Abstract
Background
Allied health services are an important part of providing effective team-based care. The Champlain BASE™ (Building Access to Specialists through eConsultation) eConsult service facilitates quick and secure communication between primary care providers (PCPs) and allied health professionals (AHPs).
Aim
To assess the eConsult service’s ability to improve access to advice from AHPs.
Design and setting
A cross-sectional study was carried out on all cases submitted to AHPs through the eConsult service between April 2011 and May 2016. The service covers Ottawa, Canada, and its surrounding rural communities.
Method
A descriptive overview of all cases submitted to allied health services was conducted. Utilisation and survey metrics for AHP eConsults were compared with those sent to medical specialties, in order to understand the potential differences and generalisability of eConsult access beyond the traditional medical specialty referral.
Results
PCPs submitted 127 cases to nine allied health specialties during the study period. The most popular specialty was clinical pharmacist, which received an average of 1.5 cases per month. The median specialist response time was 2.1 days (interquartile range [IQR] 0.7–5.3 days, range 0.01–14.2 days) versus 0.9 days (IQR 0.2–3.4 days, range 0–49.5 days) for medical specialties. PCPs received advice for a new or additional course of action in 70% (versus 58% for medical specialties) of cases. They rated the service as being of high or very high value for their patients in 88% of cases (versus 93% for medical specialties), and for themselves in 89% (94% for medical specialties) of cases.
Conclusion
The eConsult service has demonstrated the ability to support prompt communication between PCPs and AHPs, improving patients’ access to AHP care. Given the importance of AHPs in providing primary care, allied health services should be offered in the menu of specialties available through electronic consultation services.
Keywords: allied health personnel, chronic disease, eConsult, primary care, referral
INTRODUCTION
Team-based care, in which primary care providers (PCPs) treat patients alongside allied health professionals (AHPs) such as chiropodists, social workers, and dieticians, is becoming increasingly important as ageing populations in many developed countries have resulted in PCPs caring for more patients with complex chronic conditions. Chronic diseases are a major cause of morbidity and mortality,1 affecting hundreds of millions of patients in Canada, the US, and the UK.1–3 Managing chronic diseases can be challenging in a primary care environment as these conditions often require lengthy and frequent treatment, which many PCPs struggle to deliver within the constraints of typical office visits.4 In response to this issue, some jurisdictions have highlighted the importance of providing more team-based care.5 An example of this approach is the introduction of new primary care models (for example, community health centres, family health teams) in which allied health services are incorporated directly into the practice, facilitating patients’ ability to receive well-coordinated multi-practitioner care.6
However, many patients continue to receive primary care outside of a team-based environment, which can make allied health services difficult to access.7 Although PCPs can arrange appointments with AHPs for their patients, there is often little to no communication between the two professional groups, which can negatively affect care coordination and result in delays, redundancies (for example, duplication of tests or procedures), and an overall lower quality of patient care. Researchers from several countries have cited a number of access barriers in allied health services, including excessive case volumes and siloed care, resulting in poor inter-provider communication.8–10
In Australia, researchers conducted focus groups with PCPs to assess barriers they experienced when managing patients with diabetes or chronic kidney disease; cited as significant barriers were difficulties navigating the allied health referral system and poor coordination between providers.9 A study set in Alberta, Canada, had similar findings, with PCPs citing a lack of knowledge about allied health services as a key barrier in offering care to patients with stage-five chronic kidney disease.11 Furthermore, many allied health services are not covered by provincial arrangements for Medicare (the Canadian national healthcare system) and must be paid for by patients, unless provided in a hospital or covered by private health insurance.12 Consequently, many healthcare systems are taking steps to address access issues for allied health services in order to provide patients with the services that are essential to their care.13–15
How this fits in
Allied health professionals are vital to the effective treatment of chronic illness, but many patients face barriers to accessing their services. Evaluations of electronic consultation services have demonstrated their ability to improve access to specialist care. This study provides a novel look at the utilisation, outcomes, and benefits of cases submitted electronically to allied health services, offering insight into when primary care providers refer to such services and how access may be improved.
In 2010, the research team launched the Champlain BASE™ (Building Access to Specialists through eConsultation) eConsult service, an online platform that facilitates quick and secure communication between PCPs and specialists.16 During the initial proof of concept, it was requested that diabetes education be added to the list of available specialty services. Other specialty groups followed, including several other allied health services (such as chiropodists, dieticians, and social workers); as a result, the eConsult service allows PCPs to seek advice directly from AHPs at no cost to the patient.
Previous studies have established the eConsult service’s ability to improve access to specialist advice, reduce wait times, deliver high levels of provider satisfaction, and lower costs.17–19 Studies of specific sub-populations (for example, older patients, patients suffering from chronic pain) have revealed similar findings.20,21 However, given the unique challenges associated with referral to allied health specialties, a detailed examination of eConsult’s impact on this subgroup was warranted. In this article, the eConsult service’s ability to improve access to allied health services was examined by assessing the utilisation, outcomes, and benefits associated with cases requiring such advice.
METHOD
Study design
A cross-sectional study was conducted of all cases submitted to AHPs through the Champlain BASE eConsult service between April 2011 and May 2016.
Setting
The eConsult service is established in the Champlain Local Health Integration Network (LHIN), a health region in eastern Ontario with a population of 1.2 million.22 It covers the city of Ottawa and the surrounding rural communities. Medical services in the province are publicly funded by the Ontario Health Insurance Plan; however, allied health services are generally not publicly funded and most patients pay for these services themselves.
The Champlain BASE eConsult service
To use the eConsult service, PCPs log on to the platform, then complete a form to supply patient information and their clinical question; they have the option of attaching test results, images, or other relevant documents. The electronic consultation is then assigned to a specialist who has 7 days to respond. The specialist can request additional information, reply to the consultation, or suggest a face-to-face referral. Even if recommending a face-to-face referral, the specialist can provide advice for treatment in the meantime, or suggest laboratory and imaging tests that will lead to a more effective visit.
Data collection
The eConsult service automatically collects utilisation data for each case, including information about the:
PCP (medical doctor [MD] or nurse practitioner [NP], city);
specialty referred to;
patient (age, sex); and
the case itself (data created, date responded to, date closed, specialist self-reported response time, log of the correspondence between the PCP and specialist).
Additionally, PCPs complete a mandatory survey before closing each case, the results of which are also recorded by the system. The survey questions are presented in Box 1.
Box 1. Mandatory closing survey completed by primary care providers at the end of each electronic consultation.
- Q1. Which of the following best describes the outcome of this eConsultation for your patient?
- I was able to confirm a course of action that I originally had in mind.
- I got new advice for a new or additional course of action.
- I did not find the response very useful.
- None of the above.
- Q2. As a result of the eConsultation would you say that:
- Referral was originally contemplated but now avoided at this stage.
- Referral was originally contemplated and is still needed — this eConsult likely leads to a more effective visit.
- Referral was not originally contemplated and is still not needed — this eConsult provided useful feedback/instruction.
- Referral was not originally contemplated, but the eConsult process resulted in a referral being initiated.
- There was no particular benefit to using eConsult in this case.
- Other (please explain).
- Q3. Please rate the overall value of the eConsult service for your patient:
- Minimal 1 2 3 4 5 Excellent
- Q4. Please rate the overall value of the eConsult service in this case for you as a primary care provider:
- Minimal 1 2 3 4 5 Excellent
Q5. We would value any additional feedback you provide:
Data analysis
All allied health specialties available through the eConsult service were identified. A descriptive overview was conducted of all cases submitted to these services. Comparison was made between the utilisation and survey metrics for eConsults sent to AHPs and those sent to medical specialties, in order to understand the potential differences and generalisability of eConsult access beyond the traditional medical specialty referral. As allied health specialties included in the analysis were added at different times, the specialty distribution was reported as a monthly average for the number of months it had been available via the eConsult service.
RESULTS
A total of 12 allied health specialties were made available through the eConsult service between April 2011 and May 2016; only nine of these received cases (Table 1). Allied health specialties received 127 cases out of a total of 15 237 electronic consultations submitted during the study period. In 74% of cases, patients were adults aged 18–65 years, 22% of cases were seniors (aged >65 years) and 4% were for patients <18 years. In comparison, 62% of cases referred to medical specialties were adults aged 18–65 years, and 16% were for patients <18 years. The remaining 22% were aged >65 years.
Table 1.
eConsult data, April 2011–May 2016
| Specialty | Date service became available via eConsult | Total eConsults, n | Average eConsults per month, n | Average specialist response time, minutes | Average cost per eConsult (C$) |
|---|---|---|---|---|---|
| Addiction assessment/treatment services | 14 Sep 2014 | 17 | 0.81 | 12.65 | n/a |
| Back and neck (spine) care | 13 Apr 2015 | 9 | 0.64 | 15.00 | 50.00 |
| Bariatric care | 15 Feb 2015 | 4 | 0.25 | 25.00 | 20.83 |
| CCAC — Champlain | 20 Nov 2013 | 4 | 0.13 | 15.00 | n/a |
| Chiropody | 19 Feb 2014 | 8 | 0.29 | 11.25 | n/a |
| Clinical pharmacist | 1 Mar 2013 | 59 | 1.51 | 15.85 | 13.21 |
| Diabetes education | 1 Jan 2011 | 15 | 0.23 | 16.67 | 13.89 |
| HIV pharmacist | 14 Jun 2014 | 9 | 0.38 | 13.89 | 11.57 |
| HIV psychologist | 14 Jun 2014 | 0 | 0.00 | n/a | n/a |
| HIV social worker | 14 Jun 2014 | 0 | 0.00 | n/a | n/a |
| Musculoskeletal rehabilitation | 13 Apr 2015 | 2 | 0.14 | 17.50 | 58.33 |
| Parkinson’s patient care coordination | 10 Feb 2016 | 0 | 0.00 | n/a | n/a |
C$ = Canadian dollars. CCAC = Community Care Access Centre. n/a = not applicable.
The most popular specialty was clinical pharmacist, which received an average of 1.5 cases per month when controlling for the number of months available (Table 1). This was followed by addiction assessment/treatment services (0.8 cases per month) and back and neck (spine) care (0.6 cases per month). The total cost of remunerating specialists for the 127 cases submitted to allied health specialties was C$1741.67. Table 1 shows the average allied health specialist cost per consult.
Examples of questions submitted via the eConsult service are given in Table 2. Medical doctors submitted 87% of the electronic consultations, whereas 13% originated from NPs — this proportion was similar to that for electronic consultations sent to medical specialties. Most allied health cases originated from PCPs in urban clinics (75%), whereas 22% originated from rural clinics, and 2% from semi-urban clinics. One originated from Nunavut (rurality was measured using an Ontario-based index, which doesn’t apply outside of the province; as such, Nunavut could not be classified on the same scale). The proportion of rural cases submitted to allied health specialties is higher than the proportion for those submitted to medical specialties, where only 12% originated from rural PCPs.
Table 2.
Questions submitted to allied health specialties
| Specialty | Example questiona |
|---|---|
| Addiction assessment/treatment services | ‘Patient is addicted to benzodiazepines but is motivated to taper off and is seeking support from community resources. Previous efforts at withdrawal have resulted in binging and relapse. Family has offered support. Please provide advice on how to manage reduction of drug intake.’ |
| Clinical pharmacist | ‘What is the risk of adverse effects (for example, serotonin syndrome, seizures) when combining tramadol with an SSRI? Many of my patients with chronic pain are also on SSRIs or tricyclics, and I would prefer to keep them off more potent opiates. Are adverse effects seen quite quickly after initiation, or could a delayed effect take place? Advice on how long and aggressively to monitor would be appreciated.’ |
| Diabetes education | ‘Patient is in his fifties with type 2 diabetes. His A1C levels are better than they have been previously [PCP lists A1C percentage]. He is taking multiple oral medications for diabetes, high blood pressure, and anxiety [lists medications and dosages], but requires further treatment. He refuses to take anything via injection. Are there any other oral options for his diabetes?’ |
| Musculoskeletal rehabilitation | ‘Patient is in late fifties and has been experiencing pain in her tailbone for approximately 1 month due to a fall. Current treatment consists of a donut cushion for sitting and over-the-counter pain medication. An X-ray revealed dislocation [gives details]. Given these findings, would surgical intervention be recommended?’ |
Question specifics have been altered to ensure patient and provider confidentiality. PCP = primary care provider. SSRI = selective serotonin reuptake inhibitor.
The median allied health specialist response time from receipt of request was 2.1 days (interquartile range [IQR] 0.7–5.3 days, range 0.01–14.2 days). This is longer than for medical specialties — for which the median response time was 0.9 days (IQR 0.2–3.4 days, range 0–49.5 days) — but remains well within the service’s required 7-day response time. The self-reported time specialists needed to complete the consultation was:
<10 minutes in 29% of cases;
10–15 minutes in 44% of cases;
15–20 minutes in 18% of cases; and
>20 minutes in 9% of cases.
Responses from AHPs took slightly longer than from physicians, who answered nearly half of consultations in <10 minutes. Table 1 shows the average response time and average cost by specialty.
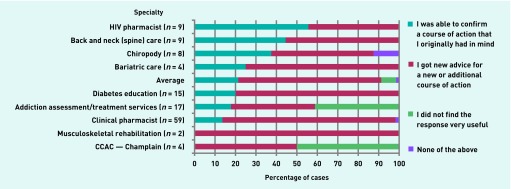
During the closing survey, PCPs indicated that they got advice for a new or additional course of action in 70% of cases, and confirmed a course of action they already had in mind in 21% of cases. In comparison, only 58% of electronic consultation cases sent to medical specialties resulted in a new or additional course of action, while 40% confirmed a course of action that the PCP already had in mind. A breakdown of the eConsult service’s impact on the PCP’s course of action by specialty is presented in Figure 1.
Figure 1.
Impact of the eConsult service on primary care provider’s course of action, by specialty (n = 127).
CCAC = Community Care Access Centre.
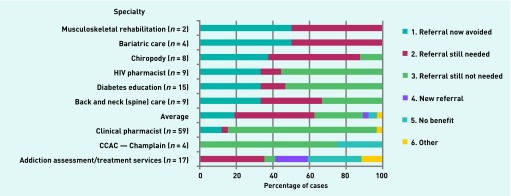
A face-to-face specialist referral was avoided in 73% of cases submitted to allied health specialties, versus 69% of cases submitted to medical specialties. The 73% includes both ‘referral now avoided’ and ‘referral still not needed’, both of which involve cases where a referral was not ultimately made for the patient. Figure 2 shows the impact of the electronic consultation on the need for a face-to-face referral by specialty.
Figure 2.
Impact of the eConsult service on need for face-to-face referral by specialty (n = 127).
CCAC = Community Care Access Centre.
For cases sent to allied health specialists, PCPs rated the eConsult service’s value for their patient as high (rated 4 or 5 on a scale of 1–5, in which 1 is minimal and 5 excellent) in 88% of cases, with an average rating of 4.5 out of 5.0. Using the same scale, PCPs rated the service’s value for themselves as 4 or 5 out of 5 in 89% of cases, with an average rating of 4.5 out of 5.0. This is slightly lower than for consultations sent to medical specialties, which PCPs rated as high (4 or 5 out of 5) for their patients and themselves in 93% and 94% of cases, respectively.
Overall, PCPs responded positively to the eConsult service. As the most frequently referred-to specialty, clinical pharmacy, in particular, received a number of positive comments. PCPs reported that, through the eConsult service, they were able to access pharmacological information they previously would not have had access to, and that it helped them sort through the difficult field of pharmacology.
The only negative feedback pertained to addiction assessment/treatment services, which some PCPs expected to be a medical specialty, overseen by a physician. One PCP said:
‘This [electronic consultation] was not very useful as it was really a medical question and the provider who answered it was not able to give a medical answer. Are there any addiction physicians who might be able to comment?’
(PCP)
Below are a selection of comments that PCPs left in response to cases submitted to allied health specialties.
Chiropody
Prompt reply that was above and beyond call of duty. Excellent recommendations.’
(PCP)
Clinical pharmacy
‘Thanks for your quick and detailed response.’
(PCP)
‘Just a wonderful service — good information each time!’
(PCP)
‘Thank you for this thorough and helpful feedback, which helps me better understand the conversions and other things to consider for this patient.’
(PCP)
‘Always great answers to help sort through the difficult field of pharmacology. Thanks.’
(PCP)
‘This consult provided information I was unable to access otherwise. Thank you VERY much.’
(PCP)
‘Better answer than any retail pharmacist could provide in their hurried and rushed environment.’
(PCP)
Addiction assessment/treatment services
‘Great advice with specific detail re next steps in referral including the telephone number — much appreciated. My patient will be very relieved to hear the recommendations. Thank you.’
(PCP)
DISCUSSION
Summary
The results have shown the potential positive impact of including allied health specialties in an eConsult service’s menu of specialties.
Although cases sent to allied health specialties comprised a small fraction of the eConsult service’s total case volume (roughly 1%), they received high ratings from PCPs regarding their value to patients and providers, and resulted in a new or additional course of action in more than two-thirds of cases.
Clinical pharmacy was especially valued and received the largest share of electronic consultations among allied health specialties.
Strengths and limitations
This study’s principal strength is its novelty. To the authors’ knowledge, this is the first study to assess the eConsult service’s ability to improve access to advice from AHPs. Other strengths include its use of data drawn directly from the service over a long period of time. However, there are also some limitations. The system does not collect patient identifiers, therefore the actual number of referrals that were initiated as a result of the eConsult service is not known; neither is whether specialist advice was implemented by PCPs. The service made certain allied health specialties available through the service in the Champlain LHIN but, as allied health services vary by region, the results may not be generalisable to other jurisdictions.
A quantitative approach was used to explore PCPs’ use of the eConsult service to access allied health services. Although this allowed the researchers to examine referral patterns and assess outcomes and rates of PCP satisfaction, a qualitative approach would allow further insight into why and how PCPs choose to access allied health specialists. A study of this group using qualitative methods would be useful and is being considered as an avenue of future study.
Comparison with existing literature
Numerous health jurisdictions have identified allied health services as an important element of the healthcare system, resulting in new policies or programmes designed to improve equity of access to AHPs.23–25 One example is the Enhanced Primary Care (EPC) initiative implemented in Australia, which subsidises allied health services for patients referred by PCPs.24 Evaluation of the initiative has suggested that it can alleviate common barriers to allied health service access, namely prohibitive costs for patients on a low income and lack of patient awareness of the services’ benefits,26 with a potential positive impact on health outcomes.27 However, several barriers have been reported that impede referral to allied health services, including lack of awareness among PCPs, waiting lists, and out-of-pocket costs when services are not subsidised through public or private insurance.26,28 By providing an alternative means of accessing allied health advice, without requiring a face-to-face referral, the eConsult service may be able to alleviate some of these challenges.
Implications for practice
AHPs play an important part in the delivery of effective chronic disease care — a fact reflected in the Preventing and Managing Chronic Disease Framework, drawn up by the Ontario’s Ministry of Health and Long-Term Care. This document highlights the need for an interdisciplinary mix of specialty care professionals working in collaboration to improve care for those people who are chronically ill.5 The framework emphasises the importance of establishing interdisciplinary care teams with defined roles and responsibilities, care planning and care paths, and outreach and population needs-based care. The service presented here supports these goals by facilitating direct, secure communication between PCPs and AHPs. Through the eConsult service, PCPs can reach out to AHPs for guidance on caring for patients with chronic diseases. In many cases, PCPs receive the information they need so they can treat patients themselves, eliminating the burdens associated with having to attend an additional appointment. These patients also avoid having to pay for care themselves if they do not have private health insurance, as AHPs who provide advice via electronic consultations are compensated by the service directly on a pro-rata basis through current research funding or as part of their salary. Non-physician services should be taken into account as policies pertaining to eConsult services and payment are developed.
The eConsult service is a valuable tool that has successfully been implemented in a health region to allow direct communication between PCPs and AHPs. Given the importance of AHPs in providing primary care, allied health services should be offered in the menu of specialties available through electronic consultation services.
Acknowledgments
The authors wish to thank the primary care providers, specialists, and allied health professionals who participated in the eConsult service; Winchester District Memorial Hospital, which hosts the servers; and Justin Joschko for his assistance in editing and formatting the manuscript.
Funding
Funding for this project was provided by the Ontario Ministry of Health and Long-Term Care, the Ottawa Hospital Academic Medical Organization Innovation Fund, eHealth Ontario, and the Champlain Local Health Integration Network.
Ethical approval
Ethical approval was granted by the Ottawa Health Science Network Research Ethics Board (Protocol #2009848-01H).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384(9937):45–52. doi: 10.1016/S0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- 2.Health Council of Canada . Self-management support for Canadians with chronic health conditions: a focus for primary health care. 2012. http://www.selfmanagementbc.ca/uploads/HCC_SelfManagementReport_FA.pdf (accessed 9 Sep 2017). [Google Scholar]
- 3.Department of Health . Long term conditions compendium of information. 3rd edn. Leeds: DH; 2012. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216528/dh_134486.pdf (accessed 9 Sep 2017). [Google Scholar]
- 4.Bodenheimer T. Coordinating care — a perilous journey through the health care system. New Eng J Med. 2008;358(10):1064–1071. doi: 10.1056/NEJMhpr0706165. [DOI] [PubMed] [Google Scholar]
- 5.Ontario Ministry of Health and Long-Term Care Preventing and managing chronic disease: Ontario’s framework. 2007 http://www.health.gov.on.ca/en/pro/programs/cdpm/pdf/framework_full.pdf (accessed 9 Sep 2017). [Google Scholar]
- 6.Ontario Ministry of Health and Long-Term Care Family health teams. http://www.health.gov.on.ca/en/pro/programs/fht/ (accessed 9 Sep 2017). [Google Scholar]
- 7.Health Council of Canada . Teams in action: primary health care teams for Canadians. Ottawa: HCC; 2009. [Google Scholar]
- 8.Nancarrow SA, Moran AM, Enderby PM, et al. The relationship between workforce flexibility and the costs and outcomes of older peoples’ intermediate care services. Clin Rehabil. 2010;24(10):953. [Google Scholar]
- 9.Lo C, Teede H, Ilic D, et al. Identifying health service barriers in the management of co-morbid diabetes and chronic kidney disease in primary care: a mixed-methods exploration. Fam Pract. 2016;33(5):492–497. doi: 10.1093/fampra/cmw041. [DOI] [PubMed] [Google Scholar]
- 10.Thylefors I, Persson O, Hellström D. Team types, perceived efficiency and team climate in Swedish cross-professional teamwork. J Interprof Care. 2005;19(2):102–114. doi: 10.1080/13561820400024159. [DOI] [PubMed] [Google Scholar]
- 11.Tam-Tham H, Hemmelgarn BR, Campbell DJ, et al. Primary care physicians’ perceived barriers, facilitators and strategies to enhance conservative care for older adults with chronic kidney disease: a qualitative descriptive study. Nephrol Dial Transplant. 2015;31(11):1864–1870. doi: 10.1093/ndt/gfv408. [DOI] [PubMed] [Google Scholar]
- 12.Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH. Improving the quality of health care for chronic conditions. Qual Saf Health Care. 2004;13(4):299–305. doi: 10.1136/qshc.2004.010744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Department of Health Report to the National Allied Health Professional Advisory Board on the outcomes of the Modernising Allied Health Professional Careers Programme. 2011 https://www.gov.uk/government/publications/report-to-the-national-allied-health-professional-advisory-board-on-the-outcomes-of-the-modernising-allied-health-professional-careers-programme (accessed 17 Sep 2017). [Google Scholar]
- 14.Young G, Hulcombe J, Hurwood A, Nancarrow S. The Queensland Health Ministerial Taskforce on health practitioners expanded scope of practice: consultation findings. Aust Health Rev. 2015;39(3):249–254. doi: 10.1071/AH14141. [DOI] [PubMed] [Google Scholar]
- 15.Siu HH-Y, Steward N, Peter J, et al. A novel primary-specialist care collaborative demonstration project to improve the access and health care of medically complex patients. Chronic Illness. 2016;13(3):151–170. doi: 10.1177/1742395316674541. [DOI] [PubMed] [Google Scholar]
- 16.Liddy C, Rowan MS, Afkham A, et al. Building access to specialist care through e-consultation. Open Med. 2013;7(1):e1–e8. [PMC free article] [PubMed] [Google Scholar]
- 17.Keely E, Liddy C, Afkham A. Utilization, benefits, and impact of an e-consultation service across diverse specialties and primary care providers. Telemed J E Health. 2013;19(10):733–738. doi: 10.1089/tmj.2013.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liddy C, Afkham A, Drosinis P, et al. Impact and satisfaction with a new eConsult service: a mixed methods study of primary care providers. J Am Board Fam Med. 2015;28(3):394–403. doi: 10.3122/jabfm.2015.03.140255. [DOI] [PubMed] [Google Scholar]
- 19.Liddy C, Drosinis P, Deri Armstrong C, et al. What are the cost savings associated with providing access to specialist care through the Champlain BASE eConsult service? A costing evaluation. BMJ Open. 2016;6(6):e010920. doi: 10.1136/bmjopen-2015-010920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liddy C, Smyth C, Poulin PA, et al. Improving access to chronic pain services through eConsultation: a cross-sectional study of the Champlain BASE eConsult service. Pain Med. 2016;17(6):1049–1057. doi: 10.1093/pm/pnw038. [DOI] [PubMed] [Google Scholar]
- 21.Liddy C, Drosinis P, Joschko J, Keely E. Improving access to specialist care for an aging population. Gerontol Geriatr Med. 2016;2:1–7. doi: 10.1177/2333721416677195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ontario Local Health Integration Network Champlain LHIN local environmental scan: spring 2016. http://www.champlainlhin.on.ca/~/media/sites/champlain/About_Us/GeoPopHlth/2016ChEnvScanEN.pdf?la=en (accessed 25 Sep 2017). [Google Scholar]
- 23.Beaulieu M, Levin A. Analysis of multidisciplinary care models and interface with primary care in management of chronic kidney disease. Semin Nephrol. 2009;29(5):467–474. doi: 10.1016/j.semnephrol.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 24.Cant RP, Foster MM. Investing in big ideas: utilisation and cost of Medicare allied health services in Australia under the Chronic Disease Management initiative in primary care. Aust Health Rev. 2011;35(4):468–474. doi: 10.1071/AH10938. [DOI] [PubMed] [Google Scholar]
- 25.McCallum CA, DiAngelis T. Direct access: factors that affect physical therapist practice in the state of Ohio. Phys Ther. 2012;92(5):688–706. doi: 10.2522/ptj.20100358. [DOI] [PubMed] [Google Scholar]
- 26.Nicholas LG, Pond CD, Roberts DC. Dietitian–general practitioner interface: a pilot study on what influences the provision of effective nutrition management. Am J Clin Nutr. 2003;77(4 Suppl):1039S–1042S. doi: 10.1093/ajcn/77.4.1039S. [DOI] [PubMed] [Google Scholar]
- 27.Haines TP, Foster MM, Cornwell P, et al. Impact of Enhanced Primary Care on equitable access to and economic efficiency of allied health services: a qualitative investigation. Aust Health Rev. 2010;34(1):30–35. doi: 10.1071/AH09732. [DOI] [PubMed] [Google Scholar]
- 28.Gucciardi E, Chan VW-S, Fortugno M, et al. Primary care physician referral patterns to diabetes education programs in southern Ontario, Canada. Can J Diabetes. 2011;35(3):262–268. [Google Scholar]