Abstract
Background
Long harsh winter in Kashmir Valley increase the incidence of pernio in children so much that common people consider every hand swelling as pernio.
Methods
10 Infants over two years were brought to our hospital as cases of pernio involving fingers.
Results
All the infants came out to be cases of impending gangrene due to mother’s hair as constriction bands around fingers.
Conclusion
Impending gangrene of fingers in infants due to mother hair as constriction band is very rare. However its symptoms overlap with symptoms of peripheral cold injuries and can be easily mistaken for each other by people.
Keywords: Gangrene, Peripheral cold injuries, Pernio, Infants
1. Introduction
Prolonged exposure of children to cold can result in systemic hypothermia and peripheral cold injuries like cold panniculitis, frostbite, pernio/chilblains or frostnip. Apical tissues like ears, cheek, toes, and fingers are mostly involved.1, 2, 3 The hands and feet in Infants in the crawling stage are in constant contact with the floor or cold surroundings. This makes them prone to peripheral cold injuries of hands and feet in areas with poor housing and heating conditions. The incidence of peripheral cold injuries in paediatric age group is unknown.4, 5 Pernio is a relatively common condition that we encounter in our hospital in winter season in all age groups, mostly in children and women.
Hair tourniquet syndrome is a rare but established medical condition mostly seen in paediatric age group.6 Clinical manifestations of this condition like swelling, pain, redness, numbness and blister formation overlap with symptoms of peripheral cold injuries. Late presenting hair tourniquet syndrome and peripheral cold injuries can be easily mistaken for each other by common people because of apparently similar presentation.
Kashmir valley is the northern most state of India, surrounded by high mountains which remain covered with snow for most part of the year. It has a long winter season with temperature as low as minus 10 °C.During winter season a large number of patients visit our hospital with symptoms of peripheral cold injuries (mostly pernio) so much so that every case of hand and feet swelling during winter is being considered as peripheral cold injury by common people. We report a unique series of 10 infants (age between 5 and 8 months) brought by parents as cases of peripheral cold injuries but came out to be cases of impending gangrene due to constriction bands around fingers at metacarpophalangeal level by mother’s hair.
2. Methods
Ten infants (4 male and 6 female) in the age group of 5 to 8 months and over a period of two years, between June 2014 to June 2016 (two winter seasons), were brought to our hospital by their parents as cases of pernio affecting the fingers. All the infants were previously healthy with no associated comorbidity. All the cases were from tribal areas of Kashmir with very limited health care facilities. All the patients were initially treated by local native practioners before being brought to our hospital. The duration of symptoms before visiting our hospital varied from 2 to 4 days. These patients were referred to orthopaedic department as signs and symptoms were more severe than routine cases of pernio as normally they are seen by dermatology department of our hospital. Parents of all the 10 infants were illiterate with absolutely no knowledge of the disease. All the Patients were wearing multilayered woolen clothes with overhanging sleeves to protect the hands and feet of the babies from cold. All the infants appeared to be in severe discomfort.
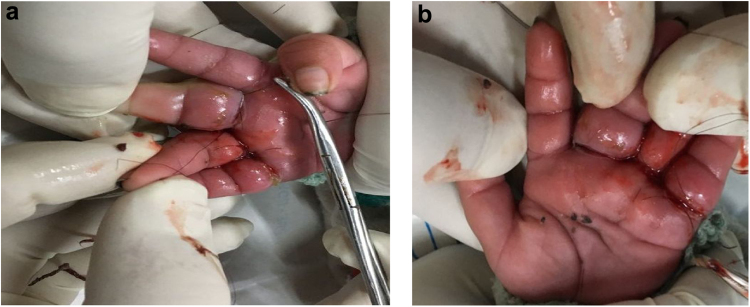
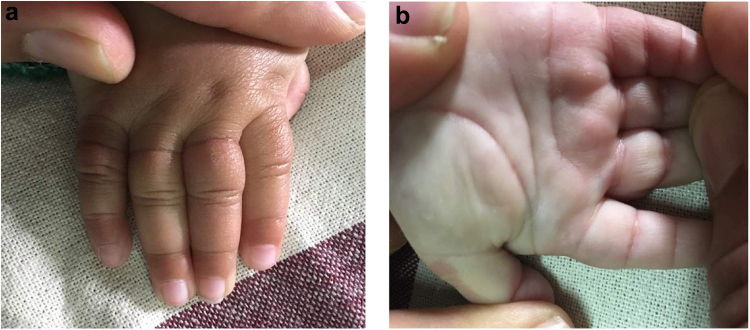
Patients were received and thoroughly examined in the emergency room. Peripheral pulses of all the infants were normally palpable. Pulse oximeter couldn’t read oxygen saturation in the affected fingers though it was normal ( >95%) in rest of the fingers. Blood work revealed a normal complete blood count, coagulogram, renal function, liver enzymes and electrolytes. X Rays of the involved hands were normal. There was no obvious cause of impending gangrene (Fig. 1a) in any patient except in one patient where an overhanging thread from the sweater sleeve of the infant was acting as a constriction band (Fig1b). Patients were immediately taken to operating room. Parts were cleaned with normal saline and Povidone Iodine. While cleaning the part wounds partially opened up. We were astonished to see hair constriction bands around the fingers at the metacarpophalangeal creases in all the patients involving one or multiple fingers (Fig. 2a and b). Hair bands were not visible to naked eye in any patient unless we washed and opened the wounds. Constriction bands were removed in all the patients after exploring the wound, vascularity was reassessed. It was observed that vascularity improved in all the patients once constriction bands were removed. None of the wound was stitched back, light antiseptic dressing was done in all the patients. All the patients were observed in the hospital for several days (2–5 days). Finger vascularity was checked clinically and with pulse oximeter frequently in the hospital till the time of discharge. Pulse oximeter recordings showed improvement in the post operative period in all the patients. Pulse oximeter showed recordings of Sp02 as 90% or more than 90% in all but 3 involved digits where saturation remained between 83% to 87%. After the discharge patients were regularly followed up in the Out Patient Department (OPD). All the patients recovered well in the follow up (Fig. 3a and b). However Recovery time varied in different patients from 6 days to 32 days.
Fig. 1.
a and b: Impending gangrene of little, middle and ring fingers (constriction band visible in only middle finger, an overhanging thread from sleeve of infant’s sweater).
Fig. 2.
a and b: Hair as constriction bands around little, middle and ring fingers at metacarpophalangeal joint creases seen intra-operatively in the same patient.
Fig. 3.
a and b: 3 months latter Fingers in good condition after constriction band removal.
Hair bands removed were sent to forensic laboratory for examination and they matched with mother’s hair in all the cases
3. Results
Out of 10 infants 3 had single digit involvement and 7 patients had multi digit involvement. Double digit involvement was seen in 5 patients, all having middle and ring finger involvement. Maximum number of involved fingers per patient were 3 (2 patients) (Fig. 1a), both having little, ring and middle involvement. Middle and ring fingers were most commonly involved. No infant had 4 or more than 4 digits involved as shown in Table 1.
Table 1.
Pattern of finger involvement.
| Pattern of finger involvement | No of patients |
|---|---|
| Single digit (1 thumb, 1 index, 1 little) | 3 |
| Double digit(middle and ring finger) | 5 |
| Triple digit(middle, ring and little finger) | 2 |
| Quadruple digit involvement | 0 |
4. Discussion
Hair tourniquet syndrome is a sporadically reported condition in literature, mostly involving patients in paediatric age group.6 Almost all the cases reported have shown involvement of fingers, toes or genitalia.7, 8, 9, 10, 11, 12, 13, 14, 15 A significant number of the cases reported in the literature are infants 2–3 months old where it is attributed to mother’s excessive hair fall due to hormonal changes after delivery.15
Hair tourniquet syndrome involving toes and fingers can be easily missed if it presents late, because of swelling of the part and very small size of the hair. Hair as constriction band around digits gets embedded in the loose skin around fingers and often becomes invisible to naked eye.
All the 10 cases in our study presented late because parents mistook the condition as pernio which is very common in our region during winter. Culture of native practioners in rural India further delayed their presentation to hospital. Patients were initially taken to native practioners for management of pernio where some ointment was applied for several days. By the time infants were brought to hospital the involved fingers had look of impending gangrene. All the involved fingers were grossly swollen, cyanotic and had blister formation.
The clinical manifestations of impending gangrene irrespective of the cause and peripheral cold injuries like pain, swelling, blister formation and numbness can be difficult to differentiate for common people when cause of gangrene in not obvious. Socioeconomic factors play an important role in the development of chilblains in our region. The long and cold winter in our region with poor housing and heating facilities during winter and virtually no health education among tribal people in rural Kashmir increases the incidence of peripheral cold injuries (mostly pernio) so much that they consider every hand and foot swelling as case of pernio and usually take treatment from native practioners. People tend to cover their children with multilayered woolen clothes. To prevent hands of infants from cold people use longer sleeves with some part overhanging beyond the level of fingers. This makes it difficult for the parents to check the hands of their infants regularly.
The treatment of hair tourniquet syndrome is early detection and immediate release of constriction band. This can be easily done if patient presents early and local reactive signs are yet to develop. Constriction band in such cases can be removed by inserting a probe between constrictor and body tissue and unwinding the hair or can be cut by inserting a small seizure between skin and hair and cutting the constriction band.15 Depilatory agents have also been used to remove hair as constriction bands without causing any pain to the patients.15, 16 However for the patients who present late constriction band is embedded into deeper tissues, re-epithelization of skin across the wound and gross swelling of the area makes constriction band invisible to naked eyes. Surgical exploration of the wound is needed to identify and remove the constriction band in such cases.15 All the patients in our series presented late. Constriction bands were visible to naked eye in only 1 case, where an overhanging thread from the sweater sleeve of the infant was acting as constriction band around a finger (Fig. 1b). Wounds were surgically explored under local anesthesia in all the cases till we reached to the bone. Hair bands were removed in all the patients.
All the patients despite having a worrisome picture of impending gangrene at the time of presentation did well in the follow up with full functional recovery. There are some case reports of impending gangrene of finger, genital gangrene, urethral fistulas and bony erosion reported due to hair/ hair thread tourniquet syndrome.17, 18, 19
Limb gangrene is a rare condition in neonates and in paediatric age group. Several factors like hypercoagulable state, uteroarterial thrombosis, polycythemia, maternal diabetes, congenital bands, birth trauma, prematurity, congenital syphilis, umbilical artery cannulation, intravenous hyperosmolar infusions and sepsis predispose gangrene formation in neonates.20 There are only few case reports of neonatal gangrene reported in the literature and in all the cases the cause of gangrene was some underlying disease.21, 22, 23, 24, 25, 26 None of the infants in our study had any associated comorbidity.
All the cases in our study were due to accidental injury and were missed by both parents and native practioners. Child abuse was ruled out as all the patients were regularly brought by parents for follow up and recovered well. Un-reporting and delayed reporting of Constriction bands can be a manifestation of child abuse.27
5. Conclusion
Lack of proper health care, poor socioeconomic status and culture of native practioners in rural India at times surprise surgeons with unusual conditions. In such circumstances always consider other differentials even while examining routine cases especially in children.
Conflict of interest
None.
Financial support
None.
Authors’ contributions
TAB has done the conception and design of the study and the writing and final approval of the manuscript. ZA wrote the manuscript and approved the final manuscript. TLM, AHS, AG and FM were involved in manuscript writing and in its critical revision and final approval. All authors read and approved the final manuscript.
Consent
Informed consent was obtained from the patient before enrolling for the study and accompanying images.
Contributor Information
Towseef Ahmad Bhat, Email: towseefortho@gmail.com.
Zameer Ali, Email: drzameeraliortho@gmail.com.
Tarseem Lal Moten, Email: tarseemoten@gmail.com.
Aabid Hussain Sofi, Email: sofiabid@gmail.com.
Furqaan Mir, Email: mirfurqaan@gmail.com.
Amara Gulzar, Email: amaragulzar@gmail.com.
References
- 1.Edlich Richard F. 2007. Cold Injuries. [ www.emedicine.com/ped/topic803.htm (Version currentat July 6, 2007)] [Google Scholar]
- 2.Gardinal-Galera I., Pajot C., Paul C., Mazereeuw-Hautier J. Childhood chilblains is an uncommon and invalidant disease. Arch Dis Child. 2010;95:567–568. doi: 10.1136/adc.2010.183145. [DOI] [PubMed] [Google Scholar]
- 3.Meltem Akkurt Z., Ucmak Derya, Yelzid Kenan. Chilblains in Turkey: a case-control study. An Bras Dermatol. 2014;89(January-February (1)):44–50. doi: 10.1590/abd1806-4841.20142376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raza N., Habib A., Razvi S.K., Dar N.R. Constitutional and behavioral risk factors for chilblains: a case-control study from Pakistan. Wilderness Environ Med. 2010;21(17):e1–e21. doi: 10.1016/j.wem.2009.12.023. [DOI] [PubMed] [Google Scholar]
- 5.Simon S., Soep T.D., Hollister J.B., JR. Pernio in pediatrics. Pediatrics. 2005;116:e472. doi: 10.1542/peds.2004-2681. [DOI] [PubMed] [Google Scholar]
- 6.Barton D.J., Sloan G.M., Nichter L.S., Reinish J.F. Hair-thread tourniquet syndrome. Pediatrics. 1988;82:925–928. [PubMed] [Google Scholar]
- 7.Garcia-Mata A., Hidalgo-Ovejero Hair tourniquet syndrome of the toe: report of 2 new cases. J Pediatr Orthop. 2009;29(8):860–864. doi: 10.1097/BPO.0b013e3181b7ff14. [DOI] [PubMed] [Google Scholar]
- 8.Peckler B., Hsu C.K. Tourniquet syndrome: a review of constricting band removal. J Emerg Med. 2001;20(3):253–262. doi: 10.1016/s0736-4679(00)00314-0. [DOI] [PubMed] [Google Scholar]
- 9.Schneider K., Kennebeck S., Madden L., Campbell A. Hair tourniquet of the circumvallate papillae: a potentially hairy situation. Pediatr Emerg Care. 2013;29(8):924–925. doi: 10.1097/PEC.0b013e31829ec4c7. [DOI] [PubMed] [Google Scholar]
- 10.Hickey B.A., Gulati S., Maripuri S.N. Hair toe tourniquet syndrome in a four year-old boy. J Emerg Med. 2013;44(2):39–58. doi: 10.1016/j.jemermed.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Dua R., Jamshidi, Lal D.R. Labial hair tourniquet: unusual complication of an unrepaired genital laceration. Pediatr Emerg Care. 2013;29(7):829–8301. doi: 10.1097/PEC.0b013e3182986184. [DOI] [PubMed] [Google Scholar]
- 12.Rich M.A., Keating M.A. Hair tourniquet syndrome of the clitoris. J Urol. 1999;162:190–191. doi: 10.1097/00005392-199907000-00067. [DOI] [PubMed] [Google Scholar]
- 13.Pomeranz M., Shachter B., Capua T., Beyth Y. Hair-thread tourniquet syndrome of labia minor. J Pediatr Adolesc Gynecol. 2009;22:e111–3. doi: 10.1016/j.jpag.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 14.Alverson B. A genital hair tourniquet in a 9-year-old girl. Pediatr Emerg Care. 2007;23:169–170. doi: 10.1097/PEC.0b013e3180328cc4. [DOI] [PubMed] [Google Scholar]
- 15.Alruwaili N., Alshehri H.A. B Halimah Hair tourniquet syndrome: successful management with a painless technique. Int J Pediatr Adolesc Med. 2015;(March):34–37. doi: 10.1016/j.ijpam.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Gorman, Ratnapalan S. Hair tourniquet management. Pediatr Emerg Care. 2011;27(3):203–204. doi: 10.1097/PEC.0b013e31820d65b7. [DOI] [PubMed] [Google Scholar]
- 17.Mat Saad A.Z., Purcell E.M., McCann J.J. Hair-thread tourniquet syndrome in an infant with bony erosion: a case report, literature review, and metaanalysis. Ann Plast Surg. 2006;57(4) doi: 10.1097/01.sap.0000222571.98387.71. [DOI] [PubMed] [Google Scholar]
- 18.Nicola Bizzotto, Andrea Sandri, Dario Regis, Guillherme Carpeggiani, Franco Lavini, Bruno Magnan. Serious delayed hair toe tourniquet syndrome with bone erosion and flexor tendon lesion. Case Rep Pediatr. 2014;592323(2006):447–452S. doi: 10.1155/2014/592323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ali Zameer, Naseer A. Mir, Shabir A. Dhar. Case report: impending gangrene of finger secondary to constriction caused by mother’s hair. Trauma Mon. 2016:e33104. [Google Scholar]
- 20.Heffelfinger M.J., Harrison E.J. Neonatal gangrene with developmental abnormality of the femoropopliteal artery. Arch Pathol. 1971;91(3) [228–. [PubMed] [Google Scholar]
- 21.Rattan Geeta Gathwala, Singh Kadian Yogender. Idiopathic unilateral lower limb gangrene in a neonate. Indian J Dermatol. 2011;56(November-December (6)):747–748. doi: 10.4103/0019-5154.91845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Musa A.A. A review of diagnosis and modes of presentation and modes of presentation of tropical idiopathic lower limb gangrene. Afr Health Sci. 2005;6:49–50. doi: 10.5555/afhs.2006.6.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kothari P.R., Gupta A., Kulkarni B. Neonatal lower extremity gangrene. Indian Pediatr. 2005;42:1156–1158. [PubMed] [Google Scholar]
- 24.Saxena R., Kannan M., Choudhry V.P. Neonatal thrombosis. Indian J Pediatr. 2003;70(11):903–907. doi: 10.1007/BF02730597. [DOI] [PubMed] [Google Scholar]
- 25.Turnpenny P.D., Stahl S., Bowers D., Bingham P. Peripheral ischaemiaand gangrene presenting at birth. Eur J Pediatr. 1992;151(8):550–554. doi: 10.1007/BF01957717. [DOI] [PubMed] [Google Scholar]
- 26.F.T. Kraus V.I. Acheen Fetal thrombotic vasculopathy in the placenta:cerebral thrombi and infarcts coagulopathies and cerebral palsy [DOI] [PubMed]
- 27.Johnson C.F. Constricting bands. Manifestations of possible child abuse. Case reports and a review. Clin Pediatr (Phila) 1988;27(9):439–444. doi: 10.1177/000992288802700905. [DOI] [PubMed] [Google Scholar]