Abstract
Introduction
Non-adherence to asthma daily controller medications is a common problem, reported to be responsible for 60% of asthma-related hospitalisations. The mean level of adherence for asthma medications is estimated to be as low as 22%. Therefore, objective measurements of adherence to medicine are necessary. This virtual observational study is designed to measure the usability of an electronic monitoring device platform that measures adherence. Understanding how patients use the BreatheSmart mobile technology at home is essential to assess its feasibility as a solution to improve medication adherence. We anticipate this approach can be applied to real-world environments as a cost-effective solution to improve medication adherence.
Methods and analysis
This is a virtual 6-month observational study of 100 adults (≥18 years) with an asthma diagnosis, using inhaled corticosteroids for at least 3 months. Participants will be recruited in the USA through ad placements online. All participants receive wireless Bluetooth-enabled inhaler sensors that track medication usage and an mSpirometerTM capable of clinical-grade lung function measurements, and download the BreatheSmart mobile application that transmits data to a secure server. All analyses are based on an intention-to-treat. Usability is assessed by patient questionnaires and question sessions. Simple paired t-test is used to assess significant change in Asthma Control Test score, quality of life (EuroQol-5D questionnaire) and lung function.
Ethics and dissemination
No ethical or safety concerns pertain to the collection of these data. Results of this research are planned to be published as soon as available.
Trial registration number
Keywords: telemanagement, mHealth, telehealth, telemedicine, real-time reminders, text message reminders, medication adherence, inhaled corticosteroids, asthma, asthma control, medication adherence, mobile health, patientmonitoring, mobile health
Introduction
Asthma is a chronic disease that affects 21 million Americans (300 million individuals globally) and has broad implications for both the health of affected individuals and for the US economy.1–4 The National Institutes of Health Morbidity and Mortality report indicates that as high as 15.6% of the US population may have asthma.1 Furthermore, this disease is responsible for a decrease in quality of life scores,5 and adult patients with asthma are twice as likely to rate their own health as ‘only fair’, ‘poor’ or ‘very poor’ when surveyed.6
In 2009 alone, 10.6 million physician visits1 and 1.5 million emergency room (ER) visits in the USA were due to asthma.7 High utilisation of asthma-related medical services, lost work and school days, and early deaths led to an estimated $56 billion in costs.8 Adults with asthma incur nearly $2000 a year (US$2008) in additional costs to the healthcare system compared with those without asthma.3 9 Furthermore, a single patient with uncontrolled asthma can cost the health system up to an extra $4423.4
Current therapies for asthma include inhaled corticosteroids (ICS), which have been hailed as ‘the cornerstone of maintenance asthma therapy’.10 They are the most widely used drug therapy among physicians, and when taken as prescribed can improve lung function over time.11 ICS must be taken daily to provide therapeutic benefit and manage chronic symptoms.
Adherence to medication treatment plans is critical to the management of this disease. Treatment adherence of 75%–80% is considered therapeutically optimal based on evidence from studies of lung function and sputum eosinophil concentration.12 13 One comprehensive report from Williams et al 12 14 determined that 24% of asthma exacerbations were attributable to ICS medication non-adherence. Further, 60% of asthma-related hospitalisations can be attributed to poor adherence.10
Currently, adherence to medications for asthma is extremely poor. The mean level of adherence for asthma medications is estimated to be 30%–40%, with a number of trials reporting adherence rates as low as 22%.10 14–16 The broad range of reported adherence values and non-consensus in the literature is due, in a large part, to the challenging nature of obtaining reliable adherence metrics.17 While self-reported adherence levels are the most straightforward and low cost, evidence suggests that patients over-report medication use when asked.16 Other techniques for capturing adherence to medication have been used, including biometric data capture and the use of prescription refill data accessed through electronic medical records.18–20 Each of these measures poses limitations on its own, and even taken together these metrics do not provide a clear, quantifiable measurement of adherence to daily controller ICS medications.21 The need for objective real-time methods of measuring adherence to ICS medication is evident, and electronic monitoring devices (EMDs) offer a solution with potential to become the gold standard in asthma care for the 21st century.22
EMDs plus electronic text messaging (SMS) interventions have been implemented in other chronic disease states, including diabetes and congestive heart failure, with marked success.23–25 Benefits of EMDs include the ability to track exact numbers of doses taken without a patient needing to add extra steps to their care plan, to provide new data to assist in clinical decision making, and to increase motivation and engagement in patients.26 SMS or other push notifications provide study participants with feedback and/or reminders based on data captured through EMDs. In most recent years (2015–2016), evidence has been more supportive in favour of EMDs with SMS and/or push notifications. One 2016 randomised controlled trial reported significant lifts in adherence (70% intervention arm, 49% control arm) in patients using EMDs and receiving daily SMS and/or push notifications to take medications.21
While the benefits to support the use of these devices are compelling, research on the ability of EMDs to improve patient outcomes in asthma has proved to be challenging to implement, leading to inconclusive evidence on their efficacy.27–29 Feasibility pilots have reported high rates of data transmission failure from devices,30 high cost of implementation17 and high rates of alert fatigue as patients are desensitised to the stimulus of message reminders.31 Additionally, such technology has faced scepticism from healthcare providers. A 2016 survey of healthcare providers and members of clinical commissioning groups reported that the number 1 cited drawback to clinically administered EMD therapies was lack of research to support efficacy.26
There is a clear need to produce more data on medication adherence and clinical outcomes in populations using EMDs to determine if these promising results can be replicated. Furthermore, as EMD devices become available outside of controlled trial settings, it will be increasingly important to understand how patients interact with such technology and what barriers exist to at-home use. In order for this technology to be made widely available and cost-effective, patients must be able to set up and use the technology independently, with little oversight from research or clinical staff. Clinical trial environments do not reflect the reality of how patients would interact with such technology in a real-world environment. This study aims to contribute to that knowledge base.
The primary purpose of this virtual observational study is to measure the usability of the comprehensive Cohero Health® mHealth asthma management platform at-home including the EMD and the mobile application (BreatheSmart), which sends real-time reminders to take medication and perform mSpirometerTM lung function testing. The secondary objectives of the study include monitoring real-time controller medication adherence and frequency of rescue medication use, and collecting data on asthma control, lung function, quality of life and frequency of provider visits for asthma-related adverse outcomes. Importantly, the virtual observational study design is meant to capture a more accurate snapshot of patient use of this technology in a ‘real-world’ setting in order to capture patient use characteristics outside of a traditional randomised controlled trial setting.
Methods and analysis
Study population
One hundred subjects with a self-identified diagnosis of asthma will be recruited within the USA through social media websites and ad placements online. Subjects will fill out an online screening form with the inclusion and exclusion criteria listed in box 1.
Box 1. Inclusion and exclusion criteria.
Inclusion criteria (all of the following):
Age 18+
Self-identified diagnosis of asthma for at least 6 months
Prescribed daily inhaled corticosteroid medication for at least 3 months
Use of a pressurised metered dose inhaler compatible with the Cohero Health mHealth HeroTracker (see online supplementary appendix A)
Possesses a compatible smartphone (iOS 8.0 or higher and Android 4.3 or higher)
Exclusion criteria (any of the following):
Inability to provide written informed consent
Inability to use electronic monitoring device/mobile application platform independently
Currently pregnant or planning to become pregnant during the study period, as pregnancy can have an independent effect on asthma symptoms
Primary language other than English
Description of Cohero Health platform
Electronic monitoring device
Cohero Health HeroTrackers® are wireless Bluetooth-enabled EMDs that track medication usage using a pressure sensitive switch. They are designed for both control and rescue medications in MDI and diskus format.
Lung function monitoring device
Cohero Health mSpirometer is capable of clinical-grade lung function measurements, including peak expiratory flow and common pulmonary function test (PFT) values such as forced expiratory volume in 1 s and forced vital capacity. The device is ISO 9001 and 13 485 certified and received 510(k) clearance as a class II medical device for in-clinic use. At-home use of the mSpirometer will be assessed in this study as users will self-administer lung function testing at home with guided instruction through the BreatheSmart mobile application interface along with real-time feedback to ensure appropriate technique. The mSpirometer can be programmed for use in two modes: a 1 s peak flow measurement and a 6 s complete PFT measurement.
Mobile application
BreatheSmart is a mobile application for iOS and Android. The application uses Bluetooth to connect with the hardware components of Cohero Health’s platform in order to collect adherence and lung function data and transmit data to the Cohero Health Health Insurance Portability and Accountability (HIPAA)-compliant server. BreatheSmart also sends notification reminders to remind users to take medication at times chosen by the user to align with their prescribed care plan.
Study design
This is a 6-month virtual observational study that will occur independent of participants’ normal asthma care. One hundred adults with asthma will be recruited in the USA through social media websites and ad placements online. Subjects will fill out an online screening form with the inclusion and exclusion criteria listed in box 1. If deemed eligible on the online self-screening form, they will be contacted by the study team to further discuss the study and conduct the informed consent process via an online web portal. The participants’ attention is specifically called to the portion of the consent form that indicated that this study does not replace normal care by a licensed provider, and that this study is an observation of use of EMDs, and not a treatment study in any way.
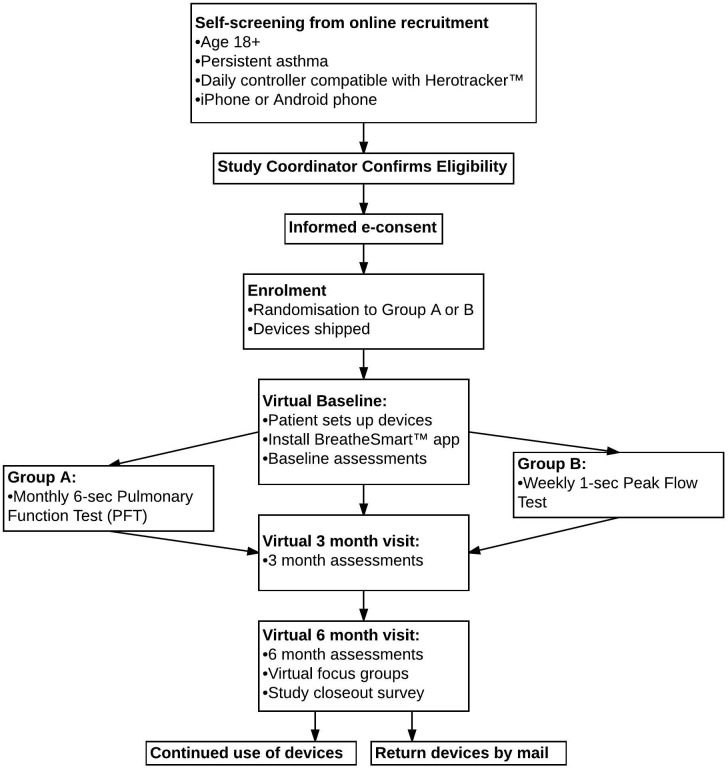
Study participants will be asked to attend regular visits with their care providers and continue to take their asthma medication as recommended by their clinician. Once they are enrolled in the study, patients will be randomised to one of two arms and follow the study design outlined in figure 1. Fifty participants will be placed in group A and receive the mSpirometer programmed for 6 s complete PFT testing and 50 participants will be placed in group B and receive the mSpirometer programmed for 1 s peak flow measurement in order to assess patient experiences with each version of the technology.
Figure 1.
CONSORT flow diagram. PFT, pulmonary function test.
Once enrolled and randomised in the study, participants will be shipped a device package including EMDs for control and rescue inhalers as well as an mSpirometer. Devices will be accompanied by user manuals with detailed instructions for research participants to download the BreatheSmart application to their mobile device and to set up EMDs on their own. Users who are unable to set up the mobile application and devices on their own will be offered optional interactive phone or video conference assistance from the research team.
As part of the virtual baseline visits, participants will complete an online form of the Asthma Control Test (ACT), EuroQol-5D validated quality of life questionnaire, baseline asthma disease and demographic questionnaire, as well as instructed to perform lung function testing using the mSpirometer.
Throughout the study, group A will receive reminders from the mobile app to perform monthly 6 s PFT testing on the mSpirometer and group B will receive reminders to perform a weekly 1 s peak flow testing on the mSpirometer. Both groups will also receive daily reminders from the mobile app to take their medication and will be able to monitor their own medication usage on a daily and weekly basis.
Study participants will also be asked to fill out questionnaires online at 3 months and 6 months (including ACT and EuroQol-5D). At the end of the study, participants will be invited to end-of-study focus groups in a virtual text chat room.
Study enrolment is planned to start in March 2017 and the final patient is planned to finish in March 2018.
Outcomes
Primary study endpoint
Usability is measured by:
backend measures of subjects’ use of the EMD and mobile app and ability of platform to sync and upload data
usability questionnaire
acceptability questionnaire including subjects’ opinion of the platform and its features
virtual focus groups with study subjects.
Important secondary objectives
Outcome measures include:
real-time controller medication adherence
frequency of rescue medication use as measured by the EMDs
asthma control
lung function
quality of life using the EuroQol-5D
healthcare utilisation during the study period.
Measurements
Patient usage and interaction with the mobile app as well as timing and frequency of controller and rescue medication use will be measured daily during the study period. Additionally, per the study design described above, patients will be prompted to perform regular lung function measurements during the study period (monthly 6 s PFT for group A, weekly 1 s peak flow for group B).
Questionnaires
Asthma control will be measured by the ACT at baseline, 3 months and 6 months. Quality of life during the study period will be assessed using the EuroQol-5D. Self-reported healthcare utilisation including provider visits for asthma-related adverse outcomes will be assessed by questionnaire. Self-reported asthma exacerbations including ER visits, hospitalisations or systemic corticosteroid therapy will also be assessed for this period.
Statistical methods and data analysis plan
Logistics
Backend measures of usability are also recorded and uploaded into the Structured Query Language (SQL) database. Analysis will be performed by the research team at Cohero Health. All analyses will be based on an intention-to-treat.
Simple paired t-test will be used to assess for significant change in ACT, quality of life and lung function. Lung function metrics will be aggregated across the study period to look for population trends. Other baseline and follow-up survey findings, including adverse asthma events, will be assessed for change from baseline to follow-up.
Sample size
This is a cohort observational study in which we aim to assess the usability of the Cohero Health mobile platform for at-home patient use as an asthma self-management tool. As the primary outcome cannot be boiled down to a single quantitative measure, we were not able to perform appropriate sample size calculation for the primary objective. However, with 100 patients for 6 months, we will be obtaining, if it is assumed an average patient takes two medication puffs per day, 2×30×6=up to 360 real-time medication measurements during the study period per patient.
Data collection
Research survey responses will be input directly by study subjects into the BreatheSmart mobile application where they are saved into a backend SQL database. Medication adherence data are recorded on the EMD, which then transmitsSupplementary file 1 that information via Bluetooth Low Energy to the mobile app and up to our HIPAA-compliant server and backend SQL database. The lung function data are recorded directly by the mSpirometer and also sent via Bluetooth Low Energy to the mobile app and again to the SQL database.
bmjresp-2017-000204supp001.pdf (53.6KB, pdf)
Data monitoring and quality assurance
Prior to study enrolment, all research staff will be trained in principles of human subject’s protection and maintenance of confidentiality of participant data. This study will be monitored by a representative of Cohero Health. Routine interim monitoring of the data will be conducted every quarter with two audits to be conducted between each quarter. Monitoring will be in the form of a review of the data recorded in the BreatheSmart applications. Any issues identified will be communicated to the investigator. The investigator is expected to resolve any outstanding action items in a timely manner.
Discussion
This study aims to assess the use of an EMD and asthma management system in a deployment consistent with the intended use of such technologies. By using a virtual study design without traditional in-person study visits, we intend to emulate the real-world scenario in which patients might interact with the technology and to demonstrate the ability of EMDs to engage patients, sustain engagement and assess usability of these products with minimal research staff support. Thus we seek to reliably and objectively validate EMD as a method for adherence measurement. As this study is being conducted by Cohero Health, which designs the EMD and asthma management platform being assessed, we hope the virtual study design will in particular minimise potential bias by having fewer interactions between the study team and study participants, as well as by minimising Hawthorne effect, which may induce patients to be more adherent because they are aware they are being observed. We aim to be as inclusive as possible by not imposing restrictions on location, quality of phones, access to Wi-Fi and phone data plans, socioeconomic status, and technological proficiency.
If Cohero Health mobile technology proves easy to use at home, it will validate this technology as a cost-effective solution to improve medication adherence and outcomes in patients with asthma using daily ICS. If there prove to be challenges in the implementation of the study related to such a ‘hands-off’ approach, it will enable technology and usability optimisation to improve this product for patient use based on the direct feedback of study participants and thus lead to patient-centred improvements in the design of this technology. The use of an electronic recruitment strategy means that we anticipate a more diverse patient population as it is not limited to those patients in a specific zip code or seen at a specific health centre. Thus, we anticipate findings will be more broadly applicable to the general asthma patient population in the USA. This study will be an important stepping stone for future endeavours to provide evidence of the cost-effectiveness that would be invaluable for providers and payers in considering this approach for daily clinical practice.
Footnotes
Contributors: EM drafted portions of the paper, prepared the article for submission and iterated on draft versions of the paper. AC contributed to the design of the protocol, iterated on draft versions of the paper, assisted in management of the paper submission and provided clinical expertise. AT contributed to the design of the protocol, drafted portions of the paper, iterated on draft versions of the paper and assisted in management of the paper submission. RK contributed to the design of the protocol and drafting of the paper. MM oversaw the creation and submission of the protocol and provided senior clinical and professional expertise and guidance.
Funding: This work was supported Cohero Health. This research received no specific grant from any other funding agency in the public or not-for-profit sectors.
Competing interests: None declared.
Patient consent: This is a protocol paper and therefore this article contains no personal medical information about any identifiable living individuals, and therefore does not require the patient’s explicit consent for publication.
Ethics approval: Approval Number: 20162351. Board Name: Western Institutional Review Board Board. Affiliation: WIRB-Copernicus Group. Board Contact: Western Institutional Review Board, 1019 39th Avenue SE, Suite 120, Puyallup, WA 98374-2115.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. National Institutes of Health: National Heart LaBI. Morbidity & Mortality: 2012 Chart Bookk on Cardiovascular, lung, and blood diseases: National Institutes of Health, 2012. [Google Scholar]
- 2. Lethbridge-Cejku M, Schiller JS, Bernadel L, et al. Summary health statistics for U.S. adults: National Health Interview Survey, 2002. Vital and health statistics Series 10, Data from the National Health Survey 2004;222:1–151. [PubMed] [Google Scholar]
- 3. Sullivan PW, Slejko JF, Ghushchyan VH, et al. The relationship between asthma, asthma control and economic outcomes in the United States. J Asthma 2014;51:769–78. doi:10.3109/02770903.2014.906607 [DOI] [PubMed] [Google Scholar]
- 4. Sullivan PW, Ghushchyan VH, Slejko JF, et al. The burden of adult asthma in the United States: evidence from the medical expenditure panel survey. J Allergy Clin Immunol 2011;127:363–9. doi:10.1016/j.jaci.2010.10.042 [DOI] [PubMed] [Google Scholar]
- 5. Goldney RD, Ruffin R, Fisher LJ, et al. Asthma symptoms associated with depression and lower quality of life: a population survey. Med J Aust 2003;178:437–41. [DOI] [PubMed] [Google Scholar]
- 6. Meltzer EO, Blaiss MS, Nathan RA, et al. Asthma burden in the United States: results of the 2009 Asthma Insight and Management survey. Allergy Asthma Proc 2012;33:36–46. doi:10.2500/aap.2011.32.3519 [DOI] [PubMed] [Google Scholar]
- 7. Janson SL, McGrath KW, Covington JK, et al. Individualized asthma self-management improves medication adherence and markers of asthma control. J Allergy Clin Immunol 2009;123:840–6. doi:10.1016/j.jaci.2009.01.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Prevention CfDCa. Asthma in the US: growing every year. 2011. https://www.cdc.gov/vitalsigns/asthma/.
- 9. Bahadori K, Doyle-Waters MM, Marra C, et al. Economic burden of asthma: a systematic review. BMC Pulm Med 2009;9:24 doi:10.1186/1471-2466-9-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bårnes CB, Ulrik CS. Asthma and adherence to inhaled corticosteroids: current status and future perspectives. Respir Care 2015;60:455–68. doi:10.4187/respcare.03200 [DOI] [PubMed] [Google Scholar]
- 11. National Asthma Education and Prevention Program TEPotDaMoA. Expert Panel Report 3: guidelines for the diagnosis and management of Asthma. Bethesda (MD): National Heart, lung, and Blood Institute (US), 2007. [Google Scholar]
- 12. Williams LK, Peterson EL, Wells K, et al. Quantifying the proportion of severe asthma exacerbations attributable to inhaled corticosteroid nonadherence. J Allergy Clin Immunol 2011;128:1185–91. doi:10.1016/j.jaci.2011.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Murphy AC, Proeschal A, Brightling CE, et al. The relationship between clinical outcomes and medication adherence in difficult-to-control asthma. Thorax 2012;67:751–3. doi:10.1136/thoraxjnl-2011-201096 [DOI] [PubMed] [Google Scholar]
- 14. Williams LK, Peterson EL, Wells K, et al. A cluster-randomized trial to provide clinicians inhaled corticosteroid adherence information for their patients with asthma. J Allergy Clin Immunol 2010;126:225–31. doi:10.1016/j.jaci.2010.03.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rand CS, Wise RA. Measuring adherence to asthma medication regimens. Am J Respir Crit Care Med 1994;149:S69–S76. discussion S7-8 doi:10.1164/ajrccm/149.2_Pt_2.S69 [DOI] [PubMed] [Google Scholar]
- 16. Sumino K, Cabana MD. Medication adherence in asthma patients. Curr Opin Pulm Med 2013;19:49–53. doi:10.1097/MCP.0b013e32835b117a [DOI] [PubMed] [Google Scholar]
- 17. Morton RW, Everard ML, Elphick HE. Adherence in childhood asthma: the elephant in the room. Arch Dis Child 2014;99:949–53. doi:10.1136/archdischild-2014-306243 [DOI] [PubMed] [Google Scholar]
- 18. Krishnan JA, Bender BG, Wamboldt FS, et al. Adherence to inhaled corticosteroids: an ancillary study of the childhood asthma management program clinical trial. J Allergy Clin Immunol 2012;129:112–8. doi:10.1016/j.jaci.2011.10.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Foster JM, Usherwood T, Smith L, et al. Inhaler reminders improve adherence with controller treatment in primary care patients with asthma. J Allergy Clin Immunol 2014;134:1260–8. doi:10.1016/j.jaci.2014.05.041 [DOI] [PubMed] [Google Scholar]
- 20. Latry P, Pinet M, Labat A, et al. Adherence to anti-inflammatory treatment for asthma in clinical practice in France. Clin Ther 2008;30:1058–68. Spec No doi:10.1016/j.clinthera.2008.06.011 [DOI] [PubMed] [Google Scholar]
- 21. Morton RW, Elphick HE, Rigby AS, et al. STAAR: a randomised controlled trial of electronic adherence monitoring with reminder alarms and feedback to improve clinical outcomes for children with asthma. Thorax 2017;72 doi:10.1136/thoraxjnl-2015-208171 [DOI] [PubMed] [Google Scholar]
- 22. Bush A, Fleming L. Is asthma overdiagnosed? Arch Dis Child 2016;101:688–9. doi:10.1136/archdischild-2015-309053 [DOI] [PubMed] [Google Scholar]
- 23. Klersy C, De Silvestri A, Gabutti G, et al. A meta-analysis of remote monitoring of heart failure patients. J Am Coll Cardiol 2009;54:1683–94. doi:10.1016/j.jacc.2009.08.017 [DOI] [PubMed] [Google Scholar]
- 24. Polisena J, Tran K, Cimon K, et al. Home telehealth for diabetes management: a systematic review and meta-analysis. Diabetes Obes Metab 2009;11:913–30. doi:10.1111/j.1463-1326.2009.01057.x [DOI] [PubMed] [Google Scholar]
- 25. Russell-Minda E, Jutai J, Speechley M, et al. Health technologies for monitoring and managing diabetes: a systematic review. J Diabetes Sci Technol 2009;3:1460–71. doi:10.1177/193229680900300628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Howard S, Lang A, Sharples S, et al. What are the pros and cons of electronically monitoring inhaler use in asthma? A multistakeholder perspective. BMJ Open Respir Res 2016;3:e000159 doi:10.1136/bmjresp-2016-000159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Federico MJ, Hoch HE, Anderson WC, et al. Asthma Management for Children: risk identification and Prevention. Adv Pediatr 2016;63:103–26. doi:10.1016/j.yapd.2016.04.010 [DOI] [PubMed] [Google Scholar]
- 28. Voorend-van Bergen S, Vaessen-Verberne AA, Brackel HJ, et al. Monitoring strategies in children with asthma: a randomised controlled trial. Thorax 2015;70:543–50. doi:10.1136/thoraxjnl-2014-206161 [DOI] [PubMed] [Google Scholar]
- 29. Zhao J, Zhai YK, Zhu WJ, et al. Effectiveness of Telemedicine for Controlling Asthma Symptoms: a systematic review and Meta-analysis. Telemed J E Health 2015;21:484–92. doi:10.1089/tmj.2014.0119 [DOI] [PubMed] [Google Scholar]
- 30. Kenyon CC, Chang J, Wynter SA, et al. Electronic adherence monitoring in a High-Utilizing Pediatric Asthma Cohort: a Feasibility Study. JMIR Res Protoc 2016;5:e132 doi:10.2196/resprot.5362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Vasbinder EC, Goossens LM, Rutten-van Mölken MP, et al. e-Monitoring of Asthma therapy to improve compliance in children (e-MATIC): a randomised controlled trial. Eur Respir J 2016;48:758–67. doi:10.1183/13993003.01698-2015 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjresp-2017-000204supp001.pdf (53.6KB, pdf)