Abstract
Background:
Elbow ulnar collateral ligament (UCL) injuries are common, particularly in adolescent athletes playing overhead sports. While the incidence and outcomes of surgical UCL injuries are well documented, the nonsurgical UCL injury patterns and injury management in this population are not yet known.
Purpose/Hypothesis:
The purpose of this study was to retrospectively assess the injury severity and subsequent management of UCL injuries among competitive athletes aged 11 to 22 years. We hypothesized that nonsurgical UCL injuries would occur more frequently in younger athletes compared with older athletes.
Study Design:
Descriptive epidemiological study.
Methods:
Electronic medical records (using International Classification of Diseases, 9th Revision and 10th Revision and Current Procedural Terminology codes) and keyword searches were used to identify all patients with sports-related UCL injuries between January 2000 and April 2016. A total of 136 records were included. Patients were stratified into 3 age brackets (age 11-13 years, n = 17; age 14-16 years, n = 49; age 17-22 years, n = 70). There were no prior elbow surgical interventions. The main outcome measures included the frequency and severity of UCL injuries and injury management (surgical, nonsurgical). Independent variables included age, UCL injuries per year, and sport classification.
Results:
There were 53 surgical and 83 nonsurgical UCL injuries. The number of nonsurgical cases increased 9-fold from 2000-2008 to 2009-2016. The UCL injuries were distributed as follows: 60 sprains, 39 partial tears, 36 ruptures, and 1 rerupture. Moreover, 7% of sprains, 51% of partial tears, and 78% of ruptures underwent UCL reconstruction. Nonsurgical management was most common in the youngest athletes (age 11-13 years, 100.0% of total injuries; age 14-16 years, 71.4% of total injuries; and age 17-22 years, 44.3% of total injuries) (P = .007). UCL injury volume was most commonly associated with javelin (odds ratio, 6.69; 95% CI, 0.72-61.62; P = .07) and baseball (odds ratio, 1.55; 95% CI, 0.69-3.51; P = .32).
Conclusion:
Younger athletes sustained less severe UCL injuries more often than older athletes. Participation in javelin and baseball was associated with a greater likelihood of UCL injuries based on our dataset. This is the first study to provide data on the volume of nonsurgical UCL injuries among athletes in various sports.
Keywords: adolescent, elbow, injury, sports, ulnar collateral ligament
The ulnar collateral ligament (UCL) is the primary stabilizer of the elbow, and it resists valgus stress applied to the elbow joint.32 Injuries to the UCL greatly compromise stability of the elbow. UCL injuries and subsequent ruptures are common among participants in overhead-throwing sports.12,25 Damage to the UCL in the overhead-throwing athlete is a severe and potentially career-threatening injury. This injury can be managed conservatively or with surgical reconstruction (UCL-R).
UCL-R has become increasingly common among players at all levels of experience since the 1990s.1,14,21,43 Evidence shows that the number of UCL-R in youth has increased 6-fold since the mid-1990s and continues to grow.1,17 Unfortunately, this trend is expected to continue through the year 2025, particularly in athletes 15 to 24 years of age.35
With a continuing rise in these injuries, there has also been a growth of misinformation in the media, which can lead to inaccurate information regarding UCL injuries in the general public.8 Johnson et al23 reported that patients are using the Internet for information regarding this injury and that the quality, accuracy, and readability regarding UCL injuries are potentially incorrect. Thus, a study of this type is warranted so that all physicians, including nonoperative physicians who care for athletes with this type of injury, are aware of the most up-to-date information.
At present, considerable information is known about the prevalence, incidence, and outcomes of UCL-R8–11; the epidemiology of UCL-R at advanced levels of competition7; surgical techniques; and new research on UCL repair versus UCL-R.13,15,49 The frequency and severity of UCL injuries and the proportion of those injuries that undergo surgical versus nonsurgical management remain unknown. These findings are important for clinicians who care for athletes with this injury.
The purposes of this study were to determine (1) whether the frequency and severity of UCL injuries differed based on an athlete’s age, sport, and time participating in competitive sports and (2) whether there were different patterns of surgical and conservative management for these injuries based on injury severity. We hypothesized that (1) less severe UCL injuries would occur more frequently in younger athletes in sports with repetitive, high-volume stress (such as baseball) compared with their older cohorts and (2) younger athletes would be managed conservatively for their injury, and older athletes would demonstrate the highest frequency of UCL-R among our patient groups.
Methods
Study Design
This was a retrospective chart review study. Data were reviewed from medical records from January 1, 2000, to April 26, 2016. Approval was obtained from our institutional review board for all study procedures. Once approval was obtained, a formal medical request was made with the above criteria to our institution’s Faculty Practice Health Department for chart retrieval.
Patients
Patients aged 11 to 22 years who sustained a UCL injury to the elbow during a sports competition were included. International Classification of Diseases, 9th Revision (ICD-9) and 10th Revision (ICD-10) and Current Procedural Terminology (CPT) codes were used to find patients. Elbow sprain (ICD-9 841.1, 841.9, 842.00, 848.9 or ICD-10 [UCL sprain of the elbow] S53.449A, S53.441A, S53.442A), elbow UCL rupture (ICD-9 841.1, 905.7 or ICD-10 S53.30XA, S53.31XA, S53.32XA), and UCL rupture reconstruction (CPT 24346) were used as the main injuries for the patient search.
Data Abstraction
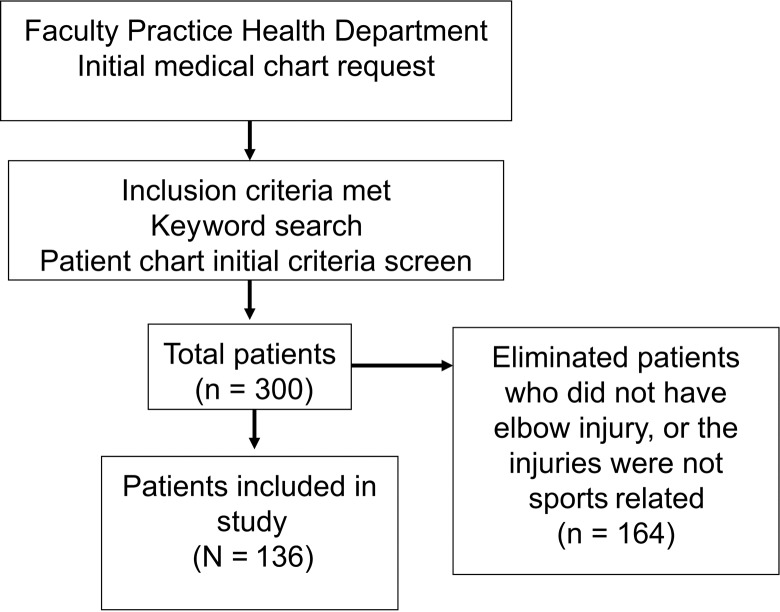
Patient charts were identified using ICD-9, ICD-10, and CPT codes. Using these codes, we added a keyword search to ensure that we obtained every possible UCL injury with our inclusion criteria. The keyword search involved any of the following words in combination with the above codes: athlete, athletic, baseball, basketball, college, elbow, football, high school, javelin, Little League, pitcher, professional, quarterback, soccer, softball, sports, swimming, and tennis. There were 300 total charts initially obtained. After an initial chart screen to check that inclusion was appropriate, this list was narrowed down to 136 charts. Charts that were not included (n = 164) described patient injuries that did not pertain to the above criteria. These included injuries to the olecranon, osteochondritis dissecans of the capitellum, loose bodies of the elbow, ulnar nerve injuries, medial epicondylitis, avulsions of the medial epicondyle, mallet finger, flexor carpi ulnaris strain, stress reactions of the distal humerus and olecranon, UCL injuries of the elbow due to trauma and not related to sports (such as falling off a bicycle), elbow dislocations, lumbago, triceps tendinitis, valgus extension overload syndrome, ulnar fractures, radius fractures due to blunt trauma, plica syndrome, and labral injuries of the shoulder (flow of chart selection process is shown in Figure 1).
Figure 1.
Chart selection process for patients with an ulnar collateral ligament (UCL) injury.
Patient-related data points included age, time of injury per year, sport played, and position in sport. Injury-related data points included injury severity (sprain vs partial tear vs complete rupture of the UCL), hand dominance, injury management (surgical intervention vs nonsurgical management), and imaging modality used to diagnose the injury (clinical examination alone, radiography, magnetic resonance imaging [MRI], magnetic resonance arthrography [MRA], or combination). Injury severity was determined based on a clinical examination combined with imaging (119 underwent advanced imaging of which 82 underwent MRA plus radiographs, 34 underwent MRI plus radiographs, 16 radiograph only, 2 had MRI only, 1 MRA only, and 1 underwent radiographs plus ultrasound only). For statistical analyses, data were categorized based on patient age (11-13, 14-16, and 17-22 years), time frame (4-year clusters spanning 2000-2016), and sport (baseball, javelin, softball, and American football).
For the purposes of this study, the severity of UCL injuries was defined based on the presence of a sprain, partial tear, or complete rupture. This categorization was based on the scheme used by Ford et al.20 A sprain of the UCL had no tear, thickening, or stripping with or without edema around the anterior band, with positive clinical symptoms (such as pain at the sublime tubercle and/or pain with valgus loading of the medial elbow). A partial tear was defined as at least a partial tear of the anterior band of the UCL. A complete rupture was defined as at least a complete tear of the anterior band of the UCL. Position in sport was determined via a chart review and listed per history in each chart.
All surgical reconstruction procedures were performed by board-certified orthopaedic surgeons. All patients were initially evaluated by board-certified primary care sports medicine physicians (primary specialties included physical medicine and rehabilitation, pediatrics, or family medicine), orthopaedic sports medicine surgeons, or pediatric orthopaedic surgeons. All 9 nonoperative primary care sports medicine physicians who were involved in the care of the included patients obtained a certificate of additional qualification in sports medicine and have been team physicians at the high school and/or collegiate levels.
Statistical Analysis
Descriptive statistics of UCL injuries by sport and age group were performed. Differences in injury frequency and severity were determined using chi-square analyses. Odds ratios and 95% CIs were determined for sport type. Statistics were performed using the Statistical Package for the Social Sciences (v24; SPSS).
Results
Injury Severity and Injury Management
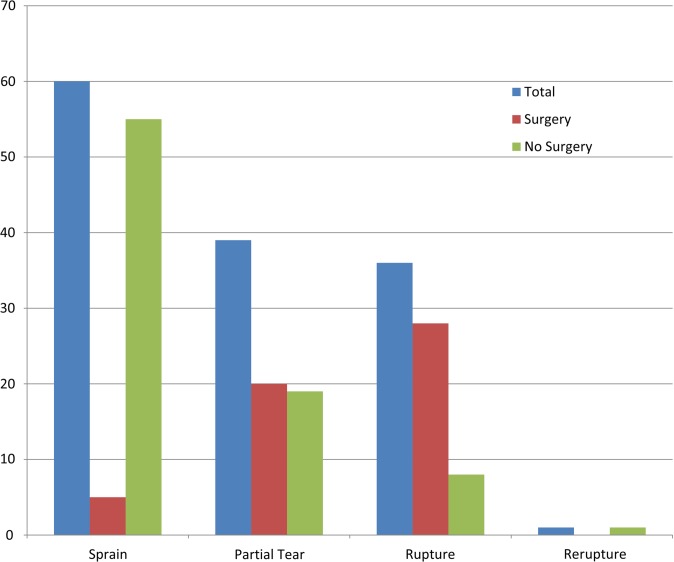
There were 136 total UCL injuries, including 53 that were treated with UCL-R and 83 that were managed conservatively. All patients were assessed clinically and with imaging modalities. There were a total of 60 UCL sprains, 39 partial tears, 36 ruptures, and 1 rerupture (Figure 2). Most sprains did not require surgery, however surgical management increased with greater injury severity. There were 16 patients who underwent radiography only, 34 who underwent radiography plus MRI, 82 who underwent MRA plus radiography, 2 who underwent MRI only, 1 who underwent MRA only, and 1 who underwent radiography plus ultrasound only. All cases of radiography only (plus the 1 case with combined ultrasound) were diagnosed as sprains and did not result in surgery.
Figure 2.
Severity and management type (by No. of injuries) for ulnar collateral ligament injuries among athletes aged 11 to 22 years.
Age at Time of Injury
The mean age at the time of injury for all patients was 16.7 years. The mean age of patients undergoing UCL-R and conservative management was 16.0 and 17.1 years, respectively. Less severe UCL injuries occurred with a higher frequency in younger patients. Patients who sustained sprains had a mean age of 15.9 years, those with partial tears had a mean age of 16.9 years, and patients with ruptures had a mean age of 17.6 years (Table 1). There were increasing numbers of UCL injuries with increasing age (χ2(4, 136) = 14.209, P = .007) (Table 1).
TABLE 1.
Severity of UCL Injury by Agea
| n | Mean Age, y | |
|---|---|---|
| Sprain | 60 | 15.9 |
| Partial tear | 39 | 16.9 |
| Complete tear | 36 | 17.6 |
| Rerupture | 1 | 19.0 |
aThere were increasing numbers of ulnar collateral ligament (UCL) injuries with increasing age (χ2(4, 136) = 14.209, P = .007). UCL sprains accounted for 100.0% of the total injuries in the 11- to 13-year age group, 71.4% in the 14- to 16-year age group, and 44.3% in the 17- to 22-year age group.
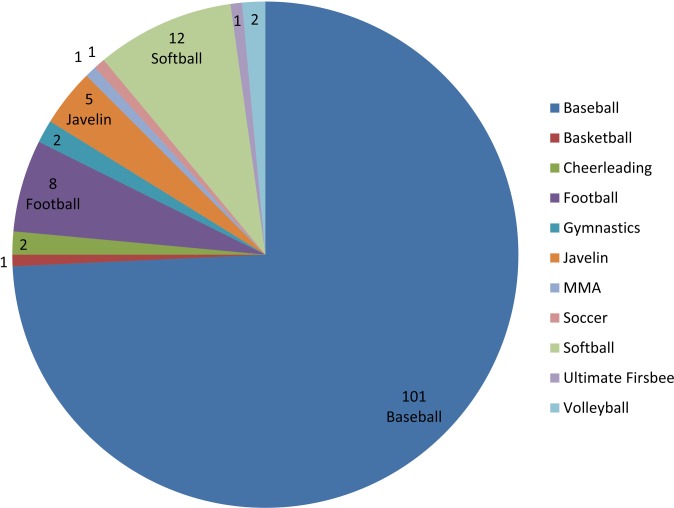
Sport Type and Injury
The injury incidence among different sports is shown in Figure 3. The odds ratio (OR) for UCL injuries was highest in patients who played javelin (OR, 6.69; 95% CI, 0.72-61.62; P = .07) and baseball (OR, 1.55; 95% CI, 0.69-3.51; P = .32) compared with all other sports activities. Of the 42 UCL-R procedures performed on baseball players, 37 were performed on pitchers. There were 20 pitchers who sustained complete ruptures, 14 partial tears, and 3 sprains (2 of which failed rehabilitation).
Figure 3.
Ulnar collateral ligament (UCL) injuries by sport. Values represent the number of cases. MMA, mixed martial arts.
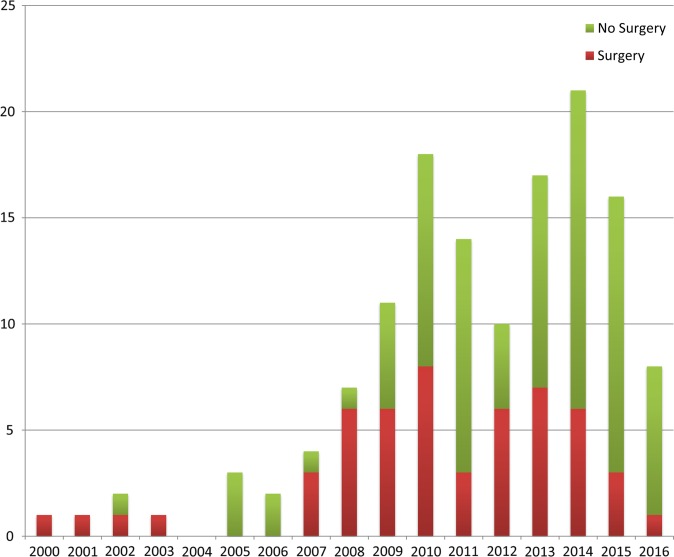
Time Frame and Injury Incidence
There were a total of 5 injuries from 2000 to 2003, 9 from 2004 to 2007, 50 from 2008 to 2011, and 72 from 2012 to April 26, 2016 (date determined according to institutional review board approval). This represented a more than 12-fold increase in less than 16 years (Figure 4).
Figure 4.
Annual incidence of ulnar collateral ligament (UCL) injuries during the time frame from 2000 to 2016. Note that 2016 data were available for a partial year through April 26 (per Institutional Review Board approval).
Discussion
We report that among patients aged 11 to 22 years, those who had less severe UCL injuries were younger compared with patients who had more severe injuries. Fewer surgeries were performed among the patients with less severe injuries. These findings are consistent with our hypotheses. In addition, our data, similar to those of prior large-scale studies, revealed that baseball players (particularly pitchers) sustained the greatest number of UCL injuries.4,41 In our dataset, 101 of our 136 patients were baseball players (74.3%). Furthermore, our findings agree with published trends of the increasing incidence of UCL-R over the past 20 years.7,14,21
While UCL injuries are a well-known issue in baseball players, there have also been reports of UCL injuries in overhead athletes who participate in American football, javelin, gymnastics, softball, tennis, and water polo.11,12,39 Our data revealed that 80% of our javelin athletes and 54% of our baseball pitchers with complete ruptures underwent UCL-R. This is likely in part because of sport-specific biomechanical factors. The severity of UCL injuries is influenced by the amount of stress placed on the medial elbow with overhead throwing. Javelin throwers can generate an angular velocity of about 1900 deg/s, while baseball pitchers can approach nearly 2480 deg/s of elbow angular velocity.9,19 These 2 sports generate the greatest velocity and resulting stress across the medial elbow compared with other overhead-throwing sports. Older and higher-level pitchers throw with greater linear velocity and generate greater torque during the acceleration phase of throwing (nearly 50 N·m at the collegiate level).19
A case can be made that older pitchers also throw more pitches. While it is difficult to differentiate whether higher-level and older pitchers suffer UCL injuries because of more pitches thrown versus greater velocity and forces on the elbow, restrictions have been enacted at the high school level in a majority of states to prevent overuse.31,37 Given new pitch count regulations, future research may be able to differentiate whether an elbow injury was from greater velocity or a greater volume of throwing.
A significant volume of science surrounds UCL-R in the literature4,7,14,41 but not on nonsurgical management. We found that 61% of our UCL injuries did not undergo UCL-R. One study of 18 National Football League players described that 100% of injured players returned to play after nonsurgical management, with a mean loss of game time of 0.64 games.28 However, other studies have reported less success with nonoperative management. For example, 2 studies of overhead-throwing baseball athletes reported a 42% to 50% rate of return to play.3,46 However, there are challenges interpreting these findings because of the absence of injury severity data. The time frame for making the decision to pursue surgery is based on several factors. These include location of the UCL injury, severity of the injury, timing of the injury (in season or out of season), year of the athlete in school, and potential ability to continue playing above the current level of play.45 At our institution, nonoperative management of these injuries typically includes a period of nonthrowing physical therapy until the patient is asymptomatic. We make sure that there is no valgus force or strain applied in any maneuver during this time. The use of orthobiologics is also considered and made on a case-by-case basis.10,44 After the first 6 weeks, return to a throwing program (if the patient is a thrower) is initiated over an approximate 6-week period. After this 3-month period, if the patient continues to have pain and/or difficulty with throwing or overhead activities without a significant improvement in symptoms, then a surgical referral is placed. While this program has evolved over the past 16 years, the overall components have remained the same.
When considering injury prevention in younger athletes, significant research exists surrounding the relationships between an overuse throwing injury and pitch volume, fatigue, rotator cuff weakness, poor pitching mechanics, and possibly year-round pitching.16,18,26,33,50 However, there are no data on the severity of UCL injuries by age and management pathway (Figure 2). In this study, athletes who suffered less severe injuries were younger in age than players who had more severe injuries (Table 1). Surgery was used less frequently in cases where injuries were less severe (Figure 2). We feel that this finding does lend credibility to the notion that athletes are sustaining more UCL injuries at a younger age, and this may predispose these athletes to suffer more severe injuries as they become older. Prior research has reported that 26% to 29% of young baseball athletes suffer from elbow pain.34,36 Even more concerning, youth pitchers between 9 and 14 years old have a 5% risk of a severe injury, which is defined as elbow or shoulder surgery, or retirement from the sport within 10 years due to an injury.18,34
Application of Findings
The challenge is to prevent the further progression of a less severe UCL injury and/or to develop novel treatments as an alternative to UCL surgical intervention in non–full-thickness ruptures. Treatment decision making of UCL injuries is dependent in part on the severity of the injury. Imaging modalities are extremely useful in combination with a thorough history and physical examination. MRI has typically been the standard in identifying UCL injuries, particularly full-thickness tears.20,48 However, there is evidence that MRA may provide additional imaging details for evaluating the severity of UCL injuries, particularly partial tears.5,38,47
Additional challenges arise when trying to determine the severity of partial tears of the UCL. Ford et al20 created an MRI grading scale to classify UCL injuries into 4 levels of severity: I (intact ligament with or without edema), IIA (partial tear with incomplete fiber disruption), IIB (chronic healed injury with thickened ligament but no fiber disruption), and III (complete tear with fiber disruption). Our definitions of a sprain, partial tear, and complete tear of the UCL were based on this scheme. Newer research has developed a UCL classification system using a combination of valgus laxity on radiography in conjunction with MRI. Joyner et al24 proposed a 4-level grading system: type I, edema in the UCL only (called a low-grade partial tear); type II, a partial tear of the UCL with no extravasation of fluid on MRA (called a high-grade partial tear); type III, a complete full-thickness tear of the UCL with extravasation of fluid on MRA; and type IV, a tear in more than 1 location on the UCL. While these newer grading schemes are similar, it is important to note that a correlation of pain must be present to make the diagnosis of a UCL injury. Prior research has shown that overhead athletes, particularly baseball players, may be asymptomatic but still have abnormalities on MRA.22,30,42 Thus, the combination of a clinical examination was required to make the diagnosis of a UCL injury. It should be noted that ultrasonography with an experienced operator is another imaging modality that can be used to make a diagnosis.2,6,27,29
Limitations
This study has various limitations. The retrospective nature precludes the determination of the ultimate use of surgical management. Second, we were unable to ascertain the severity of the partial tears sustained in our dataset. Only reports of MRI and/or MRA were available in some cases, not the images themselves. This limited the classification of partial tears further into lower versus higher grades and could have affected decision making for operative versus nonoperative treatment. In addition, with the growing awareness of UCL injuries, it is possible that this diagnosis is identified more by clinicians now than in the past.40 Injury incidence may not have changed among the sports over time, but the recognition and reporting of the injuries may have improved from 2000 to 2016. Finally, we could not determine what percentage of these injuries in the community came to our facility versus other offices and centers, although our center does have the largest number of fellowship-trained orthopaedic and sports medicine providers in the region.
Conclusion
Younger athletes are more likely to sustain less severe UCL injuries than older athletes in those patients who present for medical care. In this study sample, participation in javelin and baseball was associated with a greater likelihood of UCL injuries compared with other sports. This is the first study to provide data on the volume of nonsurgical UCL injuries among athletes aged 11 to 22 years in a variety of sports. Clinicians need to be aware of the significant rise in nonsurgical UCL injuries in adolescent athletes. These data suggest that the majority of UCL injuries sustained in such athletes do not necessarily require surgical intervention, only severe ones in throwing athletes.
Footnotes
Presented at the International Olympic Committee’s World Conference on Prevention of Injury and Illness in Sport, Monte Carlo, Monaco, March 2017.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the University of Florida (Institutional Review Board No. 201600546).
References
- 1. American Sports Medicine Institute. Adolescent UCL surgery (“Tommy John surgery”). Available at: http://www.asmi.org/research.php?page=research§ion=UCL. Accessed June 5, 2016.
- 2. Atanda A, Buckley PS, Hammoud S, Cohen SB, Nazarian LN, Ciccotti MG. Early anatomic changes of the ulnar collateral ligament identified by stress ultrasound of the elbow in young professional baseball pitchers. Am J Sports Med. 2015;43(12):2943–2949. [DOI] [PubMed] [Google Scholar]
- 3. Barnes DA, Tullos HS. An analysis of 100 symptomatic baseball players. Am J Sports Med. 1978;6(2):62–67. [DOI] [PubMed] [Google Scholar]
- 4. Cain EL, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38(12):2426–2434. [DOI] [PubMed] [Google Scholar]
- 5. Carrino JA, Morrison WB, Zou KH, Steffen RT, Snearly WN, Murray PM. Noncontrast MR imaging and MR arthrography of the ulnar collateral ligament of the elbow: prospective evaluation of two-dimensional pulse sequences for detection of complete tears. Skeletal Radiol. 2001;30(11):625–632. [DOI] [PubMed] [Google Scholar]
- 6. Ciccotti MG, Atanda A, Nazarian LN, Dodson CC, Holmes L, Cohen SB. Stress sonography of the ulnar collateral ligament of the elbow in professional baseball pitchers: a 10-year study. Am J Sports Med. 2014;42(3):544–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Conte SA, Fleisig GS, Dines JS, et al. Prevalence of ulnar collateral ligament surgery in professional baseball players. Am J Sports Med. 2015;43(7):1764–1769. [DOI] [PubMed] [Google Scholar]
- 8. Conte SA, Hodgins JL, ElAttrache NS, Patterson-Flynn N, Ahmad CS. Media perceptions of Tommy John surgery. Phys Sportsmed. 2015;43(4):375–380. [DOI] [PubMed] [Google Scholar]
- 9. Dines JS, Jones KJ, Kahlenberg C, Rosenbaum A, Osbahr DC, Altchek DW. Elbow ulnar collateral ligament reconstruction in javelin throwers at a minimum 2-year follow-up. Am J Sports Med. 2012;40(1):148–151. [DOI] [PubMed] [Google Scholar]
- 10. Dines JS, Williams PN, ElAttrache N, et al. Platelet-rich plasma can be used to successfully treat elbow ulnar collateral ligament insufficiency in high-level throwers. Am J Orthop (Belle Mead NJ). 2016;45(5):296–300. [PubMed] [Google Scholar]
- 11. Dodson CC, Slenker N, Cohen SB, Ciccotti MG, DeLuca P. Ulnar collateral ligament injuries of the elbow in professional football quarterbacks. J Shoulder Elbow Surg. 2010;19(8):1276–1280. [DOI] [PubMed] [Google Scholar]
- 12. Dugas J, Chronister J, Cain EL, Andrews JR. Ulnar collateral ligament in the overhead athlete: a current review. Sports Med Arthrosc Rev. 2014;22(3):169–182. [DOI] [PubMed] [Google Scholar]
- 13. Dugas JR, Walters BL, Beason DP, Fleisig GS, Chronister JE. Biomechanical comparison of ulnar collateral ligament repair with internal bracing versus modified Jobe reconstruction. Am J Sports Med. 2016;44(3):735–741. [DOI] [PubMed] [Google Scholar]
- 14. Erickson BJ, Bach BR, Cohen MS, et al. Ulnar collateral ligament reconstruction: the Rush experience. Orthop J Sports Med. 2016;4(1):2325967115626876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Erickson BJ, Chalmers PN, Bush-Joseph CA, Verma NN, Romeo AA. Ulnar collateral ligament reconstruction of the elbow: a systematic review of the literature. Orthop J Sports Med. 2015;3(12):2325967115618914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Erickson BJ, Harris JD, Tetreault M, Bush-Joseph C, Cohen M, Romeo AA. Is Tommy John surgery performed more frequently in Major League Baseball pitchers from warm weather areas? Orthop J Sports Med. 2014;2(10):2325967114553916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Erickson BJ, Nwachukwu BU, Rosas S, et al. Trends in medial ulnar collateral ligament reconstruction in the United States: a retrospective review of a large private-payer database from 2007 to 2011. Am J Sports Med. 2015;43(7):1770–1774. [DOI] [PubMed] [Google Scholar]
- 18. Fleisig GS, Andrews JR, Cutter GR, et al. Risk of serious injury for young baseball pitchers: a 10-year prospective study. Am J Sports Med. 2011;39(2):253–257. [DOI] [PubMed] [Google Scholar]
- 19. Fleisig GS, Bolt B, Fortenbaugh D, Wilk KE, Andrews JR. Biomechanical comparison of baseball pitching and long-toss: implications for training and rehabilitation. J Orthop Sports Phys Ther. 2011;41(5):296–303. [DOI] [PubMed] [Google Scholar]
- 20. Ford GM, Genuario J, Kinkartz J, Githens T, Noonan T. Return-to-play outcomes in professional baseball players after medial ulnar collateral ligament injuries: comparison of operative versus nonoperative treatment based on magnetic resonance imaging findings. Am J Sports Med. 2016;44(3):723–728. [DOI] [PubMed] [Google Scholar]
- 21. Hodgins JL, Vitale M, Arons RR, Ahmad CS. Epidemiology of medial ulnar collateral ligament reconstruction: a 10-year study in New York state. Am J Sports Med. 2016;44(3):729–734. [DOI] [PubMed] [Google Scholar]
- 22. Hurd WJ, Eby S, Kaufman KR, Murthy NS. Magnetic resonance imaging of the throwing elbow in the uninjured, high school-aged baseball pitcher. Am J Sports Med. 2011;39(4):722–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Johnson CC, Garcia GH, Liu JN, Stepan JG, Patel RM, Dines JS. Internet resources for Tommy John injuries: what are patients reading? J Shoulder Elbow Surg. 2016;25(12):e386–e393. [DOI] [PubMed] [Google Scholar]
- 24. Joyner PW, Bruce J, Hess R, Mates A, Mills FB, Andrews JR. Magnetic resonance imaging-based classification for ulnar collateral ligament injuries of the elbow. J Shoulder Elbow Surg. 2016;25(10):1710–1716. [DOI] [PubMed] [Google Scholar]
- 25. Kacprowicz RF. Ulnar collateral ligament injury. Available at: http://emedicine.medscape.com/article/97451-overview. Accessed June 15, 2016.
- 26. Kaplan KM, Elattrache NS, Jobe FW, Morrey BF, Kaufman KR, Hurd WJ. Comparison of shoulder range of motion, strength, and playing time in uninjured high school baseball pitchers who reside in warm- and cold-weather climates. Am J Sports Med. 2011;39(2):320–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Keller RA, Marshall NE, Bey MJ, et al. Pre- and postseason dynamic ultrasound evaluation of the pitching elbow. Arthroscopy. 2015;31(9):1708–1715. [DOI] [PubMed] [Google Scholar]
- 28. Kenter K, Behr CT, Warren RF, O’Brien SJ, Barnes R. Acute elbow injuries in the National Football League. J Shoulder Elbow Surg. 2000;9(1):1–5. [DOI] [PubMed] [Google Scholar]
- 29. Kim NR, Moon SG, Park J-Y, Choi JW, Oh K-S. Stress ultrasound in baseball players with ulnar collateral ligament injuries: additional value for predicting rehabilitation outcome. J Shoulder Elbow Surg. 2017;26(5):815–823. [DOI] [PubMed] [Google Scholar]
- 30. Kooima CL, Anderson K, Craig JV, Teeter DM, van Holsbeeck M. Evidence of subclinical medial collateral ligament injury and posteromedial impingement in professional baseball players. Am J Sports Med. 2004;32(7):1602–1606. [DOI] [PubMed] [Google Scholar]
- 31. Lara-Cinisomo V. High school body mandates pitch count restrictions. Available at: http://www.baseballamerica.com/college/high-school-body-mandates-pitch-count-restrictions/. Accessed March 3, 2017.
- 32. Lee ML, Rosenwasser MP. Chronic elbow instability. Orthop Clin North Am. 1999;30(1):81–89. [DOI] [PubMed] [Google Scholar]
- 33. Lyman S, Fleisig GS, Andrews JR, Osinski ED. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30(4):463–468. [DOI] [PubMed] [Google Scholar]
- 34. Lyman S, Fleisig GS, Waterbor JW, et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001;33(11):1803–1810. [DOI] [PubMed] [Google Scholar]
- 35. Mahure SA, Mollon B, Shamah SD, Kwon YW, Rokito AS. Disproportionate trends in ulnar collateral ligament reconstruction: projections through 2025 and a literature review. J Shoulder Elbow Surg. 2016;25(6):1005–1012. [DOI] [PubMed] [Google Scholar]
- 36. Matsuura T, Suzue N, Iwame T, Arisawa K, Fukuta S, Sairyo K. Epidemiology of shoulder and elbow pain in youth baseball players. Phys Sportsmed. 2016;44(2):97–100. [DOI] [PubMed] [Google Scholar]
- 37. MLB.com. Pitch smart. Available at: http://m.mlb.com/pitchsmart/pitching-guidelines/. Accessed August 31, 2016.
- 38. Nakanishi K, Masatomi T, Ochi T, et al. MR arthrography of elbow: evaluation of the ulnar collateral ligament of elbow. Skeletal Radiol. 1996;25(7):629–634. [DOI] [PubMed] [Google Scholar]
- 39. O’Brien DF, O’Hagan T, Stewart R, et al. Outcomes for ulnar collateral ligament reconstruction: a retrospective review using the KJOC assessment score with two-year follow-up in an overhead throwing population. J Shoulder Elbow Surg. 2015;24(6):934–940. [DOI] [PubMed] [Google Scholar]
- 40. Ortiz JL. Tommy John surgery now “an epidemic.” USA Today. April 11, 2014. Available at: http://www.usatoday.com/story/sports/mlb/2014/04/11/tommy-john-elbow-surgery-strasburg-parker-corbin/7583413/. Accessed October 7, 2016.
- 41. Osbahr DC, Cain EL, Raines BT, Fortenbaugh D, Dugas JR, Andrews JR. Long-term outcomes after ulnar collateral ligament reconstruction in competitive baseball players: minimum 10-year follow-up. Am J Sports Med. 2014;42(6):1333–1342. [DOI] [PubMed] [Google Scholar]
- 42. Pennock AT, Pytiak A, Stearns P, et al. Preseason assessment of radiographic abnormalities in elbows of Little League baseball players. J Bone Joint Surg Am. 2016;98(9):761–767. [DOI] [PubMed] [Google Scholar]
- 43. Petty DH, Andrews JR, Fleisig GS, Cain EL. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med. 2004;32(5):1158–1164. [DOI] [PubMed] [Google Scholar]
- 44. Podesta L, Crow SA, Volkmer D, Bert T, Yocum LA. Treatment of partial ulnar collateral ligament tears in the elbow with platelet-rich plasma. Am J Sports Med. 2013;41(7):1689–1694. [DOI] [PubMed] [Google Scholar]
- 45. Rebolledo BJ, Dugas JR, Bedi A, Ciccotti MG, Altchek DW, Dines JS. Avoiding Tommy John surgery [published online March 1, 2017]. Am J Sports Med. doi:10.1177/0363546517692548. [DOI] [PubMed] [Google Scholar]
- 46. Rettig AC, Sherrill C, Snead DS, Mendler JC, Mieling P. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am J Sports Med. 2001;29(1):15–17. [DOI] [PubMed] [Google Scholar]
- 47. Schwartz ML, al-Zahrani S, Morwessel RM, Andrews JR. Ulnar collateral ligament injury in the throwing athlete: evaluation with saline-enhanced MR arthrography. Radiology. 1995;197(1):297–299. [DOI] [PubMed] [Google Scholar]
- 48. Timmerman LA, Andrews JR. Undersurface tear of the ulnar collateral ligament in baseball players: a newly recognized lesion. Am J Sports Med. 1994;22(1):33–36. [DOI] [PubMed] [Google Scholar]
- 49. Watson JN, McQueen P, Hutchinson MR. A systematic review of ulnar collateral ligament reconstruction techniques. Am J Sports Med. 2014;42(10):2510–2516. [DOI] [PubMed] [Google Scholar]
- 50. Zaremski JL, Horodyski M, Donlan RM, Brisbane ST, Farmer KW. Does geographic location matter on the prevalence of ulnar collateral ligament reconstruction in collegiate baseball pitchers? Orthop J Sports Med. 2015;3(11):2325967115616582. [DOI] [PMC free article] [PubMed] [Google Scholar]