Abstract
Purpose
The purpose of this study was to evaluate functional results and the frequency of complications in the distal fibula Danis-Weber type B fractures caused by supination-external rotation injury in a group of lateral and antiglide plate fixation.
Methods
This prospective study evaluated 44 patients with a minimum of one-year follow-up. Patients were divided into two groups: one lateral plate group (24 patients) and group with an antiglide plate (20 patients). The patients of both groups were always positioned supine, and lateral approach was used. In the lateral plate group, the fracture was anatomically reduced, an optional anteroposterior lag screw was placed perpendicular to fracture line, and then the one-third tubular plate was applied on the lateral fibular site. In the antiglide group, the palate was implemented on the posterolateral surface of the fibula and the fracture was anatomically reduced. An optional lag-screw was used. Distal screw fixation was applied deliberately. Functional assessment according to the American Orthopaedic Foot and Ankle Society hind foot-ankle score (AOFAS) were performed at one year after surgery. The complications were recorded.
Results
According to Lauge-Hansen classification of supination-external rotation injury, a total of 27 (61.4%) patients was classified as stage 2, 2 (4.5%) patients as stage 3 and 15 (34.1%) patients with stage 4. In the lateral plate group, there were 13 (54.2%) male and 11 (45.8%) female patients. In the antiglide plate group, men comprised 12 (60%) and women 8 (40%) of patients. The AOFAS in the lateral and antiglide group performed one year after surgery was, on average, 93.7 ± 6.1 (range 85–100) and 94.5 ± 6.0 (range 85–100) points respectively. There were no statistically significant differences in both groups (p = 0.37). Complications were observed in 7 (29.3%) patients of lateral plate and 3 (15%) patients of an antiglide plate (p = 0.31). There was no case of tendinopathy. Revision surgery was performed in one patient with superficial infection.
Conclusion
In the present study, the outcome of the surgically treated Weber type B fractures caused by supination external rotation injury was comparable in both groups. The antiglide plate fixation showed no signs of peroneal tendinopathy, low rate of complications. We believe this technique is safe and a good method of fixation as well as traditional lateral plating.
Keywords: Fibula fracture, Lateral malleolus fracture, Antiglide plate, Lateral plate
1. Introduction
Danis-Weber type B ankle fractures are the most commonly occurring fractures which are mainly the result of a supination-external rotation (SER) injury characterized by the oblique shape of the fracture line.1 In such displaced fractures, anatomical length and rotational restoration of the distal fibula is required, usually by open reduction, lag screw insertion and plate fixation. A plate is applied to the lateral aspect of the fibula functioning as protection plate. Another method is posterior antiglide plating as described by Brunner and Weber in 1982.2 The antiglide plate prevents the distal oblique fragment from gliding through the proximal fragment when axial forces are applied.2 Although, there are some studies which have shown many advantages of posterior plating over lateral, still, the latter one seems to be widely favored option, even in our institution. One of the reason might be a fear of peroneal tendinopathy reported in some papers. The purpose of our study was to compare both techniques in their clinical outcomes and focus on complications.
2. Materials and methods
Between March 2014 and June 2015, we prospectively identified and treated patients with lateral malleolus fractures with Danis-Weber B type. The fractures had to be closed and caused by a supination-external rotation mechanism according to Lauge-Hansen classification. The fractures could be in the second (isolated lateral malleolus fracture), the third (lateral malleolus and posterolateral tibia fracture) or in the fourth (lateral malleolus, posterolateral tibia, and medial malleolus fracture) stage of a supination-external rotation injury. Patients younger than 18 years of age, polytraumatized, with additional lower limb injury, old and pathological fractures were excluded. We also excluded patients who did not attend the scheduled controls. Finally, we have evaluated 44 patients with a minimum of one-year follow-up. Basic demographic data (age, gender), time data (operative time, duration of hospitalization) were recorded. Patients were divided into two groups: one lateral plate group and group with an antiglide plate. Divisions were based on the operating surgeon preferences.
Surgery was performed by surgeons experienced treatment of ankle fractures. All patients had their surgery within 14 days which was depended by soft tissue conditions. The patients of both groups were always positioned supine with a slightly flexed knee. Using of a tourniquet was dependent on operating surgeon. A longitudinal, lateral skin incision was made with careful dissection of the soft tissue. In the lateral plate group, the fracture line was debrided, anatomically reduced with a temporarily applied reduction forceps. After reduction, an optional anteroposterior lag screw (3,5 mm) was placed perpendicular to fracture line and then one-third tubular plate (Poldi, Czech) was applied on the lateral fibular site (Fig. 1). In the antiglide group, the fracture line was debrided and washed out. The peritendon was not opened, and peroneal tendons were left untouched. The plate was slightly inward pre-contoured and implemented on the posterolateral surface of the fibula. In fractures with a slight displacement, the reduction was achieved by the plate screwing the first proximal screw close to the fracture line. In more displaced fractures, the distal fragment was reduced by traction with a hook and plate was screwed to the bone with a screw proximal to the fracture line. Additional proximal screws were then inserted. In the next step, an optional anteroposterior lag-screw (3,5 mm) or posteroanterior screw (trough plate) was used to secure anatomic reduction (Fig. 2). Distal screw fixation was applied in cases when movements in a fracture line were still detected. Indication for posterolateral tibia fracture fixation was primarily per-operative ankle instability and secondarily considered when fracture involves more than 1/3 of distal tibia articular surface. All patients received Redon drainage and skin was closed in anatomical layers.
Fig. 1.
Postoperative radiograph of isolated malleolar fracture treated with lateral plating with (left) and without lag screw (right).
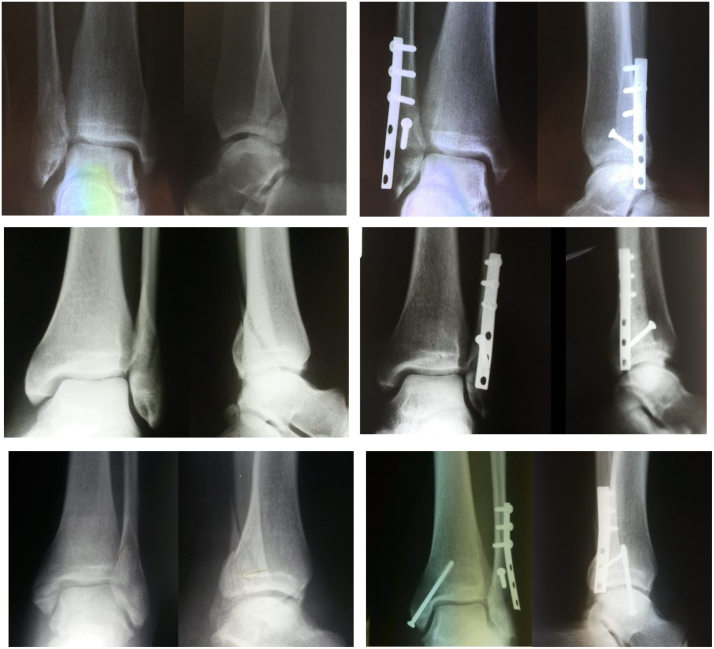
Fig. 2.
Pre and postoperative radiographs of isolated lateral malleolar (a), lateral and posterior malleolar (b) and lateral, posterior and medial malleolar (c) fractures treated with antiglide plate, anteroposterior lag screw and cancellous bone screw for medial malleolar fracture.
Postoperatively, the ankle was immobilized for a maximum of 3 weeks only if the fracture of posterior malleolus was present. Passive motion in ankle joint was allowed on the second postoperative day with the active motion after three weeks. Partial weight bearing was allowed three weeks after surgery with full weight bearing after six weeks in the antiglide group. In the patients in the lateral plating group, any weight bearing was allowed after six weeks. This division was implicated from the perspective that antiglide plate positioning is on the posterolateral part of the distal fibula, the same as direction of fracture dislocation. Radiological evaluation was performed at six weeks, three months, six months and one year after surgery. Functional assessment according to the American Orthopaedic Foot and Ankle Society hind foot-ankle score (AOFAS) were performed one year after surgery. All complications were recorded. Peroneal tendinopathy was diagnosed when there was a pain to palpation directly on the peroneal tendons and if pain presented in foot inversion and dorsal flection. If patients showed no pain but only some tenderness over the plate, this was recorded as hardware irritation. Hardware removal was advised to all patients at one year postoperatively and was undertaken anytime in symptomatic patients who wished to remove it.
Data were compared using an independent T – test, Mann-Whitney, and Fisher exact test. Testing was performed at a significance level of alpha equals 0.05. Statistical evaluation and interpretation of results used statistical programs: IBM SPSS Statistics 23.
3. Results
A total of 44 ankle fractures (24 in the lateral and 20 in the antiglide plate group) with Weber type B injury was evaluated in this study. According to Lauge-Hansen classification of supination-external rotation injury, a total of 27 (61.4%) patients was classified as stage 2, 2 (4.5%) patients as stage 3 and 15 (34.1%) patients with stage 4. The posterolateral tibia fracture was treated only in one case by anteroposterior cancellous bone screw fixation. The medial malleolus fractures were fixed by single 3.5 mm cancellous bone screw (10 cases) or by two Kirschner pins and figure of eight cerclage (4 cases) and in one instance without any fixation. In the lateral plate group, there were 13 (54.2%) male and 11 (45.8%) female. The average patient age was 42.6 ± 15.8 (range 20–72) years. In the antiglide plate group, men comprised 12 (60%) and women 8 (40%) of patients with the average age 47.9 ± 13.2 (range 29–74) years. Mean operative time in the lateral plating group was 57.5 ± 27.4 (range 20–120) minutes and 61.3 ± 13.9 (range 40–90) minutes in the antiglide group, and no statistically significant differences were found (p = 0. 29, T-test). There was also no statistically significant difference in length of hospitalization (average 4.8 versus 4.5 days) between the groups (p = 0.95, Mann-Whitney test). The most commonly used plates were six holes (n = 14; 58.3%) in the lateral plate group. A five-hole plate was used in three cases (12.5%) and seven-hole in 7 (29.2%) cases. In the antiglide group, five-hole plates were used in 8 (40%) patients. In 8 (40%) patients six-hole and in 4 (20%) patients seven-hole were used. The median number of screws distal to the fracture line in the antiglide plate was 0.5 (range 0–2); 10 (50%) fibulas with no fixation, 8 (40%) with one and 2 (10%) with two screws. The AOFAS in the lateral and antiglide group performed at one year after surgery was, on average, 93.7 ± 6.1 (range 85–100) and 94.5 ± 6.0 (range 85–100) points respectively. There were no statistically significant differences in both groups (p = 0.37, Mann-Whitney test). Complications were observed in 7 (29.3%) patients of lateral plate and 3 (15%) patients of an antiglide plate (p = 0.31, Fischer exact test) (Table 1). There was no case of tendinopathy. Hardware removal was undertaken in 9 (45%) patient in antiglide group and 19 (79.2%) patients in the lateral plating. Revision surgery was performed in one patient with superficial infection treated with negative wound pressure therapy.
Table 1.
Functional results and complications of both group.
| Group | Lauge-Hansen | Plate holes | complications Patients (%) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| stage (n) | (n) | AOFAS at 1 year |
Wound dehiscence | Wound infection | Hardware irritation | Screw Loosen-ing |
Peroneal tendino-pathy | Skin reaction | Deep venous thrombosis | |
| Lateral n = 24 |
2 (20) | 5 (3) | 93.7 (85–100) | 1(4.2) | 1(4.2) | 0 | 1(4.2) | |||
| 3 (1) | 6 (14) | 4(16.7) | ||||||||
| 4 (3) | 7 (7) | |||||||||
| Antiglide n = 20 |
2 (7) | 5 (8) | 94.5 (85–100) | 0 | 0 | 2(10) | 0 | 0 | 1(5) | |
| 3 (1) | 6 (8) | |||||||||
| 4 (12) | 7 (4) | |||||||||
| p | 0.17 | 0.37 | 0.31 | |||||||
4. Discussion
Supination-external rotation type of fracture is the most common pattern of ankle fractures. The first structure to rupture is the anterior tibiofibular ligament; however, it is discussed3. The second structure is fibula fracture followed by posterior malleolus fracture in the third stage and the fourth stage with deltoid ligament rupture or medial malleolus fracture.4 Treatment of these fractures mainly depends on its displacement. One millimeter of talus lateral displacement reduces the tibiotalar contact area in average by 42% and therefore displaced fractures necessitate anatomical restoration as prevention of post-traumatic arthrosis and possible inferior functional results.5 There are several options to fix the fractured ankle, but the most suitable type of fixation is not known. Simplest option is using just interfragmentary screws, although this is usually possible only in younger individuals with good bone quality. Other options are tension-band wire, intramedullary fixation, and the most widely used plating. External fixation is used less often.
Since 1982, when Brunner and Weber described antiglide plate technique, many authors encourage and recommended this fixation.3, 6, 7, 8, 9, 10, 11, 12 Posterior plating seems to have many advantages including non-prominent osteosynthesis material, less loss of fixation and ensure stiffer construct predominantly in osteoporotic bone compared to the lateral plating.3, 6, 13 Distal fibula fragment in the SER Weber B type fracture has a typical posterolateral displacement usually with slight shortening.7 Placing a plate in antiglide fashion automatically reduces the distal fragment by screwing the plate to proximal fragment.7 In the present study, we found this kind of reduction very helpful not only in osteoporotic bone but also in more complex lateral malleolus fractures with Le-Fort bony avulsion of the anteromedial part of the distal fibula (Fig. 3) which on the other hand might be laborious with lateral plate fixation. Axial loading is not allowed to patients early postoperatively, and therefore stiffness of the antiglide construct is not usually seen. In our institution, the patients in the antiglide group were allowed in partial weight bearing three weeks postoperatively. One patient reported unexpected pop in his operated leg even before stitches were removed. Analyzing of radiographs of this patient did not show any changes compared to previous radiographs. Another advantage of antiglide plating would be lesser dissection with shorter plates needed compared to lateral plating. A six-hole plate was used most often (56.3%) in the study by Ostrum.9 Lamontagne reported that the average plate length was a five-hole plate in their study, and the 79% of patients had screw fixation only proximal to the fracture line.14 In the present study, five and six-hole plates were mostly used plates (80%), and the 50% of fibula fractures has no distal fragment fixation.
Fig. 3.
Ankle fracture with antero-medial comminution extended laterally perfectly reduced by using the antiglide technique.
Lateral plating has traditionally been performed for fibular fracture fixation, although there are well-known weaknesses. The screws in the distal fragment often have poor purchase, can loosen and cause loss of fixation.9 The screw can penetrate to the distal tibiofibular and fibulotalar joint7, and it is therefore recommended to have a uni-cortical insertion.15 However, if distal screws are too short, it can lead to inadequate fixation.4 In our study, screw loosening was observed only in one patient in the lateral group, which was minimal and did not influence the healing. An intra-articular screw placement was not seen and we did not record any loss of reduction in both groups.
The posterolateral approach was used in several studies as the preferred method for antiglide plating.16, 7 However, some authors used a lateral approach rather than posterolateral and avoided prone patient positioning.14 The main advantage to the posterolateral approach is posterior malleolus fracture fixation.16 In our study, all patients were positioned supine, and lateral approach was used. Only one patient in the antiglide group required posterior malleolus fixation, and this was done by an anteroposterior cancellous bone screw. When comparing operative times between both groups, similar to others, we did not find statistically significant differences.9, 14, 15 However, it could be influenced by more patients with additional malleolar fractures in the antiglide group than in lateral plating group.
Peroneal tendinopathy is frequently discussed complication associated with posterior plating. Only one study showed the higher incidence of peroneal tendinitis, while 30 of 70 (43%) patients had discomfort or signs of peroneal tendinitis.13 Nine (30%) of these thirty patients had proven peroneal lesions with a significant correlation between a peroneal tendon injury and a prominent or oblique screw head in the most distal hole of the plate.13 Other studies showed a minimal presence of peroneal tendinopathy (Table 2). We recorded two patient who complained of discomfort behind the ankle in the antiglide group. However, there was no clinical evidence of peroneal lesion and no evidence during the hardware removal in those two patients. No presence of tendinopathy in our patients might be attributed to our preference for no or minimal number of screws used in the most distal plate holes.
Table 2.
Review of studies of the antiglide plate fixation since 1990 with focusing on complications and functional results at one year.
| Study (antiglide plate) | No of patients |
Wound dehiscence |
Wound infection |
Hardware irritation Discomfort |
Peroneal tendinopathy/lesions* |
Loss of fixation |
Nerve problems |
Functional results at 1 year |
|---|---|---|---|---|---|---|---|---|
| n (%) | ||||||||
| Winkler et al.6 | 93 | – | 0 | – | 0 | – | 2 (2.2) | Scale of Weber |
| 66.7% excellent results | ||||||||
| 27.9% good results | ||||||||
| 5.4% poor results | ||||||||
| Wissing et al.7 | 48 | – | 0 | – | 0 | – | – | – |
| Treadwell and Fallat8 | 70 | 0 | 0 | 0 | 2 (2.9) | lag screw | 0 | – |
| Ostrum9 | 32 | 0 | 0 | 0 | 4 (12.5) | 0 | – | Questionnaire |
| 62% very satisfied | ||||||||
| 33% moderately satisfied | ||||||||
| 5% dissatisfied | ||||||||
| Lamontagne et al.14 | 85 | 1 (1.2) | 6 (7.1) | – | 0 | plate | – | Olerud and Molander scoring system mean ankle score 91% |
| Velez et al.15 | 22 | 0 | 0 | 2 (9.1) | – | – | – | Scale of Weber |
| 13.63% excellent results | ||||||||
| 81.81% good results | ||||||||
| 4.5% poor results | ||||||||
| Weber and Krause13 | 70 | – | – | 30 (42.8) | 9 (30.0)* | – | – | – |
| Shin et al.10 | 22 | – | 0 | 0 | 2 (9.1) | 0 | – | AOFAS score |
| 80 | ||||||||
| Ha et al.12 | 49 | – | 0 | 0 | 0 | – | 0 | Ankle scoring system |
| mean ankle score 94% | ||||||||
| Ahn et al.17 | 70 | – | – | 2 (2.9) | 3 (4.3) | screw | 2 (2.9) | AOFAS score |
| 90.8 (55–100) | ||||||||
Wound dehiscence rates are higher in the lateral plate group. Lamontagne et al. reported 4 (3.7%) cases in lateral versus 1 (1.2%) case in the antiglide group.14 The rate of infection in our study was also little and was associated with wound dehiscence in the lateral plating group. The superficial peroneal nerve is another complication using lateral approach.18 In the present study, no nerve complications were observed in both groups.
In general, the clinical outcome of plating fixation of displaced Weber type – B fractures is satisfying.6, 7, 9, 14, 10, 12, 17 According to antiglide plating, poor results are infrequent. Winkler at al. reported 5.4% of poor results, similar as in the study of Velez with 4.5% of cases with poor functional results.6, 15 Ostrum observed 5% and Ahn et al., 5.97% of patients who were dissatisfied.9, 17 Our study show no dissatisfied patients in both groups.
5. Conclusion
The fear of peroneal tendinopathy is too effusive and therefore can lead to the lesser use of the antiglide plate fixation. In the present cohort, we did not find any significant differences between both groups. We did not observe peroneal tendinopathy and also other complications were not frequent. We believe that the use of the antiglide plate in a posterolateral position, without using unreasonable distal screws, is an appropriate method of fixation in every short oblique lateral malleolus fractures.
Conflict of interest
The authors have none to declare.
Authors’ contributions
All authors contributed equally to the conception and design of this paper. M.K. and P.C. carried out literature searches, quality assessments, data extraction and statistical analysis and was responsible for drafting of the manuscript. J.L. also carried out quality assessments. R.Z. and S.V. were responsible for supervision, including interpretation of data and critical revision of the manuscript. All authors read and approved the final manuscript.
Acknowledgments
Grant KEGA 071UK-4/2016
References
- 1.Lauge-Hansen N. Fractures of the ankle. II. combined experimental-surgical and experimental-roentgenologic investigations. Arch Surg. 1950;60:957–985. [PubMed] [Google Scholar]
- 2.Brunner C.F., Weber B.G. Springer-Verlag; New York: 1982. Special Techniques in Internal Fixation. [Google Scholar]
- 3.Schaffer J.J., Manoli A. The antiglide plate for Distal Fibular Fixation. A biomechanical comparsion with fixation with a lateral plate. J Bone Joint Surg. 1987;69A:596. [PubMed] [Google Scholar]
- 4.Singh R., Kamal T., Roulohamin N., Maoharan G., Ahmed B., Theobald P. Ankle fractures a literature review of current treatment methods. Open J Orthoped. 2014;4:292–303. [Google Scholar]
- 5.Ramsey P.L., Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg (Am.) 1976;58:356–357. [PubMed] [Google Scholar]
- 6.Winkler B., Weber B.G., Simpson L.A. The dorsal antiglide plate in the treatment of Danis-weber type-B factures of the distal fibula. Clin Orthop Relat Res. 1990;259:207–209. [PubMed] [Google Scholar]
- 7.Wissing J.C., van Laarhoven C.J.H.M., van der Werken C. The posterior antiglide plate for fixation of fractures of the lateral malleolus. Injury. 1992;23(2):94–96. doi: 10.1016/0020-1383(92)90040-y. [DOI] [PubMed] [Google Scholar]
- 8.Treadwell J.R., Fallat L.M. The antiglide plate for the Danis-Weber type-B fibular fracture:a review of 71 cases. J Foot Ankle Surg. 1993;32(6):573–579. [PubMed] [Google Scholar]
- 9.Ostrum R.F. Posterior plating of displaced weber B fibula fractures. J Orthop Trauma. 1996;10(3):199–203. doi: 10.1097/00005131-199604000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Shin H.K., Choi J.Y., Kang D.H. Comparative study for the fixation method in the Danis-Weber type B lateral malleolar fractures: an antiglide plate fixation versus a lateral plate fixation. J Korean Foot Ankle Soc. 2006;10(2):201–206. [Google Scholar]
- 11.Minihane K.P., Lee C.H., Ahn C.h., Zhang L.Q., Merk B.R. Comparison of lateral locking plate and antiglide plate for fixation of distal fibular fractures in osteoporotic bone: a biomechanical study. J Orthop Trauma. 2006;20:526–566. doi: 10.1097/01.bot.0000245684.96775.82. [DOI] [PubMed] [Google Scholar]
- 12.Ha W.J., Kim H.B., Ko M.S., Yoon H.K. Comparsion of antiglide plate fixation and lateral plate fixation for Danis-Weber type B isolated malleolar fractures. J Korean Foot Ankle Soc. 2011;15(3):153–158. [Google Scholar]
- 13.Weber M., Krause F. Peroneal tendon lesions caused by antiglide plate sused for fixation of lateral malleolar fractures: the effect of plate and screw position. Foot Ankle Int. 2005;26(4):281–285. doi: 10.1177/107110070502600403. [DOI] [PubMed] [Google Scholar]
- 14.Lamontagne J., Blachut P.A., Broekhuyse H.M., Oʼ Brien P.J., Meek R.N. Surgical treatment of a displaced lateral malleols Fracture: the antiglide technique versus lateral plate fixation. J Orthop Trauma. 2002;16(7):498–502. doi: 10.1097/00005131-200208000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Velez N.M., Moreno A.S., Martínez O.S., Gutiérrez E.J. Posterior antiglide plate vs lateral plate to treat Weber type B ankle fractures. Acta Ortopéd Mexicana. 2004;18(1):39–44. [Google Scholar]
- 16.Litte M.T.M., Berkes M.B., Lazaro L.E., Sculco P.K., Helfet D.L., Lorich D.G. Complications following treatment of supination external rotation ankle fractures through the posterolateral approach. Foot Ankle Int. 2013;34(4):523–529. doi: 10.1177/1071100713477626. [DOI] [PubMed] [Google Scholar]
- 17.Ahn J., Kim S., Lee J.S., Woo K., Sung K.S.S. Incidence of peroneal tendinopathy after application of a posterior antiglide plate for repair of supination external rotation lateral malleolar fractures. J Foot Ankle Surg. 2016;55:90–93. doi: 10.1053/j.jfas.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 18.Redfern D.J., Sauvé P.S., Sakellariou A. Investigation of incidence of superficial peroneal nerve injury following ankle fracture. Foot Ankle Int. 2003;24(10):771–774. doi: 10.1177/107110070302401006. [DOI] [PubMed] [Google Scholar]