Abstract
Background
Little is known about the feasibility of providing massage or music therapy to medical inpatients at urban safety-net hospitals or the impact these treatments may have on patient experience.
Objective
To determine the feasibility of providing massage and music therapy to medical inpatients and to assess the impact of these interventions on patient experience.
Design
Single-center 3-arm feasibility randomized controlled trial.
Setting
Urban academic safety-net hospital.
Patients
Adult inpatients on the Family Medicine ward.
Interventions
Massage therapy consisted of a standardized protocol adapted from a previous perioperative study. Music therapy involved a preference assessment, personalized compact disc, music-facilitated coping, singing/playing music, and/or songwriting. Credentialed therapists provided the interventions.
Measurements
Patient experience was measured with the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) within 7 days of discharge. We compared the proportion of patients in each study arm reporting “top box” scores for the following a priori HCAHPS domains: pain management, recommendation of hospital, and overall hospital rating. Responses to additional open-ended postdischarge questions were transcribed, coded independently, and analyzed for common themes.
Results
From July to December 2014, 90 medical inpatients were enrolled; postdischarge data were collected on 68 (76%) medical inpatients. Participants were 70% females, 43% non-Hispanic black, and 23% Hispanic. No differences between groups were observed on HCAHPS. The qualitative analysis found that massage and music therapy were associated with improved overall hospital experience, pain management, and connectedness to the massage or music therapist.
Conclusions
Providing music and massage therapy in an urban safety-net inpatient setting was feasible. There was no quantitative impact on HCAHPS. Qualitative findings suggest benefits related to an improved hospital experience, pain management, and connectedness to the massage or music therapist.
Keywords: patient experience, patient satisfaction, Hospital Consumer Assessment of Healthcare Providers and Systems, massage therapy, music therapy, inpatient medicine
Introduction
Positive patient experience is associated with clinically effective care.1 A widely used measurement of patient experience, the Hospital Consumer Assessment of Healthcare Provider Survey (HCAHPS), allows hospitals to be compared nationally and can affect Medicare and Medicaid reimbursement.2 Inpatients frequently present with complex medical histories and a range of symptoms that require medical management, eg, pain, anxiety, and insomnia. Inpatients from low-income communities are more likely to report inadequate symptom management during inpatient care,3 and safety-net hospitals, on average, receive lower HCAHPS scores.4 Expanding treatment options for medical inpatients at safety-net hospitals may aid symptom management and enhance inpatient experience.
Massage5,6 and music therapy7–10 may improve the experience of medical inpatients and reduce bothersome symptoms, eg, pain and anxiety. While these therapies have been evaluated in hospital settings,11–20 little is known about the feasibility and impact of providing massage or music therapy for medical inpatients in urban safety-net hospitals. Thus, we conducted a prospective, 3-arm, parallel design mixed-methods randomized controlled trial comparing massage therapy, music therapy, and usual care. We hypothesized that it would be feasible to implement massage and music therapy in a busy safety-net hospital medical inpatient service and that participants would report a better patient experience on the HCAHPS questionnaire and in qualitative interviews.
Methods
Participants
We recruited 90 medical inpatients at Boston Medical Center, a tertiary care urban safety-net hospital. English- or Spanish-speaking inpatients admitted to the family medicine inpatient service age 18 years or older were eligible. Participants had to be willing to accept either massage or music therapy when randomized. Exclusion criteria included contact or respiratory precautions, clotting disorders, eg, due to thrombocytopenia and hemophilia, and altered mental status or inability to provide informed consent, eg, due to hepatic encephalopathy, alcohol withdrawal, and dementia. Inpatients were also excluded if they required constant one-on-one supervision, eg, due to incarceration or psychosis, or if the attending physician or nurse did not approve their participation due to safety or other health concerns. Inpatients admitted under “observation status” (ie, expected to be discharged within 24 h) were also excluded.
Study staff screened newly admitted inpatients through review of the electronic medical record and confirmed eligibility with the attending physician or nurse. Study staff approached potentially eligible inpatients and provided a detailed explanation of the risks, benefits, and alternatives to participation. Patients provided written consent. Directly following consent, inpatients were randomized in a 1:1:1 ratio using a permuted block method with varying block sizes to receive daily massage therapy, music therapy, or usual care for the duration of their admission. Research assistants assigned a treatment group to newly enrolled participants through sequential opening of consecutively numbered opaque envelopes previously prepared by one of the authors who had no patient contact (CL). The Boston University Medical Campus Institutional Review Board approved the study.
Interventions
Inpatients randomized to massage or music therapy were offered a 10- to 40-min therapy session each day during their stay from a licensed massage therapist or board-certified music therapist, respectively.
Massage therapy
We adapted a study protocol previously developed for perioperative care.11 Before the start of the study, research staff and 5 study massage therapists reviewed the protocol for face and content validity, and suggestions were incorporated. The resulting semistandardized inpatient massage protocol included Swedish and acupressure techniques (Appendix 1). The therapist tailored the intervention to the needs and preferences of individual inpatients. Unscented lotion was used at the therapists’ discretion.
Music therapy
A 2-phase intervention was based on previous research protocols developed by Hanser (Appendix 2).19–21 The music therapist assessed each participant’s needs to determine goals, such as management of pain, anxiety, or other symptoms. During the first phase of the intervention, the therapist created a customized music playlist on a CD and provided a portable CD player with headphones for use in the hospital and after discharge. Follow-up visits in the second phase of the intervention included music-facilitated relaxation/meditation, songwriting, singing, and other techniques.
Usual care
The control group continued to receive usual medical care during their admission. After completing the study, participants were offered a choice of either a voucher for 1 free outpatient massage therapy session at the hospital or a music meditation CD.
Data Collection
Feasibility
Study staff recorded total number of patients admitted during the entire study period, including number of eligible and consented participants. For enrolled participants, we extracted sociodemographic characteristics from their electronic medical record. Therapists noted the total number and duration of massage or music therapy sessions provided to each participant. Study staff instructed patients during the informed consent process to self-report any potential adverse events to the music or massage therapist, study staff, or principal investigator. Music and massage therapists were also instructed to note any potential adverse events to study staff.
Patient experience
Unblinded research staff measured patient experience using the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey through telephone interviews within 7 days of hospital discharge (Appendix 3).22 The HCAHPS survey is used nationally to measure patient experience in hospital settings and includes 27 questions regarding various aspects of the hospital stay captured in 9 domains. We assessed 3 individual domains of the HCAHPS survey identified a priori: pain management, recommendation of hospital, and overall hospital rating. We identified “top box” participants22 who selected the most favorable answer for individual HCAHPS questions. The “top box” response was “always” for 2 questions on pain management, eg, their pain was “always” well controlled; “definitely yes” for likelihood of recommending hospital; and a score of 9 or 10 for overall hospital rating.
Qualitative
For participants receiving massage or music therapy interventions, we also asked 10 open-ended questions in our telephone survey regarding the effect of the therapy on pain, hospital experience, and frequency of use (Appendix 4). Research staff transcribed verbatim the patients’ responses.
Data Analysis
Participant sociodemographic and health information was summarized using descriptive statistics. We compared the proportion of “top box” participants in each group for pain management, recommendation of hospital, and overall hospital rating domains using the χ2 test. Data were analyzed using the intention to treat method and SAS version 9.3 statistical software (SAS Institute, Cary, NC).
We evaluated responses to open-ended survey questions using thematic analysis.23 An iterative process of meeting, discussion, and consensus was used. After an initial review, 2 team members (OC and KR) agreed upon a uniform list of codes, independently coded the transcripts, and grouped them into higher order themes. A third researcher (JW) helped reach consensus when there were differences.
Results
Study Population
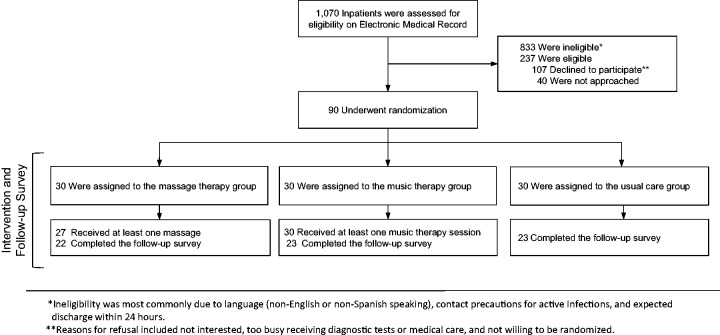
Of 1070 medical inpatients admitted from July to December 2014, 237 met eligibility criteria, and 90 were enrolled and successfully randomized (Figure 1). The majority were racial and ethnic minorities and reported having pain at admission (Table 1). Although the principal admitting diagnosis varied widely, the most common were gastrointestinal (20%), cardiac (16%), and pulmonary (14%) (Table 2).
Figure 1.
Study Flow Diagram.
Table 1.
Baseline Characteristics of 90 Participants Randomized to Massage Therapy, Music Therapy, or Usual Care.
| Characteristic | Massage Therapy (n = 30) | Music Therapy (n = 30) | Usual Care (n = 30) | P Value |
|---|---|---|---|---|
| Mean age, years (SD) | 55.4 (16) | 51.6 (16) | 56.1 (16) | .49 |
| Female, n (%) | 22 (73) | 17 (57) | 24 (80) | .13 |
| Race/ethnicity, n (%) | .82 | |||
| Non-Hispanic black | 13 (43) | 14 (47) | 11 (37) | |
| Non-Hispanic white | 8 (27) | 7 (23) | 6 (20) | |
| Hispanic | 8 (27) | 7 (23) | 9 (30) | |
| Other | 1 (3) | 2 (7) | 4 (13) | |
| Participants w/pain >0, n (%) | 17 (57) | 18 (60) | 17 (57) | .95 |
SD: standard deviation.
Table 2.
Common Categories for Principal Admitting Diagnosis Among 90 Medical Inpatients.
| n (%) | |
|---|---|
| Gastrointestinal (eg, abdominal pain, gastrointestinal bleeding) | 18 (20%) |
| Cardiac (eg, chest pain, congestive heart failure) | 14 (16%) |
| Pulmonary (eg, COPD, asthma exacerbation) | 13 (14%) |
| Infection (eg, cellulitis, fever) | 10 (11%) |
| Renal/genitourinary (eg, pyelonephritis) | 8 (9%) |
| Hematology/allergy (eg, sickle cell crisis, anemia) | 6 (7%) |
| Diabetes (eg, hypoglycemia, diabetic foot ulcer) | 6 (7%) |
| Musculoskeletal (eg, back pain, cervical radiculopathy) | 5 (6%) |
| Othera | 10 (11%) |
COPD: chronic obstructive pulmonary disease.
aOther categories included neurologic, trauma, alcohol withdrawal, and postsurgical admission.
Intervention Feasibility
Fifty-four massage and 96 music therapy sessions were administered during the study. In both treatment arms, a median of 1 treatment (range: 0–2) was administered per participant per day. Mean lengths of sessions were 35 (range: 15–60) and 40 (range: 5–90) min for massage and music, respectively. All music therapy participants received a CD (phase I of protocol) and 29 (97%) engaged in phase 2 which included songwriting, lyric analysis, and other music therapy interventions. Reasons for delaying or missing a daily session of massage or music therapy included sleeping or too tired, being discharged currently or shortly, meeting with hospital care team, off the floor for testing, with family/visitors, speaking on the phone, and not feeling well. No adverse events potentially attributed to a study intervention were reported during the duration of the study. Two participants (1 massage therapy and 1 usual care) died within 1 week after leaving the hospital for reasons not related to the study.
Patient Experience
We collected postdischarge survey data on 68 (76%) patients. Patient experience scores are summarized in Table 3, showing “top box” and average scores. We observed no differences between groups for pain management, recommendation of hospital, and overall hospital rating domains.
Table 3.
Patient Experience “Top Box” Scores Using Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) Administered over the Phone Within 7 Days of Hospital Discharge.
| HCAHPS Questions | Massage Therapy (n = 22)a | Music Therapy (n = 23)a | Usual Care (n = 23)a | P Value |
|---|---|---|---|---|
| “During this hospital stay, how often was your pain well controlled?” Response of “always,” n (%) | 7/18 (39) | 7/19 (37) | 10/16 (63) | .60 |
| “During this hospital stay, how often did the hospital staff do everything they could to help you with your pain?” Response of “always,” n (%) | 14/18 (78) | 11/19 (58) | 12/16 (75) | .72 |
| “Would you recommend this hospital to your friends and family?” Response of “definitely yes,” n (%) | 14 (64) | 14 (61) | 17 (74) | .67 |
| Overall rating of hospital (0 = worst possible, 10 = best possible), Response of 9 or 10, n (%) | 9 (30) | 12 (40) | 13 (43) | .54 |
aAll percentages use this denominator except if otherwise noted.
Qualitative Analysis
Patients’ experience of massage or music therapy centered on 3 main themes: improvement in overall hospital stay, improved pain management, and increased connectedness to the massage or music therapist.
Improved overall hospital experience
Thirteen massage therapy and 17 music therapy participants mentioned that the interventions improved their overall hospital stay. For many patients, despite common negative perceptions of being hospitalized, eg, constant noise and difficulty feeling rested, massage or music therapy resulted in reporting a positive hospital experience. Reasons for this included improved sleep quality, relaxation, and distraction from hospital distress. Environmental factors causing distress included sharing a hospital room and noise (alarms, staff, or other patients). Massage therapy was often linked to physical relaxation, while music therapy tended to yield a more healing environment.
The massage therapy sessions made me feel like I mattered in the hospital. Overall, it made me feel comfortable in the hospital, which is not easy.
My hospital experience was made more stressful because of my roommate. I have to say that the massage sessions definitely improved that aspect.
[Music therapy] just brought me to a whole other place in my head. It wasn’t about being miserable in the hospital room. It was about getting better.
I was a little anxious in the hospital. Just your normal anxiety. Listening to the music, especially the live keyboard played in my room, was very soothing and changed the mood in the room. The room felt more calm. This made me feel less stressful.
Improved pain management
Fourteen massage and 5 music therapy participants described positive effects on pain. Massage therapy participants with pain reported substantial short-term reduction in pain intensity. In contrast, music therapy appeared to improve ability to cope with the pain, even if the overall intensity did not change.
Let [me] put it this way, when I was there in the hospital, the pain from my foot was a 10. After I got massage from the study, my pain would go down to a 3.5 or 4 and stayed that way for a good bit of time.
[Massage] soothed the pain and made it more bearable. I didn’t feel pain during the massage and felt better after.
The music therapy was good for my pain. It eased my pain. Maybe it didn’t lower my pain, but the music made me forget about the pain for a while.
My pain levels themselves did not change much, but I did notice that the throbbing nature of my pain improved and became less noticeable during the music therapy sessions. The music therapy sessions helped me focus away from my pain.
Connectedness
Connectedness, defined as the closeness of the relationship between a patient and a massage or music therapist, emerged as a third theme.24 Three massage therapy and 9 music therapy participants mentioned the relationship and level of connection the patient felt with the therapist. Participants valued having someone to talk to and attention given by the therapist.
No one wants to be in the hospital or call it home. Having the [massage] therapist there to talk to, to provide relief, the whole thing made me feel comfortable and cared for really.
It was nice to have company in the hospital room. I was laughing and had fun with the [music] therapist.
[With music therapy] it was good to connect to someone too. Sucks to just lay there and not have anyone to be there with you.
Discussion
In this trial based at an urban safety-net hospital, we found it feasible to recruit, enroll, and successfully randomize 90 medical inpatients to 2 new services—massage and music therapy—and compare their experience with those receiving usual care. Massage or music therapy compared to usual care did not show any statistically significant differences in HCAHPS, a standardized quantitative measure of patient experience. In contrast, qualitative data from massage and music therapy participants suggest that both interventions improved their overall hospital experience, pain management, and connectedness to the massage or music therapist.
Our results were not consistent with a previous case–control study of music therapy that found an increased likelihood of medical inpatients recommending the hospital on HCAHPS.7 Additional studies of massage5 and music therapy8 have demonstrated improved patient experience using Likert satisfaction scores and the Press Ganey Inpatient Survey, respectively. This is the first study to report the impact of massage or music therapy on the “Pain Management” HCAHPS domain. While systematic reviews of massage6 and music9,10 therapy suggest that these therapies effectively reduce pain, we did not see a difference between groups on the HCAHPS pain management domain. In contrast, our participants’ responses to open-ended questions reflected themes of improved pain management. For massage therapy, patients reported an immediate, albeit temporary, reduction in pain intensity. For music therapy, patients reported distraction from their pain, making the pain less bothersome.
Patient experience is complex and influenced by many aspects of care and environment. Given the complexity of patient experience, a single intervention like massage or music therapy may not be sufficient to elicit changes in HCAHPS score metrics. While increasing the dosage of either therapy (session duration and frequency) may improve patient experience, it was challenging in our environment to provide additional massage or music therapy sessions when considering therapist staffing, potential interruptions, eg, testing, rounds, related to a busy hospital environment, and relatively brief hospital stays. Furthermore, patient preference was not incorporated into choice of therapy, which may have limited the potential benefit to patient experience.
Our study had important limitations. As this was a feasibility study, a lack of quantitative findings may be due to limited statistical power. Our small sample was heterogeneous, with patients presenting with various admitting diagnoses. Previous work has shown that different health conditions are independently associated with patient experience scores.25,26 Additionally, pain patients were a subset of randomized patients, and therefore, randomization may not have been preserved. Our trial also excluded participants who were willing to be randomized to one therapy but not the other. Lastly, our outcome assessors were not blinded to treatment allocation during phone interviews. Since it would not be possible to collect the qualitative data without knowing allocation, it would have been ideal for blinded staff to collect the HCAHPs and unblinded staff gather qualitative data. However, due to resource limitations for this small pilot study, this was not feasible.
Future work should evaluate less heterogeneous samples to try to identify subgroups that would particularly benefit.26 Studies that incorporate patient preference may also be useful. Preference for a specific therapy over another may predict a more favorable response.27 Our qualitative findings suggest that massage and music therapy provided temporary, yet clinically meaningful, pain reduction which may have subsequently reduced use of pain medication. This is in contrast with our quantitative assessment of pain management, ie, HCAHPS questionnaire, which did not show any differences between massage, music therapy, and usual care. However, HCAHPS questions were assessed at a single time point (within 1 week after discharge from the hospital) and may not have captured temporary pain relief immediately following massage or music therapy sessions. Future studies should use disease or symptom-specific outcome measures at baseline and multiple time points to better characterize symptom management over the duration of hospital stay. It would also be helpful to measure a range of symptoms, eg, pain, anxiety, depression, fatigue, immediately before and after sessions. Whether any reduction in pain or pain perception is associated with lower analgesic and psychotropic medication use could also be determined. More in-depth interviews in future trials may reveal additional themes relevant to improving patient experience and suggest alternative assessments or methodologies. Finally, the potential for massage or music therapists to improve the work environment and workload for the physician, nursing, and ancillary staff is yet to be tested.
Conclusion
In summary, providing massage and music therapy in an urban safety-net inpatient setting was feasible. Preliminary findings do not suggest a quantitative impact on HCAHPS pain management, recommendation of hospital, and overall hospital rating domains. However, qualitative findings suggest benefits related to a better hospital experience, improved pain management, and connectedness to the massage or music therapist. Additional larger studies with expanded outcome measurement, eg, evaluating pain and medication use immediately before and after intervention, are needed to further assess the therapeutic effects of massage and music therapy in the inpatient setting.
Appendix 1: Massage Therapy Protocol
During their stay on the inpatient unit, patients randomized to the massage therapy group received 1 to 3 massage sessions a day with each session lasting 10 to 40 min. Working with experts in hospital-based massage therapy, we developed a semistandardized inpatient massage protocol that utilized Swedish techniques and acupressure. The protocol was adapted from our previous study of massage for perioperative care of patients undergoing implantation of permanent intravenous access devices. (11)
The protocol was designed for patients to receive massage while in their hospital bed or chair. Thus, the massage protocol focused on the hands, feet, arms, and neck. However, the massage therapist also covered the shoulders, back, scalp, and head, when possible.
Comfort of the patient was prioritized, so the protocol below served as a guideline. Adjustments in the massage techniques and their order were made by the massage therapist.
Suggested Massage Protocol:
Effleurage strokes from hand to shoulders 3 times and effleurage strokes at shoulder joint 3 times; repeat other side.
Gentle compression to shoulders.
Hand massage including pressure on acupressure points LI 4, P6; repeat other side.
Cradle hold head.
Finger-tip massage on the whole scalp up to the forehead.
Light-stroking effleurage over the forehead.
Circular light strokes over the temple region; finished with a slight compression hold.
Effleurage down sides of neck with gentle strokes.
Gentle, light downward pressure to shoulders.
Effleurage and petrissage of upper and lower back.
Effleurage across shoulders and down arms.
Light-stroking effleurage down legs.
Foot massage bilaterally.
Appendix 2: Music Therapy Protocol
Patients randomized to the music therapy condition received 1 or 2 music therapy sessions of 10- to 40-min duration, each day of their stay in the Family Medicine Inpatient Unit. The Music Therapy Protocol consisted of 2 phases.
Phase 1: Each patient was given a brief introduction to music therapy and the music therapy protocol. A board-certified music therapist then conducted an informal assessment of clinical objectives, eg, pain/anxiety management, learning coping strategies, psychosocial support, opportunities for emotional expression. To assess music preferences and background, the music therapist utilized iTunes to sample music of preferred genres and artists, allowing the patient to listen passively and discuss the memories and associations elicited by this music. The music therapist created a playlist of 12 preferred songs on iTunes and burned those onto a CD. The patient was given the opportunity to title the CD and select an image for the CD label. Each participant was then provided with this personalized CD, 1 portable CD player with headphones, and a prerecorded CD, “Manage Your Stress and Pain Through Music” by Hanser and Mandel.21 The patient was encouraged to listen to both CDs as often as desired.
Phase 2: This phase encompassed follow-up visits that included a variety of passive and active music therapy interventions.21 Examples included the following:
Passive: Music listening to preferred music
Music-assisted relaxation, based on:
Positive suggestion
Progressive muscle relaxation
Breathing techniques/mindfulness
Guided imagery
Active: Singing
Playing/learning instruments
Lyric analysis
Lyric substitution
Improvisation
Drumming
Music-facilitated coping strategies
Songwriting and composition (when possible)
Recording of original songs
Opportunities to compose music and write songs were provided, when feasible, given patient interest and sufficient length of hospital stay. This original music was recorded using the application, GarageBand (http://www.apple.com/ios/garageband), and burned onto a CD for the patient to listen to and take home.
Appendix 3: Postdischarge HCAHPS Survey
| HCAHPS Questions | |||||
|---|---|---|---|---|---|
| Please answer the questions in this survey about your recent stay at Boston Medical Center. When thinking about your answers, do not include any other hospital stays. | |||||
| Domain: Communication with nurses | |||||
| 1. During this hospital stay, how often did nurses treat you with courtesy and respect? | Never | Sometimes | Usually | Always | NA or DK |
| 2. During this stay, how often did nurses listen carefully to you? | Never | Sometimes | Usually | Always | NA or DK |
| 3. During this stay, how often did nurses explain things in a way you could understand? | Never | Sometimes | Usually | Always | NA or DK |
| Domain: Responsiveness to hospital staff 4. During this stay, after you pressed the call button, how often did you get help as soon as you wanted it? | Never | Sometimes | Usually | Always | NA or DK |
| 5. During this hospital stay, did you need help from nurses or other staff in getting to the bathroom or using a bedpan? [STAFF: If don’t know, answer NO] | Yes | No | |||
| 6. How often did you get help getting to the bathroom or using a bedpan as soon as you wanted? | Never | Sometimes | Usually | Always | NA or DK |
| Domain: Communication with doctors | |||||
| 7. During this stay, how often did doctors treat you with courtesy and respect? | Never | Sometimes | Usually | Always | NA or DK |
| 8. During this stay, how often did doctors listen carefully to you? | Never | Sometimes | Usually | Always | NA or DK |
| 9. During this stay, how often did doctors explain things in a way you could understand? | Never | Sometimes | Usually | Always | NA or DK |
| Domain: Cleanliness of hospital environment | |||||
| 10. During this stay, how often were your room and bathroom kept clean? | Never | Sometimes | Usually | Always | NA or DK |
| Domain: Quietness of hospital environment | |||||
| 11. During this stay, how often was the area around your room quiet at night? | Never | Sometimes | Usually | Always | NA or DK |
| Domain: Pain management | |||||
| 12. On a scale of 0 to 10, with 0 being no pain and 10 being the worst possible pain, how would you rate your pain right now? | 0 1 2 3 4 5 6 7 8 9 10 | ||||
| 13. During this hospital stay, did you need medicine for pain? [STAFF: If don’t know, answer NO] | Yes | No | |||
| 14. During this hospital stay, how often was your pain well controlled? | Never | Sometimes | Usually | Always | NA or DK |
| 15. During this hospital stay, how often did the hospital staff do everything they could to help you with your pain? | Never | Sometimes | Usually | Always | NA or DK |
| 16. On a scale of 0 to 10, with 0 being no anxiety and 10 being the worst possible anxiety, how would you rate your anxiety right now? | 0 1 2 3 4 5 6 7 8 9 10 | ||||
| 17. During this hospital stay, did you need medicine for anxiety? [STAFF: If don’t know, answer NO] | Yes | No | |||
| Domain: Communication about Medicines | |||||
| 18. During this hospital stay, were you given any medicine that you had not taken before? [STAFF: If don’t know, answer NO] | Yes | No | |||
| 19. Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? | Never | Sometimes | Usually | Always | NA or DK |
| 20. Before giving you any new medicine, how often did hospital staff describe possible side effects in a way you could understand? | Never | Sometimes | Usually | Always | NA or DK |
| The next questions are about when you left the hospital. | |||||
| 21. After you left the hospital, did you go directly to: your own home, someone else’s home, or to another health facility? | Your own home | Someone else’s home | Another health facility | ||
| 22. During this hospital stay, did doctors, nurses, or other staff talk with you about whether you would have the help you needed when you left the hospital? [STAFF: If don’t know, answer NO] | Yes | No | |||
| 23. During this hospital stay, did you get information in writing about what symptoms or health problems to look out for after you left the hospital? [STAFF: If don’t know, answer NO] | Yes | No | |||
| Domain: Overall rating of hospital | |||||
| 24. Using any number from 0 to 10, where 0 is the worst hospital possible and 10 is the best hospital possible, what number would you use to rate this hospital during your stay? | 0 1 2 3 4 5 6 7 8 9 10 | ||||
| Domain: Recommend the hospital | |||||
| 25. Would you recommend this hospital to your friends and family? | Definitely no | Probably no | Probably yes | Definitely yes | |
| Additional questions | |||||
| 26. During this hospital stay, staff took my preferences and my family’s [or caregiver’s] preferences into account in deciding what my health care needs would be when I left. | Strongly agree | Agree | Disagree | Strongly disagree | NA or DK |
| 27. When I left the hospital, I had a good understanding of the things I was responsible for in managing my health. | Strongly agree | Agree | Disagree | Strongly disagree | NA or DK |
| 28. When I left the hospital, I clearly understood the purpose for taking each of my medications. [STAFF: If they are confused or ask about prescriptions, this includes prescriptions given when discharged.] | Strongly agree | Agree | Disagree | Strongly disagree | NA or DK |
| 29. In general, how would you rate your overall health? | Excellent | Very good | Good | Fair poor | NA or DK |
| 30. In general, how would you rate your overall mental or emotional health? | Excellent | Very good | Good | Fair poor | NA or DK |
Appendix 4: Postdischarge Survey (Open-ended Questions)
| Open-ended Questions | |
|---|---|
| The next questions are about the music therapy you received during your stay. | |
| 1. How did your music therapy sessions affect your stay at the hospital? | |
| 2. How did your music therapy sessions affect your pain levels while in the hospital? | |
| 3. How did your music therapy sessions affect your stress or anxiety while in the hospital? | |
| 4. What other effects did you notice from your massage/music therapy sessions? | |
| 5. When did you notice these other effects? [Follow up: During music? After music? Morning? Evening?] | |
| 6. During your time in the hospital, how often did you listen to the music provided to you outside of the massage/music therapy sessions? For how long on average? | |
| 7. Did you use any of the recommendations the massage/music therapist gave you while you were in the hospital (breathing exercises, playlists, etc.)? [Follow up: Which ones?] | |
| 8. How did these music therapy practices affect you while in the hospital? | |
| 9. Have you used these music therapy practices since being discharged? How often? | |
| 10. Do you have any other comments on your recent stay in the hospital or being in the study in general? | |
| The next questions are about the massage therapy you received during your stay. | |
| 1. How did your massage therapy sessions affect your stay at the hospital? | |
| 2 How did your massage therapy sessions affect your pain levels while in the hospital? | |
| 3. How did your massage therapy sessions affect your stress or anxiety while in the hospital? | |
| 4. What other effects did you notice from your massage therapy sessions? | |
| 5. When did you notice these other effects? [Follow up: During massage? After massage? Mornings? Evenings?] | |
| 6. Did you use any of the recommendations the massage therapist gave you (stretching, deep breathing, etc.)? [Follow up: Which ones?] | |
| 7. How did these massage therapy practices affect you while in the hospital? | |
| 8. Have you used any of the massage therapy practices since being discharged? How often? | |
| 9. Do you have any other comments on your recent stay in the hospital or being in the study in general? | |
| 10. Do you have any other comments on your recent stay in the hospital or being in the study in general? | |
Author Contributions
Roseen, Cornelio-Flores, and Saper had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Saper and Hanser. Acquisition, analysis, or interpretation of data: Roseen, Cornelio-Flores, Lemaster, Hernandez, Fong, Resnick, Wardle, Hanser, and Saper. Drafting of the manuscript: Roseen, Cornelio-Flores, Hanser, and Saper. Critical revision of the manuscript for important intellectual content: Roseen, Cornelio-Flores, Lemaster, Hernandez, Fong, Resnick, Wardle, Hanser, and Saper. Statistical analysis: Roseen and Cornelio-Flores. Obtained funding: Saper and Hanser. Administrative, technical, or material support: Roseen, Cornelio-Flores, and Lemaster. Study supervision: Roseen, Saper, and Lemaster. ClinicalTrials.gov Identifier: NCT02227680
Author Note
This article has previously been presented in part at the following events: The International Congress for Integrative Medicine and Health, May 17, 2016, Henderson, NV; Integrative Medicine for the Underserved (IM4US), August 6 to 8, 2015, Boston, MA; and Inaugural Osher Integrative Medicine Research Forum 2014, Harvard Medical School and Brigham and Women’s Hospital, November 3, 2014, Boston, MA.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Saper is the Director of the Program for Integrative Medicine and Health Disparities at Boston Medical Center. Hanser is the founding chair of the Music Therapy Department at Berklee College of Music and has conducted previous trials of music therapy in hospital settings. None of the other authors have any conflicts of interest to declare of relevance to this work.
Disclaimer
As part of our agreement with the funding institutions, we committed to disseminating our findings in articles like this one. None of the sponsors had any involvement in our decision to submit this manuscript or in the determination of its contents.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr Roseen is supported by a Ruth L Kirschtein National Research Service Award (1F32AT009272) from the National Center for Complementary and Integrative Health (NCCIH). This work was supported by the Muscular Therapy Institute Foundation and Berklee College of Music.
References
- 1.Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3(1):1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tefera L, Lehrman W, Conway P. Measurement of the patient experience: clarifying facts, myths, and approaches. JAMA. 2016;315(20):2167–2168. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education.. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press, 2011. [PubMed] [Google Scholar]
- 4.Chatterjee P, Joynt KE, Orav EJ, et al. Patient experience in safety-net hospitals. Arch Intern Med. 2012;172(16):1204. [DOI] [PubMed] [Google Scholar]
- 5.Miller J, Dunion A, Dunn N, et al. Effect of a brief massage on pain, anxiety, and satisfaction with pain management in postoperative orthopedic patients. Orthop Nurs. 2015;34(4):227–234. [DOI] [PubMed] [Google Scholar]
- 6.Moyer CA, Rounds J, Hannum JW. A meta-analysis of massage therapy research. Psychol Bull. 2004;130(1):3–18. [DOI] [PubMed] [Google Scholar]
- 7.Mandel SE, Davis BA, Secic M. Effects of music therapy on patient satisfaction and health-related quality of life of hospital inpatients. Hosp Top. 2014;92(2):28–35. [DOI] [PubMed] [Google Scholar]
- 8.Yinger OS, Standley JM. The effects of medical music therapy on patient satisfaction: as measured by the Press Ganey Inpatient Survey. Music Ther Perspect. 2011;29(2):149–156. [Google Scholar]
- 9.Dileo C. Effects of music and music therapy on medical patients: a meta-analysis of the research and implications for the future. J Soc Integr Oncol. 2006;4(2):67–70. [DOI] [PubMed] [Google Scholar]
- 10.Lee JH. The effects of music on pain: a meta-analysis. J Music Ther. 2016;53(4):430–477. [DOI] [PubMed] [Google Scholar]
- 11.Rosen J, Lawrence R, Bouchard M, et al. Massage for perioperative pain and anxiety in placement of vascular access devices. Adv Mind Body Med. 2013;27(1):12–23. [PubMed] [Google Scholar]
- 12.Smith MC, Stallings MA, Mariner S, Burrall M. Benefits of massage therapy for hospitalized patients: a descriptive and qualitative evaluation. Altern Ther Health Med. 1999;5(4):64–71. [PubMed] [Google Scholar]
- 13.Wilkinson SM, Love SB, Westcombe AM, et al. Effectiveness of aromatherapy massage in the management of anxiety and depression in patients with cancer: a multicenter randomized controlled trial. J Clin Oncol. 2007;25(5):532–539. [DOI] [PubMed] [Google Scholar]
- 14.Bauer BA, Cutshall SM, Wentworth LJ, et al. Effect of massage therapy on pain, anxiety, and tension after cardiac surgery: a randomized study. Complement Ther Clin Pract. 2010;16(2):70–75. [DOI] [PubMed] [Google Scholar]
- 15.Huang S-T, Good M, Zauszniewski JA. The effectiveness of music in relieving pain in cancer patients: a randomized controlled trial. Int J Nurs Stud. 2010;47(11):1354–1362. [DOI] [PubMed] [Google Scholar]
- 16.Gallagher LM, Lagman R, Walsh D, Davis MP, LeGrand SB. The clinical effects of music therapy in palliative medicine. Support Care Cancer. 2006;14(8):859–866. [DOI] [PubMed] [Google Scholar]
- 17.Good M, Albert JM, Anderson GC, et al. Supplementing relaxation and music for pain after surgery. Nurs Res. 2010;59(4):259–269. [DOI] [PubMed] [Google Scholar]
- 18.Comeaux T, Steele-Moses S. The effect of complementary music therapy on the patient’s postoperative state anxiety, pain control, and environmental noise satisfaction. Medsurg Nurs. 2013;22(5):313–318. [PubMed] [Google Scholar]
- 19.Mandel SE, Hanser SB, Secic M, Davis BA. Effects of music therapy on health-related outcomes in cardiac rehabilitation: a randomized controlled trial. J Music Ther. 2007;44(3):176–197. [DOI] [PubMed] [Google Scholar]
- 20.Hanser SB, Bauer-Wu S, Kubicek L, et al. Effects of a music therapy intervention on quality of life and distress in women with metastatic breast cancer. J Soc Integr Oncol. 2006;4(3):116–124. [DOI] [PubMed] [Google Scholar]
- 21.Hanser SB, Mandel SE. Manage Your Stress and Pain Through Music. Boston: Berklee Press, 2010. [Google Scholar]
- 22.Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). Summary Analyses. http://www.hcahpsonline.org/SummaryAnalyses.aspx. Accessed July 5, 2016.
- 23.Miles MB, Huberman MA, Saldaña J. Qualitative Data Analysis: A Methods Sourcebook. Thousand Oaks, CA: Arizona State University, SAGE Publications Inc, 2014. [Google Scholar]
- 24.Atlas SJ, Grant RW, Ferris TG, Chang Y, Barry MJ. Patient-physician connectedness and quality of primary care. Ann Intern Med. 2009;150(5):325–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li L, Lee NJ, Glicksberg BS, Radbill BD, Dudley JT. Data-driven identification of risk factors of patient satisfaction at a large urban academic medical center. PLoS One. 2016;11(5):1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elliott MN, Lehrman WG, Goldstein E, Hambarsoomian K, Beckett MK, Giordano LA. Do hospitals rank differently on HCAHPS for different patient subgroups? Med Care Res Rev. 2010. 67(1):56–73. [DOI] [PubMed] [Google Scholar]
- 27.Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA. Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine. 2001;26(13):1418–1424. [DOI] [PubMed] [Google Scholar]