Abstract
Background and Purpose
Standard operating procedures (SOP) incorporating plasma levels of rivaroxaban might be helpful in selecting patients with acute ischemic stroke taking rivaroxaban suitable for IVthrombolysis (IVT) or endovascular treatment (EVT).
Methods
This was a single-center explorative analysis using data from the Novel-Oral-Anticoagulants-in-Stroke-Patients-registry (clinicaltrials.gov:NCT02353585) including acute stroke patients taking rivaroxaban (September 2012 to November 2016). The SOP included recommendation, consideration, and avoidance of IVT if rivaroxaban plasma levels were <20 ng/mL, 20‒100 ng/mL, and >100 ng/mL, respectively, measured with a calibrated anti-factor Xa assay. Patients with intracranial artery occlusion were recommended IVT+EVT or EVT alone if plasma levels were ≤100 ng/mL or >100 ng/mL, respectively. We evaluated the frequency of IVT/EVT, door-to-needle-time (DNT), and symptomatic intracranial or major extracranial hemorrhage.
Results
Among 114 acute stroke patients taking rivaroxaban, 68 were otherwise eligible for IVT/EVT of whom 63 had plasma levels measured (median age 81 years, median baseline National Institutes of Health Stroke Scale 6). Median rivaroxaban plasma level was 96 ng/mL (inter quartile range [IQR] 18‒259 ng/mL) and time since last intake 11 hours (IQR 4.5‒18.5 hours). Twenty-two patients (35%) received IVT/EVT (IVT n=15, IVT+EVT n=3, EVT n=4) based on SOP. Median DNT was 37 (IQR 30‒60) minutes. None of the 31 patients with plasma levels >100 ng/mL received IVT. Among 14 patients with plasma levels ≤100 ng/mL, the main reason to withhold IVT was minor stroke (n=10). No symptomatic intracranial or major extracranial bleeding occurred after treatment.
Conclusions
Determination of rivaroxaban plasma levels enabled IVT or EVT in one-third of patients taking rivaroxaban who would otherwise be ineligible for acute treatment. The absence of major bleeding in our pilot series justifies future studies of this approach.
Keywords: Rivaroxaban, Stroke, Plasma levels, Thrombolysis
Introduction
Intravenous thrombolysis (IVT) with alteplase is an effective clot-eliminating treatment that improves outcome after acute ischemic stroke [1-3]. IVT carries a risk of symptomatic intracranial hemorrhage (sICH) ranging from 1.7% to up to 7.3% in the relevant trials [1,4] according to different definitions (please see methods section). Rivaroxaban is a direct factor Xa-inhibitor used for systemic oral anticoagulation in patients with atrial fibrillation [5] and other thrombo-embolic diseases. Patients receiving prior treatment with anticoagulants were excluded from all randomized controlled trials studying IVT and the decision to use IVT in patients on oral anticoagulation represents a major challenge for clinicians [6].
Observational studies showed that in patients taking vitamin K antagonists (VKA), using the international normalized ratio (INR) to select patients for IVT is safe [7,8]. Patients presenting with therapeutic INR values should not be considered for IVT, but may instead safely receive endovascular treatment (EVT) [9,10]. Measuring the anticoagulant effect of rivaroxaban using standard coagulation parameters like the INR is not recommended due to the lack of linear correlation [11-13]. Using commercially available calibrated anti-factor Xa assays, rapid measurement of drug specific plasma levels of rivaroxaban (RivLev) is feasible [14] and represents the intensity of the systemic anticoagulation effect [13]. IVT has been used in selected patients on rivaroxaban based on RivLev [15].
Upon the introduction of rivaroxaban for atrial fibrillation in Switzerland in April 2012, we established an institutional interdisciplinary standard operating procedure (SOP) at our stroke center to guide decision for the use of IVT in patients with ischemic stroke taking rivaroxaban based on RivLev. After 4 years of experience, we evaluated this SOP using data from our prospective novel oral anticoagulants in stroke patients (NOACISP) registry. In detail, we evaluated 1) the frequency of IVT/EVT used in clinical practice, 2) the door-to-needle-time (DNT), in particular, whether a DNT <60 minutes as per European Stroke Organisation (ESO) recommendations [16] was met, 3) reasons for avoiding IVT/EVT, and 4) post-treatment rate of symptomatic intracranial or major extracranial hemorrhage, good outcome, and death.
Methods
Study design, period, and population
We performed a single-center explorative analysis using data from the prospective, ongoing NOACISP registry (clinicaltrials. gov:NCT02353585) [14,17]. As defined in the NOACISP registry protocol, we prospectively collected data on all patients treated with acute ischemic or hemorrhagic stroke and prior treatment with oral anticoagulants. Data were collected at baseline and after 3 months by trained and certified stroke physicians using predefined variables and an electronical case report form as outlined in prior publications [14,17]. All data used for the present analysis were collected prospectively.
For the present analysis, we selected all patients with acute ischemic stroke presenting under rivaroxaban (defined as last intake <48 hours prior to stroke onset or intake >48 hours and elevated RivLev) treated in the Stroke Center of the University Hospital Basel from September 2012 until November 2016. This time window has been chosen as current guidelines allow the use of IVT and EVT in patients taking non-vitamin K antagonist oral anticoagulants (NOACs) with a prior intake of >48 hours and normal renal function without prior coagulation testing [18,19]. From those individuals we then selected all patients admitted within <270 minutes after symptom onset who were formally eligible for IVT/EVT apart from taking rivaroxaban.
Baseline and follow-up data
From the registry, the following baseline variables were used: age, sex, indication for the use of rivaroxaban, stroke severity as assessed by the National Institutes of Health Stroke Scale (NIHSS) [20] on admission, presence or absence of occlusion of proximal intracranial artery confirmed by computed tomography angiography or magnetic resonance angiography, INR, glomerular filtration rate applying the Chronic Kidney Disease Epidemiology Collaboration [21] equation as done in prior IVT-research [22], the risk factors of atrial fibrillation, history of stroke, hypertension, diabetes mellitus, hypercholesterolemia with criteria used previously [17,22-24], concomitant use (vs. non-use) of antiplatelets, antihypertensive drugs, and statins; dosage and time of last intake of rivaroxaban, time of symptom onset, and time of hospital admission with RivLev measurement.
Furthermore, we used prospectively ascertained data about use (or non-use) of acute recanalization treatment in the following categories: 1) IVT, 2) IVT+EVT combined, and 3) EVT alone. In patients receiving IVT (either alone or prior to EVT), the DNT was calculated.
Outcome measures include the rate of 1) any ICH seen on follow-up imaging using the radiological ECASS-2 [25] categorization (hemorrhagic infarction 1 and 2, parenchymal hemorrhage 1 and 2); 2) sICH based on the criteria of the ECASS-II1 (sICHECASS) and the NINDS [26] (sICHNINDS); 3) major extracranial hemorrhage defined as in the “Rivaroxaban Once Daily Oral Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation (ROCKET AF)” trial [5] leading to the approval of rivaroxaban for atrial fibrillation; 4) death and good (defined as modified Rankin Scale [mRS] 0−2) 3-month functional outcome assessed by structured interview at outpatient visit or telephone calls [27].
Measurement of drug specific RivLev
Venous blood samples of stroke patients were drawn at presentation to the emergency department as part of routine assessment in our stroke center and analyzed in our central lab [14]. We used a commercially available automated anti-factor Xa-based chromogenic assay with specific rivaroxaban calibrators to determine RivLev (Rivaroxaban-Screen; Hyphen-Biomed, Neuville- sur-Oise, France). The test is 24 hours and 7 days/week available in our institution and results are rapidly available before the start of IVT/EVT [14]. These results guided clinical decision. All results were later-on confirmed with a second rivaroxabancalibrated specific test (DiXal; Hyphen-Biomed).
Intravenous thrombolysis, endovascular treatment, and standard operating procedure
At our institution, IVT is used according to current guidelines [19] except that prior intake of rivaroxaban is not an absolute exclusion criterion but use is possible depending on rivaroxaban plasma levels, as defined in a SOP (Supplementary Figure 1). All patients eligible for IVT with proximal intracranial vessel occlusion are considered for EVT with mechanical stent retriever [28]. Pure EVT might be considered based on individual decisions in patients not eligible for IVT for example due to therapeutic anticoagulation [28]. All patients or next-of-kin are informed in the emergency situation about risk and benefits of IVT/EVT and can refuse treatment.
In 2012, our multidisciplinary stroke center steering group, advised by a diagnostic hemostasiologist, had agreed upon a SOP for the use of IVT in patients with acute ischemic stroke taking rivaroxaban. RivLev was a key selection criterion, in patients otherwise eligible to IVT. We defined thresholds of RivLev retrieved from literature [29] and based on theoretical considerations (Figure 1) [30].
Figure 1.
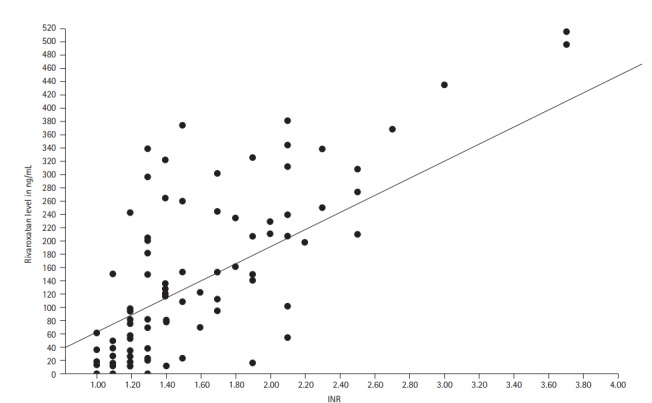
Distribution of rivaroxaban plasma level and international normalized ratio (INR).
To summarize, IVT was recommended in patients with RivLev <20 ng/mL (RivLevlow); this level is the lowest trough level of rivaroxaban measured in patients receiving prophylactic anticoagulation (24 hours after intake of 10 mg) and was considered to be clinically safe. Patients with RivLev of 20−100 ng/mL (RivLevintermediate) should be considered for IVT after balancing individual benefits and risk. In patients with RivLev >100 ng/mL (RivLevhigh), IVT should be avoided because this level represents an efficient systemic anticoagulation effect; these patients should be considered for pure EVT if otherwise eligible (i.e., have proximal vessel occlusion). The SOP was made available to all members of the stroke team involved in the selection of patients for IVT or EVT.
By review of patients’ charts and record an experienced rater (D.S.) evaluated reasons for non-adherence to the SOP, in particular, the reasons for non-use of IVT although this treatment has been recommended or considered. Criteria for the latter include mild, non-disabling stroke (NIHSS≤4), severe comorbidities, advanced age, and refusal of patients or relatives.
Statistics
We performed explorative statistics analyzing the correlation of RivLev with the INR and RivLev with time since last intake of rivaroxaban using Spearman test. All tests were 2-tailed, and statistical significance was determined at α-level of 0.05. Statistical analyses were performed using SPSS version 23.0 for Windows (IBM Corp., Armonk, NY, USA).
Ethics
NOACISP was approved by the local ethics committee (“Ethikkomission Nordwest- und Zentralschweiz,” EKNZ 2014-027).
Results
Study population
During the study period of 50 months, 114 patients with acute ischemic stroke taking rivaroxaban were admitted to our stroke center. The number increased numerically over the years: 2 patients (1.8%) in 2012, 7 (6.1%) in 2013, 21 (18.4%) in 2014, 41 (36%) in 2015, and 43 (37.7%) in 2016. Out of these patients, 68 (59.6%) 1) arrived within 270 minutes after symptom onset and 2) were otherwise eligible for IVT.
In 5/68 patients, RivLev was not measured yielding a study population of 63 patients. The median age was 81 years (inter quartile range [IQR] 76‒86), 51% (n=32) were female, and the median NIHSS on admission was 6 (IQR 2‒16). Last-intake of rivaroxaban took place a median of 11 hours (IQR 4.5–18.5 hours) before admission. The daily dosage of rivaroxaban was 10 mg in 9 patients (14.3%), 15 mg in 18 (26.8%) patients, 20 mg in 32 (50.8%) patients, and 30 mg in 4 (6.3%). The majority of 75 patients (65%) took rivaroxaban for stroke prevention in atrial fibrillation. Other reasons for rivaroxaban intake were treatment of deep vein thrombosis in 10 patients (9%), pulmonary embolism in 13 patients (11%), prevention of thrombosis after surgery in 6 patients (5%), and others/not known in 10 patients (9%).
RivLev
Among the 63 patients included in the analysis, median RivLev was 96 ng/mL (IQR 18−259). Applying the RivLev-categories of the SOP, we observed: RivLevlow, (n=17; 27%), RivLevintermediate (n=15; 22.1%) and RivLevhigh (n=31; 45.6%). Correlation between RivLev and INR was statistical significant with a Spearman rank correlation coefficient of 0.711 (P<0.01, see Figure 1).
Distribution of time since last intake of rivaroxaban and measured RivLev in patients treated with IVT and those not treated with IVT is displayed in Figure 2. We could not find any statistically significant correlation between time since last intake and RivLev (Spearman rank correlation coefficient -0.123, P=0.25). In addition, 11 of 63 patients took the last dosage of rivaroxaban >24 hours before admission and 4 of these 11 (36%) patients had RivLevhigh.
Figure 2.
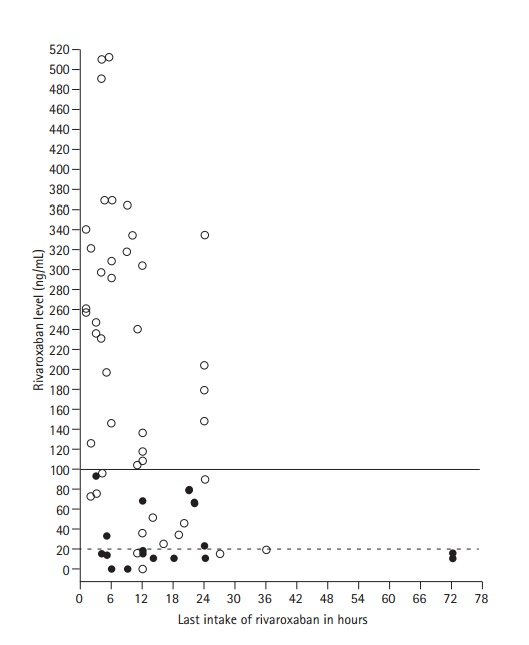
Distribution of time since last intake of rivaroxaban and measured rivaroxaban plasma levels in patients treated with intravenous thrombolysis (IVT) (●) and those not treated with IVT (○). The rivaroxaban plasma level thresholds for IVT recommended (brocken line) and IVT to-beconsedered (continuous line) are indicated.
Intravenous thrombolysis
It is noted that 18 of 63 (28.6%) patients received IVT either alone (n=15) or followed by EVT (n=3). The median DNT was 37 minutes (IQR 30‒60 minutes). All patients receiving IVT had RivLevlow (n=12) or RivLevintermediate (n=6). No patient on RivLevhigh (n=31) received IVT.
Fourteen patients with 1) RivLevlow or RivLevintermediate, and 2) absence of intracranial artery occlusions were neither treated with IVT nor with EVT. The reason for withholding IVT was mild, non-disabling stroke (NIHSS≤4) in 10 (71.4%) and severe comorbidities combined with advanced age in 4 of 14 patients (28.6%). The baseline characteristics and outcome of patients treated with IVT (alone or followed by EVT), with EVT only and those not treated with recanalization therapies are displayed in Table 1.
Table 1.
Baseline characteristics of patients on rivaroxaban treated with IVT (including IVT followed by EVT), EVT only and those receiving no recanalization therapy
| Any intravenous thrombolysis*,† (n=18) | Endovascular treatment only† (n=4) | No recanalization therapy (n=41) | |
|---|---|---|---|
| Age (years) | 77 (74–82) | 75 (70–81) | 82 (76–87) |
| Female | 11 (61) | 0 | 24 (58) |
| Prior antiplatelets | 3 (167) | 0 | 9 (22) |
| Prior statins | 9 (50) | 2 (50) | 17 (41) |
| Prior antihypertensives | 16 (89) | 4 (100) | 35 (85) |
| NIHSS on admission | 13 (7–19) | 18 (12–27) | 3 (1–6) |
| Time since last intake of rivaroxaban in hours | 12 (6–22) | 14 (7–20) | 10 (4–12) |
| Risk factors | |||
| Atrial fibrillation | 14 (78) | 2 (50) | 27 (66) |
| Diabetes mellitus | 3 (17) | 1 (25) | 10 (24) |
| Arterial hypertension | 17 (94) | 4 (100) | 34 (83) |
| Hypercholesterinemia | 10 (56) | 2 (50) | 12 (29) |
| Smoking | 0 | 0 | 4 (9.8) |
| History of stroke/TIA | 5 (28) | 0 | 13 (32) |
| Coagulation and renal function | |||
| Rivaroxaban plasma levels (ng/mL) | 15 (10–22) | 125 (102–218) | 204 (75–313) |
| INR | 1.2 (1.0–1.3) | 1.2 (1.1–1.4) | 1.5 (1.2–2.1) |
| Creatinin clearance | 63 (48–85) | 65 (61–93) | 58 (42–70) |
| RivLevlow | 12 (67) | 0 | 5 (10) |
| RivLevintermediate | 8 (33) | 0 | 9 (18) |
| RivLevhigh | 0 | 4 (100) | 27 (66) |
| Outcome | |||
| Any ICH | 2 (11) | 0 | 3 (7) |
| Hemorhagic transformation type 1 or 2 | 2 (11) | 0 | 3 (7) |
| Parenchymal hemorrhage type 1 or 2 | 0 | 0 | 0 |
| sICHNINDS | 0 | 0 | 0 |
| sICHECASS | 0 | 0 | 0 |
| mRS at 3 months | 3 (2–4) | 3 (2–4) | 3 (1–4) |
| Good outcome‡ at 3 months | 8 (44) | 1 (25) | 16 (39) |
| Death at 3 months | 3 (17) | 0 | 3 (7) |
Values are presented as median, IQR or n (%).
IVT, IV-thrombolysis; EVT, endovascular treatment; NIHSS, National Institutes of Health Stroke Scale; TIA, transient ischemic attack; INR, international normalized ratio; RivLev, plasma levels of rivaroxaban; ICH, intracranial hemorrhage; sICH, symptomatic intracerebral hemorrhage; mRS, modified Rankin Scale; IQR, inter quartile range.
Includes 3 patients receiving IVT+EVT;
Some patient data from a previously published study17 was included to allow all available data to contribute to this analysis;
Defined as mRS 0–2.
Endovascular treatment
Seven of 63 patients (11.1%) received EVT either combined with IVT (n=3, all RivLevlow or RivLevintermediate) or as pure EVT (n=4, all RivLevhigh; 12.9% of all 31 patients with RivLevhigh). Among the 27 patients with RivLevhigh not treated with EVT, 21 patients (77.8%) did not have proximal vessel occlusion eligible for EVT. Among the remaining patients, reasons not to use EVT were mild, non-disabling stroke (n=3, 9.7%, NIHSS 0, 1, and 6, respectively) and high age (n=2, 6.5%, age 88 and 92). None of the patients or next-of-kin refused treatment after being offered IVT or EVT according to SOP.
Bleeding complications, 3-month outcome, and mortality
Asymptomatic hemorrhagic transformation seen on follow-up imaging occurred in 2 patients receiving IVT (11%) and 3 patients not treated with IVT or EVT (7%). No patient treated with IVT or EVT suffered sICH or major extracranial bleeding complications. Functional outcome measured using the mRS at 3 months and proportion of patients achieving good outcome and mortality is displayed in Table 1.
Discussion
This observational study yielded the following key findings: adding RivLev for selection of patients for IVT with acute ischemic stroke on rivaroxaban 1) enabled to use IVT in 28% of patients otherwise not eligible based on current guidelines [19]; 2) patients with elevated RivLev could be triaged for pure EVT resulting in an overall rate of acute recanalization therapies in over 1/3 of patients; 3) allowed for rapid administration of IVT in a median DNT of 37 minutes and thus within the recommended delay of <60 minutes for ESO stroke centers [16]; and 4) did not yield major safety concerns.
Interestingly although the proportion of good outcome in IVT/EVT was numerically higher than in no recanalization therapy, the poor outcome or death in IVT/EVT was also numerically higher than in no IVT/EVT. We cannot provide a convincing explanation for this unexpected observation. One might speculate, that the latter group represented patients with particularly poor prognosis due to factors like poor collateral, which were not assessed in our study.
Our analysis has the following strengths: 1) all data were collected prospectively and irrespective of the current analysis. 2) We report on a long-standing, 4-year, and real-world experience from a stroke center. This implicates that our approach can be transferred to other experienced stroke centers.
Our study has the following limitations: 1) we report on a single-center experience limiting the generalizability of our findings. 2) Although we report the longest and largest singlecenter study of patients on rivaroxaban receiving IVT, the overall numbers are small and our study was not powered to prove that this approach is ultimately safe and effective. Nevertheless, our data did not raise any major safety concerns and justify the use of this approach in larger samples. 3) We did not perform detailed analysis of baseline images like the ASPECTS [31] score which can modify the bleeding risk in patients treated with IVT. 4) We could not find a significant correlation of measured RivLev with time since last intake in our study population of acute stroke patients although this has been reported previously [29,32]. There might be by other modifying factors in patients with stroke that should be analyzed in larger samples of acute stroke patients. Interestingly, we found that about one-third of patients reporting last intake of rivaroxaban >24 hours before admission had plasma levels of >100 ng/mL excluding IVT. Nevertheless, this finding underlines the importance to measure RivLev in order to assess the anticoagulant activity in individual patients.
Treatment of patients with a prior intake of oral anticoagulants has always been challenging. Overall, the off-label use of IVT in selected patients with contraindications according to the license of alteplase was not associated with poor outcome in experienced stroke centers [33]. In patients taking vitamin K antagonists and based on theoretical considerations, a subtherapeutic INR threshold of <1.7 was used to select patients for IVT but only recent large scale observational data showed this approach seems to be safe [7,8]. In analogy, the use of drug specific RivLev has been proposed to be used to select patients on rivaroxaban for IVT [15,30,34]. The used RivLev thresholds of <20 and <100 ng/mL in our SOP are based on theoretical considerations [30] and supported by data from pharmacokinetic studies [29].
First pilot data showed that IVT in patients taking NOAC including rivaroxaban was not associated with an increased risk for bleeding complications compared to patients on subtherapeutic VKA or patients without anticoagulation [17]. However, the appropriate selection criteria remain unclear and drug – specific coagulation assays in this study were only measured in 31% of patients indicating low or subtherapeutic NOAC plasma levels. In addition, a recently published study using data from a large US registry with 251 patients on NOAC treated with IVT [35], no increased bleeding risk was found neither. Unfortunately, this study did not report on drug specific NOAC plasma levels.
The aim of the current study was not to show whether IVT or EVT in patients on NOAC is safe and effective but using drugspecific plasma levels for patients’ selection is feasible. This approach offers the advantage to base the selection on drug specific plasma levels rather than on non-specific coagulation tests prone to underestimate the anticoagulant effect of NOAC [12].
The use of standard coagulation parameters like INR or activated partial thromboplastin time to evaluate the anticoagulant effect of rivaroxaban is not recommended [11]. Currently, no point-of-care (POC) device exists to reliably measure RivLev. Although, POC to measure INR has been used in patients on NOAC [36] and approaches using the INR to guide the decision for IVT in patients on rivaroxaban have been proposed [34], the correlation between INR and RivLev in patients with acute ischemic stroke is currently unclear and risk of false-negative results has been reported [12].
Our approach differs by using a more specific coagulation test. For patients on rivaroxaban who have an ischemic stroke, approaches taking into account RivLev in the decision process about the use of IVT/EVT will likely increase the rate of such patients receiving acute recanalization therapies. In particular, as recent research showed that RivLev are available within 34 minutes (median) after stroke patient entered the hospital [14]; thus early enough to guide descusion whether to use IVT or EVT.
Conclusions
Our study shows that using RivLev to select patients with acute ischemic stroke taking rivaroxaban for IVT/EVT can offer recanalization therapies to about one-third of those patients, who were not eligible for this treatment based on current guidelines. The absence of major safety concerns justifies using this approach in larger studies. Such future studies could also analyze factors influencing RivLev in patients with acute stroke.
Footnotes
Conflicts of interest and disclosures
David J. Seiffge has received funding from the Swiss Heart Foundation, the Science Funds of the University Hospital Basel, and the University of Basel and served on a scientific advisory board for Bayer and Pfizer.
Nils Peters has received travel honoraria from Boehringer-Ingelheim, honoraria for advisory board from Bayer, BoehringerIngelheim, and BMS/Pfizer, as well as funding from Bayer, Boehringer-Ingelheim, BMS/Pfizer, CSL Behring, Covidien, and Eisai.
Leo H Bonati has received funding from the Swiss National Science Foundation, the University of Basel, the Swiss Heart Foundation, and AstraZeneca; received consultancy fees from Claret Medical; received travel honoraria from Bayer and served on scientific advisory boards for Bayer.
Gian Marco De Marchis was or is supported by the following grants: Swiss National Science Foundation; Science Funds [Wissenschaftsfonds] of the University Hospital Basel and University of Basel; Bangerter-Rhyner-Stiftung; Swisslife Jubiläumsstiftung for Medical Research; Swiss Neurological Society; Fondazione Dr. Ettore Balli; De Quervain research grant; Travel honoraria by Bayer; speaker honoraria by Medtronic and BMS/Pfizer.
Raoul Sutter received research grants from the Swiss National Foundation (No 320030_169379), the Research Fund of the University Basel, the Scientific Society Basel, and the Gottfried Julia Bangerter-Rhyner Foundation. He received personal grants from UCB-pharma and holds stocks from Novartis and Roche.
The Department of Radiology, University Hospitals Basel, Switzerland, receives financial support from Bayer Healthcare, Bracco, and Guerbet and has a research agreement with SIEMENS Medical Solutions. The submitted work is not related to these agreements. C. Stippich receives no other financial support related to the submitted work.
Christian H Nickel received research support from the Science Funds [Wissenschaftsfonds] of the University Hospital Basel and the University of Basel, as well.
Philipp A. Lyrer has served on scientific advisory boards for Bayer, Daiichi-Sankyo, Schering Pharma, and Boehringer Ingelheim has received funding for travel or speaker honoraria from Bayer Schering Pharma, Boehringer Ingelheim, and Shire plc; he has received research support from AstraZeneca, Boehringer Ingelheim, Sanofi-aventis, PhotoThera, the Swiss National Science Foundation, and the Swiss Heart Foundation.
D.A. Tsakiris has received speaker honoraries and unrestricted educational grands in the past from Bayer, Boeringer Ingelheim, Pfizer.
Stefan Engelter has received funding for travel or speaker honoraria from Bayer and Boehringer Ingelheim, he has served on scientific advisory boards for Bayer, Boehringer Ingelheim, BMS/Pfizer, and Covidien and on the editorial board of Stroke. He has received an educational grant from Pfizer and research support from the Science Funds [Wissenschaftsfonds] of the University Hospital Basel, the University Basel, the Swiss Heart Foundation, and the Swiss National Science Foundation.
CT, LH, AAP, ST, BW, RG, UF, MDM, SM, and HG have no conflicts of interest.
The NOACISP registry was supported by a grant from the Swiss Heart Foundation. David J. Seiffge was supported by a fellowship for excellent young researchers from the University of Basel.
The authors have no financial conflicts of interest.
Supplementary Material
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2017.00395.
Standard operating procedure (SOP) Stroke Center University Hospital Basel for selection of patients with acute ischemic stroke taking Rivoraxoaban for treatment with intravenous thrombolysis (IVT) and endovascular treatment (EVT) based on rivaroxaban plasma levels. *Consider no IVT if mild stroke NIHSS≤4 or comorbidities; † Consider EVT if proximal vessel occlusion is present. NIHSS, National Institutes of Health Stroke Scale.
References
- 1.Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–1329. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 2.Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet. 1998;352:1245–1251. doi: 10.1016/s0140-6736(98)08020-9. [DOI] [PubMed] [Google Scholar]
- 3.IST-3 collaborative group, Sandercock P, Wardlaw JM, Lindley RI, Dennis M, Cohen G, et al. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet. 2012;379:2352–2363. doi: 10.1016/S0140-6736(12)60768-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wahlgren N, Ahmed N, Davalos A, Ford GA, Grond M, Hacke W, et al. Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet. 2007;369:275–282. doi: 10.1016/S0140-6736(07)60149-4. [DOI] [PubMed] [Google Scholar]
- 5.Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–891. doi: 10.1056/NEJMoa1009638. [DOI] [PubMed] [Google Scholar]
- 6.Hankey GJ, Norrving B, Hacke W, Steiner T. Management of acute stroke in patients taking novel oral anticoagulants. Int J Stroke. 2014;9:627–632. doi: 10.1111/ijs.12295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mazya MV, Lees KR, Markus R, Roine RO, Seet RC, Wahlgren N, et al. Safety of intravenous thrombolysis for ischemic stroke in patients treated with warfarin. Ann Neurol. 2013;74:266–274. doi: 10.1002/ana.23924. [DOI] [PubMed] [Google Scholar]
- 8.Xian Y, Liang L, Smith EE, Schwamm LH, Reeves MJ, Olson DM, et al. Risks of intracranial hemorrhage among patients with acute ischemic stroke receiving warfarin and treated with intravenous tissue plasminogen activator. JAMA. 2012;307:2600–2608. doi: 10.1001/jama.2012.6756. [DOI] [PubMed] [Google Scholar]
- 9.Nogueira RG, Smith WS, MERCI and Multi MERCI Writing Committee Safety and efficacy of endovascular thrombectomy in patients with abnormal hemostasis: pooled analysis of the MERCI and multi MERCI trials. Stroke. 2009;40:516–522. doi: 10.1161/STROKEAHA.108.525089. [DOI] [PubMed] [Google Scholar]
- 10.De Marchis GM, Jung S, Colucci G, Meier N, Fischer U, Weck A, et al. Intracranial hemorrhage, outcome, and mortality after intra-arterial therapy for acute ischemic stroke in patients under oral anticoagulants. Stroke. 2011;42:3061–3066. doi: 10.1161/STROKEAHA.111.615476. [DOI] [PubMed] [Google Scholar]
- 11.Harenberg J, Kraemer R. Measurement of the new anticoagulants. Thromb Res. 2012;129 Suppl 1:S106–S113. doi: 10.1016/S0049-3848(12)70028-2. [DOI] [PubMed] [Google Scholar]
- 12.Purrucker JC, Haas K, Rizos T, Khan S, Poli S, Kraft P, et al. Coagulation testing in acute ischemic stroke patients taking non-vitamin K antagonist oral anticoagulants. Stroke. 2017;48:152–158. doi: 10.1161/STROKEAHA.116.014963. [DOI] [PubMed] [Google Scholar]
- 13.Cuker A, Siegal DM, Crowther MA, Garcia DA. Laboratory measurement of the anticoagulant activity of the non-vitamin K oral anticoagulants. J Am Coll Cardiol. 2014;64:1128–1139. doi: 10.1016/j.jacc.2014.05.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seiffge DJ, Traenka C, Polymeris A, Hert L, Fisch U, Peters N, et al. Feasibility of rapid measurement of rivaroxaban plasma levels in patients with acute stroke. J Thromb Thrombolysis. 2017;43:112–116. doi: 10.1007/s11239-016-1431-7. [DOI] [PubMed] [Google Scholar]
- 15.Seiffge DJ, Traenka C, Gensicke H, Tsakiris DA, Bonati LH, Peters N, et al. Intravenous thrombolysis in stroke patients receiving rivaroxaban. Eur J Neurol. 2014;21:e3–e4. doi: 10.1111/ene.12285. [DOI] [PubMed] [Google Scholar]
- 16.Ringelstein EB, Chamorro A, Kaste M, Langhorne P, Leys D, Lyrer P, et al. European Stroke Organisation recommendations to establish a stroke unit and stroke center. Stroke. 2013;44:828–840. doi: 10.1161/STROKEAHA.112.670430. [DOI] [PubMed] [Google Scholar]
- 17.Seiffge DJ, Hooff RJ, Nolte CH, Béjot Y, Turc G, Ikenberg B, et al. Recanalization therapies in acute ischemic stroke patients: impact of prior treatment with novel oral anticoagulants on bleeding complications and outcome. Circulation. 2015;132:1261–1269. doi: 10.1161/CIRCULATIONAHA.115.015484. [DOI] [PubMed] [Google Scholar]
- 18.Demaerschalk BM, Kleindorfer DO, Adeoye OM, Demchuk AM, Fugate JE, Grotta JC, et al. Scientific rationale for the inclusion and exclusion criteria for intravenous alteplase in acute ischemic stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47:581–641. doi: 10.1161/STR.0000000000000086. [DOI] [PubMed] [Google Scholar]
- 19.Jauch EC, Saver JL, Adams HP, Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- 20.Lyden P, Brott T, Tilley B, Welch KM, Mascha EJ, Levine S, et al. Improved reliability of the NIH stroke scale using video training. NINDS TPA Stroke Study Group. Stroke. 1994;25:2220–2226. doi: 10.1161/01.str.25.11.2220. [DOI] [PubMed] [Google Scholar]
- 21.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gensicke H, Zinkstok SM, Roos YB, Seiffge DJ, Ringleb P, Artto V, et al. IV thrombolysis and renal function. Neurology. 2013;81:1780–1788. doi: 10.1212/01.wnl.0000435550.83200.9e. [DOI] [PubMed] [Google Scholar]
- 23.Gensicke H, Seiffge DJ, Polasek AE, Peters N, Bonati LH, Lyrer PA, et al. Long-term outcome in stroke patients treated with IV thrombolysis. Neurology. 2013;80:919–925. doi: 10.1212/WNL.0b013e3182840c35. [DOI] [PubMed] [Google Scholar]
- 24.Scheitz JF, Seiffge DJ, Tütüncü S, Gensicke H, Audebert HJ, Bonati LH, et al. Dose-related effects of statins on symptomatic intracerebral hemorrhage and outcome after thrombolysis for ischemic stroke. Stroke. 2014;45:509–514. doi: 10.1161/STROKEAHA.113.002751. [DOI] [PubMed] [Google Scholar]
- 25.Hacke W, Kaste M, Fieschi C, Toni D, Lesaffre E, von Kummer R, et al. Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. The European Cooperative Acute Stroke Study (ECASS) JAMA. 1995;274:1017–1025. [PubMed] [Google Scholar]
- 26.National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–1587. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 27.Dennis M, Mead G, Doubal F, Graham C. Determining the modified rankin score after stroke by postal and telephone questionnaires. Stroke. 2012;43:851–853. doi: 10.1161/STROKEAHA.111.639708. [DOI] [PubMed] [Google Scholar]
- 28.Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:3020–3035. doi: 10.1161/STR.0000000000000074. [DOI] [PubMed] [Google Scholar]
- 29.Mueck W, Lensing AW, Agnelli G, Decousus H, Prandoni P, Misselwitz F. Rivaroxaban: population pharmacokinetic analyses in patients treated for acute deep-vein thrombosis and exposure simulations in patients with atrial fibrillation treated for stroke prevention. Clin Pharmacokinet. 2011;50:675–686. doi: 10.2165/11595320-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 30.Steiner T, Böhm M, Dichgans M, Diener HC, Ell C, Endres M, et al. Recommendations for the emergency management of complications associated with the new direct oral anticoagulants (DOACs), apixaban, dabigatran and rivaroxaban. Clin Res Cardiol. 2013;102:399–412. doi: 10.1007/s00392-013-0560-7. [DOI] [PubMed] [Google Scholar]
- 31.Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta stroke programme early CT score. Lancet. 2000;355:1670–1674. doi: 10.1016/s0140-6736(00)02237-6. [DOI] [PubMed] [Google Scholar]
- 32.Mueck W, Borris LC, Dahl OE, Haas S, Huisman MV, Kakkar AK, et al. Population pharmacokinetics and pharmacodynamics of once- and twice-daily rivaroxaban for the prevention of venous thromboembolism in patients undergoing total hip replacement. Thromb Haemost. 2008;100:453–461. [PubMed] [Google Scholar]
- 33.Meretoja A, Putaala J, Tatlisumak T, Atula S, Artto V, Curtze S, et al. Off-label thrombolysis is not associated with poor outcome in patients with stroke. Stroke. 2010;41:1450–1458. doi: 10.1161/STROKEAHA.109.576140. [DOI] [PubMed] [Google Scholar]
- 34.Kepplinger J, Prakapenia A, Barlinn K, Siegert G, Gehrisch S, Zerna C, et al. Standardized use of novel oral anticoagulants plasma level thresholds in a new thrombolysis decision making protocol. J Thromb Thrombolysis. 2016;41:293–300. doi: 10.1007/s11239-015-1229-z. [DOI] [PubMed] [Google Scholar]
- 35.Xian Y, Federspiel JJ, Hernandez AF, Laskowitz DT, Schwamm LH, Bhatt DL, et al. Use of intravenous recombinant tissue plasminogen activator in patients with acute ischemic stroke who take non-vitamin K antagonist oral anticoagulants before stroke. Circulation. 2017;135:1024–1035. doi: 10.1161/CIRCULATIONAHA.116.023940. [DOI] [PubMed] [Google Scholar]
- 36.Ebner M, Peter A, Spencer C, Härtig F, Birschmann I, Kuhn J, et al. Point-of-care testing of coagulation in patients treated with non-vitamin K antagonist oral anticoagulants. Stroke. 2015;46:2741–2747. doi: 10.1161/STROKEAHA.115.010148. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Standard operating procedure (SOP) Stroke Center University Hospital Basel for selection of patients with acute ischemic stroke taking Rivoraxoaban for treatment with intravenous thrombolysis (IVT) and endovascular treatment (EVT) based on rivaroxaban plasma levels. *Consider no IVT if mild stroke NIHSS≤4 or comorbidities; † Consider EVT if proximal vessel occlusion is present. NIHSS, National Institutes of Health Stroke Scale.


