Abstract
Background
Acetabular fractures are complex high-energy injuries. Increasing in recent years with the increased use of high-speed motor vehicles. One of the most important complications of acetabular fracture is the post-traumatic hip osteoarthritis; this complication has been associated to poor fracture reduction, type of fracture and delay in the reduction and fixation of acetabular fracture (Timing surgery). The aims of this study were to determine the incidence of post-traumatic hip osteoarthritis after acetabulum fracture and demonstrate whether the delay surgery is associated to early post-traumatic hip osteoarthritis.
Methods
Using the database of patients with acetabular fractures treated with open reduction and internal fixation (ORIF) over 3 years (2011–2014) with minimum of 2 years follow-up. Data was acquired and saved in a digital format. Demographic information was obtained from each patient with minimum of 2 years follow-up. Acetabular fracture was distributed according to the classification of Judet. The quality of reduction was classified in anatomic (0–1 mm) and non-anatomic (>1 mm) and the timing surgery, early (<7 days) and delay (>7 days). Clinical and radiographic follow-up was generally performed at six weeks, three months, one and two years after fracture fixation. Multivariate logistic regression analyses were performed to assess the strength of the covariates in relation to the development of post-traumatic hip osteoarthritis.
Results
59 (48%) patients of 122, developed post-traumatic hip osteoarthritis before 2 years. Posterior wall fracture with or without transverse fracture was associated with higher post-traumatic hip osteoarthritis compared with other types of fractures (p < 0.05). Patients with better anatomical reduction had less post-traumatic hip osteoarthritis compared with those who had nonanatomic reduction (p < 0.05). There was no evidence of association between early timing of the surgical procedure and the presence post-traumatic hip osteoarthritis (p = 7092).
Conclusions
According to our results, the anatomical reduction of the articular surface in acetabular fractures is the most important factor in hip osteoarthritis prevention. This factor is strongly associated with early surgical treatment, preferably done within seven days. The timing surgery it is not a factor associated with post-traumatic osteoarthritis.
Keywords: Acetabular fractures, Timing surgery, Post-traumatic, Hip osteoarthritis, Delay surgery, Accuracy of reduction
1. Introduction
Acetabular fractures are life-altering injuries that commonly occur in young, active, and productive members of society, although the number of elderly patients sustaining acetabular fractures has increased.1 The main goal of treatment of fractures of the acetabulum is to preserve the native hip joint, so that it can continue to function for the remainder of the patient́s life.1, 2 Acetabular fractures are complex high-energy injuries, increasing in recent years along with the increased use of high-speed motor vehicles.1, 2, 3, 4, 5 The diagnosis and classification of acetabular fractures is based on radiographic findings. the most widely used classification is Letournel's, but also the classification of the AO is widely accepted, which is more specific but with greater complexity which is why its use is limited.6, 7, 8, 9 One of the most important complications of acetabular fracture is the hip osteoarthritis; this complication has been associated mainly to poor fracture reduction, the type of fracture and the delay in the reduction and fixation of acetabular fracture (Timing surgery).2, 5, 10 The aims of this study were to determine the incidence of post-traumatic hip osteoarthritis after acetabulum fracture and demonstrate whether the delay in surgery is associated to early post-traumatic hip osteoarthritis.
2. Methods
This study was approved by our local institutional review board. Using the database of patients with acetabular fractures treated with open reduction and internal fixation (ORIF) over 3 years (2011–2014) with minimum of 2 years follow-up. Data was acquired and saved in a digital format. Demographic information was obtained from each patient which included age (years), sex, and BMI, mechanism of injury, timing of surgery, classification of the fracture and complication as well as follow-up and patients with hip osteoarthritis demonstrated by radiography, according to the classification of hip osteoarthritis by Bombelli.11 Acetabular fractures that were treated non-operatively, those that required acute primary total hip, and those in which the acetabular fracture was periprosthetic were excluded. Surgical site infections were also excluded, because if it’s narrow association with implant loosening or avascular necrosis of the femoral head.
All patients were evaluated with the use of five standard radiographic views: anteroposterior radiograph, two Judet views, cephalic and caudal views of the pelvis. All patients were further evaluated with computed tomography (CT) of the pelvis. Each fracture was classified on the basis to the method of Letournel and Judet.12 Patients were divided into 2 groups: Those, which are operated within 7 days (early surgery), and those operated after 7 days (delay surgery). Each group was analyzed by the accuracy of reduction, measurements of the greatest residual displacement of any of the six acetabular reference lines of Letournel and Judet. The reduction was graded as anatomical (0–1 mm of residual displacement) or non-anatomical (>1 mm). Clinical and radiographic follow-up was generally performed at six weeks, three months, one and two years after fracture fixation.
3. Statistical analysis
SPSS version 21 statistical software (Chicago, Illinois, United States) was utilized to perform the statistical analyses. The chi-square test was used to compare the categorical data. A p value less that 0.05 with the two-tailed test was considered statistically significant. Multivariate logistic regression analyses were performed to assess the strength of the covariates (Timing surgery, type of fracture, accuracy of reduction, age, gender and BMI) in relation to the development of post-traumatic hip osteoarthritis, emphasizing the placed upon impact of timing surgery. A threshold for statistical significance was also established at p < 0.05.
4. Results
According to the data collected, 147 patients were initially obtained. Exclusion criteria were applied to eleven patients that present surgical site infection during follow-up (7%), fourteen had avascular necrosis of the femoral head.
Of the 122 patients remaining, 90 (74%) male and 32 (26%) were female. Mean age was 41 years (range 20–79 years) with a mean duration of follow-up of 2.4 years. We found 59 (48%) patients with development of post-traumatic hip osteoarthritis before 2 years. No difference was found between age, gender, BMI and post-traumatic hip osteoarthritis (p > 0.05). (Table 1)
Table 1.
Demographics. *Average age. OA = Osteoarthritis.
| No (%) | Hip OA (%) | |
|---|---|---|
| Total | 122 (100) | 59 (48) |
| Gender | ||
| Male | 90 (74) | 44 (36) |
| Female | 32 (32) | 15 (12) |
| Age* | 20–79 (41) | |
| Type of accident | ||
| Car accident | 70 (57) | |
| Motorcycle accident | 32 (26) | |
| Fall (3 m heights) | 20 (16) | |
| Intensive Care Unit (ICU) | 16 (13) | |
| Sciatic nerve injury (before surgery) | 21 (17) | |
| Sciatic nerve injury (after surgery) | 5 (4) | |
The mechanism of injury was high-energy trauma in all cases (100%) (70 car accidents, motorcycle 32 and 20 falling more than 3 m high). 16 patients (13%) had associated lesions, which required admission to the ICU for hemodynamic stabilization. 30 patients with associated dislocation, 24 were reduced closed form within 24 h of admission, remaining 6, continued dislocated between 24 and 48 h, due to delay in the transfer to a first level hospital, skeletal traction was used until surgery in all cases. Directly related to trauma 21 (17%) patients had neurological symptoms from admission with sciatic nerve injury. Six patients (4%) had sciatic nerve injury after surgery, all by posterior approach. Two of them clinically recovered at 3 months, two at 6 months and one patient at 12 months.
4.1. Type of fracture and hip osteoarthritis
Of the 122 acetabular fractures, 80 (65%) had a simple fracture pattern and 42 (34%) had an associated fracture pattern. Of the 59 patients with post-traumatic hip osteoarthritis, 12 (9%) were associated with transverse fractures, 26 (21%) had posterior wall fracture, 19 (16%) had transverse with posterior wall fracture and 2 (2%) had both columns fracture. Patients with anterior column and anterior wall fracture did not present hip osteoarthritis at 2 years.
Patients with posterior wall fracture, and with transverse plus posterior wall fracture being higher rate of post-traumatic arthritis compared with other types of fracture (p < 0.05) (Fig. 1)
Fig. 1.
Post-traumatic hip osteoarthritis and type of fracture.
4.2. Accuracy of reduction
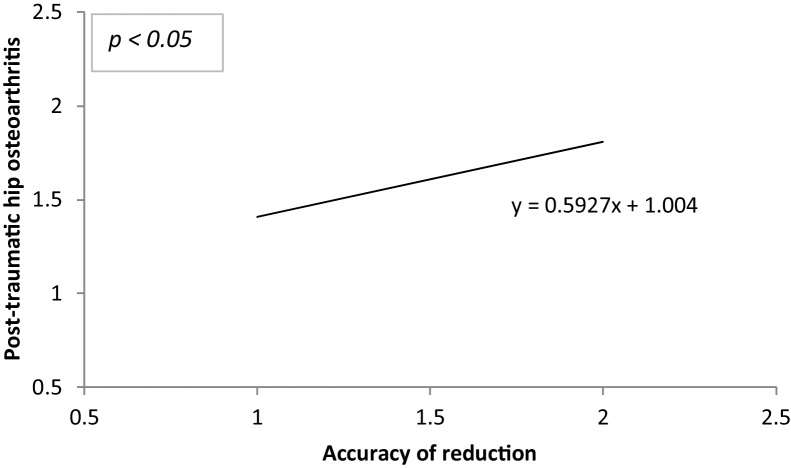
The postoperative reduction was graded as anatomical in 75 (61%) patients and nonanatomic in 47 (39%). Patients with better anatomical reduction had less post-traumatic hip osteoarthritis compared with those who had nonanatomic reduction (24:35 p < 0.05). The rate of anatomical reduction was significantly higher in hips with simple fracture (posterior wall fracture mainly) compared with associated fracture types (p < 0.05). Fractures with involvement of the quadrilateral plate had a significantly lower rate of anatomic reduction (p = 0.05). (Fig. 2)
Fig. 2.
Post-traumatic hip osteoarthritis distribution with timing surgery and accuracy of reduction.
4.3. Timing surgery
The average time between injury and surgery was 11 days ± 7.5 days with a range from 4 to 18 days. The main reason why the surgery was performed after 7 days was because our hospital is not a trauma center and operating room time is shared with other specialties. 83 patients were operated after 7 days (41 with anatomic reduction), and 39 within 7 days (34 with anatomic reduction). In the univariate analyses, it was found that the post-traumatic hip osteoarthritis was lower in patients who were operated within the first 7 days compared with those operated after 7 days (OR: 0.2393, 95% CI: 0.1031 to 0.5550 p < 0.05). When analyzed, the relationship between timing surgery and quality of reduction, better results are found in patients who underwent surgery within 7 days (OR: 0.1162, 95% CI: 0.0418 to 0.3230 p < 0.0001) (Fig. 2, Fig. 3).
Fig. 3.
The multivariate regression model shows association between accuracy of reduction of fracture and post-traumatic hip osteoarthritis. (p < 0.05).
Based on the multivariate regression analyses, an association between the type of fracture (95% CI: −0.1966 to −0.041 p < 0.001), the quality of reduction (95% CI: 0.3643 to 0.8241 p < 0.0001) and the presence of post-traumatic hip osteoarthritis was identified. (Fig. 4)
Fig. 4.
The multivariate regression model shows no association between timing surgery of and post-traumatic hip osteoarthritis. (p > 0.05).
There was no evidence of association between early timing of the surgical procedure and the presence post-traumatic hip osteoarthritis (95% CI: −0.2572 to 0.1755 p = 0.7092), for either age (95% CI: −0.0066 to 0.0083 p = 0.82), gender (95% CI: −0.2591 to 0.1181 p = 0.46) or body mass index (BMI) (95% CI: −0.0118 to 0.050 p = 0.22) (Table 2).
Table 2.
Results.
| N = 122 (100%) | # Hip Osteoarthritis | P value | |
|---|---|---|---|
| Univariate analyses | |||
| Quality of reduction | <0.05 | ||
| Anatomical | 75 (61) | 24 | |
| Non-anatomical | 47 (39) | 35 | |
| Timing Surgery | <0.05 | ||
| Early <7 days | 39 (32) | 13 | |
| Delay >7 days | 83 (68) | 46 | |
| Multivariate analyses (regression) | |||
| Quality of reduction | 0.00001 | ||
| Type of fracture | 0.001 | ||
| Timing Surgery | 0.70 | ||
| Age | 0.82 | ||
| Gender | 0.46 | ||
| BMI | 0.22 | ||
5. Discussion
In the retrospective analysis, we examined 122 patients from 2011 to 2014 with acetabular fracture provided epidemiological data that coincides with recent literature. The male-female ratio of 3:1 was comparable with other series.1, 2, 3, 13, 14, 15 Age distribution was also broadly similar to literature reports, with a mean age of 41.5 years, a range of 20–79 years and a median of 41 years.1, 14, 15 There have been many reports of poor functional outcomes in patients aged over 65 years, and some authors recommend primary hip arthroplasty.16 In our series, 9 patients were older than 60 years and needed arthroplasty before 1 year. In view of the poor results in elderly osteoporotic patients, Spencer recommended restricting internal fixation to younger subjects.17 The distribution of fracture types varies between series1, 4, 14, 18, 19, 20, and in our series we found that simple fractures were more frequent, a total of 65%.
Studies that report poor results in acetabular fractures are those restricted to posterior wall, transverse plus posterior wall or complex posterior wall fractures.21, 22, 23, 24 Posterior wall fracture account for a poor prognosis due to the high rate of comminution, which results in lack of stability, or posterior wall defects leading to secondary osteoarthritis. In our series posterior wall fractures, was the most associated with hip osteoarthritis.
Any patient experiencing hip dislocation should be reduced urgently in the first 24 h to reduce the risk of avascular necrosis of the femoral head.25 The decision of which surgical approach to perform is directly related to the type of fracture.26, 27 For transverse fractures, posterior column and posterior wall, a Kocher-Langenbeck approach is recommended, and in the case of anterior wall fracture and/or anterior column fractures, an ilioinguinal approach is preferred.26, 27, 28, 29, 30 Recently, the use of a modified Stoppa approach proposed a surgical option for fracture with medial displacement of the quadrilateral plate along with a direct exposure of the fracture zone, but the learning curve for this approach is high.31, 32 In our study, a Stoppa approach was not performed. We believe the use of this approach could improve the reduction in patients with displacement of the quadrilateral plate (Fig. 5, Fig. 6, Fig. 7, Fig. 8, Fig. 9 )
Fig. 5.
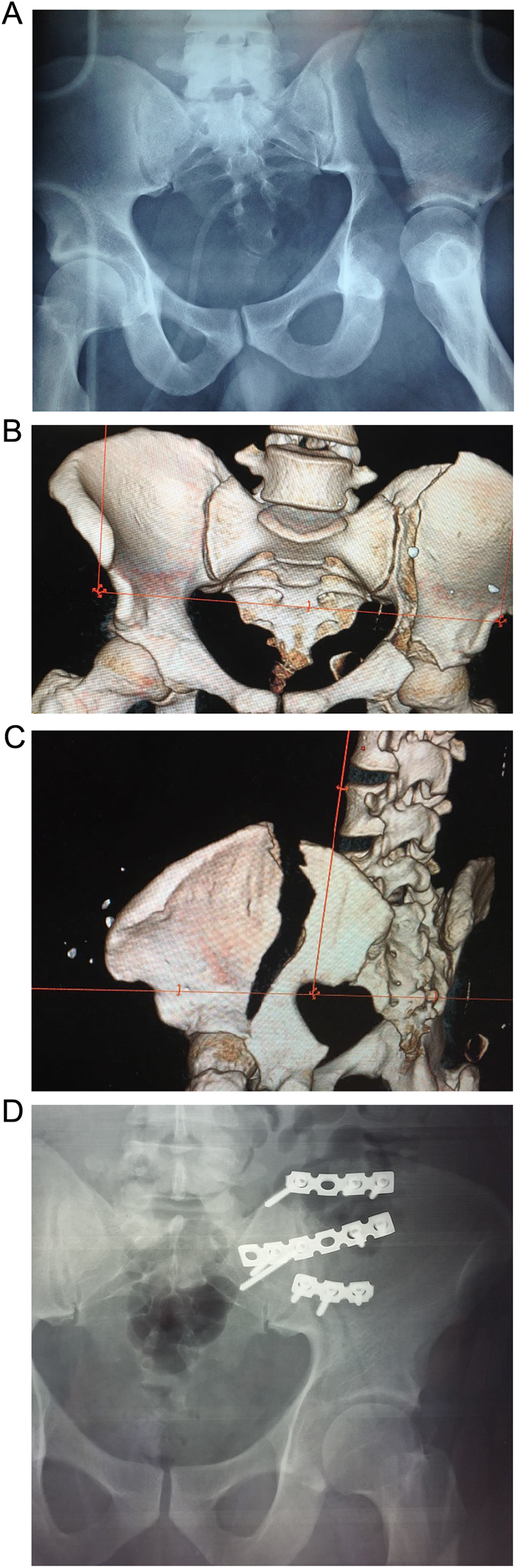
Anterior column fracture.
Fig. 6.

Posterior wall fracture with severe upper osteoarthritis with rise of the femoral head.
Fig. 7.
Posterior wall fracture with upper outer and inferomedially osteoarthritis.
Fig. 8.
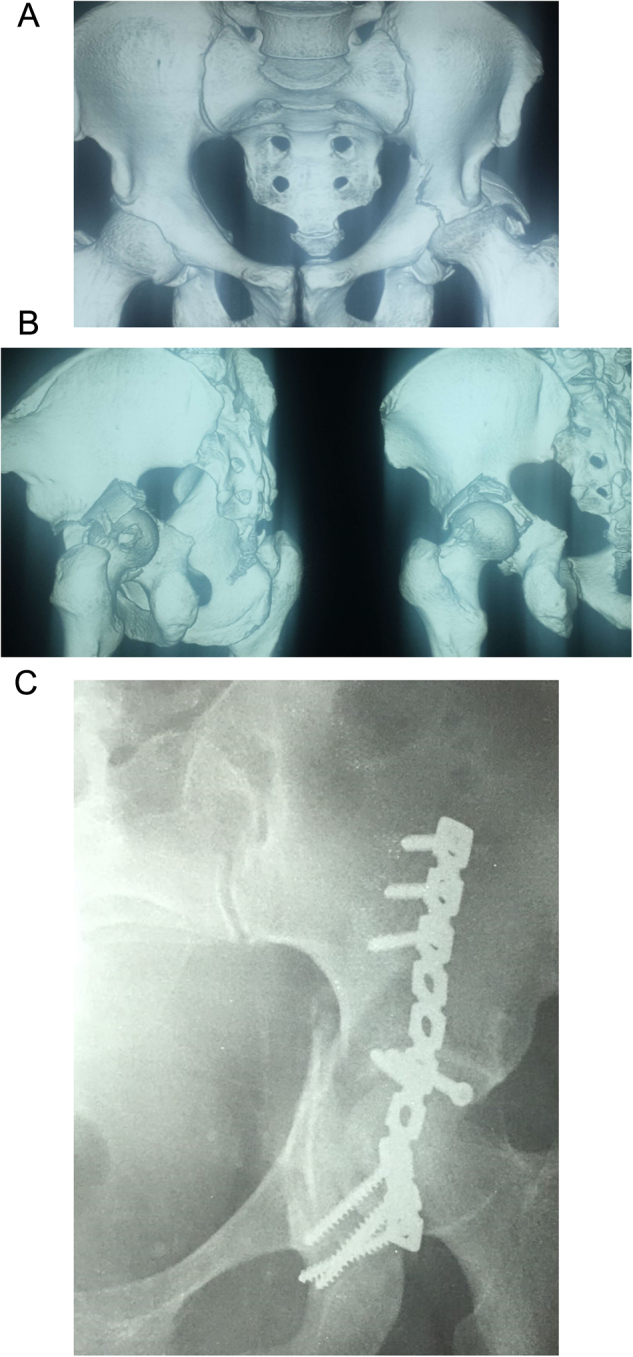
Transverse plus posterior wall fracture with upper outer osteoarthritis.
Fig. 9.

Transverse fracture.
Many authors have highlighted the need for optimal reduction to improve functional results, as anatomical reduction has shown to be the most important factor to prevent the development of osteoarthritis.33, 34, 35, 36, 37 It has been shown that the damage of articular cartilage affects anatomical fracture reduction.37
The present findings showed that surgical intervention within seven days of the fracture, significantly improves anatomic fracture reduction this is compared to other series.38, 39 The mobilization of the fragments is easier when surgery is done early, unlike of patients operated after seven days. We hypothesized that the timing of the surgical procedure is a variable directly associated to the presence of post-traumatic hip osteoarthritis, but were not able to confirm this. Along with surgical timing, the gender, age and body mass index of the patients did not seem to influence the development of post-traumatic hip osteoarthritis. The fracture type and quality of reduction were the main significant factors determining the presence of post-traumatic hip osteoarthritis. We considered this analysis accurate given the considerable number of patients included in the study.
The incidence of post-traumatic hip osteoarthritis due to acetabular fracture, within two years follow-up was 48%. We believe this is a high rate compared to other studies.40, 41 Due to the fact that our hospital is not a specialized trauma center, the treatment of acetabular fractures and pelvis in multiply injured patients is delayed.
6. Conclusions
The present study highlights the importance of initial reduction. This study lacks a full statistical analysis, mainly because of it is categorical variables and noncontinuous. The same surgeon did not perform the surgeries, and we believe this may affect surgical outcomes. According to our results, the anatomical reduction of the articular surface in acetabular fractures is the most important factor in hip osteoarthritis prevention. This factor is strongly associated with early surgical treatment, preferably done within seven days. The timing surgery it is not a factor associated with post-traumatic osteoarthritis.
Conflict of interest
None.
References
- 1.Prevezas N. Evolution of pelvic and acetabular surgery from ancient to modern times. Injury. 2007;38(April (4)):397–409. doi: 10.1016/j.injury.2007.01.035. [DOI] [PubMed] [Google Scholar]
- 2.Morshed S., Knops S., Jurkovich G.J., Wang J., MacKenzie E., Rivara F.P. The impact of trauma-center care on mortality and function following pelvic ring and acetabular injuries. J Bone Joint Surg Am. 2015;97(February (4)):265–272. doi: 10.2106/JBJS.N.00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gänsslen A., Oestern H.J. Acetabular fractures. Chirurg. 2011;82(December (12)):1133–1148. doi: 10.1007/s00104-011-2135-3. [quiz 1149-50] [DOI] [PubMed] [Google Scholar]
- 4.Lawrence D.A., Menn K., Baumgaertner M., Haims A.H. Acetabular fractures: anatomic and clinical considerations. AJR Am J Roentgenol. 2013;201(September (3)):W425–W436. doi: 10.2214/AJR.12.10470. [DOI] [PubMed] [Google Scholar]
- 5.Gettys F.K., Russell G.V., Karunakar M.A. Open treatment of pelvic and acetabular fractures. Orthop Clin North Am. 2011;42(January (1)):69–83. doi: 10.1016/j.ocl.2010.08.006. [vi] [DOI] [PubMed] [Google Scholar]
- 6.Cimerman M., Kristan A. Preoperative planning in pelvic and acetabular surgery: the value of advanced computerized planning modules. Injury Int J Care Injured. 2007;38:442–449. doi: 10.1016/j.injury.2007.01.033. [DOI] [PubMed] [Google Scholar]
- 7.Schmidt-Rohlfing B., Reilmann H., Pape H.C. Fractures of the acetabulum. Diagnostic and therapeutic strategies. Unfallchirurg. 2010;113(March (3)):217–229. doi: 10.1007/s00113-010-1748-1. [DOI] [PubMed] [Google Scholar]
- 8.Prevezas N., Antypas G., Louverdis D., Konstas A., Papasotiriou A., Sbonias G. Proposed guidelines for increasing the reliability and validity of Letournel. Injury Int J Care Injured. 2009;40:1098–1103. doi: 10.1016/j.injury.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 9.Smith R.M., Frcs M.D. AO principles of fracture management. J Bone Joint Surg Am. 2002;84(July (7)) 1293-1293. [Google Scholar]
- 10.Meena U.K., Tripathy S.K., Sen R.K., Aggarwal S., Behera P. Predictors of postoperative outcome for acetabular fractures. Orthopaedics Traumatol: Surg Res. 2013;99:929–935. doi: 10.1016/j.otsr.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 11.Bombelli R. Classification of coxarthrosis as the basis of operative joint salvage therapy. Biomechanics of cranial-lateral hip arthrosis; aim and technique of extension-valgisation osteotomy; aim and technique of extension-varus osteotomy, results. Orthopade. 1979;8(May (3)):245–263. [PubMed] [Google Scholar]
- 12.Saterbak A.M., Marsh J.L., Turbett T., Brandser E. Acetabular fractures classification of Letournel and Judet–a systematic approach. Iowa Orthop J. 1995;15:184–196. [PMC free article] [PubMed] [Google Scholar]
- 13.Reilmann H., Weinberg A.M. Surgical approaches, choice of approach and surgical techniques for internal stabilization of acetabulum fractures. Orthopade. 1992;21(November (6)):442–448. [PubMed] [Google Scholar]
- 14.Magala M., Popelka V., Božík M., Heger T., Zamborský V., Šimko P. Conservative treatment of acetabular fractures: epidemiology and medium-term clinical and radiological results. Acta Chir Orthop Traumatol Cech. 2015;82(1):5160. [PubMed] [Google Scholar]
- 15.Laird A., Keating J.F. Acetabular fractures: a 16-year prospective epidemiological study. J Bone Joint Surg Br. 2005;87:969–973. doi: 10.1302/0301-620X.87B7.16017. [DOI] [PubMed] [Google Scholar]
- 16.Mears D.C. Surgical treatment of acetabular fractures in elderly patients with osteoporotic bone. J Am Acad Orthop Surg. 1999;7(March-April (2)):128–141. doi: 10.5435/00124635-199903000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Spencer R.F. Acetabular fracture in older patients. J Bone Joint Surg Br. 1989;71:774–776. doi: 10.1302/0301-620X.71B5.2584245. [DOI] [PubMed] [Google Scholar]
- 18.Moed B.R., Yu P.H., Gruson K.I. Functional outcomes of acetabular fractures. J Bone Joint Surg Am. 2003;85:1879–1883. doi: 10.2106/00004623-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Matta J.M., Anderson L.M., Epstein H.C., Hendricks P. Fractures of the acetabulum: a retrospective analysis. Clin Orthop Relat Res. 1986;(April (205)):230–240. [PubMed] [Google Scholar]
- 20.Kumar A., Shah N.A., Kershaw S.A., Clayson A.D. Operative management of acetabular fractures. A review of 73 fractures. Injury. 2005;36(May (5)):605–612. doi: 10.1016/j.injury.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 21.Mears D.C., Velyvis J.H., Chang C.P. Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res. 2003;(February (407)):173–186. doi: 10.1097/00003086-200302000-00026. [DOI] [PubMed] [Google Scholar]
- 22.Kreder H.J., Rozen N., Borkhoff C.M. Determinants of functional outcome after simple and complex acetabular fractures involving the posterior wall. J Bone Joint Surg Br. 2006;88(June (6)):776–782. doi: 10.1302/0301-620X.88B6.17342. [DOI] [PubMed] [Google Scholar]
- 23.Scheinfeld M.H., Dym A.A., Spektor M., Avery L.L., Dym R.J., Amanatullah D.F. Acetabular fractures: what radiologists should know and how 3D CT can aid classification. Radiographics. 2015;35(March-April (2)):555–577. doi: 10.1148/rg.352140098. [DOI] [PubMed] [Google Scholar]
- 24.Baumgaertner M.R. Fractures of the posterior wall of the acetabulum. J Am Acad Orthop Surg. 1999;7(January (1)):54–65. doi: 10.5435/00124635-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Milenković S., Mitković M., Saveski J. Avascular necrosis of the femoral head in the patients with posterior wall acetabular fractures associated with dislocations of the hip. Acta Chir Iugosl. 2013;60(2):65–69. doi: 10.2298/aci1302065m. [DOI] [PubMed] [Google Scholar]
- 26.Reilmann H., Weinberg A.M. Surgical approaches, choice of approach and surgical techniques for internal stabilization of acetabulum fractures. Orthopade. 1992;21(November (6)):442–448. [PubMed] [Google Scholar]
- 27.Sarlak A.Y., Selek O., Inanir M., Musaoglu R., Baran T. Management of acetabular fractures with modified posterior approach to spare external hip rotators. Injury Int J Care Injured. 2014;45:732–737. doi: 10.1016/j.injury.2013.11.010. [DOI] [PubMed] [Google Scholar]
- 28.Alexa O., Malancea R.I., Puha B., Luncă S., Veliceasa B. Results of surgical treatment of acetabular fractures using Kocher-Langenbeck approach. Chirurgia (Bucur) 2013;108(November-December (6)):879–885. [PubMed] [Google Scholar]
- 29.Fan X.H., Shi P.S., Xue Y., Zhou S.G., Deng X.W., Li X.S. Case-control study on the modified ilioinguinal incision of anterior approach for the treatment of pelvic and acetabular fractures. Zhongguo Gu Shang. 2014;27(April (4)):335–340. [PubMed] [Google Scholar]
- 30.Elmadağ M., Güzel Y., Acar M.A., Uzer G., Arazi M. The Stoppa approach versus the ilioinguinal approach for anterior acetabular fractures: a case control study assessing blood loss complications and function outcomes. Orthopaedics Traumatol: Surg Res. 2014;100:675–680. doi: 10.1016/j.otsr.2014.05.020. [DOI] [PubMed] [Google Scholar]
- 31.Kim H.Y., Yang D.S., Park C.K., Choy W.S. Modified stoppa approach for surgical treatment of acetabular fracture. Clin Orthop Surg. 2015;7(March (1)):29–38. doi: 10.4055/cios.2015.7.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kurylo J.C., Templeman D., Mirick G.E. Perfect reduction: approaches and techniques. Injury. 2015;46(March (3)):441–444. doi: 10.1016/j.injury.2014.11.027. [DOI] [PubMed] [Google Scholar]
- 33.Moed B.R., Yu P.H., Gruson K.I. Functional outcomes of acetabular fractures. J Bone Joint Surg Am. 2003;85:1879–1883. doi: 10.2106/00004623-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Levine R.G., Renard R., Behrens F.F. Biomechanical consequences of secondary congruence after both-column acetabular fracture. J Orthop Trauma. 2002;16:87–91. doi: 10.1097/00005131-200202000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Ovre S., Madsen J.E., Roise O. Acetabular fracture displacement, roof arc angles and 2 years outcome. Injury. 2008;39:922–931. doi: 10.1016/j.injury.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 36.Rommens P.M., Ingelfinger P., Nowak T.E., Kuhn S., Hessmann M.H. Traumatic damage to the cartilage influences outcome of anatomically reduced acetabular fractures: a medium-term retrospective analysis. Injury. 2011;42:1043–1048. doi: 10.1016/j.injury.2011.03.058. [DOI] [PubMed] [Google Scholar]
- 37.Sen R.K., Veerappa L.A. Long-term outcome of conservatively managed displaced acetabular fractures. J Trauma. 2009;67:155–159. doi: 10.1097/TA.0b013e31819db092. [DOI] [PubMed] [Google Scholar]
- 38.Johnson E.E., Matta J.M., Mast J.W., Letournel E. Delayed reconstruction of acetabular fractures 21–120 days following injury. Clin Orthop Relat Res. 1994;305:20–30. [PubMed] [Google Scholar]
- 39.Dailey S.K., Phillips C.T., Radley J.M., Archdeacon M.T. Achieving anatomic acetabular fracture reduction – when is the best time to operate? J Orthop Trauma. 2016;(March (11)) doi: 10.1097/BOT.0000000000000576. [DOI] [PubMed] [Google Scholar]
- 40.Boudissa M., Ruatti S., Kerschbaumer G., Milaire M., Merloz P., Tonetti J. Part 2: outcome of acetabular fractures and associated prognostic factors-a ten-year retrospective study of one hundred and fifty six operated cases with open reduction and internal fixation. Int Orthop. 2015;(December (21)) doi: 10.1007/s00264-015-3070-6. [DOI] [PubMed] [Google Scholar]
- 41.Briffa N., Pearce R., Hill A.M., Bircher M. Outcomes of acetabular fracture fixation with ten years' follow-up. J Bone Joint Surg Br. 2011;93(February (2)):229–236. doi: 10.1302/0301-620X.93B2.24056. [DOI] [PubMed] [Google Scholar]