Abstract
Cystic adventitial disease is a rare disorder that occurs in peripheral arteries. Calf claudication caused by compression of the popliteal artery is a typical presentation of this disease. This is a report of two cases of occluded popliteal artery decompression by percutaneous ultrasound-guided cyst aspiration. In both cases, decompression of the artery was achieved with a significant decrease in the size of adventitial cysts and restoration of flow. Both patients reported complete resolution of symptoms and no calf pain 5 years after the procedure. MR findings and resolution of symptoms in these two patients show the efficacy of percutaneous adventitial cyst aspiration in a 5-year follow-up.
Keywords: popliteal artery, popliteal cyst, peripheral vascular disease
Introduction
Lower extremity ischemia is a common disorder usually caused by peripheral artery disease. Adventitial cystic disease (ACD) is a very rare cause of lower extremity ischemia, affecting mainly young to middle-aged patients. Adventitial cystic disease accounts for 1:1200 calf claudication cases. It affects peripheral arteries with popliteal artery being the most common location. Calf claudication caused by compression of the popliteal artery by cysts filled with gelatinous content is a typical presentation of this disease. There is a strong male predilection. The pathogenesis of the disease includes ectopic ganglia from adjacent joint capsules. Doppler ultrasound is usually a sufficient method for adventitial cystic disease diagnosis. In selected cases, computed tomography angiography or magnetic resonance angiography can be used; digital subtraction angiography is rarely required. Although there is no consensus, many publications suggest surgical resection as the preferred treatment of ACD(1–4). It is also believed that aspiration “is not suitable for the treatment of cases with total occlusion of the popliteal artery, which require vascular reconstruction”(3). This report features two cases of cystic adventitial disease treated with decompression of the popliteal artery by percutaneous ultrasound-guided cyst aspiration.
Materials and methods
Patient 1
An 80-year-old male presented to the Hospital with right calf pain when walking and tiredness, suggesting right lower extremity ischemia. Claudication distance was 200 meters. Computed tomography angiography (CTA) and Doppler ultrasound of the lower extremities revealed a multilocular cyst in the right popliteal fossa compressing the popliteal artery which was occluded over a short segment (Fig. 1). The estimated volume of the cyst was 6 ml. The presence of the lobulated contour, septa in this lesion as well as only minimal atherosclerotic changes despite the patient’s advanced age were not consistent with a thrombosed aneurysm which, however, should be included in the differential diagnosis. Prior to intervention, the presence of a septated cyst occluding the popliteal artery was confirmed by ultrasound (Siemens Acuson Antares, Siemens Healthcare, Erlangen, Germany) performed in the Department of Interventional and Vascular Radiology. Then, the largest cystic area was selected while making sure to avoid puncture of the collateral vessels. After prone positioning and application of local anesthetic, the puncture of the cyst was performed with a 14 G needle under ultrasound guidance. About 4 ml of gelatinous substance was aspirated resulting in partial restoration of flow in the popliteal artery confirmed in Doppler ultrasound. Because stenosis of the artery was still present, another part of the cyst was punctured and aspirated, thereby restoring good flow in the artery (Fig. 2 and Fig. 3).
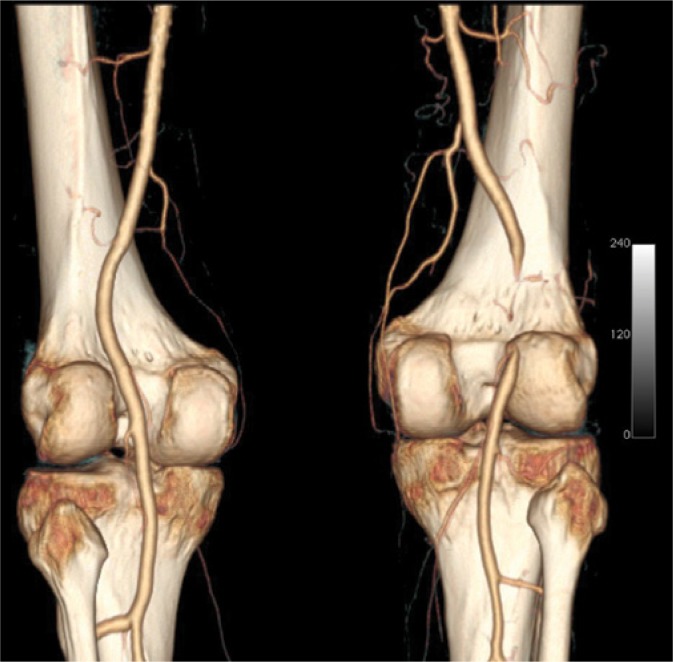
Fig. 1.
Patient 1, occlusion of the right popliteal artery – CTA, 3D reconstruction
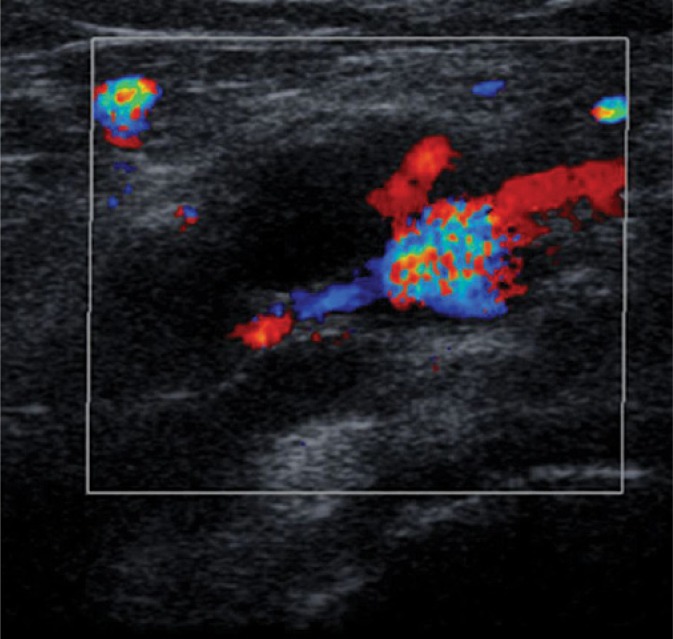
Fig. 2.
Patient 1, Doppler ultrasound, partially restored flow in the popliteal artery after the first aspiration
Fig. 3.
Patient 1, Doppler ultrasound, good flow in the popliteal artery after the second aspiration
After the procedure, palpable pulse on the dorsalis pedis artery was detected (not present before the intervention). The ankle brachial index (ABI) was 1 (0.58 before the procedure).
Patient 2
A 61-year-old male was admitted to the Hospital due to tingling sensation in the right calf and foot. Claudication distance was 500 meters. Magnetic resonance imaging (MRI) of the lower extremities demonstrated an adventitial cyst causing occlusion of the right popliteal artery (Fig. 4).
Fig. 4.
Patient 2. A fat suppressed PD-weighted TSE MR image demonstrates an adventitial cyst causing occlusion of the right popliteal artery (arrow)
The estimated volume of the cyst measured on T2-weighted images was 7 ml. The cyst was punctured with a 14 G needle in the manner mentioned above. Initially, only a small amount of gelatinous substance was aspirated, and therefore additional punctures of the cyst were performed at different sites. In total, less than 4 ml of gelatinous substance was aspirated. The flow in the popliteal artery was restored, but the pulse on the foot was weak. After the procedure, ABI was 0.85 (0.5 before the procedure). In both patients, early postprocedural ultrasound examinations revealed the presence of residual cysts.
In both cases, follow-up was conducted with MRI (Siemens Magnetom Avanto 1.5T, Siemens Healthcare, Erlangen, Germany) fourteen months after the procedure in patient 1 and eleven months after the procedure in patient 2. The following sequences were used: PD TSE FS axial, sagittal and coronal, T1 TSE axial, sagittal and coronal, TOF 3D, PC 3D, T2 TIRM coronal, T2 TSE sagittal. No intravenous contrast was given. In patient 1, no residual cyst was shown on follow-up MR examination, whereas in patient 2 MRI revealed 0.5 ml residual cystic structures next to the artery, markedly hyperintense on T2-weighted images and on fat suppressed PD-weighted TSE MR images (Fig. 5).
Fig. 5.
Patient 2, 11 months after aspiration. A small residual cyst (arrow) is seen on a fat suppressed PD-weighted TSE MR image
There was no recurrent stenosis of the popliteal artery in patient 1, while in patient 2 follow-up MRI depicted residual stenosis caused by a band of tissue. Despite the suboptimal result in patient 2, a significant shrinkage of the cyst was noted. The next follow-up assessment was done in both patients 5 years after aspiration. In patient 1, MRI showed no residual cyst, which was similar to the previous study done 1 year after aspiration (Fig. 6).
Fig. 6.
Patient 1, fat suppressed PD-weighted TSE MRI showed no residual cyst 5 years after aspiration
In patient 2, MRI showed a residual cyst of a similar size to the previous examination and no significant compression of the artery. Doppler ultrasound (Toshiba Aplio 500, Toshiba Medical Systems, Otawara, Japan) showed good flow in the popliteal arteries in both patients 5 years after the procedures (Fig. 7). In both cases, the patients presented with no claudication and no other clinical symptoms of popliteal artery stenosis during follow-up.
Fig. 7.
Patient 2, Doppler ultrasound, good result still visible 5 years after the procedure
Discussion
Adventitial cystic disease, along with trauma or entrapment syndrome, belong to non-atherosclerotic causes of arterial stenosis or occlusion. The etiology of adventitial cystic disease is not clear. According to the majority of authors, cystic adventitial degeneration may represent ectopic ganglia from adjacent joint capsules(5,6). Adventitial cysts are usually treated surgically, and US- or CT-guided aspiration is an alternative method of treatment, but the reported efficacy of these interventional techniques is ambiguous(7–9).
In the presented material consisting of two patients, surprisingly the decrease in the volume of the cysts significantly exceeded the amount of gelatinous substance that was actually aspirated. In both patients, ultrasound examinations showed restoration of flow immediately after aspiration, which was the main goal of the procedure. Follow-up MRI revealed that the treated cysts had almost disappeared. These findings probably correspond with leakage of the cystic content into the soft tissues through multiple puncture sites. Spontaneous resolution of adventitial cystic disease has been previously reported(10). The results of the treatment suggest that percutaneous aspiration of adventitial cysts is a safe and efficient method of treatment and facilitates restoration of flow in the affected vessel. Early recurrence suggested by some authors(11,12) is not confirmed by the treatment results in the reported cases. Furthermore, aspiration of even small amount of gelatinous content, especially through several puncture sites, may be sufficient despite unsatisfactory early postprocedural effect demonstrated in imaging. Potential complications include hematoma, possible infection at the site of puncture, and pseudoaneurysm of the artery. MRI, due to its excellent soft-tissue resolution and multiplanar imaging capability, proved to be a very effective method of follow-up in patients who underwent percutaneous aspiration of adventitial cysts. MRI enables not only detailed evaluation of the cyst morphology, size and relationship with vascular and articular structures, but also facilitates assessment of flow in the popliteal artery(13). Even though MRI gives more details on the surrounding structures, ultrasound with Doppler seems to be a reliable method to assess treatment results. The correlation between ABI and distance of claudication was poor, especially in patient 2. The reasons for this can be possibly explained by a different occlusion mechanism and normal arteries in other segments. It is worth noting that the occlusion (in the position of examination) of the popliteal artery is limited to the level of cystic changes, whereas atherosclerotic occlusion affects a longer segment between major vessel branches (acting as bridging vessels).
Conclusion
Ultrasound-guided percutaneous aspiration can be considered as an alternative treatment in patients with adventitial cystic disease, especially in elderly patients. This relatively minimally invasive procedure gives a chance for a major decrease in the cyst size along with restitution of flow in the popliteal artery and long-term resolution of clinical symptoms, without a risk of serious complications related to surgical reconstruction. In the case of insufficient improvement of flow in the popliteal artery after this procedure, surgery remains the subsequent therapeutic option.
Conflict of interest
None of the authors have financial relationships or conflicts of interest.
References
- 1.Baxter AR, Garg K, Lamparello PJ, Mussa FF, Cayne NS, Berland T. Cystic adventitial disease of the popliteal artery: is there a consensus in management? Vascular. 2011;19:163–166. doi: 10.1258/vasc.2010.cr0233. [DOI] [PubMed] [Google Scholar]
- 2.Del Canto Peruyera P, Vázquez MJV-V, Velasco MB, Álvarez PC, Salgado AÁ, Álvarez JC, et al. Cystic adventitial disease of the popliteal artery: two case reports and a review of the literature. Vascular. 2015;23:204–210. doi: 10.1177/1708538114541652. [DOI] [PubMed] [Google Scholar]
- 3.Igari K, Kudo T, Toyofuku T, Inoue Y. Surgical treatment of cystic adventitial disease of the popliteal artery: five case reports. Case Rep Vasc Med. 2015;2015:1–6. doi: 10.1155/2015/984681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Motaganahalli RL, Smeds MR, Harlander-Locke MP, Lawrence PF, Fujimura N, DeMartino RR, et al. A multi-institutional experience in adventitial cystic disease. J Vasc Surg. 2016;65:157–161. doi: 10.1016/j.jvs.2016.08.079. [DOI] [PubMed] [Google Scholar]
- 5.Ortmann J, Widmer MK, Gretener S, Do DD, Willenberg T, Daliri A, et al. Cystic adventitial degeneration: ectopic ganglia from adjacent joint capsules. VASA Zeitschrift für Gefässkrankheiten. 2009;38:374–377. doi: 10.1024/0301-1526.38.4.374. [DOI] [PubMed] [Google Scholar]
- 6.Warhadpande S, Go MR, El Sayed H, Satiani B, Vaccaro PS. Popliteal artery cystic adventitial disease: early lessons in treatment. Ann Vasc Surg. 2017;38:255–259. doi: 10.1016/j.avsg.2016.05.112. [DOI] [PubMed] [Google Scholar]
- 7.Holden A, Merrilees S, Mitchell N, Hill A. Magnetic resonance imaging of popliteal artery pathologies. Eur J Radiol. 2008;67:159–168. doi: 10.1016/j.ejrad.2007.06.015. [DOI] [PubMed] [Google Scholar]
- 8.Do DD, Braunschweig M, Baumgartner I, Furrer M, Mahler F. Adventitial cystic disease of the popliteal artery: percutaneous US-guided aspiration. Radiology. 1997;203:743–746. doi: 10.1148/radiology.203.3.9169698. [DOI] [PubMed] [Google Scholar]
- 9.Seo H, Fujii H, Aoyama T, Sasako Y. A case of adventitial cystic disease of the popliteal artery progressing rapidly after percutaneous ultrasound-guided aspiration. Ann Vasc Dis. 2014;7:417–420. doi: 10.3400/avd.cr.14-00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pursell R, Torrie EPH, Gibson M, Galland RB. Spontaneous and permanent resolution of cystic adventitial disease of the popliteal artery. J R Soc Med. 2004;97:77–78. doi: 10.1258/jrsm.97.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sieunarine K, Lawrence-Brown MM, Kelsey P. Adventitial cystic disease of the popliteal artery: early recurrence after CT guided percutaneous aspiration. J Cardiovasc Surg (Torino) 1991;32:702–704. [PubMed] [Google Scholar]
- 12.Desy NM, Spinner RJ. The etiology and management of cystic adventitial disease. J Vasc Surg. 2014;60:235–245. doi: 10.1016/j.jvs.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Tomasian A, Lai C, Finn JP, Gelabert H, Krishnam MS. Cystic adventitial disease of the popliteal artery: features on 3T cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2008;10:38. doi: 10.1186/1532-429X-10-38. [DOI] [PMC free article] [PubMed] [Google Scholar]