Virginia | 1512 | 11.0 | 1.08 | [0.82, 1.43] |
|
| ||||
| Severity of TBI | N | Crude % | RR | 95% CI |
|
| ||||
| Serious | 35155 | 12.8 | Referent | Referent |
| Severe | 32623 | 14.0 | 1.11 | [1.06, 1.16] |
| Critical/Unsurvivable | 460 | 30.2 | 2.23 | [1.90, 2.63] |
|
| ||||
| Type of Insurance | N | Crude % | RR | 95% CI |
|
| ||||
| Government | 42373 | 13.4 | Referent | Referent |
| Private | 18844 | 16.9 | 1.18 | [1.11, 1.26] |
| Uninsured | 7021 | 5.1 | 0.36 | [0.30, 0.43] |
|
| ||||
| Age | Crude % | RR | 95% CI | |
|
| ||||
| Age (Per Year 19–85) | 0.999 | [0.998, 1.001] | ||
| Age (Per Year 86+) | 0.940 | [0.925, 0.955] | ||
Adjusted for hospital state, severity of TBI, type of insurance, and age
Multivariable Poisson Regression: Relative Risk of Mortality and Inpatient Rehabilitation Discharge
The multivariable Poisson regression examining inpatient mortality showed adult patients with at least a serious TBI in Arkansas were approximately 34% more likely to die during a hospitalization as an otherwise similar patient in California (Figure 1 and Table 2). Additionally, an adult patient without insurance was approximately 13% more likely to die in the hospital than an otherwise similar patient with government-based or private insurance.
Figure 1.
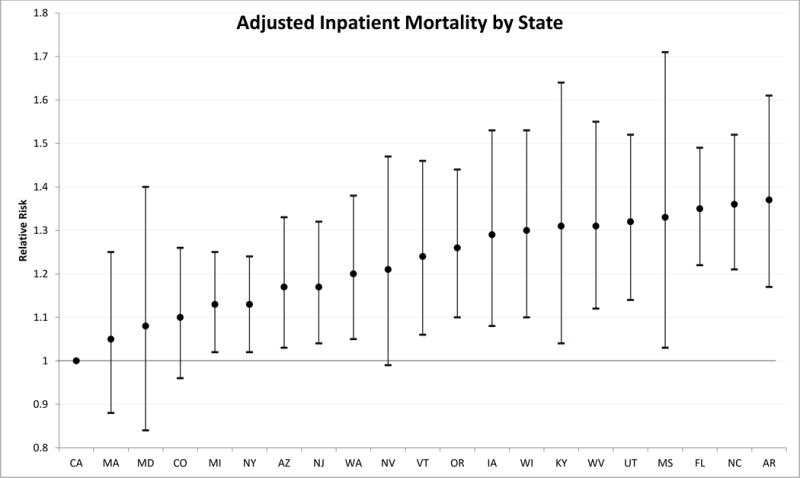
Multivariable Poisson Regression Relative Risk Estimates for Inpatient Mortality by State with robust 95% confidence interval estimates.
The multivariable Poisson regression examining discharge to rehabilitation among living patients showed an adult patient in Arkansas was approximately twice as likely to receive inpatient rehabilitation after a hospitalization with at least a serious TBI than an otherwise similar patient in Florida (Figure 2 and Table 3). Additionally, an adult patient without insurance was 0.35 times as likely to be discharged to inpatient rehabilitation as one with government based insurance (e.g. Medicare or Medicaid).
Figure 2.
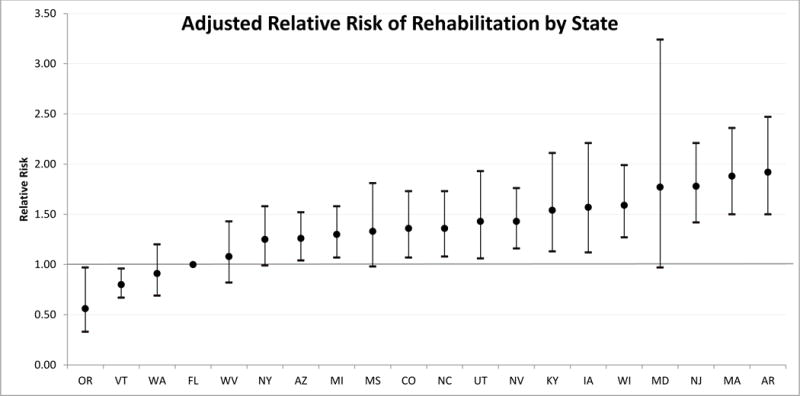
Multivariable Poisson Regression Relative Risk Estimates for Discharge to Inpatient Rehabilitation by State with robust 95% confidence interval estimates.
Discussion
The magnitude (and statistical significance) of differences observed suggest there was clinically significant state-to-state variation in inpatient mortality and rehabilitation hospitalization in adult patients hospitalized for TBI. This variation was only partially attenuated after adjusting for other factors known to affect these outcomes. These differences translate to a substantial number of additional adults with TBI who could potentially receive rehabilitation care annually in the United States. Alternatively, this could also translate to a substantial number of adults unnecessarily receiving inpatient rehabilitation. This study also identified significant state-to-state variation in mortality among adult TBI patients.
Our study demonstrates clinically significant variation in adult TBI outcomes by state, and is one of the largest studies to examine TBI outcomes by age, insurance status and severity of TBI. This study also confirms what has been observed in previous studies27, that there are clinically significant variations in outcomes of patients by insurance status. Uninsured patients were less likely to receive rehabilitation after a TBI (68%) and were more likely higher to die in the hospital (13%) than patients with government or private insurance. While these results may be subject to residual confounding from an incomplete adjustment of variables used in this analysis or confounding from causes not adjusted for in this analysis (e.g. the role socioeconomic status has on health), there still may be other potential causes of this difference that occur before (e.g. prehospital or emergency department care) or after admission (e.g. physician care practices) to the hospital. Inpatient mortality differences may be due to patient factors due to state average differences in comorbidities or system factors such as quality of treatment by pre-hospital providers in the first few hours of care. Similarly, likelihood of discharge to rehabilitation may vary due to regional practice patterns and preferences as well as availability of inpatient rehabilitation beds or differences in state requirements for qualification for an inpatient rehabilitation bed.
There are some study limitations. The sample of states analyzed represents approximately half the US population of adults, thus potentially limiting generalizability. Our analysis does not include race or comorbid conditions. Race is incompletely reported in the SID and sometimes not reported separately from ethnicity, making inference and misclassification a substantial concern if it were to be included. While comorbidity could be estimated with other reported ICD-9-CM diagnosis codes, it was our belief that comorbidity should correlate substantially with age in our sample (and would be methodologically difficult to add as an independent variable in a multivariable model) and would be mostly estimated by adjusting for age. One state in the analysis did not provide sufficient data on rehabilitation discharges: California used the same code indicating “discharge to a rehabilitation hospital” as discharge to a skilled nursing facility. We did not have information on treatment variation nor could we address issues of access bias as availability of emergency care may have an effect on out of hospital death, thereby affecting overall injury severity of patients who present to the emergency department. There may also be variation between states in practices for location of declaration of death. Analysis of these practices would allow examination of the types of patients that are being hospitalized with TBI (e.g. if emergency responders in one state are more likely to declare death before hospitalization, the state in question would have a population of patients hospitalized with TBI that may be less likely to die and have a lower inpatient mortality rate). While location of declaration of death is technically available via the CDC WONDER database (wonder.cdc.gov), much of this information is missing. Lastly, while we did not adjust for severity of other injuries, we assumed that severity of co-occurring non-head injuries is similar between states, and thus an unlikely source of bias.
We would also like to note that the interpretation of a clinically significant result can be debated. This study demonstrated statistical significance, which permits us to then discuss whether or not the results observed are clinically significant. In our collective opinion, the variation observed (which has been shown not to be due to chance alone) is large enough that it is of “clinical significance.” While we were expecting less variation in the adult population (as compared to the pediatric population) because of the established guidelines for treatment of traumatic brain injury, we found the degree of variation observed for both outcomes clinically relevant and interesting. We should also use caution when applying these results to states and years not measured in this analysis. This analysis was restricted to 20 of the 50 states in the United states in the year 2010. While it may seem reasonable to infer that there may be clinically significant variation in states or years not measured, the data presented in this study does not allow us to do so.
Future work should be done to examine differences in health policy affecting access and use of inpatient rehabilitation care that may exist between states and what can be done at both state and local levels to decrease these variations in outcomes by state. Health policies and systems of states at both ends of the spectrum (with regard to relative risk of the studied outcomes) should be analyzed closely to identify different types and functioning of trauma care systems as there are many steps in the care of each adult TBI patient from when the initial injury occurs to being discharged from the hospital. States with a high rate of inpatient rehabilitation utilization should be examined to ensure patients are utilizing resources appropriately while states with a low rate of rehabilitation utilization should be examined to ensure adequacy of available rehabilitation beds and providers are referring patients appropriately to rehabilitation after a hospitalization for TBI. High and low mortality states should also be examined to determine what types of practices may be contributing to or preventing inpatient mortality. It should be noted that the care examined in this analysis specifically starts with admission to a hospital and end with discharge from the acute care hospital.
While there are national TBI guidelines to guide appropriate treatment28, these guidelines need to be implemented uniformly, in every state, to best treat TBI patients. Next steps should involve examining why this variation exists, and assessing whether it is as simple as adherence to national guidelines for treatment of TBI or if there are other important factors responsible for the substantial differences in outcomes observed throughout the United States.
Acknowledgments
This study had no external source of funding.
Footnotes
The authors have no conflicts of interest to declare.
This material has not been presented at any professional meetings.
References
- 1.Coronado VG, Xu L, Basavaraju SV, McGuire LC, Wald MM, Faul MD, et al. Surveillance for traumatic brain injury-related deaths–United States, 1997–2007. MMWR Surveill Summ. 2011;60(5):1–32. [PubMed] [Google Scholar]
- 2.Coronado VG, McGuire LC, Sarmiento K, Bell J, Lionbarger MR, Jones CD, et al. Trends in Traumatic Brain Injury in the U.S. and the public health response: 1995–2009. Journal of safety research. 2012;43(4):299–307. doi: 10.1016/j.jsr.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 3.Zammit C, Knight WA. Severe traumatic brain injury in adults. Emergency medicine practice. 2013;15(3):1–28. [PubMed] [Google Scholar]
- 4.Kannus P, Niemi S, Parkkari J, Palvanen M, Sievanen H. Alarming rise in fall-induced severe head injuries among elderly people. Injury. 2007;38(1):81–3. doi: 10.1016/j.injury.2006.08.027. [DOI] [PubMed] [Google Scholar]
- 5.Hartholt KA, Van Lieshout EM, Polinder S, Panneman MJ, Van der Cammen TJ, Patka P. Rapid increase in hospitalizations resulting from fall-related traumatic head injury in older adults in The Netherlands 1986–2008. Journal of neurotrauma. 2011;28(5):739–44. doi: 10.1089/neu.2010.1488. [DOI] [PubMed] [Google Scholar]
- 6.Jamieson LM, Roberts-Thomson KF. Hospitalized head injuries among older people in Australia, 1998/1999 to 2004/2005. Injury prevention : journal of the International Society for Child and Adolescent Injury Prevention. 2007;13(4):243–7. doi: 10.1136/ip.2007.015354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Utomo WK, Gabbe BJ, Simpson PM, Cameron PA. Predictors of in-hospital mortality and 6-month functional outcomes in older adults after moderate to severe traumatic brain injury. Injury. 2009;40(9):973–7. doi: 10.1016/j.injury.2009.05.034. [DOI] [PubMed] [Google Scholar]
- 8.Hukkelhoven CW, Steyerberg EW, Rampen AJ, Farace E, Habbema JD, Marshall LF, et al. Patient age and outcome following severe traumatic brain injury: an analysis of 5600 patients. Journal of neurosurgery. 2003;99(4):666–73. doi: 10.3171/jns.2003.99.4.0666. [DOI] [PubMed] [Google Scholar]
- 9.McIntyre A, Mehta S, Aubut J, Dijkers M, Teasell RW. Mortality among older adults after a traumatic brain injury: a meta-analysis. Brain injury : [BI] 2013;27(1):31–40. doi: 10.3109/02699052.2012.700086. [DOI] [PubMed] [Google Scholar]
- 10.Agrawal M, Joshi M. Impact of rehabilitation on functional outcome during the first year of moderate and severe traumatic brain injury. Brain injury : [BI] 2014;28(3):292–7. doi: 10.3109/02699052.2013.865266. [DOI] [PubMed] [Google Scholar]
- 11.Hamlat CA, Arbabi S, Koepsell TD, Maier RV, Jurkovich GJ, Rivara FP. National variation in outcomes and costs for splenic injury and the impact of trauma systems: a population-based cohort study. Annals of surgery. 2012;255(1):165–70. doi: 10.1097/SLA.0b013e31823840ca. [DOI] [PubMed] [Google Scholar]
- 12.Rice-Townsend S, Chen C, Barnes JN, Rangel SJ. Variation in practice patterns and resource utilization surrounding management of intussusception at freestanding Children’s Hospitals. Journal of pediatric surgery. 2013;48(1):104–10. doi: 10.1016/j.jpedsurg.2012.10.025. [DOI] [PubMed] [Google Scholar]
- 13.Scales CD, Jr, Krupski TL, Curtis LH, Matlaga B, Lotan Y, Pearle MS, et al. Practice variation in the surgical management of urinary lithiasis. The Journal of urology. 2011;186(1):146–50. doi: 10.1016/j.juro.2011.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seel RT, Barrett RS, Beaulieu CL, Ryser DK, Hammond FM, Cullen N, et al. Institutional Variation in Traumatic Brain Injury Acute Rehabilitation Practice. Archives of physical medicine and rehabilitation. 2015;96(8 Suppl):S197–208. doi: 10.1016/j.apmr.2015.02.034. [DOI] [PubMed] [Google Scholar]
- 15.Rivara FP, Ennis SK, Mangione-Smith R, MacKenzie EJ, Jaffe KM. Variation in adherence to new quality-of-care indicators for the acute rehabilitation of children with traumatic brain injury. Archives of physical medicine and rehabilitation. 2012;93(8):1371–6. doi: 10.1016/j.apmr.2012.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greene NH, Kernic MA, Vavilala MS, Rivara FP. Variation in pediatric traumatic brain injury outcomes in the United States. Archives of physical medicine and rehabilitation. 2014;95(6):1148–55. doi: 10.1016/j.apmr.2014.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Slomine BS, McCarthy ML, Ding R, MacKenzie EJ, Jaffe KM, Aitken ME, et al. Health care utilization and needs after pediatric traumatic brain injury. Pediatrics. 2006;117(4):e663–74. doi: 10.1542/peds.2005-1892. [DOI] [PubMed] [Google Scholar]
- 18.Svenson JE, Spurlock CW. Insurance status and admission to hospital for head injuries: are we part of a two-tiered medical system? The American journal of emergency medicine. 2001;19(1):19–24. doi: 10.1053/ajem.2001.18041. [DOI] [PubMed] [Google Scholar]
- 19.Haider AH, Efron DT, Haut ER, DiRusso SM, Sullivan T, Cornwell EE., 3rd Black children experience worse clinical and functional outcomes after traumatic brain injury: an analysis of the National Pediatric Trauma Registry. The Journal of trauma. 2007;62(5):1259–62. doi: 10.1097/TA.0b013e31803c760e. discussion 62-3. [DOI] [PubMed] [Google Scholar]
- 20.Haas JS, Goldman L. Acutely injured patients with trauma in Massachusetts: differences in care and mortality, by insurance status. American journal of public health. 1994;84(10):1605–8. doi: 10.2105/ajph.84.10.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morrison WE, Arbelaez JJ, Fackler JC, De Maio A, Paidas CN. Gender and age effects on outcome after pediatric traumatic brain injury. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2004;5(2):145–51. doi: 10.1097/01.pcc.0000112373.71645.2a. [DOI] [PubMed] [Google Scholar]
- 22.Sears JM, Blanar L, Bowman SM. Predicting work-related disability and medical cost outcomes: A comparison of injury severity scoring methods. Injury. 2013 doi: 10.1016/j.injury.2012.12.024. [DOI] [PubMed] [Google Scholar]
- 23.Clark DE, O TM, Hahn DR. ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores. Available from: URL: http://ideas.repec.org/c/boc/bocode/s457028.html.
- 24.Greene NH, Kernic MA, Vavilala MS, Rivara FP. Validation of ICDPIC software injury severity scores using a large regional trauma registry. Injury prevention : journal of the International Society for Child and Adolescent Injury Prevention. 2015 doi: 10.1136/injuryprev-2014-041524. [DOI] [PubMed] [Google Scholar]
- 25.Zou G. A modified poisson regression approach to prospective studies with binary data. American journal of epidemiology. 2004;159(7):702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 26.Cummings P. The relative merits of risk ratios and odds ratios. Archives of pediatrics & adolescent medicine. 2009;163(5):438–45. doi: 10.1001/archpediatrics.2009.31. [DOI] [PubMed] [Google Scholar]
- 27.Englum BR, Villegas C, Bolorunduro O, Haut ER, Cornwell EE, 3rd, Efron DT, et al. Racial, ethnic, and insurance status disparities in use of posthospitalization care after trauma. Journal of the American College of Surgeons. 2011;213(6):699–708. doi: 10.1016/j.jamcollsurg.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guidelines for the management of severe traumatic brain injury. Journal of neurotrauma. 2007;24(Suppl 1):S1–106. doi: 10.1089/neu.2007.9999. [DOI] [PubMed] [Google Scholar]


