Abstract
Background
Invasive pulmonary aspergillosis (IPA) has high mortality rate but prognostic factors are not well established. The aim of our study was to evaluate the trend in in-hospital mortality over a period of 11 years and identify factors affecting the clinical outcomes of patients with IPA.
Method
We conducted a nationwide inpatient population study using data from the Taiwan National Health Insurance Research Database. A total of 407 IPA patients from 2002 to 2012 were included in the study. Differences in demographics, comorbidities, and treatment were evaluated between in-hospital death group and survival group. Multivariate analysis was also performed to identify risk factors for mortality.
Result
Male patients represented 63.14% of the patients (n = 257) and the mean age was 53.15 ± 20.93 years. Hematological cancer (n = 216, 53.07%) and diabetes mellitus (n = 75, 18.43%) were the most common underlying conditions. The overall case fatality rate was 30.22% with female slightly higher then male (32.67% versus 28.79%). The in-hospital case fatality rate increased since 2002 and peaked in 2006. It then declined over time with an in-hospital mortality of 25% in 2012. The in-hospital death group had a higher intubation rate (p<0.0001), a longer ICU stay (p = 0.0062), higher percentages of DM (p = 0.0412) and COPD (p = 0.0178), and a lower percentage of hematological cancer (p = 0.0079) as compared to survivor. The in-hospital death group was more likely to have steroid treatment (p<0.0001), develop acute renal failure (p<0.0001) and other infectious diseases (p = 0.0008) during hospitalization. Multivariate analysis identified female gender, older age (≥ 65 years old), intubation, bone marrow transplantation, acute renal failure, other infectious diseases and steroid use as predictive factors for mortality.
Conclusion
The present study shows the trend in mortality among patients with IPA over an 11-year period. Female gender, older age, intubation, bone marrow transplantation, acute renal failure, other infectious diseases and steroid use were identified as risk factors for mortality.
Introduction
Invasive aspergillosis (IA) is a common invasive mold infection that mostly affects immunocompromised patients. Most cases of IA have pulmonary involvement and often lead to severe pneumonia with respiratory failure requiring intubation and mechanical ventilation [1, 2]. The incidence of invasive pulmonary aspergillosis (IPA) has been increasing over the years [3], and patients with pre-existing conditions such as end-stage renal disease (ESRD), diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD), and long-term steroid use are more susceptible than previously suspected [4].
The high mortality rate associated with IA remains an important issue, with studies reporting a crude mortality ranging from 35.6% to as high as 70% in critically ill patients [1, 2, 5–10]. Though new diagnostic tools such as the galactomannan (GM) test, newer anti-mold medicines and increased disease awareness in non-hematological patients have been shown in studies to be effective in improving early diagnosis and clinical outcomes [11–13], it is unclear whether mortality has been consequently reduced over time. In the study done by Kim et al., crude mortality rates were significantly lower in 2005–2006 compared with 2000–2004 (31.2% versus 39.0%) [6]. Nevertheless, another population-based analysis illustrated no obvious change in mortality rates from 2001 to 2010 [14].
Identification of predictors for mortality, in addition to newer diagnostic methods and anti-mold treatment, may help recognize patients with higher mortality rate who could benefit from more aggressive therapies and lead to better clinical outcomes [5]. However, previous studies have been inconsistent in identifying prognostic factors. A single center study of IA by Hsiue et al. reported that steroid use correlated with poorer survival [15], while Iqbal et al. found no significant association between steroid exposure and morality in Pakistani patients with IPA [16]. The latter authors identified respiratory failure, DM, and longer length of hospital stay to be independent factors that predicted poor outcome. A large-scale international multicenter study conducted by Tacoone et al. investigated ICU patient with IA and found that older age, bone marrow transplant, higher sequential organ failure assessment (SOFA) score, mechanical ventilation use and requirement for renal replacement therapy were predictors of a poor outcome [1]. Another multicenter study by Porpon et al. evaluated the epidemiology of invasive mold infection in five Asian countries and concluded that disseminated diseases, rheumatologic condition and higher GM levels were predictors of mortality [8]. Since there is no overall consensus, it is necessary to have more evidence regarding prognostic factors to identify patients with IPA who are at a higher risk of mortality.
Therefore, the aim of this study is to describe the trend in mortality among Taiwanese patients with IPA over an 11-year period and to identify the associated prognostic factors based on data from the national health insurance database.
Materials and methods
Data sources
The data for this population-based case-control study were retrieved from the Taiwan National Health Insurance Research Database (NHIRD). The NHIRD is a comprehensive medical claims database that contains demographic information such as sex and date of birth as well as health care information such as the dates of visits and admissions, records of prescriptions, and up to five discharge diagnoses. The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes were used for disease diagnosis. The Ethics Review Board of the Ditmanson Medical Foundation Chia-Yi Christian Hospital in Taiwan approved this study. Because all patient identification numbers in NHIRD were scrambled before data release to protect confidentiality, no informed consent was necessary.
Study subjects
We identified all first-admitted patients with the diagnosis of IPA (ICD-9-CM codes 484.6) between 2002 and 2012 who were treated with either oral and/or intravenous antifungal therapy, which included voriconazole, posaconazole, micafungin, itraconazole, caspofungin, anidulafungin and amphotericin B during their hospitalization. Only patients who received at least 3 days of antifungal therapy were selected to ensure the accuracy of the IPA diagnosis. This definition of IPA was applied in our previous study [3]. We defined patients who died during the hospitalization (in-hospital death) as the case group, and patients who were discharged from the hospital (survival) as the control group.
Definition of characteristics, comorbidity, and drug use
The demographics, comorbidity, and drug use among patients were assessed in this study. Age was categorized into four groups: 0 to 18, 19 to 49, 50 to 64, and over 65 years old. The comorbidities included DM (ICD-9-CM code 250), ESRD (ICD-9-CM codes 585.5, 585.6 combined with ICD-9-CM procedure codes 39.95, 38.95), liver cirrhosis (ICD-9-CM code 571), COPD (ICD-9-CM codes 491, 492, 496 and age over 40 years), asthma (ICD-9-CM code 493), bronchiectasis (ICD-9-CM code 494), tuberculosis (ICD-9-CM codes 011, 012, 018), acquired immune deficiency syndrome (AIDS, ICD-9-CM code 042), autoimmune disease (ICD-9-CM codes 710.0–710.4, 714), solid organ cancer (ICD-9-CM codes 140–195), hematological cancer (ICD-9-CM codes 204–208), and transplantation classified into bone marrow (ICD-9-CM codes V428.1-V428.2) and organ transplantation (ICD-9-CM codes V420, V421, V426, V427, V428.3-V428.4). We also investigated the impact of acute renal failure (ICD-9-CM code 584.5–584.9), other infectious diseases excluding tuberculosis, AIDS, aspergillosis (ICD-9-CM codes 001–010, 013–016, 019.0–117.2, 117.4–139.8, 320–326, 480.0–484.5, 484.7–487.8), and medications such as voriconazole and steroids during the hospitalization.
Statistical analysis
A t-test and chi-square test were used to evaluate the differences in patient characteristics, comorbidity, and drug used between the in-hospital death group and the survival group. The in-hospital mortality rate was calculated and plotted by year and age group. To investigate the risk of in-hospital mortality in patients with IPA, we used a logistic regression model to calculate the odds ratios (ORs) and 95% confidence intervals (CIs). All statistical analyses were performed using SPSS software, Version 21 of the SPSS System for Windows (version 21.0; IBM Corporation, Somers, NY, USA). A two-tailed P-value < 0.05 was considered statistically significant.
Results
A total of 407 cases were identified from our database. Patient characteristics are shown in Table 1. The mean age was 53.15 ± 20.93 years, and male patients represented 63.14% of the patients (n = 257). A total of 147 (36.12%) patients were admitted to the intensive care unit (ICU), and 136 (33.42%) patients were intubated. The median overall duration of hospital stays was 35 days and was 11 days for ICU stays. Chest computed tomography was performed in the majority of the patients (n = 300, 73.71%). Bronchoscopy and the GM test were performed in 31.45% and 30.71% of the patients, respectively. The most common comorbid conditions are hematological cancer (n = 216, 53.07%) and diabetes mellitus (n = 75, 18.43%). COPD (n = 41, 10.07%) and asthma (n = 25, 6.14%) were the most common underlying lung diseases. In terms of medications, steroids were prescribed in 331(81.33%) patients and voriconazole was used in 282 (69.29%) patients as either mono-therapy or part of a combination therapy.
Table 1. Demographic characteristics, clinical features, and resource utilizations of patients with invasive aspergillosis pneumonia (N = 407).
| Variables -Number (%) | Total (N = 407) | Survival (N = 284) | In-hospital death (N = 123) | P value |
|---|---|---|---|---|
| Gender | ||||
| Female | 150 (36.86) | 101 (35.56) | 49 (39.84) | 0.4118 |
| Male | 257 (63.14) | 183 (64.44) | 74 (60.16) | |
| Age, years | ||||
| 0–18 | 34 (8.35) | 31 (10.92) | 3 (2.44) | <0.0001 |
| 19–49 | 121 (29.73) | 90 (31.69) | 31 (25.20) | |
| 50–64 | 117 (28.75) | 87 (30.63) | 30 (24.39) | |
| 65+ | 135 (33.17) | 76 (26.76) | 59 (47.97) | |
| mean±SD | 53.15±20.93 | 50.46±21.01 | 59.36±19.46 | <0.0001 |
| GM test | 125 (30.71) | 84 (29.58) | 41 (33.33) | 0.4507 |
| Bronchoscopy | 128 (31.45) | 75 (26.41) | 53 (43.09) | 0.0009 |
| Computered tomography | 300 (73.71) | 207 (72.89) | 93 (75.61) | 0.5667 |
| Use of intubation and MV | 136 (33.42) | 45 (15.85) | 91 (73.98) | <0.0001 |
| ICU admission | 147 (36.12) | 59 (20.77) | 88 (71.54) | <0.0001 |
| Length of stay, days- Median (IQR) | ||||
| Overall | 35 (21–54) | 35.0 (20.5–52.5) | 33.0 (21.0–56.0) | 0.4297 |
| In ICU admission | 11 (5–22) | 8.0 (2.0–18.0) | 14 (6.0–24.5) | 0.0062 |
| Medical cost, US dollars- Median (IQR) | 15045 (7127–27743) | 13120 (5983–25836) | 19729 (10919–34599) | <0.0001 |
| Comorbidity | ||||
| DM | 75 (18.43) | 45 (15.85) | 30 (24.39) | 0.0412 |
| ESRD | 14 (3.44) | 9 (3.17) | 5 (4.07) | 0.6488 |
| Liver cirrhosis | 25 (6.14) | 20 (7.04) | 5 (4.07) | 0.2507 |
| COPD | 41 (10.07) | 22 (7.75) | 19 (15.45) | 0.0178 |
| Asthma | 25 (6.14) | 18 (6.34) | 7 (5.69) | 0.8029 |
| Bronchiectasis | 19 (4.67) | 14 (4.93) | 5 (4.07) | 0.7042 |
| Tuberculosis | 40 (9.83) | 29 (10.21) | 11 (8.94) | 0.6931 |
| AIDS | 4 (0.98) | 2 (0.70) | 2 (1.63) | 0.5876 |
| Autoimmune disease | 27 (6.63) | 17 (5.99) | 10 (8.13) | 0.4248 |
| Cancer | ||||
| Solid organ cancer | 59 (14.50) | 39 (13.73) | 20 (16.26) | 0.5059 |
| Hematological cancer | 216 (53.07) | 163 (57.39) | 53 (43.09) | 0.0079 |
| Transplantation | ||||
| No | 386 (94.84) | 270 (95.07) | 116 (94.31) | 0.3809 |
| Bone marrow transplantation | 8 (1.97) | 4 (1.41) | 4 (3.25) | |
| Organ transplantation | 13 (3.19) | 10 (3.52) | 3 (2.44) | |
| During the hospitalization | ||||
| Other infectious diseases | 171 (42.01) | 104 (36.62) | 67 (54.47) | 0.0008 |
| Acute renal failure | 20 (4.91) | 6 (2.11) | 14 (11.38) | <0.0001 |
| Use of voriconazole | ||||
| No | 125 (30.71) | 83 (29.23) | 42 (34.15) | 0.3230 |
| Yes | 282 (69.29) | 201 (70.77) | 81 (65.85) | |
| Use of steriod | ||||
| No | 76 (18.67) | 69 (24.30) | 7 (5.69) | <0.0001 |
| Yes | 331 (81.33) | 215 (75.70) | 116 (94.31) |
SD: standard deviation. IQR: inter-quartile range. MV: mechanical ventilator
Of 407 patients the overall case fatality rate was 30.22% with female slightly higher then male (32.67% compared to 28.79%). Compared to patients who survived, patients who died during the hospitalization were older, more likely to be intubated, admitted to ICU, had a longer ICU stay, and underwent bronchoscope study. They also had a greater prevalence for underlying DM, COPD, and were more likely to have acute renal failure and other infectious diseases during hospitalization. Steroid was used more frequently in the in-hospital death group as compared to patient who survived.
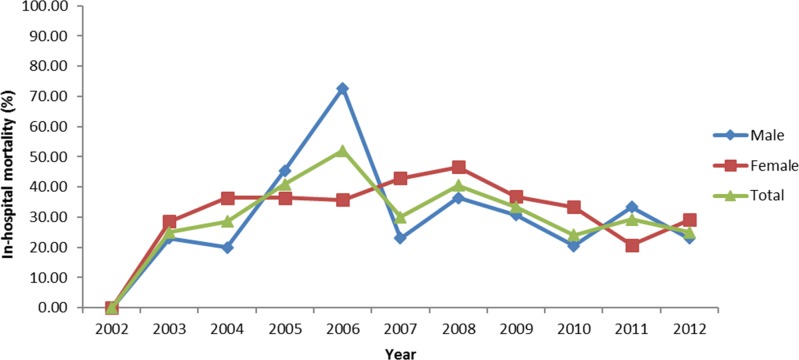
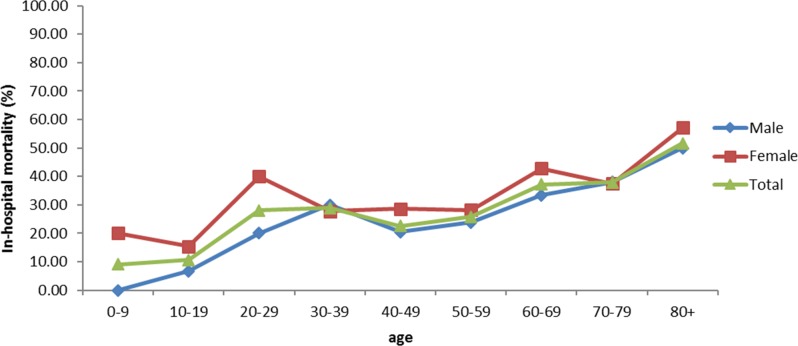
Fig 1 shows the trend in mortality over time. For both genders, the in-hospital case fatality rate increased since 2002, peaked in 2006 and 2008, then declined over time with an overall in-hospital mortality of 25% in 2012. Of note, there were more cases identified from 2007 to 2012 compared to the period from 2002 to 2006 (307 versus 100). Fig 2 shows the relationship between mortality and age. The proportion of deaths increased with age, regardless of sex. Furthermore, females had a higher mortality compared to males across almost all age groups. Table 2 shows the results of the logistic regression using both univariate and multivariate models. In the multivariate model, female gender, older age (≥ 65 years old), intubation, bone marrow transplantation, acute renal failure, other infectious diseases and steroid use were identified as predictive factors for mortality in patients with IPA.
Fig 1. Relationship of mortality in different sex over time.
Fig 2. Relationship of mortality with age in different sex.
Table 2. Odds ratio and 95%CI for in-hospital mortality in patients with invasive aspergillosis pneumonia.
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| Variables -Number (%) | OR | 95%CI | OR | 95%CI |
| Gender | ||||
| Female | Reference | — | Reference | — |
| Male | 0.87 | 0.56–1.36 | 0.49 | 0.25–0.96 |
| Age, years | ||||
| 0–18 | Reference | — | Reference | — |
| 19–49 | 3.56 | 1.02–12.47 | 1.50 | 0.33–6.84 |
| 50–64 | 3.48 | 0.99–12.26 | 1.74 | 0.39–7.81 |
| 65+ | 7.89 | 2.30–27.07 | 5.55 | 1.23–24.93 |
| GM test | 1.21 | 0.77–1.91 | 0.92 | 0.49–1.74 |
| Use of intubation and MV | 15.36 | 9.15–25.77 | 25.78 | 12.59–52.81 |
| Comorbidity | ||||
| DM | 1.74 | 1.04–2.94 | 2.01 | 0.93–4.37 |
| ESRD | 1.31 | 0.43–4.00 | 2.93 | 0.37–23.42 |
| Liver cirrhosis | 0.57 | 0.21–1.55 | 0.52 | 0.12–2.33 |
| COPD | 2.21 | 1.15–4.26 | 2.11 | 0.77–5.79 |
| Asthma | 0.90 | 0.37–2.22 | 0.33 | 0.09–1.17 |
| Bronchiectasis | 0.83 | 0.29–2.35 | 0.69 | 0.17–2.83 |
| Tuberculosis | 0.88 | 0.42–1.82 | 0.82 | 0.27–2.46 |
| AIDS | 2.36 | 0.33–16.96 | 4.73 | 0.24–91.98 |
| Autoimmune disease | 1.41 | 0.63–3.18 | 0.53 | 0.16–1.82 |
| Cancer | ||||
| Solid organ cancer | 1.17 | 0.64–2.11 | 1.73 | 0.73–4.08 |
| Hematological cancer | 0.58 | 0.38–0.89 | 1.89 | 0.89–4.00 |
| Transplantation | ||||
| No | Reference | Reference | ||
| Bone marrow transplantation | 2.36 | 0.58–9.60 | 16.09 | 3.16–82.04 |
| Organ transplantation | 0.71 | 0.19–2.62 | 0.38 | 0.04–3.52 |
| During the hospitalization | ||||
| Other infectious diseases | 2.03 | 1.32–3.12 | 2.54 | 1.38–4.68 |
| Acute renal failure | 6.04 | 2.26–16.13 | 6.65 | 1.4–31.55 |
| Use of voriconazole | ||||
| No | Reference | — | Reference | — |
| Yes | 0.78 | 0.50–1.23 | 0.97 | 0.50–1.90 |
| Use of steriod | ||||
| No | Reference | — | Reference | — |
| Yes | 5.15 | 2.29–11.58 | 3.25 | 1.18–8.97 |
Discussion
The present study illustrates the trend in in-hospital mortality among patients with IPA over a period of 11 years. Several risk factors for in-hospital mortality were also identified, including female gender, old age, mechanical ventilation, bone marrow transplantation, acute renal failure, other infectious diseases, and use of steroid.
Population-based epidemiological reports evaluating IA are not common, and risk factors for mortality have been poorly identified. Many of the research have been carried out at single institutions with limited case numbers and in some cases, studies targeted only patients with hematological disorders [17, 18]. Therefore, it is difficult to generalize the results of these studies, and a clear understanding of the epidemiology of aspergillosis is lacking.
This nationwide study in Taiwan identified several factors relevant to patient outcomes, which can be used as a guide for clinical judgment and future studies. Age is a significant factor for predicting mortality. Fig 2 shows that the in-hospital mortality rate increases with age. In the multivariate regression model, the odds ratio for mortality was as high as 5.55 for patients aged 65 years and over compared to patients less than 19 years old. This result is consistent with a previous international multicenter epidemiological study by Taccone et al [1], though other studies did not identify age as a risk factor for mortality. One possible explanation for this discrepancy is that these studies included patients from single healthcare institutions who were less representative than the patients in our nationwide study and multicenter research. In our study, female patients were more likely to die from IPA; this finding has never been observed in previous studies. The reason for this novel finding is unknown, and additional studies are required to further substantiate and explain this observation.
Underlying comorbidities may affect the outcome of patients with IA. Previous studies have demonstrated that bone marrow transplantation, diabetes and neutropenia are associated with an increased risk of mortality [1, 16, 19]. In the present study, bone marrow transplantation was the only comorbidity found to be predictive of mortality. This inconsistency may be a result of different study designs, disease definition, and the quality of patient care. Additional large-scale reports are necessary to better demonstrate this correlation.
Mechanical ventilation, acute renal failure and other infectious diseases were also identified as predictive factors for mortality. In line with previous reports [15, 19, 20], use of a mechanical ventilator was the single most important risk factor for mortality in our study population. Feasible comparisons could not be made with other similar studies that did not include mechanical ventilation or respiratory failure in their analyses. The correlation between mechanical ventilation and mortality is not surprising since the need for a ventilator signifies severe lung involvement, indicating a poor prognosis. Similarly, acute renal failure and other infectious diseases during hospital stay are complications that may occur in patients with severe fungal infection. The associations between these two conditions and increased risk of death have been illustrated in studies investigating invasive aspergillosis [14, 21, 22].
The case fatality rate was 30.22%, which was similar to the results of two large-scale registry studies [23, 24]. Over the years, the trend in in-hospital mortality fluctuated and decreased in the latter period of the study. The introduction of new diagnostic tools and anti-fungal agents may have contributed to this reduction in mortality. However, even though the mortality gradually decreased, it remained high. The results suggest that, in addition to the available diagnostics and medications, further research and better patient care models are needed to improve the outcome of patients with IPA. As a nationwide study that included a large set of patients with IPA over a period of 11 years, the results are likely to be representative of the Taiwanese population.
However, there are some limitations. First, because the data were retrieved from a national health insurance registration system, information on clinical symptoms and culture results are not available. This did not allow us to include and classify patients on the basis of the definition proposed by the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group Consensus Group [25]. We acknowledged this weakness and attempted to overcome it. Following Kim et al., we used strict inclusion criteria, i.e. hospitalized patients receiving at least 3 days of anti-mold medications, which we believe covers the patients most likely to have IPA. Second, the lack of clinical data also made it difficult to account for disease severity by using standardized scales such as SOFA score, which may also influence the results of risk factor analysis for mortality. Third, we did not evaluate causes of death, and we could not exclude the possibility that some mortality may have been due to the concomitant disease, such as co-infections.
In conclusion, we identified several factors that were associated with death among patients with IPA. Risk factors for mortality included old age, female gender, mechanical ventilation, bone marrow transplantation and steroid use. The development of acute renal failure and other infectious diseases during hospitalization were also indicators for in-hospital death. The trend in mortality over the study period was also illustrated. Further research on better patient management is needed to reduce mortality and the clinical burden of IPA.
Data Availability
All relevant data are within the paper.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Taccone FS, Van den Abeele AM, Bulpa P, Misset B, Meersseman W, Cardoso T, et al. Epidemiology of invasive aspergillosis in critically ill patients: clinical presentation, underlying conditions, and outcomes. Critical care (London, England). 2015;19:7 Epub 2015/05/01. doi: 10.1186/s13054-014-0722-7 ; PubMed Central PMCID: PMCPMC4344741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Montagna MT, Lovero G, Coretti C, Martinelli D, Delia M, De Giglio O, et al. SIMIFF study: Italian fungal registry of mold infections in hematological and non-hematological patients. Infection. 2014;42(1):141–51. Epub 2013/10/24. doi: 10.1007/s15010-013-0539-3 ; PubMed Central PMCID: PMCPMC3906525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sun KS, Tsai CF, Chen SC, Chen YY, Huang WC. Correction: Galactomannan Testing and the Incidence of Invasive Pulmonary Aspergillosis: A 10-Year Nationwide Population-Based Study in Taiwan. PloS one. 2016;11(6):e0156566 Epub 2016/06/02. doi: 10.1371/journal.pone.0156566 ; PubMed Central PMCID: PMCPMC4889043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bassetti M, Righi E, De Pascale G, De Gaudio R, Giarratano A, Mazzei T, et al. How to manage aspergillosis in non-neutropenic intensive care unit patients. Critical care (London, England). 2014;18(4):458 Epub 2014/08/30. doi: 10.1186/s13054-014-0458-4 ; PubMed Central PMCID: PMCPMC4220091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nivoix Y, Velten M, Letscher-Bru V, Moghaddam A, Natarajan-Amé S, Fohrer C. Factors associated with overall and attributable mortality in invasive aspergillosis. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2008;47 doi: 10.1086/592255 [DOI] [PubMed] [Google Scholar]
- 6.Kim A, Nicolau DP, Kuti JL. Hospital costs and outcomes among intravenous antifungal therapies for patients with invasive aspergillosis in the United States. Mycoses. 2011;54(5):e301–12. Epub 2010/06/19. doi: 10.1111/j.1439-0507.2010.01903.x . [DOI] [PubMed] [Google Scholar]
- 7.Baddley JW, Stephens JM, Ji X, Gao X, Schlamm HT, Tarallo M. Aspergillosis in Intensive Care Unit (ICU) patients: epidemiology and economic outcomes. BMC infectious diseases. 2013;13:29 Epub 2013/01/25. doi: 10.1186/1471-2334-13-29 ; PubMed Central PMCID: PMCPMC3562254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Porpon R, Chen YC, Chakrabarti A, Li RY, Shivaprakash RM, Yu J, et al. Epidemiology and clinical characteristics of invasive mould infections: A multicenter, retrospective analysis in five Asian countries. Medical mycology. 2017. Epub 2017/05/20. doi: 10.1093/mmy/myx029 .28525619 [Google Scholar]
- 9.Alvarez Lerma F, Olaechea Astigarraga P, Palomar Martinez M, Rodriguez Carvajal M, Machado Casas JF, Jimenez Quintana MM, et al. [Respiratory infections caused by Aspergillus spp. in critically ill patients admitted to the intensive care units]. Medicina intensiva. 2015;39(3):149–59. Epub 2014/04/10. doi: 10.1016/j.medin.2014.02.004 . [DOI] [PubMed] [Google Scholar]
- 10.Steinbach WJ, Marr KA, Anaissie EJ, Azie N, Quan SP, Meier-Kriesche HU, et al. Clinical epidemiology of 960 patients with invasive aspergillosis from the PATH Alliance registry. The Journal of infection. 2012;65(5):453–64. Epub 2012/08/18. doi: 10.1016/j.jinf.2012.08.003 . [DOI] [PubMed] [Google Scholar]
- 11.Ullmann AJ, Lipton JH, Vesole DH, Chandrasekar P, Langston A, Tarantolo SR, et al. Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. The New England journal of medicine. 2007;356(4):335–47. Epub 2007/01/26. doi: 10.1056/NEJMoa061098 . [DOI] [PubMed] [Google Scholar]
- 12.Maertens J, Theunissen K, Verhoef G, Verschakelen J, Lagrou K, Verbeken E, et al. Galactomannan and computed tomography-based preemptive antifungal therapy in neutropenic patients at high risk for invasive fungal infection: a prospective feasibility study. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2005;41(9):1242–50. Epub 2005/10/06. doi: 10.1086/496927 . [DOI] [PubMed] [Google Scholar]
- 13.Tan BH, Low JG, Chlebicka NL, Kurup A, Cheah FK, Lin RT, et al. Galactomannan-guided preemptive vs. empirical antifungals in the persistently febrile neutropenic patient: a prospective randomized study. International journal of infectious diseases: IJID: official publication of the International Society for Infectious Diseases. 2011;15(5):e350–6. Epub 2011/03/15. doi: 10.1016/j.ijid.2011.01.011 . [DOI] [PubMed] [Google Scholar]
- 14.Bitar D, Lortholary O, Le Strat Y, Nicolau J, Coignard B, Tattevin P, et al. Population-based analysis of invasive fungal infections, France, 2001–2010. Emerging infectious diseases. 2014;20(7):1149–55. Epub 2014/06/25. doi: 10.3201/eid2007.140087 ; PubMed Central PMCID: PMCPMC4073874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsiue HC, Wu TH, Chang TC, Hsiue YC, Huang YT, Lee PI, et al. Culture-positive invasive aspergillosis in a medical center in Taiwan, 2000–2009. European journal of clinical microbiology & infectious diseases: official publication of the European Society of Clinical Microbiology. 2012;31(7):1319–26. Epub 2011/10/15. doi: 10.1007/s10096-011-1445-1 . [DOI] [PubMed] [Google Scholar]
- 16.Iqbal N, Irfan M, Zubairi AB, Jabeen K, Awan S, Khan JA. Clinical manifestations and outcomes of pulmonary aspergillosis: experience from Pakistan. BMJ open respiratory research. 2016;3(1):e000155 Epub 2017/01/12. doi: 10.1136/bmjresp-2016-000155 ; PubMed Central PMCID: PMCPMC5174800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miceli MH, Grazziutti ML, Woods G, Zhao W, Kocoglu MH, Barlogie B, et al. Strong correlation between serum aspergillus galactomannan index and outcome of aspergillosis in patients with hematological cancer: clinical and research implications. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2008;46(9):1412–22. doi: 10.1086/528714 . [DOI] [PubMed] [Google Scholar]
- 18.Han SB, Kim Sk, Lee JW, Yoon J-S, Chung N-G, Cho B, et al. Serum galactomannan index for early prediction of mortality in immunocompromised children with invasive pulmonary aspergillosis. BMC infectious diseases. 2015;15(1):271 doi: 10.1186/s12879-015-1014-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gallien S, Fournier S, Porcher R, Bottero J, Ribaud P, Sulahian A, et al. Therapeutic outcome and prognostic factors of invasive aspergillosis in an infectious disease department: a review of 34 cases. Infection. 2008;36(6):533–8. Epub 2008/11/18. doi: 10.1007/s15010-008-7375-x . [DOI] [PubMed] [Google Scholar]
- 20.Thammahong A, Thayidathara P, Suksawat K, Chindamporn A. Invasive Aspergillus Infections in a Thai Tertiary-Care Hospital during 2006–2011. Advances in Microbiology. 2015;5:298–306. [Google Scholar]
- 21.Burghi G, Lemiale V, Seguin A, Lambert J, Lacroix C, Canet E, et al. Outcomes of mechanically ventilated hematology patients with invasive pulmonary aspergillosis. Intensive Care Med. 2011;37(10):1605–12. doi: 10.1007/s00134-011-2344-8 . [DOI] [PubMed] [Google Scholar]
- 22.Vandewoude KH, Blot SI, Benoit D, Colardyn F, Vogelaers D. Invasive aspergillosis in critically ill patients: attributable mortality and excesses in length of ICU stay and ventilator dependence. Journal of Hospital Infection. 56(4):269–76. doi: 10.1016/j.jhin.2004.01.006 [DOI] [PubMed] [Google Scholar]
- 23.Husain S, Silveira FP, Azie N, Franks B, Horn D. Epidemiological features of invasive mold infections among solid organ transplant recipients: PATH Alliance(R) registry analysis. Medical mycology. 2017;55(3):269–77. Epub 2016/10/06. doi: 10.1093/mmy/myw086 . [DOI] [PubMed] [Google Scholar]
- 24.Perkhofer S, Lass-Florl C, Hell M, Russ G, Krause R, Honigl M, et al. The Nationwide Austrian Aspergillus Registry: a prospective data collection on epidemiology, therapy and outcome of invasive mould infections in immunocompromised and/or immunosuppressed patients. International journal of antimicrobial agents. 2010;36(6):531–6. Epub 2010/10/16. doi: 10.1016/j.ijantimicag.2010.08.010 . [DOI] [PubMed] [Google Scholar]
- 25.De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2008;46(12):1813–21. doi: 10.1086/588660 ; PubMed Central PMCID: PMCPMC2671227. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.