Abstract
We examined the effects of sleep quality on next day driving outcomes in a 3.5-month naturalistic driving study of 67 OSA and 47 matched control drivers. Sleep quality measures included total sleep time and sleep fragmentation from actigraphy. The driving outcomes included average speed, lateral control, longitudinal control, distraction, attention to driving- and non-driving related tasks. Sleep quality affected next day’s driving performance differently for OSA and control drivers. Better sleep quality was associated with better lateral and longitudinal control during highway driving for control drivers. The reverse was true for OSA drivers. Similar effects were also seen in terms of distractions and attention to the driving task. These effects suggest improved sleep leads to greater risky driving and ‘activation’ among OSA drivers. Collectively, the findings suggest investment in long-term monitoring of sleep quality in commercial vehicle drivers both with and without sleep disorders may help manage safety risks.
Keywords: Obstructive Sleep Apnea, Sleep Quality, Naturalistic Driving
1 Introduction
Meta-analytic studies indicate that Obstructive Sleep Apnea (OSA) is associated with increased crash risk [1]. Positive Airway Pressure (PAP), the standard treatment for OSA, appears to mitigate crash risk [2]. Processes that are associated with increased crash risk pre-PAP and decreased risk post-PAP are poorly understood [3–5]. One hypothesis is that sleep quality predicts driver attention and sleepiness which in turn affects driving safety measures such as improved vehicle control. Sleep quality as might be measured with indices of fragmentation, such as wake-minutes-after-sleep-onset (WASO), and adequacy of sleep as measured by total sleep time (TST) are critical for functioning irrespective of sleep disorders [6–13]. Importantly, several sleep surveys indicate that chronic partial sleep restriction, sleeping less than the minimum recommended 7 hours of sleep per night, is the norm in the general population [12]. Furthermore, experimental studies show that restricting sleep to even 6.5 hours for 14 consecutive days in non-sleep disordered healthy populations can produce performance decrements comparable to total sleep deprivation or 24 hours without sleep [7]. Importantly, experimental work indicates that there is large individual difference variation in ability to tolerate disruption to sleep and the sources of these differences are poorly understood [14,15].
The goal of this study was to examine the day-to-day associations of sleep quality as measured by actigraphy with next day’s driving outcomes in a 3.5 month naturalistic driving study in patients with OSA and matched control drivers. Recent work based on this sample showed that OSA patients continued to experience greater sleep fragmentation as measured by WASO, lower sleep efficiency despite adequate PAP treatment compared to controls. Furthermore, both OSA and matched control drivers without sleep disorders showed evidence of chronic partial sleep restriction [16]. In other work also based on this sample, we demonstrated that OSA drivers were less alert than controls both pre and post-PAP, and when vehicle speed was less than 45mph, likely corresponding to city/residential driving environments, they showed less variability in speed and lateral control than controls suggesting lackluster reactivity and less risky driving profiles [5]. While these findings with regard to driving outcomes are consistent with the insidious onset of OSA, possibly associated with adjustment in risk tolerances over time, they also suggest that the effectiveness of PAP on improving sleep quality as well as driving outcomes may be limited when performance is observed in the context of chronic partial sleep restriction.
Because adaptation to both disease and chronic partial sleep restriction is already well-documented but poorly understood [7,14, 15], it may be important to go beyond the description of general patterns within sleep, within driving or even the associations between sleep quality and driving performance. To that end, we adopted a complete individual differences perspective and quantified the within-person or within-driver bivariate associations between sleep quality metrics from a given night and driving outcomes observed the next day. This analytic framework makes minimal assumptions about what is adequate sleep for any given driver, what is safe with respect to driving outcomes. Rather, the analytic framework simply quantifies the magnitude of prediction from sleep quality to driving outcomes for each driver separately. The within-person associations essentially describe the extent to which changes around the habitual levels of sleep within a given driver vary with changes around the habitual levels of driving outcome measures for that same driver. We then asked whether the magnitude of these within-person or within-driver associations could be predicted by driver characteristics including disease status, cognitive functioning, and impulsivity.
2 Methods
2.1 Sample
Eighty-five OSA and 50 control drivers were recruited into a naturalistic driving study lasting 3.5 months. Control drivers were matched with OSA drivers at the group level on age within 5 years, education within 2 years, and distribution of gender, and county of residence for rural vs. urban driving. Patients met ICSD-2 clinical criteria for OSA [17] and had a Respiratory Distress Index (RDI) > 15, while controls had no sleep complaints and an RDI < 5 as confirmed by overnight polysomnography. Subject drop-out: Twenty-one of these participants were excluded from the current report for a variety of reasons including: a) participant’s car was incompatible with the instrumented vehicle data acquisition system (IV-DAS, aka ‘black-box’), or had technical issues that caused large drop out in either drive or video data (e.g. < 20 days of useable driving data); b) participants dropped out of study too early because of other commitments. The final sample in this report had 67 OSA (27 female; mean-age = 44.26; mean-education = 16.21 years) and 47 control (18 female; mean-age = 45.74 mean-education = 15.45 years) drivers. There were no systematic differences between those included or excluded in terms of disease severity, age, educational level (min p = .364). Group/disease status did not increase the likelihood of exclusion from this report (p = .744 Fisher’s exact).
2.2 Study Procedures
The protocol called for observing OSA drivers with the IV-DAS for 2-weeks before beginning PAP-therapy and for 3-months after. Control drivers were evaluated on the same schedule to assure comparable data acquisition. Participants were given wrist actigraphy (Actiwatch Spectrum Plus, Philips Respironics, Murrysville, PA) throughout 3.5 month study period.
Procedures Pertinent to Driving Data Collection
IV-DAS contained four devices: an internal camera cluster, a GPS, OBD-II, and accelerometers. Two cameras were located beneath the rear view mirror. One pointed forward toward the road (i.e. driver’s eye view). The other aimed at the driver face and upper body and car interior. Electronic drive files and associated video clips were transmitted to a remote server daily. Video data collection was triggered based on accelerometer exceedances (at least .35g’s) and a baseline data collection schedule [18]. Only data generated during trigger clips were used in this report. OBD speed, lateral, and longitudinal g’s sampled at 1Hz in each ignition on to off cycle were used in this report.
2.3 Measures
Driving measures
In order to contextualize the electronic sensor data into likely-highway versus non-highway driving, each drive file was first segmented into consecutive sections where the OBD speed was below 45mph or 45 mph and above. In each of these sections within a drive, mean OBD speed (in mph), standard deviation in lateral and longitudinal acceleration (in g units) were computed prior to producing averages across trips within a day as the primary vehicle-based performance measures. Clips were evaluated in 20-second segments in three broad domains: safety, exposure, and driver state [18] based on prior work [19–21]. Table 1 provides examples of coded dimensions used in this report. Coders were trained on sample clips illustrating the range of behaviors in each of the dimensions listed in Table 1 until they achieved the minimum inter-rater reliability of Kappa=.61. All coders were blind to actigraphy data. Percentage of 20-second segments in which the driver made driving related gaze movements and rate of distractions (total number of distractions per 20-second segment) in trigger clips were computed for each driving day.
Table 1.
Coded dimensions in 20-second segments from each video clip in two domains of interest
| Driver State | Examples |
|---|---|
| Attention to the Driving Task | Driving related gaze (e.g., checking mirrors, scanning the road ahead) |
| Non-driving related attention | Gaze movements to side of the of the road, inside the vehicle |
| Distraction | Hygiene, cell phone, cognitive, in-vehicle, passenger, eating/drinking, smoking |
Cognitive Function and Impulsivity
Extensive battery of cognitive function assessments tapping processing speed (Grooved pegboard, Useful Field of View, Trail-Making-Part-A), memory (Controlled Oral Word Association, Complex Figure-Recall, Auditory Verbal Learning-30 minute Recall, Benton Visual Retention Test), visuospatial construction (Complex Figure-Copy, Line Orientation, Block Design), and executive function (Stroop Interference, Wisconsin Card Sort, Trail-Making-Part-B) were administrated prior to PAP and at the end of the study. Administration and scoring details for cognitive function assessments are described elsewhere [22–23]. Following prior work, the raw scores from each test were standardized and averaged to form a composite scores quantifying participants relative standing in all of these four domains [24]. Participants also completed Zuckerman’s Impulsivity scale, and Dula Dangerous Driving Index [25,26]. The subscale scores were standardized and averaged to form a composite of Impulsive-Risky driving.
Sleep Quality
Actigraphy data were analyzed using the manufacturer's proprietary software set at low threshold [16]. In this report, we used Total Sleep Time (TST) and Wake Minutes After Sleep Onset (WASO) an index of sleep fragmentation (high values indicate restless sleep quality).
Data Reduction and Analysis
Each night’s actigraphy data were linked with the following day’s driving data from both video (e.g. relative frequency of driving related gaze movements) and electronic vehicle sensors (e.g. mean lateral control when speed <45mph). These daily measures were then used to compute Pearson correlations between the sleep metric and driving metric separately for each driver. The driver specific Pearson correlations were then r-to-z transformed and used as outcome measures in multiple regressions with disease status, cognitive function, and impulsivity as predictors.
3 Results
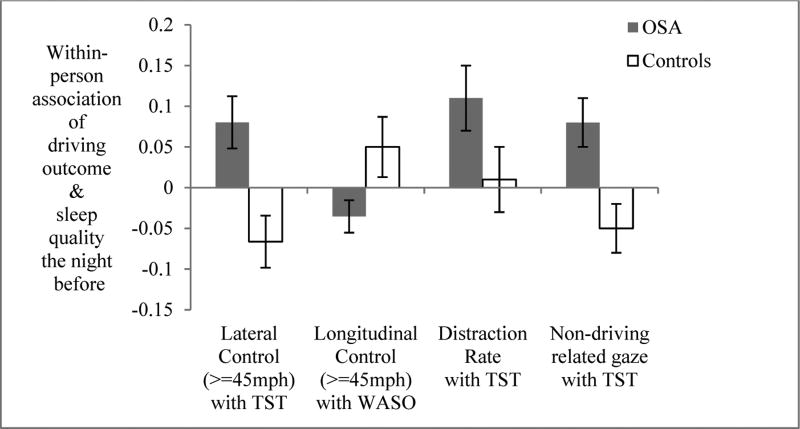
The within-person (or driver) correlations showing the effect of two sleep quality metrics, TST and WASO, on next day’s driving outcome measures (both video and vehicle measures) are listed in the left-most column of Table 2. These within-person correlations served as the outcome measure in multiple regressions and each driver’s disease status, impulsivity, and cognitive function served as predictors. The table provides the standardized regression coefficients obtained from these models. The possibility of interactions among the predictors was also evaluated but these were non-significant in every case, hence are not shown in Table 2. Fig 1 and Fig 2 depict the direction of effects from key findings in Table 2. For example, Fig 1 shows the differences in the magnitude of the within-person associations between sleep quality metrics and next day’s driving outcome separately for OSA and control drivers. The first contrast indicates that lateral control in high speed segments had positive associations with TST the night before for OSA drivers but this association was negative for control drivers. This effect indicates that greater TST predicts smaller standard deviations in lateral g’s in high speed segments for control drivers consistent with more sleep being associated with improved lateral control. However, the reverse was true for OSA drivers. Similarly, following nights of greater WASO or sleep fragmentation, control drivers’ showed larger variability in longitudinal g’s in high speed segments consistent with poorer performance. However, the reverse was true for OSA drivers. Similar patterns were also observed for driver state measures. Longer sleep time was associated with greater distraction rates and greater non-driving related attentional focus the next day for OSA drivers than control drivers. The direction of effects suggests that better sleep quality was associated with an increase in alertness and activity for OSA drivers.
Table 2.
Standardized regression coefficients for predicting the effects of sleep quality on driving outcomes given person-factors: disease status, impulsivity, and cognitive function
| Outcomes: | Predictors: | Disease status | Impulsivity | Cognitive Function |
|---|---|---|---|---|
| Within-person effect of TST on: | ||||
| Lateral control (<45mph) | .07 | .07 | −.04 | |
| Longitudinal control (<45mph) | .05 | −.01 | −.04 | |
| Average Speed (<45mph) | .16 | .13 | .06 | |
| Lateral control (>=45mph) | .22+ | .02 | −.05 | |
| Longitudinal control (>=45mph) | .00 | −.09 | .01 | |
| Average Speed (>=45mph) | .01 | −.15 | −.07 | |
| Distraction Rate | .28* | −.08 | .07 | |
| Attention to the driving task | .19+ | −.02 | .23* | |
| Non-driving related attention | .32* | .08 | .14 | |
| Within-person effect of WASO on: | ||||
| Lateral control (<45mph) | −.05 | −.16 | .07 | |
| Longitudinal control (<45mph) | .02 | −.22* | −.02 | |
| Average Speed (<45mph) | .02 | −.13 | .26* | |
| Lateral control (>=45mph) | −.18+ | −.13 | .14 | |
| Longitudinal control (>=45mph) | −.25* | −.13 | −.10 | |
| Average Speed (>=45mph) | −.08 | −.02 | −.14 | |
| Distraction Rate | −.20+ | .19+ | −.01 | |
| Attention to the driving task | −.01 | −.05 | −.09 | |
| Non-driving related attention | −.06 | .01 | .05 | |
p < .10,
p <.05 or better.
Abbrv. TST = Total Sleep Time, WASO = Wake Minutes After Sleep Onset
Fig 1.
Within-person associations of driving outcomes with sleep quality the night before on vehicle control and driver state variables for OSA and control drivers.
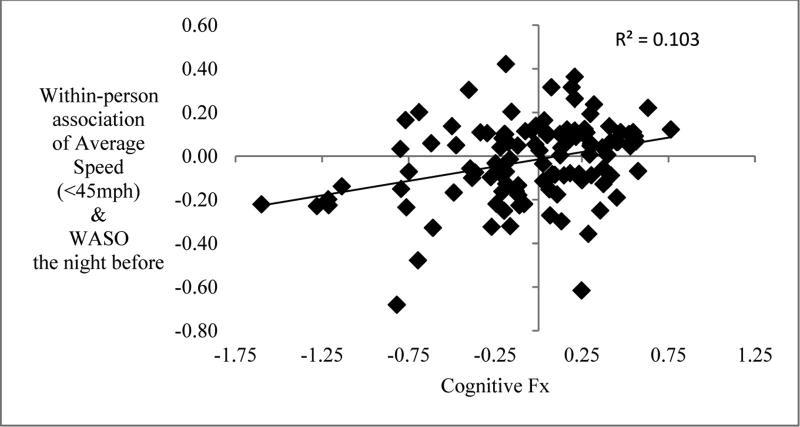
Fig 2.
Higher WASO was associated with lower average speed in low speed drive segments among drivers with low cognitive function. In contrast higher WASO was associated with higher average speed among drivers with high cognitive function.
Some of the models in Table 2 indicated cognitive functioning emerged as a predictor of these associations instead of disease. For example, Fig 2 shows the effects of sleep fragmentation on average speed in low speed segments varied as a function of driver’s cognitive functioning but not disease status. Drivers with higher cognitive function tended to show more positive correlations between fragmentation and average speed. In contrast to drivers with lower cognitive functioning tended to show negative correlations between fragmentation and average speed. Similar patterns were evident in the association between TST and attention to the driving task the next day. Longer sleep was associated with better attention to the driving task and this was particularly true for drivers with higher cognitive function. Impulsivity also predicted the effects of fragmentation on longitudinal control in low speed segments and distraction rate. For example, greater fragmentation was associated with a greater tendency to be distracted during trigger events but this was particularly true for more impulsive than less impulsive drivers.
4 Discussion
The findings showed that sleep quality affected next day’s driving performance differently for OSA and control drivers. While longer and more restful sleep was associated with improved performance for control drivers such as lower variability in lateral and longitudinal g’s in high speed segments, the reverse was true for OSA drivers. Similar patterns were also observed for driver state measures. Longer sleep time was associated with greater distraction rates and greater attention to non-driving related tasks the next day for OSA drivers than control drivers. These effects suggest improved sleep leads to greater risky driving and ‘activation’ among OSA drivers for whom good quality sleep is a rare, welcome experience despite adequate treatment with PAP [24].
When the effects of sleep on driving performance was similar for OSA and control drivers, cognitive function emerged as a predictor of the association between sleep quality and next day’s driving outcome measures. For example, longer sleep was associated with better attention to the driving task particularly for drivers with higher cognitive function. Similarly, greater fragmentation was associated with lower average speed in low speed segments (city/residential driving) especially for drivers who scored low in cognitive functioning. Those effects suggest that cognitive function can mitigate the adverse effects of sleep quality on driving performance.
The findings together with earlier work from this same naturalistic study have implications for commercial vehicle industry in terms of managing safety risks. The effectiveness of PAP on improving sleep quality as well as driving outcomes may be limited especially when driving performance is observed in the context of chronic partial sleep restriction. The findings thus encourage long-term tracking of sleep quality, specifically fragmentation and total sleep time, in all drivers in addition to compliance with PAP among those with sleep disorders. The findings also suggest driver’s cognitive function and impulsivity may be relevant to gauging how changes in sleep are likely to influence their driving performance.
Acknowledgments
The data collection was supported by RO1 HL091917, Real-World Driving Safety in OSA. We thank Sayeh Sabbegh, Michelle Nutting, Lacy Flanagan, Tara Ohrt, Courtney Waite, Nicholas Heisermann, Kelsey Thompson, Katherine Read, Mark Schall, Bryan Fiscus for their diligence and endurance in coding video clips for the study. The analyses presented in this paper were supported by Toyota Collaborative Safety Research Center.
References
- 1.Tregear S, Reston J, Schoelles K, Phillips B. Obstructive Sleep Apnea and Risk of Motor Vehicle Crash: Systematic Review and Meta-Analysis. J. Clin. Sleep Med. 2009;5:573–581. [PMC free article] [PubMed] [Google Scholar]
- 2.Tregear S, Reston J, Schoelles K, Phillips B. Continuous Positive Airway Pressure Reduces Risk of Motor Vehicle Crash Among Drivers with Obstructive Sleep Apnea: Systematic Review and Meta-Analysis. Sleep. 2010;33:1373–1380. doi: 10.1093/sleep/33.10.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Connor J, Nortin R, Ameratunga S, et al. Driver Sleepiness and Risk of Serious Injury to Car Occupants: Population Based Case Control Stud. Br. Med. J. 2002;324:1125–1129. doi: 10.1136/bmj.324.7346.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aksan N, Dawson J, Tippin J, Lee JD, Rizzo M. Effects of Fatigue on Real-World Driving in Diseased and Control Participants; Proceedings of Ninth International Driving Symposium on Human Factors in Driver Assessment, Training, and Vehicle Design; 2015. pp. 274–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aksan N, Marini R, Dawson J, Tippin J, Rizzo M. Driving Performance and Driver State in Obstructive Sleep Apnea: What changes with Positive Airway Pressure; Proceedings of Tenth International Driving Symposium on Human Factors in Driver Assessment, Training, and Vehicle Design; (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Banks S, Dinges DF. Behavioral and Physiological Consequences of Sleep Restriction. J. Clin. Sleep Med. 2007;3:519–528. [PMC free article] [PubMed] [Google Scholar]
- 7.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The Cumulative Cost of Additional Wakefulness: Dose-Response Effects on Neurobehavioral Functions and Sleep Physiology from Chronic Sleep Restriction and Total Sleep Deprivation. SLEEP. 2003;26:117–129. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 8.Belenky G, Wesensten NJ, Thorne DR, Thomas ML, Sing HC, Redmond DP, Balkin TJ. Patterns of Performance Degradation and Restoration during Sleep Restriction and Subsequent Recovery: A Sleep Dose-Response Study. J. Sleep Res. 2003;12:1–12. doi: 10.1046/j.1365-2869.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- 9.Goel N, Rao H, Durmer JS, Dinges DF. Neurocognitive Consequences of Sleep Deprivation. Semin. Neurol. 2009;29:320. doi: 10.1055/s-0029-1237117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krueger PM, Friedman EM. Sleep Duration in the United States: A Cross-Sectional Population-Based Study. Am. J. Epidemiol. 2009;169:1052–1063. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akerstedt T, Nilsson PM. Sleep as Restitution: An Introduction. J. Intern. Med. 2003;254:6–12. doi: 10.1046/j.1365-2796.2003.01195.x. [DOI] [PubMed] [Google Scholar]
- 12.National Sleep Foundation. https://sleepfoundation.org/sleep-polls-data/sleep-in-america-poll/2005-adult-sleep-habits-and-styles.
- 13.Short MA, Banks S. The Functional impact of Sleep Deprivation, Sleep Restriction, and Sleep fragmentation. In: Bianchi MT, editor. Sleep Deprivation and Disease: Effects on the Body, Brain and Behavior. Springer; New York: 2014. pp. 13–26. [Google Scholar]
- 14.Van Dongen HPA, Baynard MD, Maislin G, Dinges DF. Systematic Inter-individual Differences in Neurobehavioral Impairment from Sleep Loss: Evidence of Trait-Like Differential Vulnerability. SLEEP. 2004;27:423–433. [PubMed] [Google Scholar]
- 15.Van Dongen H, Maislin G, Dinges DF. Dealing with Inter-Individual Differences in the Temporal Dynamics of Fatigue and Performance: Importance and Techniques. Aviat. Space Environ. Med. 2004;75:A147–A154. [PubMed] [Google Scholar]
- 16.Tippin J, Aksan N, Dawson J, Anderson S, Rizzo M. Sleep Remains Disturbed in Obstructive Sleep Apnea Patients Treated with Positive Airway Pressure: A Three-Month Cohort Study Using Continuous Actigraphy. Sleep Med. 2016;24:24–31. doi: 10.1016/j.sleep.2016.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kushida CA, Littner MR, Hirshkowitz M, et al. Practice Parameters for the Use of Continuous and Bi-Level Positive Airway Pressure Devices to Treat Adult Patients with Sleep-Related Breathing Disorders. Sleep. 2006;29:375–80. doi: 10.1093/sleep/29.3.375. [DOI] [PubMed] [Google Scholar]
- 18.Aksan N, Schall M, Anderson SW, Dawson JD, Tippin JT, Rizzo M. Can Intermittent Video Sampling Capture Individual Differences in Naturalistic Driving; Proceedings of Seventh International Driving Symposium on Human Factors in Driver Assessment, Training, and Vehicle Design; 2013. pp. 135–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Klauer SG, Dingus TA, Neale VL, Sudweeks J, Ramsey DJ. The Impact of Driver Inattention on Near-Crash/Crash Risk: An Analysis Using the 100-Car Naturalistic Driving Study Data. National Highway Traffic Safety Administration; Washington DC: 2006. [Google Scholar]
- 20.Neale VL, Dingus TA, Klauer SG, Sudweeks J, Goodman M. An Overview of the 100-Car Naturalistic Study and Findings; 19th International Technical Conference on the Enhanced Safety of Vehicles; Washington, D.C. 2005. [Google Scholar]
- 21.Wierwille WW, Ellsworth LA. Evaluation of Driver Drowsiness by Trained Raters. Accid. Anal. Prev. 1994;26:571–581. doi: 10.1016/0001-4575(94)90019-1. [DOI] [PubMed] [Google Scholar]
- 22.Lezak MD, Howieson DB, Loring DW. Neuropsychological Assessment. 4. Oxford University Press; New York: 2004. [Google Scholar]
- 23.Anderson S, Aksan N, Dawson J, Uc E, Johnson AM, Rizzo M. Neuropsychological Assessment of Driving Safety Risk in Older Adults With and Without Neurologic Disease. J. Clin. Exp. Neuropsychol. 2012;34:895–905. doi: 10.1080/13803395.2011.630654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dawson J, Uc E, Anderson SW, Johnson AM, Rizzo M. Neuropsychological Predictors of Driving Errors in Older Adults. J. Am. Geriatr. Soc. 2010;58:1090–1096. doi: 10.1111/j.1532-5415.2010.02872.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dula C, Ballard ME. Development and evaluation of a measure of dangerous, aggressive, negative emotional, and risky driving. J Appl. Soc. Psych. 2003;33:263–282. [Google Scholar]
- 26.Zuckerman M. The Psychobiological Model for Impulsive Unsocialized Sensation Seeking: A Comparative Approach. Neuropsychobiology. 1996;34:125–129. doi: 10.1159/000119303. [DOI] [PubMed] [Google Scholar]