Abstract
Objective
To assess variables that could be related to outcomes in fractures of the tibial pilon treated by open reduction and internal fixation (ORIF).
Design
Retrospective.
Setting
University Hospital.
Patients
A total 92 fractures of the tibial pilon treated by ORIF in a 5-year period. The minimum follow-up was 1 year (mean: 3.3 years; range: 1–5).
Intervention
ORIF with LCP-LISS plate.
Primary outcome measurements
Age, sex, side, type of fracture, energy of the injury, provisional external fixation (EF), time until ORIF, stages of treatment (one or two), surgical approach, type of bone fixation, quality of reduction, bone graft, hardware removal, associated fractures (fibula and others), functional results (AOFAS scale), rates of infection, skin necrosis, flap coverage, non-union, and early posttraumatic ankle osteoarthritis (AOA).
Results
According to AOFAS scale 30.5% of results were excellent, 46.7% good, 13.1% fair and 9.7% poor. Overall, the rate of infection was 13.04%, The rate of non-union was 10.86%. The rate of skin necrosis was 7.6% and the rate of flap coverage was 13.04%. The rate of early posttraumatic AOA was 13.04%. Type 43C3 fractures of the AO classification had a higher rate of skin necrosis and flap coverage. Open fractures were related to a higher prevalence of nonunion and flap coverage. The use of a bone graft was associated with a higher rate of nonunion and poor results. Infection was related to a higher prevalence of fair and poor results. EF was associated with a higher need for flap coverage. A suboptimal anatomic reduction was related to a higher rate of fair and poor results. The anteromedial approach was associated with a higher prevalence of skin necrosis and early posttraumatic AOA than the anterolateral approach. The use of an medial plate was related to a higher rate of nonunion than the use of a lateral plate.
Conclusions
The anteromedial approach was associated with a higher rate of skin necrosis and posttraumatic AOA than the anterolateral approach. Medial plating had a higher prevalence of nonunion than lateral plating.
Level of evidence
IV (case series).
Keywords: Tibial pilon, Fractures, Osteosynthesis, Complications, Outcomes
1. Introduction
Pilon fractures are serious injuries affecting the articular surface of the distal tibia. Sometimes they are due to high-energy trauma with an axial load, whereas in other patients, they tend to be the result of low-energy trauma due to a rotational mechanism.1 Articular involvement and a high degree of comminution are common in metaphyseal fractures.2 Treatment is primarily surgical. Problems after surgery are common; complications can affect the soft tissues (skin necrosis, requirements for flap coverage and infection) 3, 4, 5, 6 or involve the bone (posttraumatic ankle osteoarthritis [AOA], osteomyelitis and nonunion).7
To achieve good function, we must restore the articular surface through optimal anatomic reduction and a stable fixation.1, 8 It is also important to appropriately handle the soft tissues.9 There is some controversy in the literature regarding the variables affecting outcome in fractures of the tibial pilon treated by open reduction and internal fixation (ORIF): One stage (<48 h) 7, 10, 11 or two stages (staged treatment), placing an external fixator (EF) or a plaster splint in the first stage, delaying definitive ORIF until the soft tissues are healed, 8, 9, 12, 13, 14 et cetera.
The aim of this study was to evaluate which variables could be related to functional results and complications after ORIF of tibial pilon fractures.
2. Patients and methods
We analyzed 94 patients with tibial pilon fractures treated by ORIF between January 2011 and December 2015 in one University Hospital. The minimum follow-up was 1 year (mean: 3.3 years; range: 1–5); 2 cases were lost to follow-up. The study was conducted on a sample of 92 patients. Data were collected from the clinical records of the patients.
The trauma energy was defined as high (traffic accidents, falls from heights) or low (domestic accidents, accidental injuries). In all cases, a preoperative CT scan was performed to define the degree of joint and metaphyseal involvement.
ORIF was performed in one stage (<48 h) when there was no edema or blisters; or in two stages, with use of EF or splint in the first stage on arrival to the emergency room, with ORIF delayed until the soft tissue state was adequate (the disappearance of edema and blisters). The choice of surgery in one stage or in two stages was made individually, depending on the soft tissue state of each patient.
All the fractures were classified according to the AO system reported by Muller.15 Open fractures were classified according to Gustilo-Anderson classification.16We also recorded whether there was an associated fibular fracture.
We performed an anteromedial, anterolateral or percutaneous approach, depending on the type of fracture and the state of the skin. As for ORIF, we divided patient groups into those who had bone fixation with a single medial plate, a single anterolateral plate, two plates or cannulated screws. The model of the plates was in all cases the locking compression pale – less invasive stabilization system (LCP-LISS). Fibula was also fixed with LCP-LISS plates (six holes) by means of a direct lateral approach at the same time of external fixation. The goal was to maintain the length of the tibioperoneal complex and the normal rotation of the fibula. The length in days of conversion of external fixation to ORIF was 6.7 days on average (range, 2–21).
Quality of reduction was defined as optimal or suboptimal in terms of the existence of an articular step-off of <2 mm or >2 mm, respectively.17 The size of step-off was measured in post-operative radiographs. The use of a bone graft in fractures with metaphyseal defect was also recorded. Bone graft was indicated when in the pre-operative radiographs we found a great lack of cancellous bone (lack of contact of cortical bone). Immobilization was performed postoperatively for 1–2 weeks for soft tissue protection and edema control. Partial weight bearing was allowed from the twelve week after ORIF.
To address potential sources of bias we defined all variables in a clear way. The study size was the number of patients treated (94) minus two that were lost to follow-up (92 overall).
We recorded complications affecting the soft tissues (necrosis of the skin, superficial or deep infection and the requirement for flap coverage due to failure of direct closure), and complications affecting the bone (nonunion and early posttraumatic AOA).
Early posttraumatic AOA was evaluated by means of a modification of the Kellgren-Lawrence scale (Table 1).18
Table 1.
Modified Kellgren-Lawrence system of classifying the severity of posttraumatic ankle osteoarthritis (AOA) in nonweight-bearing ankle radiographs.
| Grade 0- | no radiographic features of AOA are present |
| Grade 1- | doubtful joint space narrowing (JSN) and possible osteophytic lipping |
| Grade 2- | the presence of definite osteophytes and possible JSN on anteroposterior radiograph. |
| Grade 3- | multiple osteophytes, definite JSN, sclerosis, possible bony deformity |
| Grade 4- | large osteophytes, marked JSN, severe sclerosis and definitely bony deformity |
Function was assessed according to the American Orthopedic Foot and Ankle Society (AOFAS) scale, although we know that this is heavily weighted in the scoring.19 Therefore these injuries that cause significant stiffness really affect the overall score. We divided the results into excellent (>90 points), good (80–90 points), fair (70–80 points) and poor (<70 points) (Fig. 1, Fig. 2). We assessed whether there was an association between the variables analyzed and the functional outcomes (AOFAS) and the complications encountered. Quantitative variables were handled by means of well-known scales (AOFAS, et cetera). Table 2 shows patient data of this study.
Fig. 1.
(A–K) Open tibial pilon fracture. A 44-year-old man suffered an accident with trauma to his right ankle. An external fixator (EF) was implanted in the emergency department. Fifteen days later days the definitive open reduction and internal fixation (ORIF) was carried out. The result was good: (A) AP radiograph of the tibial pilon fracture. (B) Lateral view of the fracture. (C) AP radiograph after the implantation of the EF. (D) Lateral radiograph with the EF. (E) Axial view of the postoperative CT scan performed. (F) Saggital view of the postoperative CT scan. (G) Coronal view of the postoperative CT scan. (H) AP postoperative radiograph. (I) Lateral postoperative radiograph. (J) AP radiograph 5 years later. (K) Lateral radiograph at 5 years follow-up.
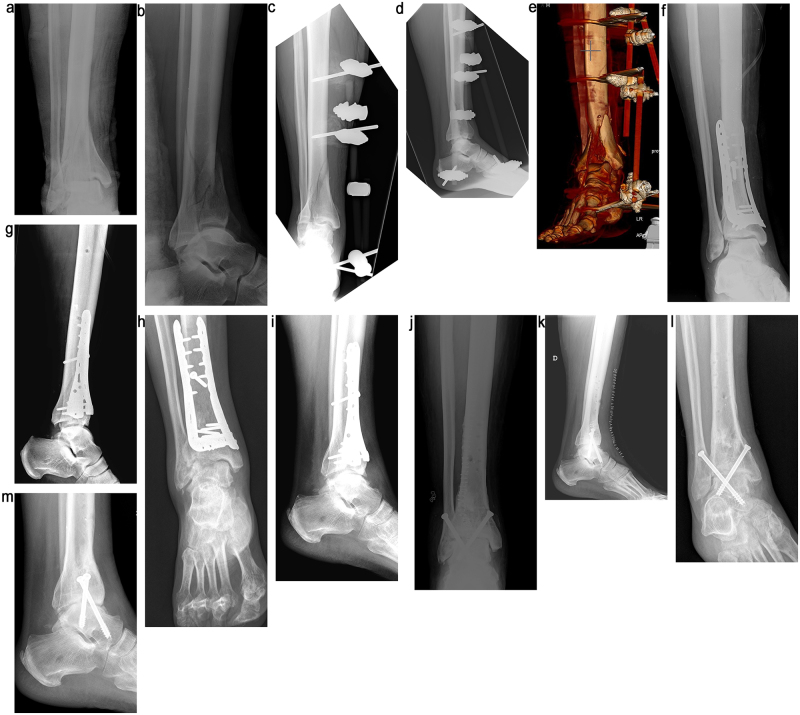
Fig. 2.
(A–M) Closed tibial pilon fracture. A 54 year-old male suffered a fall from 7 m high with blunt trauma to his right ankle. An external fixator (EF) was implanted in the emergency department. Nine days later days the definitive open reduction and internal fixation (ORIF) was carried out. The result was poor, with early posttraumatic ankle (AOA) osteoarthritis that required an early ankle fusion 15 months after the initial injury: (A) AP radiograph showed a closed fracture (type 43C3) of the tibial pilon. (B) Lateral view of the fracture. (C) AP radiograph after the implantation of the EF. (D) Lateral radiograph with the EF. (E) 3-D CT scan showing the fracture. Note gap and step-off. (F) AP radiograph after open reduction and internal fixation (ORIF) of the tibia that was carried out with two plates (anteromedial and anterolateral). Reduction was not satisfactory (note the step-off). (G) Lateral radiograph after ORIF. (H) AP radiograph 15 months later showing early posttraumatic AOA. (I) Lateral radiograph 15 months later showing early posttraumatic AOA. Ankle fusion was indicated. (J) AP radiograph after ankle fusion. (K) Lateral radiograph after ankle fusion. (L) AP radiograph 2 years after ankle fusion. (M) Lateral radiograph 2 years after ankle fusion.
Table 2.
Patient data of this study. AOFAS = American Orthopedic Foot and Ankle Society.
| Variable | Results |
|---|---|
| Age (years) | Mean 47.7 (range 22–93) |
| Sex | 49 (53.26%) male, 43 (46.73%) female |
| Side | 50 (54.34%) right, 42 (45.765%) left |
| AO-Muller classification | 24 (46.73%) 43B3, 21 (22.82%) 43 C1-2, 47 (51.08%) 43C3 |
| Type of fracture | 70 (76.08%) closed, 22 (23.91%) open |
| Energy of trauma | 49 (53.26%) high, 43 (46.8%) low |
| Fibular fracture | 68 (73.91%) yes, 24 (26.08%) no |
| External fixator (EF) | 33 (35.86%) yes, 59 (64.13%) no − plaster splint |
| Time to definitive surgery | 9.42 (1–35) days |
| Stage | 14 (15.21%) one, 78 (84.78%) two |
| Surgical approach | 51 (59.34%) anteromedial, 24 (27.9%) anterolateral, 11 (12.79%) percutaneous |
| Type of bone fixation | 49 (53.26%) medial plate, 31 (33.69%) lateral plate, 11 (12.79%) two plates, 5 (5.43%) cannulated screws |
| Quality of reduction | 78 (84.7%) optimal, 14 (15.21%) suboptimal |
| Bone graft | 14 (15.21%) yes, 78 (84.7%) no |
| Hardware removal (HR) | 23 (25%) yes, 69 (75%) no |
| Associated fractures | 17 (18.5%) yes, 75 (81.5%) no |
| AOFAS: | Mean: 83.11 (range 46–97) |
| Excellent (>90 points) | Excellent: 28 (30.5%) |
| Good (80–90 points) | Good: 43 (46.7%) |
| Fair (70–80 points) | Fair: 12 (13.1%) |
| Poor (<70 points) | Poor: 9 (9.7%) |
We carried out a statistical analysis of qualitative data (Chi-squared test, Fisher’s exact test, Mann-Whitney U test and Student’s t-test) and of quantitative data (ANOVA and Kruskal Wallis test). The variables for the study were analyzed with a Cox multivariable regression analysis. We used a value of p < 0.05 for statistically significant differences.
3. Results
A total of 92 fractures of the tibial pilon treated by ORIF in a 5-year period were analyzed. The mean follow-up was 3.3 years (range, 1–5 years).
Among the soft-tissue complications, we found 12 infections (13.04%) (4 superficial [4.34%] and 8 deep [8.69%]), 7 skin necroses (7.6%) and 12 flaps for skin coverage (13.04%) in 8 open and 4 closed fractures. Within these 12, there were 1 infected non-union, 1 injury of the posterior tibial artery and 2 patients with skin necrosis requiring closure by flap (this topic is the subject of another study).
Among the bone complications we found 10 nonunions (10.86%) (3 were infected non-unions [3.25%]) and 12 patients with early posttraumatic AOA (13.04%) (in 5 of whom [5.43%] ankle arthrodesis was performed later, with satisfactory results in terms of pain remission) (Fig. 2).
Other complications included 1 compartment syndrome, 2 complex regional syndromes, 1 sural nerve injury, 1 neuroapraxia of the deep peroneal nerve and 2 injuries of the posterior tibial artery (1 during the approach and 1 during the placement of the EF). No lower limb amputations were required in this series. Twenty-three hardware removals (HRs) (25%) were performed at an average of 1.2 years after ORIF. Implant removal was carried out because of pain. Table 3 shows the correlation or the lack of correlation among the variables studied.
Table 3.
Correlations among some variables were found in this study. Those with a statistically significant correlation (p < 0.05) are shown in black and with an asterisk. The remaining variables showed no significant (NS) correlation. AOA = ankle osteoarthritis. HR = hardware removal. AOFAS = American Orthopedic Foot and Ankle Society.
| Skin necrosis | Infection | Flap | Nonunion | Early posttraumatic AOA | AOFAS | |
|---|---|---|---|---|---|---|
| Age | NS | NS | NS | NS | NS | NS |
| Gender | NS | NS | NS | NS | NS | NS |
| Side NS | NS | NS | NS | NS | NS | |
| Type C AO classification | p = 0.006* | NS | NS | NS | NS | p= 0.018* |
| Type of fracture (closed- open) NS |
NS | p = 0.002* | p = 0.055* | NS | NS | |
| Energy of trauma NS | NS | NS | NS | NS | ||
| Fibula fracture | NS | NS | NS | NS | NS | NS |
| External fixator (EF) NS | NS | p = 0.01* | NS | NS | NS | |
| Time to definitive surgery NS | NS | NS | NS | NS | ||
| Stage | NS | NS | NS | NS | NS | NS |
| Anteromedial approach | p = 0.021 * | NS | NS | NS | p = 0.048* | NS |
| Type of osteosynthesis NS | NS | NS | p = 0.035* | NS | NS | |
| Quality of reduction NS | NS | NS | NS | NS | p = 0.002* | |
| Bone graft NS | NS | NS | p = 0.054* | NS | p = 0.054* | |
| HR | NS | NS | NS | NS | NS | p = 0.045* |
| Associated fractures NS | NS | NS | NS | NS | NS |
3.1. Skin necrosis
We observed a statistically significant correlation between skin necrosis and the anteromedial approach (p = 0.021) (OR 4.2), which might be due to the poor vascularization of the medial aspect of the tibia. We also found a significant statistical correlation between skin necrosis and 43C3 fractures (p =0.006). More complex fractures and metaphyseal comminution had a higher rate of postoperative skin necrosis. This can be explained by the broader approach that is needed to reduce the fracture or by the trauma itself, causing necrosis of the adjacent soft tissues. There were no significant correlations between skin necrosis and the other variables studied.
3.2. Infection
No correlation was found between presentation of a postoperative infection and the rest of the parameters analyzed.
3.3. Flap coverage
There was a statistically significant correlation between EF and flap coverage (p = 0.011). We think this could be due to a poorer soft tissue status in patients requiring an EF on arrival. Open fractures had a higher rate of flap coverage (p = 0.002). There were no significant correlations between the need for flap coverage and the other variables studied.
3.4. Nonunion
Open fractures showed a higher rate of nonunion (p = 0.05). Anteromedial plates also showed a higher prevalence of nonunion than anterolateral plates (p = 0.035). Patients who needed a bone graft during ORIF had a higher rate of nonunion than those who did not need a bone graft (p = 0.05). There were no significant correlations between nonunion and the rest of the parameters analyzed.
3.5. Early posttraumatic AOA
A statistically significant correlation between the anteromedial approach and early posttraumatic AOA was found. There was no significant correlation between early posttraumatic AOA and the other variables studied.
3.6. AOFAS
The AOFAS scale was more likely to show a poor (<70 points) or fair (70–80 points) result in patients who had superficial or deep infection (p = 0.017), in patients with more complex fractures (43C3, according to the AO classification), in patients with suboptimal reduction (>2 mm step-off) (p = 0.002), in those who required a bone graft during ORIF (p = 0.05) and in those who required HR (p = 0.045). There were no significant correlations between the AOFAS score and the rest of the parameters analyzed.
4. Discussion
Pilon fractures account for 1% of all fractures.1 There is controversy in the literature about its management. In this study, we analyzed important variables in the surgical treatment (ORIF) of these fractures to analyze possible correlations among them and how they relate to complications and functional results.
In our study we had 13.04% infections, 7.6% skin necroses, 13.04% flaps for skin coverage, 10.86% nonunions and 13.04% early posttraumatic AOA. We found a statistically significant correlation between skin necrosis and the anteromedial approach. We also observed a significant statistical correlation between skin necrosis and 43C3 fractures. We encountered a statistically significant correlation between EF and flap coverage.
Open fractures had a higher rate of flap coverage and a higher rate of nonunion. Anteromedial plates had a higher prevalence of nonunion than anterolateral plates. Patients who required a bone graft during ORIF had a higher rate of nonunion than those who did not require a bone graft. A statistically significant correlation between the anteromedial approach and early posttraumatic AOA was observed.
The AOFAS scale was more likely to show a poor (<70 points) or fair (70–80 points) result in patients who had infection, in patients with more complex fractures, in patients with suboptimal reduction, in those who needed a bone graft during ORIF and in those who needed HR.
The primary limitations of our study are that it is retrospective and that several surgeons were involved in the treatment of fractures. We did not analyze other variables that could influence the results, which could be associated with a poorer prognosis or a longer duration of surgery. Such variables include glucose concentration in the postoperative period, the use of negative pressure for the healing of the soft-tissues and the presence or absence of bleeding blisters on arrival to the emergency room.
The quality of anatomic reduction is the most important factor in the treatment of these fractures. Anatomic reduction of the tibial articular surface correlates with better functional outcomes1, 8; however, there is controversy on how to define perfect reduction.1, 8 In our study, a higher rate of fair and poor functional results (AOFAS) was obtained with a suboptimal quality of reduction (>2 mm articular step-off).
The literature discusses which approach must be used, given the poor condition of the skin of the distal tibia. There are a number of approaches; however, the fracture pattern frequently determines the approach to be used.20 In our study, we only used the anteromedial, anterolateral and percutaneous approaches. Percutaneous approaches were used for simpler fracture patterns. We used 3–4 incisions and the implant utilized was the LCP-LISS plate. The anterolateral approach offers improvements in the state of soft tissues, with fewer complications; however, additional approaches are needed to reach the medial aspect of the tibia.21 Anteromedial and posterolateral approaches carry a greater risk of soft-tissue complications.22 In our study, we observed that the anteromedial approach presented a higher rate of skin necrosis and early posttraumatic AOA.
More complex fractures (43C3) have poorer functional outcomes (AOFAS),1 regardless of the reduction quality. We found fair and poor results (AOFAS) in 43C3 fractures (AO), as well as a higher rate of skin necrosis.
We observed that open fractures had a higher rate of nonunion. The need for a flap after ORIF occurs in those fractures with poor skin condition or major skin defects.8 In our study, the use of EF was associated with a higher incidence of flap coverage. Fractures that required an EF were more often open, with soft tissue involvement. This finding seems to be related to the fracture pattern. The same goes for medial plating. Both approach and implants should be determined by the individual fracture pattern and soft tissue status.
There is controversy regarding the time to flap coverage. Allegrand et al. pointed out that flap coverage must be performed in less than 7 days. From the 7th day, soft complications might appear, especially infection.5 Sood et al. recorded good results by use of rotational flaps.6 In our series soft tissue coverage was performed within 48–72 h of definitive fixation.
In some fractures, ORIF of the fibula is not required.23 In our series, we always fixed the fibula; fibular fixation was performed by means of LCP-LISS plates. D'Heurle et al. found no difference in outcome between plates and other types of fixation.24
In our study, we performed both one-stage surgery (ORIF in <48 h) and two-stage surgery (delayed ORIF between 10 days and 3 weeks post-injury). We did not find differences between them using any of the studied variables. White et al. obtained similar functional results and complications by definitive surgery in less than 24–48 h compared with a later surgical procedure.10 Increased infections and wound dehiscence are more common in open fractures (19%) than in closed fractures (2.7%).10 We did not encounter differences between open and closed fractures or the stage of surgery. Tang et al. 11 found no significant differences in soft-tissue complications, nonunions and results between definitive surgery in <36 h and delayed surgery between 10 days and 3 weeks after injury. They concluded that if the skin condition is optimal, the results of definitive surgery in 1 or 2 days are similar.11 Lomax et al. 7 obtained comparable results between surgery performed in less than 48 h and that performed later: 1.6% deep infection, 6.3% superficial infection, 7.8% nonunion, 26.6% posttraumatic AOA and 26.6% requiring further surgery.7 Our results are similar to the study of Lomax et al.
Sirkin et al. achieved good results in open and closed fractures.12 We did not find differences between open and closed fractures. Crist et al. used EF when the state of the soft tissues was not suitable, deferring surgery to a later time.25
Boraiah et al. achieved very good results using an algorithm with an individualized treatment according to each patient. They found a rate of healing of 88.13%, 3% with deep infection and 5% with superficial infection.13
Deivaraju et al. 14analyzed the two-stage treatment, using a medial plate or an anterolateral plate during ORIF. They found comparable results in terms of quality of reduction and soft-tissue complications; however, they observed a higher incidence of infection and nonunion with medial plates.14 In our study, we also found a higher incidence of nonunion with open medial plates.
Regarding infection, Ren et al. reported that the risk factors for infection are postoperative glucose concentration >125 mg/dl and a surgical duration >150 min.26 In our study, we did not analyze these parameters. No variables analyzed in the study were associated with an increased risk of infection; however, infection was logically associated with fair and poor results (AOFAS).
The role of bone graft during ORIF is not clear in the literature. We found a higher rate of nonunion and a higher prevalence of fair and poor results in fractures requiring bone grafts. Maybe not the grafting for the procedure but rather the fracture pattern was responsible for the high non-union rate (10.86%) and poor results (9.7%) in this series. Use of negative pressure has been associated with improved rates of soft-tissue healing after surgery.8,25 We did not analyze this parameter.
Regarding the generalisability (external validity) of the study results, we can make some recommendations to improve the surgical treatment of tibial pilon fractures: The anteromedial approach related to a higher rate of skin necrosis and posttraumatic AOA than the anterolateral approach. Medial plating was associated with a greater rate of nonunion than lateral plating. To get good and excellent results (AOFAS), an anatomic reduction is compulsory. As for the prognosis, 43C3 fractures were related to a higher rate of skin necrosis and flap coverage. Open fractures had a higher prevalence of nonunion and required more flaps. Patients requiring bone grafting during ORIF had more nonunions and a higher rate of fair or poor results (AOFAS). Infected fractures and patients requiring HR showed a higher rate of fair or poor results (AOFAS). The use of an EF in the emergency room was associated with a greater need for flap coverage. Again, maybe not the use of an EF but rather the fracture pattern was responsible for the high need for flap coverage (13.04%) in this series.
In conclusion, the anteromedial approach was associated with a higher rate of skin necrosis and early posttraumatic AOA than the anterolateral approach. Open medial plating had a higher prevalence of nonunion than open lateral plating.
Conflict of interest
The authors declare no conflicts of interest.
References
- 1.Korkmaz A., Ciftdemir M., Ozcan M., Copuroğlu C., Sarıdoğan K. The analysis of the variables, affecting outcome in surgically treated tibia pilon fractured patients. Injury. 2013;44:1270–1274. doi: 10.1016/j.injury.2013.06.016. [DOI] [PubMed] [Google Scholar]
- 2.Bonar S.K., Marsh J.L. Tibial plafond fractures: changing principles of treatment. J Am Acad Orthop Surg. 1994;2:297–305. doi: 10.5435/00124635-199411000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Trumble T.E., Benirschke S.K., Vedder N.B. Use of radial forearm flaps to treat complications of closed pilon fractures. J Orthop Trauma. 1992;6:358–365. doi: 10.1097/00005131-199209000-00015. [DOI] [PubMed] [Google Scholar]
- 4.McFerran M.A., Smith S.W., Boulas H.J., Schwartz H.S. Complications encountered in the treatment of pilon fractures. J Orthop Trauma. 1992;6:195–200. doi: 10.1097/00005131-199206000-00011. [DOI] [PubMed] [Google Scholar]
- 5.D’Alleyrand J.C., Manson T.T., Dancy L. Is time to flap coverage of open tibial fractures an independent predictor of flap-related complications. J Orthop Trauma. 2014;28:288–293. doi: 10.1097/BOT.0000000000000001. [DOI] [PubMed] [Google Scholar]
- 6.Sood A., Khamsi B., Datiashvili R., Berberian W.S. Use of cross-leg flap for wound complications resulting from open pilon fracture. Am J Orthop (Belle Mead NJ) 2015;44:131–134. [PubMed] [Google Scholar]
- 7.Lomax A., Singh A.N., Jane M.C., Senthil K. Complications and early results after operative fixation of 68 pilon fractures of the distal tibia. Scott Med J. 2015;60:79–84. doi: 10.1177/0036933015569159. [DOI] [PubMed] [Google Scholar]
- 8.Krettek C., Bachmann S. Pilon fractures. Part 2: repositioning and stabilization technique and complication management. Chirurg. 2015;86:187–201. doi: 10.1007/s00104-014-2917-5. [DOI] [PubMed] [Google Scholar]
- 9.Liporace F.A., Mehta S., Rhorer A.S., Yoon R.S., Reilly M.C. Staged treatment and associated complications of pilon fractures. Instr Course Lect. 2012;61:53–70. [PubMed] [Google Scholar]
- 10.White T.O., Guy P., Cooke C.J. The results of early primary open reduction and internal fixation for treatment of OTA 43. C-type tibial pilon fractures: a cohort study. J Orthop Trauma. 2010;24:757–763. doi: 10.1097/BOT.0b013e3181d04bc0. [DOI] [PubMed] [Google Scholar]
- 11.Tang X., Liu L., Tu C.Q., Li J., Li Q., Pei F.X. Comparison of early and delayed open reduction and internal fixation for treating closed tibial pilon fractures. Foot Ankle Int. 2014;35:657–664. doi: 10.1177/1071100714534214. [DOI] [PubMed] [Google Scholar]
- 12.Sirkin M., Sanders R., DiPasquale T., Herscovici D., Jr. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma. 1999;13:78–84. doi: 10.1097/00005131-199902000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Boraiah S., Kemp T.J., Erwteman A., Lucas P.A., Asprinio D.E. Outcome following open reduction and internal fixation of open pilon fractures. J Bone Joint Surg Am. 2010;92:346–352. doi: 10.2106/JBJS.H.01678. [DOI] [PubMed] [Google Scholar]
- 14.Deivaraju C., Vlasak R., Sadasivan K. Staged treatment of pilon fractures. J Orthop. 2015;12(Suppl 1):S1–6. doi: 10.1016/j.jor.2015.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.http://www.aofundation.org/Documents/muller.ao.class.pdf.
- 16.Gustilo R.B., Anderson J.T. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–458. [PubMed] [Google Scholar]
- 17.Ovadia D.N., Beals R.K. Fractures of the tibial plafond. J Bone Joint Surg Am. 1986;68:543–551. [PubMed] [Google Scholar]
- 18.Kellgren J.H., Lawrence J.S. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davidovitch R.I., Elkhechen R.J., Romo S., Walsh M., Egol K.A. Open reduction with internal fixation versus limited internal fixation and external fixation for high grade pilon fractures (OTA type 43C) Foot Ankle Int. 2011;32:955–961. doi: 10.3113/FAI.2011.0955. [DOI] [PubMed] [Google Scholar]
- 20.Assal M., Ray A., Stern R. Strategies for surgical approaches in open reduction internal fixation of pilon fractures. J Orthop Trauma. 2015;29:69–79. doi: 10.1097/BOT.0000000000000218. [DOI] [PubMed] [Google Scholar]
- 21.Hak D.J. Anterolateral approach for tibial pilon fractures. Orthopedics. 2012;35:131–133. doi: 10.3928/01477447-20120123-31. [DOI] [PubMed] [Google Scholar]
- 22.Liu J., Smith C.D., White E., Ebraheim N.A. A systematic review of the role of surgical approaches on the outcomes of the tibia pilon fracture. Foot Ankle Spec. 2015;9:163–168. doi: 10.1177/1938640015620637. [DOI] [PubMed] [Google Scholar]
- 23.Kurylo J.C., Datta N., Iskander K.N., Tornetta P., 3rd. Does the fibula need to be fixed in complex pilon fractures? J Orthop Trauma. 2015;29:424–427. doi: 10.1097/BOT.0000000000000304. [DOI] [PubMed] [Google Scholar]
- 24.d́Heurle A., Kazemi N., Connelly C., Wyrick J.D., Archdeacon M.T., Le T.T. Prospective randomized comparison of locked plates versus nonlocked plates for the treatment of high-energy pilon fracture. J Orthop Trauma. 2015;29:420–423. doi: 10.1097/BOT.0000000000000386. [DOI] [PubMed] [Google Scholar]
- 25.Crist B.D., Khazzam M., Murtha Y.M., Della Rocca G.J. Pilon fractures: advances in surgical management. J Am Acad Orthop Surg. 2011;19:612–622. doi: 10.5435/00124635-201110000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Ren T., Ding L., Xue F., He Z., Xiao H. Risk factors for surgical site infection of pilon fractures. Clinics (Sao Paulo) 2015;70:419–422. doi: 10.6061/clinics/2015(06)06. [DOI] [PMC free article] [PubMed] [Google Scholar]