Abstract
Purpose of review
Our 24/7 society is dependent on shift work, despite mounting evidence for negative health outcomes from sleep displacement due to shift work. This paper reviews short- and long-term health consequences of sleep displacement and circadian misalignment due to shift work.
Recent findings
We focus on four broad health domains: metabolic health; risk of cancer; cardiovascular health; and mental health. Circadian misalignment affects these domains by inducing sleep deficiency, sympathovagal and hormonal imbalance, inflammation, impaired glucose metabolism, and dysregulated cell cycles. This leads to a range of medical conditions, including obesity, metabolic syndrome, type II diabetes, gastrointestinal dysfunction, compromised immune function, cardiovascular disease, excessive sleepiness, mood and social disorders, and increased cancer risk.
Summary
Interactions of biological disturbances with behavioral and societal factors shape the effects of shift work on health and well-being. Research is needed to better understand the underlying mechanisms and drive the development of countermeasures.
Keywords: Circadian Misalignment, Sleep Displacement, Metabolic Health, Cancer Risk, Heart Health, Mental Health
Introduction
It has long been recognized that shift work has a negative impact on health and well-being. Historically this has been attributed to adverse effects of long work hours, nighttime light exposure, and psychosocial factors—effects that are still recognized as relevant for tolerance to shift work [1,2]. However, the health consequences of shift work should first be understood in terms of a fundamental misalignment between the circadian (i.e., near-24-hour) rhythm of the endogenous biological clock and the timing of the sleep/wake cycle [3]. While this paper is concerned primarily with the long-term health consequences of shift work, the implications of circadian misalignment between the biological clock and the sleep/wake cycle are perhaps best illustrated by how such misalignment increases the risk of workplace accidents and injuries.
In healthy, non-shift workers with normal sleep patterns, daytime wakefulness is driven by the biological clock, which produces circadian rhythmicity driving increased alertness during the daytime and decreased alertness during the nighttime [4,5]. This circadian process is counteracted by a homeostatic pressure for sleep, which builds across waking hours [6,7]. When working during daytime hours, these two processes function in concert and in synchrony with the environmental light/dark cycle to maintain alertness while awake and at work, while allowing for consolidated sleep during the night. Working nights or early morning shifts means that an individual must be awake when the circadian drive for alertness is low and asleep when it is high, in opposition to the natural biological rhythm. This leads to shortened and disrupted sleep, and excessive sleepiness while awake [8,9]. This in turn yields increased errors in the workplace, greater risk of accidents and injuries, and degraded health [10,11].
Society is increasingly dependent on around-the-clock operations that require shift work. Many industries and services rely on a continuous workforce, including manufacturing, energy production, transportation, healthcare, law enforcement, and the military. Based on data collected in the US in 2004 (the last time such data were comprehensively collected), the protective services (police, fire, correction services) have the highest percentage of night and rotating shift workers of any occupation (24.8%), followed by healthcare providers (10.9%) [12]. Such workers, when assigned night shifts, early morning shifts or rotating shifts, must modify their sleep schedules from the normal nighttime hours, placing the individuals into a condition of circadian misalignment. In 2004, out of more than 15 million US employees working full time on shift or irregular schedules, 5.7 million worked schedules requiring work hours that displace sleep and force wakefulness to be misaligned with the natural circadian rhythm [12]. Given this relatively high prevalence, it is important to understand the impact of circadian misalignment resulting from shift work on workers’ health.
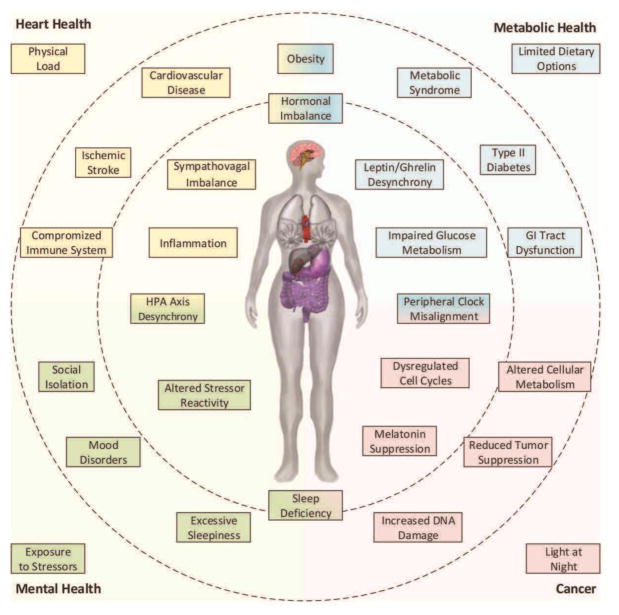
In this paper, we review short- and long-term biological effects associated with displacing the sleep/wake cycle. We also discuss the role of psychosocial factors in the expression of these effects and their impact on health and well-being. There is a wide range of medical conditions potentially caused or influenced by shift work, and an exhaustive overview of the literature in this area is beyond the scope of the paper. Rather, we focus on four broad health domains that illustrate important components of the health consequences of shift work: metabolic health, risk of cancer, heart health, and mental health, as illustrated in Figure 1.
Figure 1.
Human pathophysiology due to shift work. In this paper, we discuss four broad components of health that are adversely affected by circadian misalignment due to shift work: heart health (top left quadrant), metabolic health (top right quadrant), cancer risk (bottom right quadrant), and mental health (bottom left quadrant). The inner circle represents biological systems that are disturbed by circadian misalignment, and the outer area represents broad psychosocial factors that interact with these disturbed biological systems. The ring between them illustrates key medical conditions that may arise from the interaction, for which shift workers are at elevated risk.
Metabolic Health
Sleep displacement and altered meal timing due to shift work disturb hormonal balance—including key regulators of satiety and hunger, the hormones leptin and ghrelin, respectively [13]. Leptin reduces appetite and signals for the cessation of food intake. In addition to showing transient increases after meals, leptin levels display a circadian rhythm driven by the biological clock [13]. Ghrelin is a short-acting hormone that stimulates appetite. Ghrelin levels decrease after meals and normally display a reverse diurnal pattern from leptin [14]. Ghrelin levels are related to time fasting (i.e., time between meals) and have a central role in mediating food-seeking behavior and motivation, food intake, and body weight [15,16,17].
Under normal circumstances, ghrelin and leptin work in concert to regulate feeding behavior with appropriate meal timing, size, and nutrients. However, in shift workers, meal times must be altered in accordance with the displaced sleep/wake schedule, which disrupts the coordination between leptin and ghrelin and dysregulates downstream biological systems related to diet, weight, and metabolism. Laboratory studies focused on the immediate effects of circadian misalignment have demonstrated decreased leptin levels [13,18] and blunted post-meal suppression of ghrelin [19]. If findings from laboratory sleep restriction studies generalize to shift work, then this may be expected to promote weight gain through enhanced appetite for calorie-dense foods with high carbohydrate content [20], consumption of food at night, and increased caloric intake overall [21]. Indeed, night shift workers tend to have significantly higher body mass index (BMI) and greater waist-to-hip ratio than day shift workers [22,23,24].
Sleep displacement and altered meal timing due to shift work also disturb glucose metabolism [25], through mechanisms that have yet to be elucidated. In mice, chronic advances of meal time appear to induce insulin resistance, while chronic delays appear to elevate blood glucose levels [26]. In humans, presumably as a long-term consequence of altered glucose metabolism, shift work is associated with increased risk of type II diabetes [27,28]. Deteriorating glycemic control and glucose intolerance are also associated with shift work [29,30,31]. For long-term shift workers (>10 years), the increased risk of diabetes persists into retirement [28]. Exacerbating this problem is that night shift workers tend to crave calorie-dense foods with high carbohydrate content while on shift [32]. All-night fast food restaurants, vending machines, and institutional dining facilities cater to this by serving predominantly processed and fried foods. The increased diabetes risk may be further amplified by unhealthy changes in lifestyle associated with shift work (e.g., smoking, alcohol consumption, and lack of exercise) [33].
Metabolic syndrome and diabetes risk may be further increased by the timing of eating and food digestion being out of sync with peripheral oscillators in the liver [34] and gut [35]. Over the long run, physiological maladaptation to eating at abnormal circadian times is associated with developing metabolic syndrome (MetS) [36,37,38]. Working at night has been estimated to increase the risk of developing MetS by more than 50% [37]. Although moderators such as diet, exercise, and body weight are important, the evidence of a general connection between shift work and poor metabolic health is strong.
There is some emerging evidence that long-term exposure to sleep displacement alters the composition of the gut microbiota (i.e., the bacteria in the gastrointestinal tract) [39]. Recent work indicates that the gut microbiome shows diurnal variations that are influenced by meal times and disturbed by circadian misalignment [40]. The gut microbiome both responds and contributes to host energy balance, and disruption is associated with inflammation, insulin resistance, and adiposity [41]. Disrupted rhythmicity in the gut microbiome may be involved in an immediate and frequently reported, yet hitherto poorly understood, effect of shift work, namely, gastrointestinal discomfort [42,43]. Dysfunction of the gastrointestinal tract may also explain the significantly higher rate of ulcers in night workers compared to day workers [44], and may have impactful consequences for shift workers’ long-term health.
Cancer
The master circadian pacemaker, orchestrating rhythmicity throughout the body, is located in the suprachiasmatic nuclei (SCN) of the hypothalamus. Peripheral systems, organs, and cells also have their own circadian rhythms, a phenomenon commonly referred to as peripheral oscillators [45]. These peripheral oscillators are normally in sync with the master clock in the SCN, but altered sleep/wake schedules associated with shift work may desynchronize them [46].
Maintaining synchronized circadian rhythms in peripheral systems is critical for the fine-tuning of cellular processes including cell cycles, DNA repair, apoptosis (i.e., controlled cell death), and immune modulation [47]. Circadian misalignment may alter the rhythms of cellular circadian clocks, and it is believed that this may increase the risk of cancer [48]. Findings in animal models with environmentally disturbed circadian systems (simulated shift work) indicate that circadian disruption increases the progression of cancer, possibly through dysregulation of the cell cycle, accumulation of DNA damage, and reduced tumor suppression [49,50,51,52].
Another factor possibly involved in the link between circadian misalignment and cancer risk is the hormone melatonin. This hormone is produced by the pineal gland and normally secreted at night, with the timing of secretion regulated by the master circadian pacemaker in the SCN [53]. Circulating melatonin levels can be disrupted by circadian misalignment, as well as by nocturnal exposure to light—bright light has a direct (i.e., non-circadian) suppressing effect on melatonin secretion [54,55]. Importantly, melatonin is protective against oxidative DNA damage [56]. Thus, when melatonin is suppressed, naturally occurring DNA damage may accumulate faster than it can be repaired, which may contribute to the increased risk of cancer that has been observed among shift workers [57].
Based on information from animal models and epidemiological evidence from the shift-working population, the International Agency for Research on Cancer (IARC) of the World Health Organization (WHO) has classified night shift work as a probable carcinogen, while acknowledging that there is currently limited evidence from human studies [58]. Indeed, research findings regarding shift work and cancer have been mixed. That said, many studies have reported an association between shift work exposure and increased risk of breast cancer [59,60]. Night shift work has also been found to increase the risk of other cancers, including lung, colon, bladder, prostate, rectal, and pancreatic cancer as well as non-Hodgkin’s lymphoma [61,62,63]. However, a number of studies have found no association between cancer and shift work [64,65,66,67]. The variability in these findings may be related to other contributing factors, such as individual differences in susceptibility to carcinogenesis, occupational exposure to carcinogenic agents, and lifestyle [68,69]. Taken together, the literature suggests that further studies are needed to quantify and understand the relationship between shift work and risk of cancer.
Heart Health
The master circadian pacemaker in the SCN of the hypothalamus is centrally located at the nexus of a number of neuroendocrine systems, one of which is the hypothalamic-pituitary-adrenal (HPA) axis. The HPA axis produces a number of neurotransmitters and hormones, such as epinephrine (adrenalin) and norepinephrine (noradrenalin) as well as cortisol, with widespread effects across a range of biological systems. The production of epinephrine and norepinephrine influences the interaction between the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS), which is referred to as sympathovagal balance.
Circadian misalignment causes internal desynchronization of the HPA axis [70,71]. Sympathovagal balance is then disrupted [72], as indicated by changes in heart rate variability that are believed to reflect increased risk of cardiovascular disease (CVD) [73]. The SNS is most active in times of heightened physiological arousal, and is often referred to as the “fight or flight” system. The PNS is most active in times of reduced physiological arousal, and is sometimes referred to as the “rest and digest” system. The dysregulation of these systems can have immediate and fatal consequences, such as sudden cardiac arrest. In law enforcement, approximately 7% of line of duty deaths are due to a fatal heart attack [74]. These deaths overwhelmingly occur when officers stress the sympathovagal system during times of desynchronization, such as during nighttime physical confrontations [75].
Working night shifts and rotating shifts has been associated with elevated risk of heart disease [76] and ischemic stroke [77,78]. Working nights also raises the prevalence of metabolic risk factors associated with these conditions [79]. However, adverse heart health outcomes seem to be tied not only to shift work and circadian misalignment, but also the presence of psychological and psychosocial stressors [80,81]. Chronic stress associated with shift work has been associated with an increased risk for coronary heart disease in both blue- and white-collar workers [82]. Changes in lifestyle habits associated with shift work do not appear to account for the elevated risk of coronary heart disease in these populations [83]. Despite the established link between circadian misalignment and hormone regulation related to heart health, the specific mechanisms connecting shift work and CVD remain elusive.
Candidate mechanisms underlying elevated risk for CVD due to shift work include disrupted 24-hour rhythms of blood pressure [84] and vascular function [85], atherosclerosis [86], proinflammatory states [87], and altered lipid and glucose metabolism [88]. Shift work-related metabolic dysfunction and the various health consequences thereof, including obesity, metabolic syndrome, and type II diabetes (discussed above), also potentiate the development of CVD [88,89]. Adipokines (cell signaling proteins) secreted by fat tissue and involved in immune responses—and more generally the development of a compromised immune system due to circadian misalignment—may connect these different factors [90]. Further research into candidate mechanisms must consider not only circadian misalignment from shift work, but also socioeconomic indicators and occupational factors (e.g., physical/mental workload, workplace stressors) known to be associated with poor heart health [91].
Mental Health
As described above, circadian misalignment disrupts the internal synchronization of the HPA axis. Persistent stimulation of the HPA axis by external stressors in the face of circadian misalignment may lead to erosion of mental health in shift workers. Stimulation of the (desynchronized) HPA axis activates the fear system and blunts the reward system, leading to abnormal responses to stress [92]. As such, shift workers exposed to stressors at night may experience difficulty managing physiological and mental responses to these stressors.
The HPA axis hormone cortisol, which is central to the body’s responses to stressors [93], has been used in many studies as an index of responsivity to stressors. Cortisol levels normally exhibit a pronounced circadian rhythm with a peak in the morning hours. Night shift work has been found to shift the timing of the cortisol rhythm [94], and rotating shift work has been reported to dampen the rhythms’ amplitude [95]. Although it is unclear whether disruption of cortisol rhythms is causally involved, it is generally believed that shift work leads to heightened stress reactivity and—in those who are especially susceptible—the development of insomnia and shift work disorder [96]. In fact, the impact of altered stressor responses on the quality of sleep may be a critical mediator of emotion regulation [97], resilience to stress [98], and ultimately tolerance for shift work [1]. As many as 20% of shift workers ultimately opt out of shift work due to sleep disturbances and adverse stress reactions [82].
Although every occupation has the potential to be stressful, the protective services and healthcare occupations are inherently so [99,100]. These two occupational families also have a large proportion of staff working nights and rotating shifts. In addition to normal workplace stressors, the protective services and healthcare workers are often exposed to dangerous and traumatic events. Moreover, shift work can reduce contact with psychosocial factors that protect against stress. For example, shift schedules tend to limit social interactions—thus reducing social support [101]—and diminish sex life satisfaction [102]. Such work–life interference, whether perceived or real, has been found to be one of the most significant indicators of marital dissatisfaction for both shift workers and their partners [103].
HPA axis desynchrony due to circadian misalignment, increased exposure to stressors during night work, and reduced access to protective psychosocial factors lead to an increase in long-term adverse health outcomes. For example, law enforcement professionals have a significantly higher risk of suicide and stress-related and mood disorders [104] than the general public. More research is needed to understand the mechanisms that underlie the interaction between chronic exposure to circadian misalignment and workplace stressors and the development of mental health disorders.
Conclusion
The empirical evidence suggests that circadian misalignment is associated with a range of short- and long-term, negative health outcomes related to metabolic and gastrointestinal health, cancer, heart health, and mental health (see Figure 1). However, these associations are complex and nuanced, with many mediating and moderating factors. When considering the impact of shift work on health and well-being, it is essential to also consider the effects of behavioral, societal and environmental forces that may ameliorate or exacerbate the biological consequences of circadian misalignment.
The potential for workers to self-select out of shift work causes a systematic confound in population health research known as the “healthy worker effect” [105]. Shift workers experiencing degraded health or well-being may transfer to the day-working population, leaving the shift work cohort relatively healthier and the day work cohort relatively less so. Complicating matters further, many of the effects of shift work on health develop gradually over time, and may not manifest until workers have ceased to work shifts [106]. This is particularly common in occupations that assign shift types based on seniority, where the more junior (typically younger and healthier) individuals work the shifts most likely to displace sleep. The overarching implication is that the health consequences of shift work may be greater yet than what the available literature would already suggest at face value.
Despite mounting evidence for negative health effects, a significant portion of the population continues to be willing to engage in shift work. Workers may have a variety of reasons for dealing with the physiological and psychological consequences of shift work in their chosen occupation, including financial considerations, child care arrangements, or personal preference [12]. Some occupations have high barriers for entry (e.g., educational achievement, vocational training, psychological or background screening) and form the source of an individual’s identity (e.g., nurses, police officers, soldiers). These occupations may retain shift workers that are not well adapted to circadian misalignment because the financial, social, and psychological capital invested to enter the occupation may outweigh the negative aspects of shift work.
Shift work-induced circadian misalignment not only affects sleep and health, it also determines when people can exercise, eat, socialize, and have sex—all factors that support physical and mental health. Workers typically learn through experience the importance of getting to sleep as soon as possible at the end of a night shift in order to optimize sleep duration, while they may not explicitly understand the underlying circadian and homeostatic processes of sleep regulation. This results in competition between the need for sleep and other demands, such as exercise, healthy eating, and personal care. These latter activities are then often done quickly or to a lesser standard (e.g., fast food), or foregone altogether, making it difficult for shift workers to maintain a healthy lifestyle [107]. To illustrate this point, health promotion efforts focusing on healthy eating habits for shift workers are available [108,109]. However, actually making healthier meal choices—at odds with the night shift-induced cravings and the limited availability of healthy food options at night—is not only time-consuming but tends to be more expensive as well. Increased sleepiness and worsened mood associated with night work make it even more difficult to maintain a healthy lifestyle, and are a further impediment to change.
There is an urgent need for research to better understand the mechanisms that underlie the interactions between sleep displacement and circadian misalignment on the one hand, and behavioral and societal factors on the other hand, in shaping adverse health outcomes for shift workers. Such research is going to be critical to drive the development of effective countermeasures, without which workers—and ultimately society—continue to bear the cost of shift work-related health problems.
Footnotes
Conflict of Interest
James Stephen, Kimberly Honn, Shobhan Gaddameedhi, and Hans Van Dongen each declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Härmä M. Individual differences in tolerance to shiftwork: a review. Ergonomics. 1993;36(1–3):101–9. doi: 10.1080/00140139308967860. [DOI] [PubMed] [Google Scholar]
- 2.Saksvik IB, Bjorvatn B, Hetland H, Sandal GM, Pallesen S. Individual differences in tolerance to shift work-a systematic review. Sleep Med Rev. 2011;15:221–35. doi: 10.1016/j.smrv.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Kogi K. International research needs for improving sleep and health of workers. Industrial Health. 2005;43:71–9. doi: 10.2486/indhealth.43.71. [DOI] [PubMed] [Google Scholar]
- 4.Edgar DM, Dement WC, Fuller CA. Effect of SCN lesions on sleep in squirrel monkeys: Evidence for opponent processes in sleep-wake regulation. J Neurosci. 1993;13(3):1065–79. doi: 10.1523/JNEUROSCI.13-03-01065.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dijk DJ, Czeisler CA. Paradoxical timing of the circadian rhythm of sleep propensity serves to consolidate sleep and wakefulness in humans. Neurosci Lett. 1994;166(1):63–8. doi: 10.1016/0304-3940(94)90841-9. [DOI] [PubMed] [Google Scholar]
- 6.Borbély AA. A two process model of sleep regulation. Hum Neurobiol. 1982;1(3):195–204. [PubMed] [Google Scholar]
- 7.Daan S, Beersma DGM, Borbély AA. Timing of human sleep: recovery process gated by a circadian pacemaker. Am J Physiol. 1984;246:R161–78. doi: 10.1152/ajpregu.1984.246.2.R161. [DOI] [PubMed] [Google Scholar]
- 8.Åkerstedt T. Shift work and disturbed sleep/wakefulness. Occup Med. 2003;53:89–94. doi: 10.1093/occmedkqg046. [DOI] [PubMed] [Google Scholar]
- 9.Van Dongen HPA, Dinges DF. Sleep, circadian rhythms, and psychomotor vigilance. Clin Sports Med. 2005;24(2):237–49. doi: 10.1016/j.csm.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 10.Folkard S, Lombardi DA, Tucker PT. Shiftwork: safety, sleepiness and sleep. Industrial Health. 2005;43(1):20–3. doi: 10.2486/indhealth.43.20. [DOI] [PubMed] [Google Scholar]
- 11.Van Dongen HPA, Balkin TJ, Hursh SR. Performance deficits during sleep loss and their operational consequences. In: Kryger M, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. Philadelphia: Academic; 2016. pp. 682–88. [Google Scholar]
- 12.United States Department of Labor: Bureau of Labor Statistics. [Accessed 28 February 2017];Workers on flexible and shift schedules in May 2004. 2004 http://www.bls.gov/cps/
- 13.Nguyen J, Wright KP., Jr Influence of weeks of circadian misalignment on leptin levels. Nat Sci Sleep. 2009;2:9–18. doi: 10.2147/NSS.S7624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schoeller DA, Cella LK, Sinha MK, Caro JF. Entrainment of the diurnal rhythm of plasma leptin to meal timing. J Clin Invest. 1997;100(7):1882–7. doi: 10.1172/JCI119717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abizaid A, Lui Z, Andrews ZB, Shanabrough M, Borok E, Elsworth JD, et al. Ghrelin modulates the activity and synaptic input organization of midbrain dopamine neurons while promoting appetite. J of Clin Inves. 2006;116(12):3229–40. doi: 10.1172/JCI29867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klok MD, Jakobsdottir S, Drent ML. The role of leptin and ghrelin in the regulation of food intake and body weight in humans: a review. Obesity Rev. 2007;8(1):21–34. doi: 10.1111/j.1467-789X.2006.00270.x. [DOI] [PubMed] [Google Scholar]
- 17.Ferrini F, Salio C, Lossi L, Merighi A. Ghrelin in central neurons. Curr Neuropharmacol. 2009;7(1):37–49. doi: 10.2174/157015909787602779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18••.McHill AW, Melanson EL, Higgins J, Connick E, Moehlman TM, Stothard ER, et al. Impact of circadian misalignment on energy metabolism during simulated nightshift work. PNAS. 2014;111(48):17302–7. doi: 10.1073/pnas.1412021111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schiavo-Cardozo D, Lima MMO, Pareja JC, Geloneze B. Appetite-regulating hormones from the upper gut: disrupted control of xenin and ghrelin in night workers. Clin Endocrinol. 2013;79(6):807–11. doi: 10.1111/cen.12114. [DOI] [PubMed] [Google Scholar]
- 20.Spiegel K, Tasali E, Penev P, Van Cauter E. Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–50. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 21.Spaeth AM, Dinges DF, Goel N. Effects of experimental sleep restriction on weight gain, caloric intake, and meal timing in healthy adults. Sleep. 2013;36(7):981–90. doi: 10.5665/sleep.2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morikawa Y, Nakagawa H, Miura K, Soyama Y, Ishizaki M, Kido T, et al. Effect of shift work on body mass index and metabolic parameters. Scand J Work Environ Health. 2007;33(1):45–50. doi: 10.5271/sjweh.1063. [DOI] [PubMed] [Google Scholar]
- 23.Zhao I, Bogossian F, Turner C. Does maintaining or changing shift types affect BMI? A longitudinal study. J Occup Environ Med. 2012;54(5):525–31. doi: 10.1097/JOM.0b013e31824e1073. [DOI] [PubMed] [Google Scholar]
- 24.Siqueria K, Griep R, Rotenberg L, Silva-Costa A, Fonseca M. Weight gain and body mass index following change from daytime to night shift – a panel study with nursing professionals. Chronobiol Int. 2016;33(6):776–9. doi: 10.3109/07420528.2016.1167719. [DOI] [PubMed] [Google Scholar]
- 25.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354(9188):1435–9. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 26.Yoon JA, Han DH, Noh JY, Kim MH, Son GH, Kim K, et al. Meal time shift disturbs circadian rhythmicity along with metabolic and behavioral alterations in mice. PLoS ONE. 2012;7(8):e44053. doi: 10.1371/journal.pone.0044053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pan A, Schernhammer ES, Sun Q, Hu FB. Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Med. 2011;3(12):e1001141. doi: 10.1371/journal.pmed.1001141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28•.Knutsson A, Kempe A. Shift work and diabetes—a systematic review. Chronobiol Int. 2014;31(10):1146–51. doi: 10.3109/07420528.2014.957308. [DOI] [PubMed] [Google Scholar]
- 29.De Bacquer D, Van Risseghem M, Clays E, Kittel F, De Backer G, Braeckman L. Rotating shift work and the metabolic syndrome: a prospective study. Int J Epidemiol. 2009;38(3):848–54. doi: 10.1093/ije/dyn360. [DOI] [PubMed] [Google Scholar]
- 30.Li Y, Sato Y, Yamaguchi N. Shift Work and the Risk of Metabolic Syndrome: A Nested Case-Control Study. Int J Occup Environ Health. 2011;17(2):154–60. doi: 10.1179/107735211799030960. [DOI] [PubMed] [Google Scholar]
- 31.Oyama I, Kubo T, Fujino Y, Kadowaki K, Kunimoto M, Shirane K, et al. Retrospective cohort study of the risk of impaired glucose tolerance among shift workers. Scand J Work Environ Health. 2012;38(4):337–42. doi: 10.5271/sjweh.3297. [DOI] [PubMed] [Google Scholar]
- 32.Heath G, Roach GD, Dorrian J, Ferguson SA, Darwent D, Sargent C. The effect of sleep restriction on snacking behavior during a week of simulated shiftwork. Accid Anal Prev. 2012;45S:62–7. doi: 10.1016/j.aap.2011.09.028. [DOI] [PubMed] [Google Scholar]
- 33.Suwazono Y, Sakata K, Okubo Y, Harada H, Oishi M, Kobayasho E, et al. Long-tern longitudinal study on the relationship between alternating shift work and the onset of diabetes mellitus in male Japanese workers. J Occup Environ Med. 2006;48(5):455–62. doi: 10.1097/01.jom.0000214355.69182.fa. [DOI] [PubMed] [Google Scholar]
- 34•.Zwighaft Z, Reinke H, Asher G. The liver in the eyes of a chronobiologist. J Biol Rhythms. 2016;31(2):115–24. doi: 10.1177/0748730416633552. [DOI] [PubMed] [Google Scholar]
- 35.Schieving LA. Biological clocks and the digestive system. Gastroenterology. 2000;119(2):536–49. doi: 10.1053/gast.2000.9305. [DOI] [PubMed] [Google Scholar]
- 36.Antunes LC, Levandovski R, Dantas G, Caumo W, Hidalgo MP. Obesity and shift work: chronobiological aspects. Nutr Res Rev. 2010;23:155–68. doi: 10.1017/S0954422410000016. [DOI] [PubMed] [Google Scholar]
- 37.Wang F, Zhang L, Zhang Y, Zhang B, He Y, Xie S, et al. Meta-analysis on night shift work and risk of metabolic syndrome. Obes Rev. 2014;15:709–20. doi: 10.1111/obr.12194. [DOI] [PubMed] [Google Scholar]
- 38••.Proper KI, van de Langenberg D, Rodenberg W, Vermeulen RCH, van der Beek AJ, van Steeg H, et al. The relationship between shift work and metabolic risk factors. Am J Prev Med. 2016;50(5):el47–57. doi: 10.1016/j.amepre.2015.11.013. [DOI] [PubMed] [Google Scholar]
- 39•.Reynolds AC, Paterson JL, Ferguson SA, Stanley D, Wright KP, Jr, Dawson D, et al. The shift work and health research agenda: Considering changes in gut microbiota as a pathway linking shift work, sleep loss and circadian misalignment, and metabolic disease. Sleep Med Rev. 2016 doi: 10.1016/j.smrv.2016.06.009. pii:S1087-0792(16)30061-2. [DOI] [PubMed] [Google Scholar]
- 40•.Broussard JL, Van Cauter E. Disturbances of sleep and circadian rhythms: novel risk factors for obesity. Curr Opin Endocrinol Diabetes Obes. 2016;23(5):353–9. doi: 10.1097/MED.0000000000000276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ley RE. Obesity and the human microbiome. Curr Opinion Gastro. 2010;26(1):5–11. doi: 10.1097/MOG.0b013e328333d751. [DOI] [PubMed] [Google Scholar]
- 42.Knutsson A. Health disorders of shift workers. Occup Med. 2003;53:103–8. doi: 10.1093/occmed/kqg048. [DOI] [PubMed] [Google Scholar]
- 43.Nojkov B, Rubenstein JH, Chey WD, Hoogerwerf WA. The impact of rotating shift work on the prevalence of irritable bowel syndrome in nurses. Am J Gastroenterol. 2010;105:842–7. doi: 10.1038/ajg.2010.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pietroiusti A, Forlini A, Magrini A, Galante A, Coppeta L, Gemma G, et al. Shift work increases the frequency of duodenal ulcer in H pylori infected workers. Occup Environ Med. 2006;63:773–5. doi: 10.1136/oem.2006.027367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nagoshi E, Saini C, Bauer C, Laroche T, Naef F, Schibler U, et al. Circadian gene expression in individual fibroblasts: Cell-autonomous and self-sustained oscillators pass time to daughter cells. Cell. 2004;119:693–705. doi: 10.1016/j.cell.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 46••.Ackermann K, Plomp R, Lao O, Middleton B, Revell VL, Skene DJ, et al. Effect of sleep deprivation on rhythms of clock gene expression and melatonin in humans. Chronobiol Int. 2013;30(7):901–9. doi: 10.3109/07420528.2013.784773. [DOI] [PubMed] [Google Scholar]
- 47.Fu L, Kettner NM. The circadian clock in cancer development and therapy. Prog Mol Biol Transl Sci. 2013;119:221–82. doi: 10.1016/B978-0-12-396971-2.00009-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48•.Sancar A, Lindsey-Boltz LA, Gaddameedhi S, Selby CP, Ye R, Chiou YY, et al. Circadian clock, cancer, and chemotherapy. Biochemistry. 2015;54(2):110–23. doi: 10.1021/bi5007354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee S, Donehower LA, Herron AJ, Moore DD, Fu L. Disrupting circadian homeostasis of sympathetic signaling promotes tumor development in mice. PLoS ONE. 2010;5(6):e10995. doi: 10.1371/journal.pone.0010995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50•.Kettner NM, Voicu H, Finegold MJ, Coarfa C, Sreekumar A, Putluri N, et al. Circadian homeostasis of liver metabolism suppresses hepatocarcinogenesis. Cancer Cell. 2016;30(6):909–24. doi: 10.1016/j.ccell.2016.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51•.Papagiannakopoulos T, Bauer MR, Davidson SM, Heimann M, Subbaraj L, Bhutkar A, et al. Circadian rhythm disruption promotes lung tumorigenesis. Cell Metab. 2016;24(2):324–31. doi: 10.1016/j.cmet.2016.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52•.Van Dycke KC, Rodenburg W, van Oostrom CT, van Kerkhof LW, Pennings JL, Roenneberg T, et al. Chronically alternating light cycles increase breast cancer risk in mice. Curr Biol. 2015;25(14):1932–7. doi: 10.1016/j.cub.2015.06.012. [DOI] [PubMed] [Google Scholar]
- 53.Reiter RJ. The melatonin rhythm: both a clock and a calendar. Experientia. 1993;49(8):654–64. doi: 10.1007/BF01923947. [DOI] [PubMed] [Google Scholar]
- 54.Lewy AJ, Wehr TA, Goodwin FK, Newsome DA, Markey SP. Light suppresses melatonin secretion in humans. Science. 1980;2010(4475):1267–9. doi: 10.1126/science.7434030. [DOI] [PubMed] [Google Scholar]
- 55.Czeisler CA, Shanahan TL, Klerman EB, Martens H, Brotman DJ, Emens JS, et al. Suppression of melatonin secretion in some blind patients by exposure to bright light. N Engl J Med. 1995;332(1):6–11. doi: 10.1056/NEJM199501053320102. [DOI] [PubMed] [Google Scholar]
- 56.Rodriguez C, Mayo JC, Sainz RM, Antolín I, Herrera F, Martín V, et al. Regulation of antioxidant enzymes: a significant role for melatonin. J Pineal Res. 2004;36(1):1–9. doi: 10.1046/j.1600-079x.2003.00092.x. [DOI] [PubMed] [Google Scholar]
- 57••.Bhatti P, Mirick DK, Randolph TW, Gong J, Buchanan DT, Zhang JJ, et al. Oxidative DNA damage during sleep periods among nightshift workers. Occup Environ Med. 2016;73(8):537–44. doi: 10.1136/oemed-2016-103629. [DOI] [PubMed] [Google Scholar]
- 58.Straif K, Baan R, Grosse Y, Secretan B, El Ghissassi F, Bouvard V, et al. Carcinogenicity of shift-work, painting, and fire-fighting. Lancet Oncol. 2007;8(12):1065–6. doi: 10.1016/S1470-2045(07)70373-X. [DOI] [PubMed] [Google Scholar]
- 59.He C, Anand ST, Ebell MH, Vena JE, Robb SW. Circadian disrupting exposures and breast cancer risk: a meta-analysis. Int Arch Occup Environ Health. 2015;88(5):533–47. doi: 10.1007/s00420-014-0986-x. [DOI] [PubMed] [Google Scholar]
- 60.Lin X, Chen W, Wei F, Ying M, Wei W, Xie X. Night-shift work increases morbidity of breast cancer and all-cause mortality: a meta-analysis of 16 prospective cohort studies. Sleep Med. 2015;16(11):1381–7. doi: 10.1016/j.sleep.2015.02.543. [DOI] [PubMed] [Google Scholar]
- 61.Erren TC, Pape HG, Reiter RJ, Piekarski C. Chronodisruption and cancer. Naturwissenschaften. 2008;95:367–82. doi: 10.1007/s00114-007-0335-y. [DOI] [PubMed] [Google Scholar]
- 62.Parent M, El-Zein M, Rousseau M, Pintos J, Siemiatycki J. Night work and risk of cancer among men. Am J of Epidemiol. 2012;176(9):751–9. doi: 10.1093/aje/kws318. [DOI] [PubMed] [Google Scholar]
- 63.Rao D, Yu H, Bai Y, Zheng X, Xie L. Does night-shift work increase the risk of prostate cancer? A systematic review and meta-analysis. Onco Targets Ther. 2015;8:2817–26. doi: 10.2147/OTT.S89769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pesch B, Harth V, Rabstein S, Baisch C, Schiffermann M, Pallapies D, et al. Night work and breast cancer-results from the German GENICA study. Scand J Work Environ Health. 2010;36(2):134–41. doi: 10.5271/sjweh.2890. [DOI] [PubMed] [Google Scholar]
- 65.Kubo T, Oyama I, Nakamura T, Kunimoto M, Kadowaki K, Otomo H, et al. Industry-based retrospective cohort study of the risk of prostate cancer among rotating shift workers. Int J Urol. 2011;18:206–11. doi: 10.1111/j.1442-2042.2010.02714.x. [DOI] [PubMed] [Google Scholar]
- 66.Pronk A, Ji B, Shu X, Xue S, Yang G, Li H, et al. Night-shift work and breast cancer risk in a cohort of Chinese women. Am J Epidemiol. 2010;171(9):953–9. doi: 10.1093/aje/kwq029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67•.Travis RC, Balkwill A, Fensom GK, Appleby PN, Reeves GK, Wang SX, et al. Night shift work and breast cancer incidence: three prospective studies and a meta-analysis of published studies. J Natl Cancer Inst. 2016;108(12):djw169. doi: 10.1093/jnci/djw169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fritschi L, Glass DC, Heyworth JS, Aronson K, Girschik J, Boyle T, et al. Hypothesis for mechanisms linking shiftwork and cancer. Med Hypothesis. 2011;77:430–6. doi: 10.1016/j.mehy.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 69.Purdue MP, Hutchings SJ, Rushton L, Silverman DT. The proportion of cancer attributable to occupational exposures. Ann Epidemiol. 2015;25(3):188–92. doi: 10.1016/j.annepidem.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kalsbeek A, van der Spek R, Lei J, Endert E, Buijs RM, Fliers E. Circadian rhythms in the hypothalamo-pituitary-adrenal (HPA) axis. Mol Cell Endocrinol. 2012;349(1):20–9. doi: 10.1016/j.mce.2011.06.042. [DOI] [PubMed] [Google Scholar]
- 71.Gonnissen HK, Hulshof T, Westerterp-Plantenga MS. Chronobiology, endocrinology, and energy- and food-reward homeostasis. Obes Rev. 2013;14(5):405–16. doi: 10.1111/obr.12019. [DOI] [PubMed] [Google Scholar]
- 72••.Grimaldi D, Carter JR, Van Cauter E, Leproult R. Adverse impact of sleep restriction and circadian misalignment on autonomic function in healthy young adults. Hypertension. 2016;68(1):243–50. doi: 10.1161/HYPERTENSIONAHA.115.06847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Boudreau P, Dumont GA, Boivin DB. Circadian adaptation to night shift work influences sleep, performance, mood and the autonomic modulation of the heart. PLoS ONE. 2013;8(7):e70813. doi: 10.1371/journal.pone.0070813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zimmerman FH. Cardiovascular disease and risk factors in law enforcement personnel: a comprehensive review. Cardio Rev. 2012;20:159–66. doi: 10.1097/CRD.0b013e318248d631. [DOI] [PubMed] [Google Scholar]
- 75.Varvarigou V, Farioli A, Korre M, Dahabreh IJ, Kales SN. Law enforcement duties and sudden cardiac death among police officers in the United States: case distribution study. BMJ. 2014;349:g6534. doi: 10.1136/bmj.g6534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pimenta AM, Kac G, De Souza RRC, Ferreira LMBA, Silqueira SMF. Night-shift work and cardiovascular risk among employees of a public university. Rev Assoc Med Bras. 2011;58(2):168–77. doi: 10.1016/S2255-4823(12)70177-7. [DOI] [PubMed] [Google Scholar]
- 77.Hermansson J, Gådin KG, Karlsson B, Lindahl B, Stegmayr B, Knutsson A. Ischemic stroke and shift work. Scand J Work Environ Health. 2007;33(6):435–9. doi: 10.5271/sjweh.1165. [DOI] [PubMed] [Google Scholar]
- 78.Brown DL, Feskanich D, Sanchez BN, Rexrode KM, Schernhammer ES, Lisabeth LD. Rotating night shift work and the risk of ischemic stroke. Am J Epidemiol. 2009;169(11):1370–7. doi: 10.1093/aje/kwp056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ha M, Park J. Shiftwork and metabolic risk factors of cardiovascular disease. J Occup Health. 2005;47:89–95. doi: 10.1539/joh.47.89. [DOI] [PubMed] [Google Scholar]
- 80.Szosland D. Shift work and metabolic syndrome, diabetes mellitus and ischemic heart disease. Int J Occup Med Environ Health. 2010;23(3):287–91. doi: 10.2478/v10001-010-0032-5. [DOI] [PubMed] [Google Scholar]
- 81.Thomas C, Power C. Shift work and risk factors for cardiovascular disease: a study at age 45 years in the 1958 British birth cohort. Eur J Epidemiol. 2010;156(Pt 6):1661–72. doi: 10.1099/mic.0.037804-0. [DOI] [PubMed] [Google Scholar]
- 82.Tenkanen L, Sjoblom KR, Kalimo R, Alikoski T, Härmä M. Shift work, occupation and coronary heart disease over 6 years of follow-up in the Helsinki Heart Study. Scand J Work Environ Health. 1997;23:257–65. doi: 10.5271/sjweh.218. [DOI] [PubMed] [Google Scholar]
- 83.van Amelsvoort LG, Schouten EG, Kok FJ. Impact of one year of shift work on cardiovascular disease risk factors. J Occup Environ Med. 2004;46(7):699–706. doi: 10.1097/01.jom.0000131794.83723.45. [DOI] [PubMed] [Google Scholar]
- 84.Smolensky MH, Hermida RC, Portaluppi F. Circadian mechanisms of 24-hour blood pressure regulation and patterning. Sleep Med Rev. 2016 doi: 10.1016/j.smrv.2016.02.003. pii:S1087-0792(16)00019-8. [DOI] [PubMed] [Google Scholar]
- 85•.Rodrigo GC, Denniff M. Time-of-day variation in vascular function. Exp Physiol. 2016;101(8):1030–4. doi: 10.1113/EP085780. [DOI] [PubMed] [Google Scholar]
- 86.Haupt CM, Alte D, Dorr M, Robinson DM, Felix SB, John U, et al. The relation of exposure to shift work with atherosclerosis and myocardial infarction in a general population. Atherosclerosis. 2008;201(1):205–11. doi: 10.1016/j.atherosclerosis.2007.12.059. [DOI] [PubMed] [Google Scholar]
- 87•.Machado RM, Koike MK. Circadian rhythm, sleep pattern, and metabolic consequences: an overview on cardiovascular risk factors. Horm Mol Biol Clin Investig. 2014;18(1):47–52. doi: 10.1515/hmbci-2013-0057. [DOI] [PubMed] [Google Scholar]
- 88.Puttonen S, Härmä M, Hublin C. Shift work and cardiovascular disease-pathways from circadian stress to morbidity. Scand J Work Environ Health. 2010;36(2):96–108. doi: 10.5271/sjweh.2894. [DOI] [PubMed] [Google Scholar]
- 89.Burgueno A, Genna C, Gianotti TF, Sookoian S, Pirola CJ. Increased levels of resistin in rotating shift workers: a potential mediator of cardiovascular risk associated with circadian misalignment. Atherosclerosis. 2010;210:625–9. doi: 10.1016/j.atherosclerosis.2009.12.032. [DOI] [PubMed] [Google Scholar]
- 90•.Honn KA, Garde AH, Fischer FM, Van Dongen HPA. 22nd International Symposium on Shiftwork and Working Time: Challenges and solutions for healthy work hours. Chronobiol Int. 2016;33(6):581–8. doi: 10.1080/07420528.2016.1195632. [DOI] [PubMed] [Google Scholar]
- 91.Manrique-Garcia E, Sidorchuk A, Hallqvist J, Moradi T. Socioeconomic position and incidence of acute myocardial infarction: a meta-analysis. BMJ. 2017;65(4):301–9. doi: 10.1136/jech.2009.104075. [DOI] [PubMed] [Google Scholar]
- 92.Herman JP, Cullinan WE. Neurocircuitry of stress: central control of the hypothalamo-pituitary-adrenocortical axis. Trends Neurosci. 1997;20(2):78–84. doi: 10.1016/S0166-2236(96)10069-2. [DOI] [PubMed] [Google Scholar]
- 93.Spencer RL, Deak T. A users guide to HPA axis research. Physiol Behav. 2016 doi: 10.1016/j.physbeh.2016.11.014. pii: S0031-9384(16)30720-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Harris A, Waage S, Ursin H, Hansen HM, Bjorvatn B, Eriksen HR. Cortisol, reaction time test and health among offshore shift workers. Psychoneuroendocrinology. 2010;35:1339–47. doi: 10.1016/j.psyneuen.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 95.Touitou Y, Motohashi Y, Reinberg A, Touitou C, Bourdeleau P, Bogdan A, et al. Effect of shift work on the night-time secretory patterns of melatonin, prolactin, cortisol and testosterone. Eur J Appl Physiol. 1990;60:288–92. doi: 10.1007/BF00379398. [DOI] [PubMed] [Google Scholar]
- 96•.Kalmbach DA, Pillai V, Cheng P, Arnedt JT, Drake CL. Shift work disorder, depression, and anxiety in the transition to rotating shifts: the role of sleep reactivity. Sleep Med. 2015;16(12):1532–8. doi: 10.1016/j.sleep.2015.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97•.Van Someren EJ, Cirelli C, Dijk DJ, Van Cauter E, Schwartz S, Chee MWL. J Neurosci. 2015;35(41):13889–95. doi: 10.1523/JNEUROSCI.2592-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98••.Floam S, Simpson N, Nemeth E, Scott-Sutherland J, Gautam S, Haack M. Sleep characteristics as predictor variables of stress systems markers in insomnia disorder. J Sleep Res. 2015;24(3):296–304. doi: 10.1111/jsr.12259. [DOI] [PubMed] [Google Scholar]
- 99.Violanti KM, Aron F. Police stressors: variations in perception among police personnel. J Crim Justice. 1995;23(3):287–94. doi: 10.1016/0047-2352(95)00012-F. [DOI] [Google Scholar]
- 100.Bakker AB, Heuven E. Emotional dissonance, burnout, and in-role performance among nurses and police officers. Int J Stress Manage. 2006;13(4):423–40. doi: 10.1037/1072-5245.13.4.423. [DOI] [Google Scholar]
- 101.Monk TH. What can the chronobiologist do to help the shift worker? J Biol Rhythms. 2000;15(2):86–94. doi: 10.1177/074873040001500202. [DOI] [PubMed] [Google Scholar]
- 102.Poole CJM, Evans GR, Spurgeon A, Bridges KW. Effects of a change in shift work on health. Occup Med. 1992:42193–9. doi: 10.1093/occmed/42.4.193. [DOI] [PubMed] [Google Scholar]
- 103•.Muurlink O, Peetz D, Murray G. Work-related influences on marital satisfaction amongst shiftworkers and their partners: a large, matched-pairs study. Community Work Fam. 2014;17(3):288–307. doi: 10.1080/13668803.2014.933775. [DOI] [Google Scholar]
- 104.Violanti JM, Charles LE, Hartley TA, Mnatsakanova A, Andrew ME, Fekedulegn D, et al. Shift-work and suicide ideation among police officers. Am J of Industrial Med. 2008;51:758–68. doi: 10.1002/ajim.20629. [DOI] [PubMed] [Google Scholar]
- 105.Knutsson A, Åkerstedt T. The healthy-worker effect: Self-selection among Swedish shift workers. Work Stress. 1992;6:163–7. [Google Scholar]
- 106.Puttonen S, Viitasalo K, Härmä M. The relationship between current and former shift work and the metabolic syndrome. Scand J Work Environ Health. 2012;38(4):343–8. doi: 10.5271/sjweh.3267. [DOI] [PubMed] [Google Scholar]
- 107•.Phiri LP, Draper CE, Lambert EV, Kolbe-Alexander TL. Nurses’ lifestyle behaviours, health priorities and barriers to living a healthy lifestyle: a qualitative descriptive study. BMC Nursing. 2014;13(38):1–11. doi: 10.1186/s12912-014-0038-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kolasa KM, Firnhaber GC. 13 tips for surviving the 12-hour shift. Nursing. 2011;41(12):55–60. doi: 10.1097/01.NURSE.0000407679.19754.52. [DOI] [PubMed] [Google Scholar]
- 109.Kuehl KS, Elliot DL, Goldberg L, MacKinnon DP, Vila BJ, Smith J, et al. The safety and health improvement: enhancing law enforcement departments study: feasibility and findings. Frontiers Pub Health. 2014;2(36):1–7. doi: 10.3389/fpubh.2014.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]