Abstract
Concussion is a heterogeneous injury occurring throughout a range of impact magnitudes. Consequently, research focusing on a single or set of variables at the time of injury to understand concussive biomechanics has been thwarted by low injury prediction sensitivity. The current study examined the role of Impact Density in estimating concussive injury risk. Head impact data were collected across seven high school football seasons with the Head Impact Telemetry System (HIT System). Over the study period, 29 concussions were included for data analysis. The linear acceleration of the concussive impact was matched to a Control athlete, along with impacts in the 24 h before. Linear and rotational acceleration for the 19 impacts leading into the final event and the cumulative accelerations over time were evaluated. Analyses indicated no difference in impact counts within the final 24 h, or impact magnitudes for linear and rotational acceleration among the final 20 impacts (p > 0.05). A novel metric, Impact Density, was calculated from the final 20 impacts by summing the acceleration magnitude divided by time from the previous impact. Analyses indicated the Concussed athletes incurred a significantly higher linear (concussed: 255.4g/sec (standard error of the mean [SEM] = 40.1), controls:145.4g/sec (SEM = 23.8), p = 0.016), and rotational (Concussed:10311.3 rad/s/s/s (SEM = 1883.7), Controls: 6083.8 rad/s/s/s (SEM = 1115.9), p = 0.029) Impact Density than the Control athletes. Similar to other investigations, there was no difference in individual linear or rotational impact magnitude in the 20 impacts before and including the injury. The measure of Impact Density, however, revealed differences between the Concussed and Control athletes. These data suggest that the biomechanical threshold for concussion fluctuates downwardly with a greater impact magnitude and number with a return to pre-impact levels with time, suggesting physiological vulnerability to repeated head impacts. The current results highlight that time between impacts, not just impact magnitude, influences risk for concussion.
Keywords: : concussion, head impacts, linear and rotational acceleration
Introduction
Despite growing attention and research on sport concussion, the initial identification of the injury remains one of the most challenging aspects of injury assessment and management. Early work suggested that more than 50% of high school athletes1 and 80% of collegiate athletes2 may not report their injury to a medical professional for a variety of reasons. The number of unreported concussions has decreased in the previous decade, and high school athletes now report 70% of their injuries,3 while collegiate athletes report 53%.4 Despite the improved injury disclosure, those not reporting their injuries may be playing in a state of increased vulnerability. For example, animal models indicate impacts closer in time result in longer recovery periods and more severe alterations in brain physiology.5 In humans, subsequent concussions are most likely to occur within two weeks for the first injury6 and result in prolonged recovery times relative to the first injury.7
A variety of head impact sensors have been developed and deployed clinically to not only better identify concussed athletes and expedite removal from play, but also to reduce injury risk through technique modification. To date, helmet based systems (i.e., Head Impact Telemetry System–HIT System) have been the most broadly used in the literature for clinical and research purposes.8 The HIT System has defined the mean number of head impacts among high school9 and collegiate10 football athletes, and several attempts have been made to identify a single variable or set of variables that would permit real time concussion diagnostics using biomechanical measures.11–13 Despite multiple attempts to define diagnostic criteria using biomechanical properties, the concussion threshold remains elusive.14
While often excoriated, the first attempt in the modern era to define the concussion threshold was completed using Hybrid III mannequin reconstruction of 25 National Football League level impacts that resulted in concussion.15 The authors indicated that impacts resulting in a linear head acceleration of 70 to 75 was sufficient to result in concussion, although the mean linear acceleration of their data was 98g. The mean acceleration of 98g compares well to 13 high school level concussion recorded using the HIT System whereby the mean linear acceleration was 105g.11 In that same data however, four of the 13 concussions fell below the 98g mark, and the overall sensitivity was 3.5%, minimizing the clinical utility of that value. Greenwald and associates12 later developed a weighted principal component score including linear acceleration, rotational acceleration, head injury criterian, and impact location. Application of this algorithm to a high school dataset, however, yielded only 6% sensitivity.11 Last, a Classification and Regression Tree analysis incorporating linear and rotational acceleration values and impact location associated were applied to high school level concussions; sensitivity improved, but was still below the level of clinical utility.11
The inability to define a concussion threshold is likely multi-factorial. First, intrinsic factors such as hydration and energy status, cerebral blood flow, cerebral spinal fluid volume, and others16 are sufficiently variable both between and within athletes to blur the threshold line. In addition, statistical analyses most commonly implement measures of central tendency when defining the injury threshold, even though an impact exceeding a theoretical threshold by 1g results in the concussion being classified and analyzed the same as an impact exceeding by 20g.17 In addition, others have noted that head impacts among concussed athletes on the day of injury are greater in both magnitude and frequency relative to those without concussion.18 Indeed, in an investigation of 95 concussed athletes, those sustaining a concussion sustained nearly triple the number of impacts and the highest magnitude impact was 20g greater than on non-concussive days.18 This finding suggests that the final “smoking gun” impact may only explain partly the clinical presentation of concussion and that the threshold for injury may be influenced by previous impacts and their temporal distribution. As such, the purpose of this exploratory investigation is to further evaluate the relationship between head impact exposure preceding a concussive event.
Methods
As part of an ongoing investigation on head impact biomechanics in high school football athletes, 185 participants (16.3 [0.8] years; 180.8 [8.1) cm; 85.0 (18.3] kg; 0.3 [0.7] previous concussions reported) were recruited from three high schools between 2007 and 2014 (School 1, n = 94, 2007–2011; School 2, n = 50, 2011–2013; School 3, n = 41, 2013–2014). At the time of enrollment, all participants were fitted with a new or newly refurbished Riddell Revolution or Revolution Speed helmet that was equipped with a HIT System encoder. Participants were equipped with head impact measurement technology during normal participation in football practices (n = 373) and games (n = 94), without intervention from the study team. All participants and their parent/guardian provided written informed assent/consent at the time of enrollment in a manner that was consistent with the host institution's office of Human Subjects.
HIT system
Described elsewhere in detail,19,20 the HIT System (Simbex LLC, Lebanon, NH) implements six-axis accelerometers to estimate head center of mass acceleration after impact. Accelerations are continually monitored at 1 kHz until any unfiltered/unprocessed data from a single accelerometer meets or exceeds 14.4g. At this point, the 8 msec before the threshold and 32 msec after the threshold point are stored locally or transmitted to the sideline computer.
For each impact, algorithms filtered impact profiles known to be associated with aberrant impacts (e.g., dropped or thrown helmet), and an investigator present at all sessions marked additional errant impacts not captured by the software. Valid impacts were processed, and the three-dimensional vector sum for linear acceleration and the estimated two-dimensional rotational acceleration were calculated. Data were then filtered to exclude linear accelerations <10g, which are thought to be associated with common athletic maneuvers.19,21 Data collected from 2013 on included a rotational acceleration estimate correction,22 which was applied to all previous data before analyses. A review of the measurement properties of the HIT System was completed by Patton.23
Concussion diagnosis
Throughout the study period, a certified athletic trainer was present at all games and practices. In the event a participant sustained a blow to the head that resulted in signs and symptoms consistent with concussion, a full sideline evaluation was completed. If the athletic trainer deemed the injury to be a concussion, the athlete was removed from further play and referred to the supervising physician for injury diagnosis. The impact resulting in the concussion was marked for later analysis. In cases where the athlete did not immediately display concussive signs and symptoms (i.e., delayed reporting), the athletic trainer referred the athlete to the physician and worked with the athlete and coaching staff to identify the impact most likely associated with concussion.
Data analysis
Before analysis, head impact data were cleaned by eliminating any outliers, defined by impacts above 200g (n = 10,683) and removal of one athlete who fell outside of three standard deviations from the group mean for time between impacts.
To evaluate the relationship between impact magnitude and time relative to concussion, 31 concussive impacts identified during the study period were extracted. Control athletes were identified by matching to the following characteristics from the concussed athlete: number of impacts before the final impact (i.e., concussive impact), final impact linear acceleration, final impact rotational acceleration, final impact location, athlete position, athlete team (see Table 1). Among the matched pairs, one participant served as both a concussed and control and four participants functioned as controls in two instances. This matching approach is supported by Wacholder and coworkers.24 Chi-square analysis for position (linemen vs. skill) indicated equivalent dispersion between Concussed and Control groups (χ2 [1] = 2.51, p = 0.113). The concussive and matched non-concussive impacts are referenced as the “final impact” or impact “0” in Figures. To evaluate for head impact exposure over time, the 19 impacts before the final impact and those occurring within the 24 h before were also extracted for analyses.
Table 1.
Descriptive Data for Linear and Rotational Acceleration of Final Impact and Number of Impacts before Occurring in the Same Season
| Concussed | Controls | |||||
|---|---|---|---|---|---|---|
| Pair | Same season impacts before | Final impact: linear acceleration (g) | Final impact: rotational acceleration (rad/s/s) | Same season Impacts before | Final impact: linear acceleration (g) | Final impact: rotational acceleration (rad/s/s) |
| 1 | 195 | 122 | 4859.7 | 207 | 125.5 | 4943.6 |
| 2 | 326 | 102.6 | 3819.4 | 352 | 102.6 | 6517.6 |
| 3 | 479 | 130.6 | 5468.4 | 562 | 131 | 8202.4 |
| 4 | 284 | 111.3 | 6510.2 | 325 | 110.8 | 6750.6 |
| 5 | 593 | 107.6 | 4538.9 | 658 | 107.6 | 2425.8 |
| 6 | 366 | 116.2 | 4543.3 | 382 | 114.3 | 6097.3 |
| 7 | 346 | 97.6 | 5835.7 | 397 | 97.8 | 6123.6 |
| 8 | 324 | 72.1 | 4580.9 | 348 | 72.1 | 3148 |
| 9 | 82 | 114.4 | 2269.7 | 97 | 114.1 | 2931.6 |
| 10 | 194 | 74 | 4940.6 | 195 | 74 | 1379.6 |
| 11 | 223 | 99.1 | 5471.3 | 262 | 99.4 | 5857.4 |
| 12 | 158 | 100.9 | 5450.7 | 181 | 100.7 | 2859 |
| 13 | 165 | 85.3 | 3332 | 173 | 85.2 | 4533.1 |
| 14 | 72 | 52.7 | 3191.4 | 78 | 52.7 | 1446.6 |
| 15 | 273 | 146 | 4056.7 | 297 | 142.1 | 929.5 |
| 16 | 471 | 48 | 2928.4 | 484 | 48 | 2523.2 |
| 17 | 177 | 66.5 | 3185 | 196 | 66.3 | 3868.9 |
| 18 | 388 | 52.9 | 3323.7 | 395 | 52.7 | 3054.6 |
| 19 | 127 | 102.7 | 6486.9 | 155 | 102.8 | 820.4 |
| 20 | 50 | 58.1 | 3512.8 | 51 | 58.1 | 1886.7 |
| 21 | 250 | 70.3 | 2198.6 | 264 | 70.3 | 3816.11 |
| 22 | 37 | 69.9 | 3284.5 | 50 | 69.9 | 4325.8 |
| 23 | 330 | 77.7 | 3347 | 377 | 77.3 | 3713.9 |
| 24 | 275 | 70.7 | 2416.1 | 306 | 70.8 | 3970.1 |
| 25 | 93 | 87.7 | 4495.3 | 144 | 88.3 | 2738.3 |
| 26 | 37 | 81.9 | 3885.5 | 39 | 81.9 | 5175.4 |
| 27 | 153 | 106.3 | 5376.9 | 157 | 106.3 | 6349.3 |
| 28 | 37 | 108.1 | 3355.7 | 98 | 107.8 | 2512.3 |
| 29 | 494 | 75.2 | 2120.3 | 509 | 74.7 | 792.8 |
| 30 | 87 | 80.2 | 4939.5 | 93 | 79.6 | 4174.2 |
| 31 | 498 | 72.9 | 707.4 | 506 | 73.1 | 2139.9 |
Measures of central tendency (i.e., mean and SEM) for participant demographics were calculated first for the Concussed and Control athletes, and differences between the two groups were evaluated using paired t-tests. Paired t-tests were used to compare between group effects as impacts were matched to each other. The initial evaluation of impact magnitude (i.e., linear and rotational acceleration) of the final impact and the preceding 19 impacts (20 impacts total) were multi-variable analyses of variance between the Concussed and Control groups. To account for time, impact magnitudes in the 24 h before the final impact were inspected visually on both a continuous timeline and at 15 min intervals. Impact counts between groups for the final 3 h were evaluated using paired samples t-tests, revealing a greater number of impacts among the Concussed athletes (see below). Linear and rotational acceleration Impact Density for the final impact and the 19 preceding impacts were then calculated, and group differences were estimated using paired samples t-test. All data were analyzed using SPSS v.24 statistical software, and significance was noted when p < 0.05.
Results
A total of 154,213 head impacts were captured over the duration of the investigation with 143,530 included in the analysis after the data cleaning process outlined above. At the time of enrollment, the 31 Concussed athletes were 16.2 (SEM = 0.2) years, 179.7 (SEM = 1.0) cm, 82.8 (SEM = 12.9) kg, and reported 0.9 (SEM = 0.2) previous concussions. The 31 Control athletes were 16.2 (SEM = 0.1) years, 180.2 (SEM = 1.6) cm, 92.4 (SEM = 3.8) kg, and reported 0.4 (SEM = 0.2) previous concussions. Among the Concussed and Control athletes, 53% were from the same team and 33% from the same player group.9 Paired t-test analyses indicated no significant demographic differences for age, height, and previous concussions (p > 0.05), but the Control group was significantly heavier than the Concussed (t = −2.26, p = 0.03) with a mean difference of 10 kg.
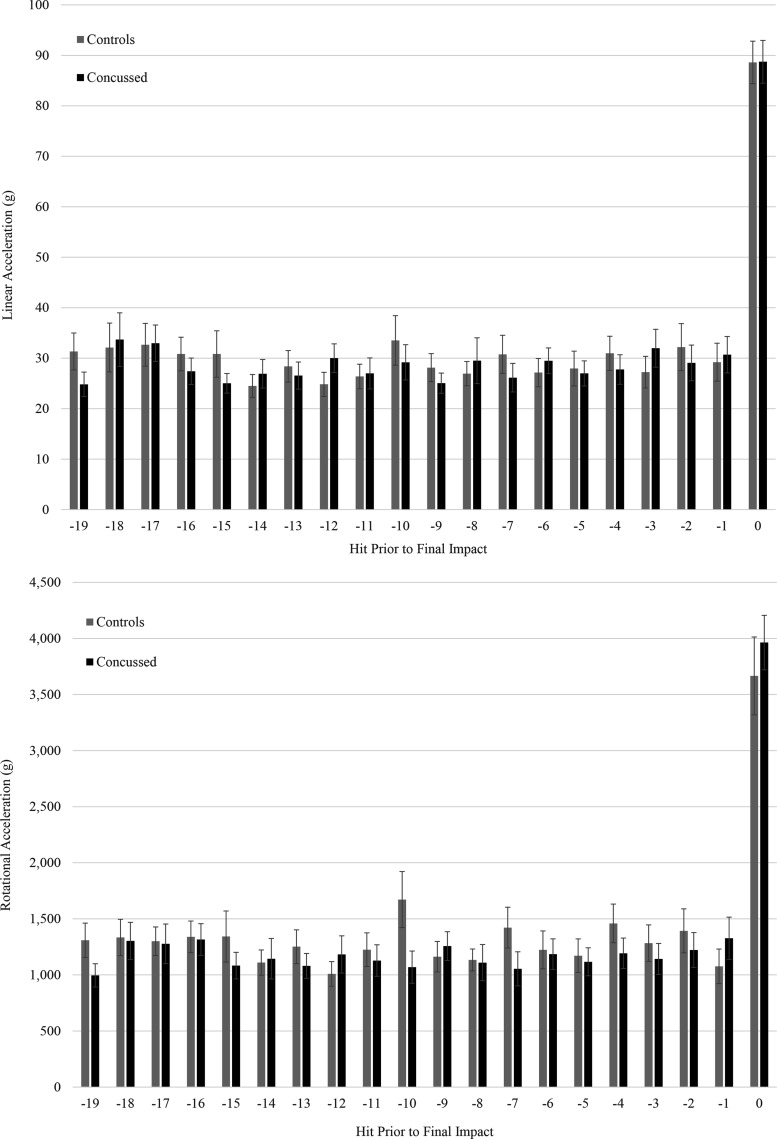
Table 1 presents each of the 31 matched concussive and non-concussive final impacts. Athletes with a diagnosed concussion sustained 21.9 (SEM = 2.7) impacts in the 24 h before injury with a final impact magnitude of 24.81 (SEM = 2.4)g and 995.60 (SEM = 103.99) rad/s/s. Non-concussed Control athletes sustained 19.7 (SEM = 2.8) impacts in the 24 h before injury with a final impact magnitude of 29.25 (SEM = 3.40)g and 1241.45 (SEM = 143.90) rad/s/s. There was no significant difference in the number of impacts sustained by the Concussed and Control athletes in the 24 h before the final impact (t = 0.58, p > 0.05). Multivariable analysis of variance indicated no significant differences between groups for linear (F = 0.146, p > 0.05) or rotational acceleration (F = 1.066, p > 0.05) magnitude for the final impact or the 19 preceding impacts (Fig. 1).
FIG. 1.
Mean and standard error for linear (top) and rotational (bottom) acceleration for the final impact (“0”) and the 19 previous impacts. There are no differences in magnitude between the Concussed and Control groups for any given impact.
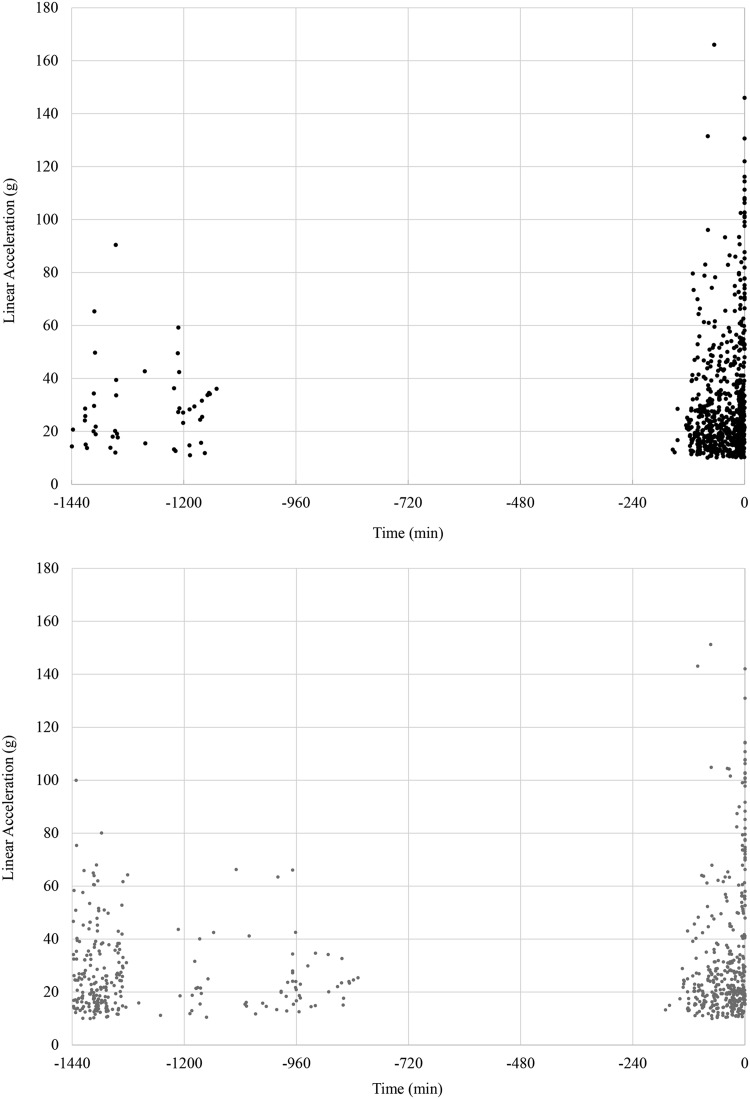
Because no differences in impact magnitudes were noted for the final impact or 19 preceding impacts, all impacts occurring in the 24 h before were plotted over time (Fig. 2). Visual inspection suggested a higher number of impacts among the Concussed athletes in the 3 h before injury (i.e., the final impact labeled as Time 0).
FIG. 2.
Differences in Impact Density between concussed (top) and matched controls (bottom) over the 24 h before the final impact. Magnitude (i.e., linear acceleration) is displayed on the vertical axis and time on the horizontal axis with the final impact indicated at time “0”.
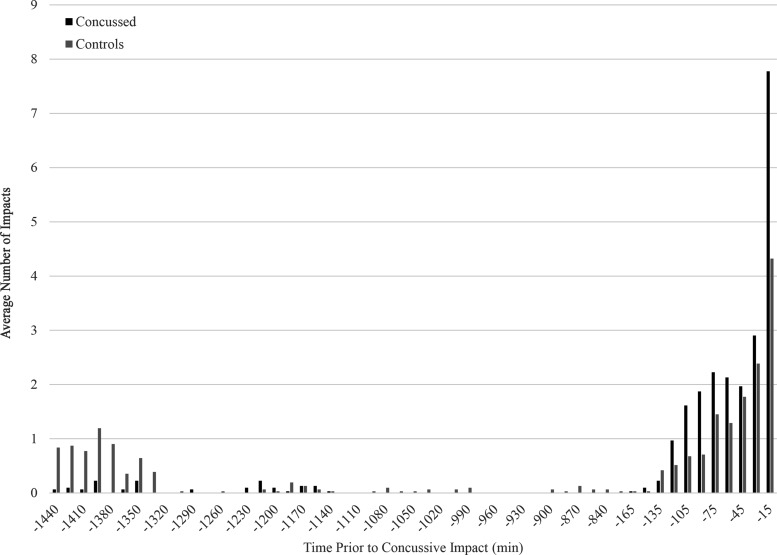
Given the lack of significant difference in the 24 h hit count relative to the impact distribution shown in Figure 2, hit counts in 15 min bins for the 24 h before the concussive impact were graphed for each group (Fig. 3). Analysis of hit counts between the Concussed and Control groups in the final 180 min indicated the Concussed athletes sustained significantly more head impacts than the Controls (Concussed: 20.5 (SEM = 2.8), Control: 12.8 (SEM = 2.0), t = 2.25, p = 0.03).
FIG. 3.
Mean number of impacts per athlete every 15 min in the 24-h period before the final impact.
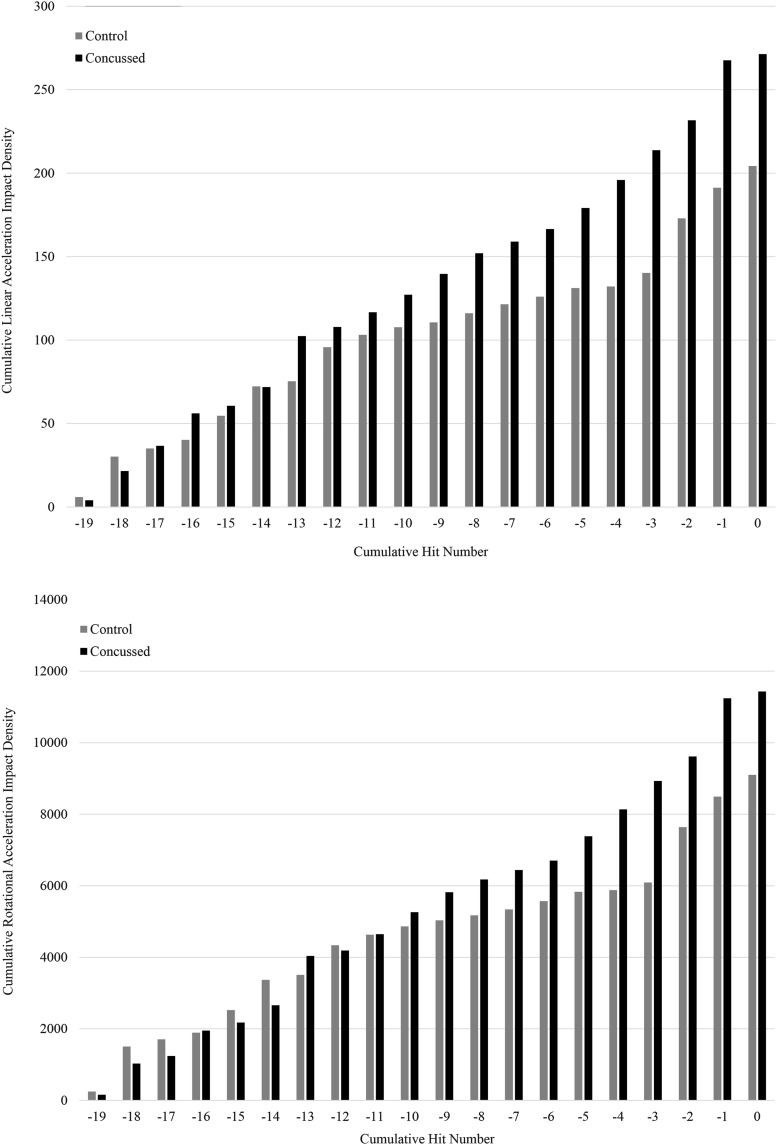
Noting the significantly higher number of impacts among the Concussed athletes in the 3 h before the final impact, we hypothesized that differences between groups would be visible when impact magnitude was adjusted for time before the previous impact. A new variable called Impact Density was created by summing the magnitude of a given impact divided by the time from the previous hit for each of the 20 impacts (see Equation below).
 |
Impact Density was calculated for both linear and rotational acceleration and plotted in Figure 4. Paired sampled t-tests were conducted to compare differences Impact Density for linear and rotational acceleration between groups. Results showed that Concussed subjects showed significantly higher linear (Concussed: 255.4g/sec (SEM = 40.1), Controls:145.4g/sec (SEM = 23.8), p = 0.016), and rotational (Concussed: 10311.3 rad/s/s/s (SEM = 1883.7), Controls: 6083.8 rad/s/s/s (SEM = 1115.9), p = 0.029) acceleration Impact Density values over time relative to Controls.
FIG. 4.
Cumulative linear (top) and rotational (bottom) acceleration Impact Density displayed for the final impact and the 19 preceding impacts. Impact Density for the final impact (i.e., impact 0) represents the sum of all previous impacts for linear or rotational acceleration sum divided by the time from the previous impact. Impact Density was higher among the Concussed athletes for both linear and rotational acceleration.
Discussion
Our current interpretation of concussion risk assumes the injury is associated with a singular impact, independent of any previous impacts.13 As such, previous attempts to identify a concussive injury threshold using impact biomechanics have focused largely on a single or set of variables related to a smoking gun impact.11,12,15 Each of these attempts has moved our understanding of concussion biomechanics closer to defining the threshold, but has fallen short of developing an algorithm suitable for clinical utility.14 While it might seem naïve to assume impacts to a biological system (i.e., cerebral tissue) are independent of each other, previous evidence suggests no cumulative mechanism for increasing concussive injury risk.16 Thus, this single impact estimate failed to meet clinical utility because 26 of the 30 concussive impacts in this dataset fell below the 25% injury probability and the remaining three fell below the 50% injury risk level.13
Failure to accurately define a single or set of variables associated with a concussive impact may have been associated, in part, with the exclusion of head impacts leading into the final injurious blow—meaning that repeated head impacts before the concussive impact may somehow alter the magnitude threshold at which the concussion occurs. Eckner and associates16 were the first to examine this by evaluating HIT System data from 19 athletes sustaining 20 concussions. Noting an equal number of impacts leading into the concussive and non-concussive impacts, the authors concluded that the cumulative impact burden (i.e., sum of impact magnitudes leading up to the concussive event) was no different than the impact burden for three non-concussive impacts of similar or larger magnitude within the same athlete within 30 min, same day, and one week of the final blow. The data presented here (Fig. 1) support this finding. In a similar investigation, Beckwith and colleagues18 evaluated 105 concussions that were reported immediately (n = 45) or went undiagnosed on the day of injury. Head kinematics and impact counts are from the 95 high school and collegiate football athletes documented using the HIT System.
While head impact magnitudes were greater on the day of diagnosed concussions, the authors also reported a greater number of impacts on those same days. This finding is similar to the data reported here (Fig. 2), demonstrating a higher Impact Density on the day of injury relative to the Control athletes and suggests that time between impacts also warrants consideration.
Indeed, these findings lead us to hypothesize that cumulative impact magnitude divided by time plays an important role in establishing the final injury threshold. Figure 1 and Table 1 offer support to this theory by demonstrating that impact counts and linear and rotational acceleration magnitudes do not differ between concussed and control athletes, yet the cumulative linear and rotational accelerations divided by time from the injury (Fig. 4) show significantly higher magnitudes by time among the Concussed athletes. Because impact magnitude was equal between the groups, the time between impacts for the Concussed cohort must be smaller than the non-concussed cohort. This indicates that the Concussed group sustains impacts at a higher frequency than non-concussed players.
The higher frequency of impacts is exemplified by the scatter plot analysis (Fig. 2) showing a much broader distribution of impacts over time among the Control athletes relative to the Concussed, despite the athletes being matched for an equal number of impacts. Quantification of this theory and application to larger datasets and over a greater window of time (i.e., inclusion of more impacts) is needed.
The biological underpinnings for this theory cannot be elucidated with the methodology employed here. Animal models of concussive impacts,5,25 however, suggest that each head impact not resulting in the clinical presentation of concussion results in a small, unregulated efflux of ions from the neuron. Because the cerebral tissue will always seek to maintain homeostasis, the ion pumps and other pathways will then activate to restore a normal balance over time. If there is adequate time before the next impact, homeostasis is restored, and the next ion efflux starts at the baseline level. If, however, there is not adequate time to restore homeostasis, the additional ion excursion may lower the impact magnitude at which a concussion may occur. Stated differently, each impact may alter the concussion threshold in a downward manner with time between impacts pushing the threshold back toward the baseline level (i.e., recovery).
We hypothesize that the degree to which the threshold decreases after impact is dependent on the impact magnitude, while the rapidity to which threshold returns to a pre-impact level is dependent on time. Therefore, a greater Impact Density—that is, a higher number of impacts with a shorter recovery period—places the athlete farther from baseline homeostasis
While this theory may explain some of the biomechanical properties of concussion, the neurobiopsychosocial aspects of the injury cannot be ignored.26 For example, recent work demonstrates that athletes with high somatization scores have protracted recoveries,27 leading one to speculate that these same persons may also be more likely to report injuries. In addition, intrinsic factors such as female sex,28 young age,29 mood disorders,30,31 learning disorders,32 migraine history,33 fatigue,34 and previous concussion history6 all likely play a role in concussion risk. In addition to these elements, some have also proposed that cerebral characteristics such as blood flow and cerebrospinal fluid viscosity, along with sleep deprivation, illness, and genetic profile may also influence risk,16 albeit the relationship is less clear than the other factors.
As with any investigation, this study is not without limitations. Perhaps most notable is that this investigation was limited to male athletes who play high school football and the Concussed and Control groups were not matched perfectly. The biological influence of team, position, mass, or older and younger athletes, females, and those in other sports remains unknown at this time. Similar analyses of collegiate and youth level football athletes that also broaden the analysis window (i.e., inclusion of more impacts before injury) should and could be completed using existing HIT System datasets. Impact biomechanics captured with the HIT System among female athletes is limited to ice hockey,35,36 although dermis affixed sensors have recently been implemented in collegiate37 and interscholastic soccer athletes.38
It should also be noted that the HIT System precision has been placed into question, with independent investigations indicating a wide range of measurement properties.23 Indeed, one investigation reported a mean absolute percentage error of 32 ± 43% for linear acceleration and 35 ± 36% for rotational acceleration.39 We do not contend with these findings, but the HIT System is currently the most robust in measuring head kinematics in football athletes. In addition, we would expect any system's error to be equally distributed between the Concussed and Control athletes evaluated in this investigation, indicating an unlikely revision of findings as head impact monitoring systems improve in the coming years.
Last, despite the best efforts of investigators and athletic organizations, it is highly likely that a number of concussions went unreported over the duration of investigation. This concern may have resulted in the exclusion of some concussive impacts from the analysis, but all of those that were included were physician confirmed injuries.
Conclusions
Concussion researchers investigating head impact biomechanics have spent the previous decade pursuing a single or array of variables to identify concussed athletes in real time. The majority of these efforts have focused on the kinematic profile of an individual smoking gun impact, failing to account for time and biological underpinnings of injury. Findings from this investigation support the notion that magnitude of the injurious blow and those preceding it, along with time influence the threshold for concussion. To that end, greater head Impact Density (i.e., higher number and magnitude of impacts over time) appears to increase concussion risk by failing to allow for the cerebral tissue to return to pre-impact status between blows. As such, when two athletes sustain a similarly large impact (e.g., 100g), the one with greater head Impact Density is more likely to have a diagnosis of concussion.
To reduce the risk of concussion, some have called for athletes to have a “hit count” similar to a pitch count in baseball.40 In light of the current results, a simple hit count may not be sufficient to limit concussion risk. Instead, an Impact Density measure may be more appropriate to attenuate head impact exposure by allowing athletes to recover sufficiently after sustaining an impact.
Finally, while the proposed density theory may help explain why some athletes become concussed and others do not after an equivalent blow, it is not a diagnostic algorithm. Until such time as a diagnostic measure is developed and validated, well-trained medical professionals with adept clinical skills are the gold standard in injury identification and management and should be present at all athletic sessions to monitor athlete health and safety.
Acknowledgments
The authors would like to thank the football players and staff of Unity High School (Tolono, IL), Skyline High School (Ann Arbor, MI), and Father Gabriel Richard High School (Ann Arbor, MI) for their support of this project. In addition, we thank Douglas Martini, PhD, and Richelle Williams, PhD, ATC, for their assistance. The project was supported partly by The National Institutes of Health: National Institute of Neurological Disorders and Stroke (1R15NS081691-01).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.McCrea M., Hammeke T., Olsen G., Leo P., and Guskiewicz K. (2004). Unreported concussion in high school football players: implications for prevention. Clin. J. Sport Med. 14, 13–17 [DOI] [PubMed] [Google Scholar]
- 2.Sefton J.M., Pirog K., Capitao A., Harackiewicz D., and Cordova M.L. (2004). An examination of factors that influence knowledge and reporting of mild brain injuries in collegiate football. J. Athl. Train. 39, S52–S53 [Google Scholar]
- 3.LaRoche A.A., Nelson L.D., Connelly P.K., Walter K.D., and McCrea M.A. (2016). Sport-related concussion reporting and state legislative effects. Clin. J. Sport Med. 26, 33–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kroshus E., Garnett B., Hawrilenko M., Baugh C.M., and Calzo J.P. (2015). Concussion under-reporting and pressure from coaches, teammates, fans, and parents. Soc. Sci. Med. 134, 66–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prins M.L., Alexander D., Giza C.C., and Hovda D.A. (2013). Repeated mild traumatic brain injury: mechanisms of cerebral vulnerability. J. Neurotrauma 30, 30–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guskiewicz K.M., McCrea M., Marshall S.W., Cantu R.C., Randolph C., Barr W., Onate J.A., and Kelly J.P. (2003). Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA Concussion Study. JAMA 290, 2549–2555 [DOI] [PubMed] [Google Scholar]
- 7.Vagnozzi R., Signoretti S., Cristofori L., Alessandrini F., Floris R., Isgro E., Ria A., Marziale S., Zoccatelli G., Tavazzi B., Del Bolgia F., Sorge R., Broglio S.P., McIntosh T.K., and Lazzarino G. (2010). Assessment of metabolic brain damage and recovery following mild traumatic brain injury: a multicentre, proton magnetic resonance spectroscopic study in concussed patients. Brain 133, 3232–3242 [DOI] [PubMed] [Google Scholar]
- 8.O'Connor K.L., Rowson S., Duma S., and Broglio S.P.(in press). Systematic review of head impact biomechanics and measurement devices. J. Athl. Train. DO YOU MEAN: O'Connor K.L., Rowson S., Duma S., and Broglio S.P. (2017). Head-impact measurement devices: a systematic review. J. Athl. Train. 52, 206_227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Broglio S.P., Eckner J.T., Martini D., Sosnoff J.J., Kutcher J.S., and Randolph C. (2011). Cummulative head impact burden in high school football. J. Neurotrauma 28, 2069–2078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crisco J.J., Wilcox B.J., Beckwith J.G., Chu J.J., Duhaime A.C., Rowson S., Duma S.M., Maerlender A.C., McAllister T.W., and Greenwald R.M. (2011). Head impact exposure in collegiate football players. J. Biomech. 44, 2673–2678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Broglio S.P., Schnebel B., Sosnoff J.J., Shin S., Feng X., He X., and Zimmerman J. (2010). Biomechanical properties of concussions in high school football. Med. Sci. Sport Exerc. 42, 2064–2071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greenwald R.M., Gwin J.T., Chu J.J., and Crisco J.J. (2008). Head impact severity measures for evaluating mild traumatic brain injury risk exposure. Neurosurgery 62, 789–798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rowson S., and Duma S.M. (2013). Brain injury prediction: assessing the combined probability of concussion using linear and rotational head acceleration. Ann. Biomed. Eng. 41, 873–882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guskiewicz K.M., and Mihalik J.P. (2011). Biomechanics of sport concussion: quest for the elusive injury threshold. Exerc. Sport Sci. Rev. 39, 4–11 [DOI] [PubMed] [Google Scholar]
- 15.Pellman E.J., Viano D.C., Tucker A.M., Casson I.R., and Waeckerle J.F. (2003). Concussion in professional football: reconstruction of game impacts and injuries. Neurosurgery 53, 799–814 [DOI] [PubMed] [Google Scholar]
- 16.Eckner J.T., Sabin M., Kutcher J.S., and Broglio S.P. (2011). No evidence for a cumulative impact effect on concussion injury threshold. J. Neurotrauma 28, 2079–2090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Broglio S.P., Eckner J.T., Surma T., and Kutcher J.S. (2011). Post-concussion cognitive declines and symptomatology are not related to concussion biomechanics in high school football players. J. Neurotrauma 28, 2061–2068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beckwith J.G., Greenwald R.M., Chu J.J., Crisco J.J., Rowson S., Duma S.M., Broglio S.P., McAllister T.W., Guskiewicz K.M., Mihalik J.P., Anderson S., Schnebel B., Brolinson P.G., and Collins M.W. (2013). Head impact exposure sustained by football players on days of diagnosed concussion. Med. Sci. Sports Exerc. 45, 737–746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crisco J.J., Chu J.J., and Greenwald R.M. (2004). An algorithm for estimating acceleration magnitude and impact location using multiple nonorthogonal single-axis accelerometers. J. Biomech. Eng. 126, 849–854 [DOI] [PubMed] [Google Scholar]
- 20.Duma S.M., Manoogian S.J., Bussone W.R., Brolinson P.G., Goforth M.W., Donnenwerth J.J., Greenwald R.M., Chu J.J., and Crisco J.J. (2005). Analysis of real-time head accelerations in collegiate football players. Clin. J. Sport Med. 15, 3–8 [DOI] [PubMed] [Google Scholar]
- 21.King D., Hume P.A., Brughelli M., and Gissane C. (2015). Instrumented mouthguard acceleration analyses for head impacts in amateur rugby union players over a season of matches. Am. J. Sports Med. 43, 614–624 [DOI] [PubMed] [Google Scholar]
- 22.Rowson S., Duma S.M., Beckwith J.G., Chu J.J., Greenwald R.M., Crisco J.J., Brolinson P.G., Duhaime A.C., McAllister T.W., and Maerlender A.C. (2012). Rotational head kinematics in football impacts: an injury risk function for concussion. Ann. Biomed. Eng. 40, 1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patton D.A. (2016). A review of instrumented equipment to investigate head impacts in sport. Appl. Bionics Biomech. 2016, 7049743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wacholder S., Silverman D.T., McLaughlin J.K., and Mandel J.S. (1992). Selection of controls in case-control studies. III. Design options. Am. J. Epidemiol. 135, 1042–1050 [DOI] [PubMed] [Google Scholar]
- 25.Giza C.C., and Hovda D.A. (2014). The new neurometabolic cascade of concussion. Neurosurgery 75(Suppl 4), S24–S33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCrea M., Broshek D.K., and Barth J.T. (2015). Sports concussion assessment and management: future research directions. Brain Inj. 29, 276–282 [DOI] [PubMed] [Google Scholar]
- 27.Nelson L.D., Tarima S., LaRoche A.A., Hammeke T.A., Barr W.B., Guskiewicz K., Randolph C., and McCrea M.A. (2016). Preinjury somatization symptoms contribute to clinical recovery after sport-related concussion. Neurology 86, 1856–1863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zuckerman S.L., Kerr Z.Y., Yengo-Kahn A., Wasserman E., Covassin T., and Solomon G.S. (2015). Epidemiology of sports-related concussion in NCAA athletes from 2009-2010 to 2013-2014: incidence, recurrence, and mechanisms. Am. J. Sports Med. 43, 2654–2662 [DOI] [PubMed] [Google Scholar]
- 29.Gessel L.M., Fields S.K., Collins C.L., Dick R.W., and Comstock R.D. (2007). Concussions among United States high school and collegiate athletes. J. Athl. Train. 42, 495–503 [PMC free article] [PubMed] [Google Scholar]
- 30.Morgan C.D., Zuckerman S.L., Lee Y.M., King L., Beaird S., Sills A.K., and Solomon G.S. (2015). Predictors of postconcussion syndrome after sports-related concussion in young athletes: a matched case-control study. J. Neurosurg. Pediatr. 15, 589–598 [DOI] [PubMed] [Google Scholar]
- 31.Wood R.L., O'Hagan G., Williams C., McCabe M., and Chadwick N. (2014). Anxiety sensitivity and alexithymia as mediators of postconcussion syndrome following mild traumatic brain injury. J. Head Trauma Rehabil. 29, E9–E17 [DOI] [PubMed] [Google Scholar]
- 32.Iverson G.L., Wojtowicz M., Brooks B.L., Maxwell B.A., Atkins J.E., Zafonte R., and Berkner P.D. (2016). High school athletes with ADHD and learning difficulties have a greater lifetime concussion history. J. Atten. Disord. Epub ahead of print [DOI] [PubMed] [Google Scholar]
- 33.Gordon K.E., Dooley J.M., and Wood E.P. (2006). Is migraine a risk factor for the development of concussion? Br. J. Sports Med. 40, 184–185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stevens S.T., Lassonde M., de Beaumont L., and Keenan J.P. (2008). In-game fatigue influences concussions in national hockey league players. Res. Sports Med. 16, 68–74 [DOI] [PubMed] [Google Scholar]
- 35.Wilcox B.J., Beckwith J.G., Greenwald R.M., Chu J.J., McAllister T.W., Flashman L.A., Maerlender A.C., Duhaime A.C., and Crisco J.J. (2014). Head impact exposure in male and female collegiate ice hockey players. J. Biomech. 47, 109–114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wilcox B.J., Beckwith J.G., Greenwald R.M., Raukar N.P., Chu J.J., McAllister T.W., Flashman L.A., Maerlender A.C., Duhaime A.C., and Crisco J.J. (2015). Biomechanics of head impacts associated with diagnosed concussion in female collegiate ice hockey players. J. Biomech. 48, 2201–2204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lynall R.C., Clark M.D., Grand E.E., Stucker J.C., Littleton A.C., Aguilar A.J., Petschauer M.A., Teel E.F., and Mihalik J.P. (2016). Head impact biomechanics in women's college soccer. Med. Sci. Sports Exerc. 48, 1772–1778 [DOI] [PubMed] [Google Scholar]
- 38.McCuen E., Svaldi D., Breedlove K., Kraz N., Cummiskey B., Breedlove E.L., Traver J., Desmond K.F., Hannemann R.E., Zanath E., Guerra A., Leverenz L., Talavage T.M., and Nauman E.A. (2015). Collegiate women's soccer players suffer greater cumulative head impacts than their high school counterparts. J. Biomech. 48, 3720–3723 [DOI] [PubMed] [Google Scholar]
- 39.Siegmund G.P., Guskiewicz K.M., Marshall S.W., DeMarco A.L., and Bonin S.J. (2016). Laboratory validation of two wearable sensor systems for measuring head impact severity in football players. Ann. Biomed. Eng. 44, 1257–1274 [DOI] [PubMed] [Google Scholar]
- 40.Gregory S. (2015). Why we need hit counts in football, in: Time. Time Inc: New York, October 12 [Google Scholar]