Abstract
Objective
Having experienced 2–3 births is associated with reduced mortality versus women with <2 or ≥4 births. The effect of 2–3 births on lifespan may be associated with delayed cellular aging. We hypothesized telomere length, a marker of cellular aging, would be longer in women who had 2–3 pregnancies.
Methods
Leukocyte telomere length was measured using quantitative real-time polymerase chain reaction in 620 women in CARDIA at the year 15 and 20 exams, expressed as the ratio of telomere repeat copy number to single-copy gene copy number (T/S). Number of pregnancies at the time of telomere length measurement was obtained (mean age = 41±0.1 years, average gravidity = 2.64±0.1 pregnancies). Participants were divided into 4 groups by number of pregnancies: 0, 1, 2–3, and ≥4, to test for differences in telomere length by gravidity group.
Results
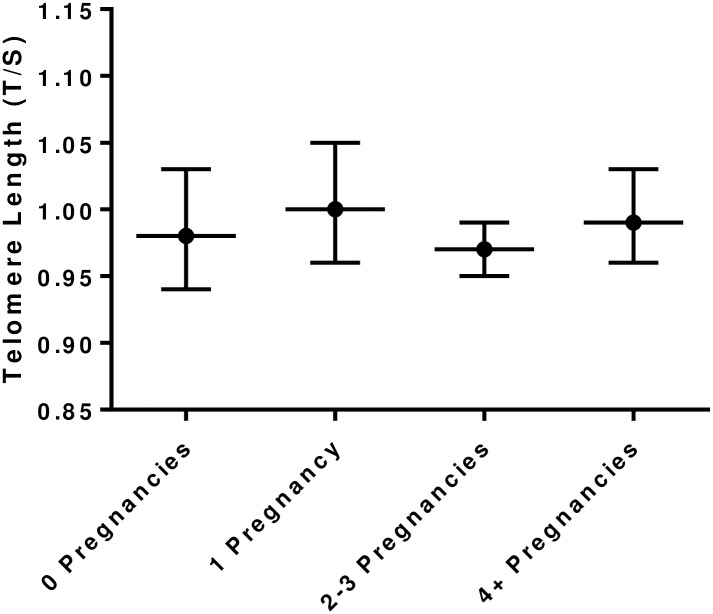
The mean and SD for telomere length was 0.98 ± 0.20 T/S in the whole cohort. There were no differences in mean telomere length between groups; 0.98±0.02 T/S in women with 0 pregnancies, 1.01±0.02 T/S in women with 1 pregnancy, 0.97±0.01 T/S in women with 2–3 pregnancies, and 0.99±0.02 T/S in women with ≥4 pregnancies (p = 0.51). We defined high-risk (shorter) telomere length as ≤25th percentile, and low-risk (longer) telomere length as ≥75 percentile. There were no differences in the prevalence of high-risk or low-risk telomere length between gravidity groups.
Conclusions
Gravidity was not associated with telomere length in early middle age; the protective association of 2–3 births may act through other mechanisms.
Introduction
Pregnancy has lasting effects on vascular function, such as reducing arterial stiffness and mean arterial pressure [1]. Parity, the number of times a woman has experienced a pregnancy lasting >20 weeks, is also related to cardiovascular disease mortality in a U-shaped pattern. Women who have had 2 or 3 births have the lowest cardiovascular mortality rate compared with women with less than 2 or more than 4 births [2]. Furthermore, women who have had 2–3 births have less evidence of subclinical atherosclerosis (reduced carotid intima-media thickness; cIMT, coronary artery calcium; CAC, and increased carotid distensibility) compared with women who have had less than 2 or 4 or more births years later [3–5]. Taken together, these data suggest that experiencing 2–3 pregnancies may reduce cardiovascular risk during aging in women.
Telomeres are comprised of nucleoproteins that form a cap at the end of chromosomes, and shorter telomere length indicates increased cell division [6]. Telomere length can be quantified as a measure of biological cellular aging, and shorter telomere length has been associated with mortality in women [7, 8]. Shorter telomere length has also been linked to increased subclinical atherosclerotic burden (CAC and arterial stiffness) [9, 10], but telomere length attrition is associated with vascular aging independent of traditional cardiovascular risk factors [11]. This is important because both traditional cardiovascular risk factors and subclinical atherosclerosis are thought to damage the cardiovascular system and lead to overt disease. The protective effect of 2–3 pregnancies on overall and cardiovascular mortality may be due to reduced cellular aging, evident by longer telomere length, in women who have had 2–3 pregnancies.
The purpose of this study was to determine whether there is an association between number of pregnancies (gravidity) and mid-life telomere length in women. We hypothesized that women who have had 2–3 pregnancies would have longer telomeres compared with women who have had less than 2 or ≥ 4 pregnancies. We further hypothesized that the strength of the relationship between number of pregnancies and telomere length would be reduced after adjustment for other cardiovascular risk factors as telomere length has been associated with CVD [9, 10]. Short telomere length (≤25th percentile) has been associated with multiple biological and behavioral risk factors for atherosclerotic cardiovascular disease [12–14]; we also hypothesized that women who have had 2–3 pregnancies would be less likely to have short telomere lengths, defined as ≤ 25th percentile, compared to women with <2 or ≥4 pregnancies. Telomere length and telomerase activity can be acutely altered during pregnancy in certain pregnancy-related conditions [15, 16], so we also tested for differences in telomere length in women with and without gestational diabetes and preterm birth.
Methods
The CARDIA Study is a longitudinal, observational, population-based, multi-center, study investigating determinants of coronary heart disease risk factors in African-American and Caucasian men and women. In 1985–1986, 5115 subjects (53% women, 52% African-American) aged 18 to 30 years were recruited from 4 urban areas in the United States: Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota; and Oakland, California. Retention rates at follow-up exams 15 and 20 years later (2000–2001 and 2005–2006) were 74%, and 72% of the surviving cohort, respectively. Institutional review boards at each study center approved the study and written, informed consent was obtained from participants.
Sample selection
Telomere length was measured in 620 women from an ancillary study in which participants were selected if they had stored DNA from whole blood available at Y15, Y20 and Y25 and also had coronary artery calcification data on the same examinations. Participants in the ancillary study from which we drew our sample were selected so that there would be a similar number of participants by race, education, sex, and study center. For those 1000 participants (620 women), telomere length was determined. In this study, we split the women in the telomere cohort into 2 groups according to age at baseline so that we could construct a sample with the same mean age because age is a main determinant of telomere length. We included the telomere length measurement at Y15 in the women who were older at baseline (24–30 yrs) and telomere length measurement at Y20 in the women who were younger at baseline (18–23 yrs) so that each woman was between 38 and 45 yrs old at the time of the measurement. Women included in the sample were younger, had higher triglycerides, more likely to be on cholesterol-lowering medication, and had a lesser percentage of preterm birth compared to women not in the sample, Table 1.
Table 1. Participant characteristics compared women not in sample.
| Telomere Sample N = 620 |
Women Not in Sample N = 1326 |
|
|---|---|---|
| Age (yrs)* | 41.5 ± 0.1 | 42.1 ± 0.1 |
| African-American (n, %) | 290, 47 | 330, 25 |
| Education (yrs) | 15 ± 0.1 | 15 ± 0.1 |
| Smoking (pack-yrs) | 0.60 ± 0.06 | 0.56 ± 0.04 |
| Alcohol (ml/day) | 6.8 ± 0.5 | 7.5 ± 0.6 |
| BMI (kg/m2) | 29.2 ± 0.3 | 29.5 ± 0.3 |
| Hypertension Meds (n, %) | 69, 11 | 163, 12 |
| SBP (mmHg) | 111 ± 1 | 112 ± 1 |
| DBP (mmHg) | 72 ± 1 | 72 ± 1 |
| Cholesterol Meds (n, %)* | 23, 4 | 27, 2 |
| Cholesterol (mg/dL) | 183 ± 1 | 182 ± 1 |
| LDL-C (mg/dL) | 108 ± 1 | 107 ± 1 |
| HDL-C (mg/dL) | 55 ± 1 | 57 ± 1 |
| Triglycerides (mg/dL)* | 94 ± 2 | 91 ± 2 |
| Diabetes (n, %) | 21, 3 | 67, 5 |
| GDM (n, %) | 33, 5 | 69, 5 |
| PTB (n, %)* | 77, 12 | 219, 17 |
Sample characteristics compared to women not the telomere sample. Education: years of formal schooling, Smoking: pack-yrs, a cumulative smoking score; 1 pack-yr = 7000 cigarettes, Hypertension Meds: percentage of women taking medication for high blood pressure, SBP: systolic blood pressure, DBP: diastolic blood pressure, Cholesterol Meds: percentage of women taking medication for high cholesterol, LDL-C: low-density lipoprotein cholesterol, HDL-C: high-density lipoprotein cholesterol, Diabetes diagnosis of diabetes mellitus, GDM: diagnosed gestational diabetes, PTB: preterm birth, any birth occurring before 37 weeks gestation.
*indicates a difference between groups. Data are mean ± SE unless otherwise indicated.
Gravidity
Women reported the number of pregnancies and the length of gestation at each exam. Participants also reported current pregnancy status and the number of pregnancies at each exam. Total number of pregnancies (gravidity) at year 15 or 20 (the year at which telomere length was measured) was used for analysis.
Blood draw and DNA extraction
Blood samples were obtained with venipuncture at exams in year 15 (for CARDIA participants aged 24–30 yrs at baseline) and year 20 (for CARDIA participants aged 18–23 at baseline) following an overnight fast (>8 h) with EDTA-containing tubes. Participants were asked not to perform heavy exercise or smoke in the two hours preceding the visit. Whole blood was stored at -70°C and shipped on dry ice to Dr. Fornage’s Genetics lab at University of Texas Health Science Center (Houston, TX) for DNA preparation. Peripheral blood mononuclear cells (PBMCs) were obtained from whole samples using Ficoll-Paque PLUS (Amersham) according to manufacturer's instructions, cryopreserved, and stored in liquid nitrogen until assays were performed. DNA was prepared using Gentra Puregene Cell kit (QIAGEN, Valencia, CA, USA) according to manufacturer’s instructions.
Telomere length
The CARDIA study shipped DNA samples in 96-well plates to the lab of Dr. Blackburn at University of California-San Francisco, where these plates were stored at -80°C. Five ul of the DNA was diluted with 10 ul of sterile water so that the concentration was 33.3 ng/ul. Diluted samples were stored at -80°C in 96-well plates until assayed. Then, they were transferred to 384-well plates after being thawed on ice. The telomere length measurement assay was adapted from the original method, detailed elsewhere [17]. Telomere length was measured using DNA with a quantitative polymerase chain reaction (qPCR) assay. The assay determines the ratio of telomere repeat copy number to single-copy gene copy number (T/S). T/S was measured in our samples and compared to a reference sample of DNA. A higher T/S ratio indicates longer telomere length. T/S were converted to base pairs using the equation: 3274+2413x T/S [17]. The coefficient of variation for the assay was 3.5%.
Co-variable measurements
Body mass index was calculated by dividing the weight in kilograms by height in meters squared. Blood pressure was measured in the right arm with a sphygmomanometer following a standardized rest period. Education, smoking, diagnosis of diabetes, gestational diabetes, use of hypertension and cholesterol-lowering medications were determined by self-report. Preterm birth (PTB) was defined as any birth occurring at <37 weeks of gestational age, according to self-report. Alcohol consumption (ml/day) was quantified as the number of drinks per week multiplied by ethanol concentration and included because alcohol has been shown to affect telomere length. Total cholesterol, LDL (calculated with the Friedewald equation), HDL cholesterol and triglycerides were measured in plasma following a fast. For a more detailed description of data collection, please visit the CARDIA website: http://www.cardia.dopm.uab.edu/
Statistical analyses
Participants were divided into 4 groups by number of pregnancies: 0, 1, 2–3, and ≥ 4 pregnancies. Group differences in participant characteristics were assessed with ANOVA, chi-square, and Mann-Whitney U tests for skewed data, as appropriate. We tested for differences in log-transformed mean telomere length between groups using ANOVA. We used multiple linear regression to test for associations between gravidity and telomere length (adjusted for age and race). Because the groups had different years of education and proportions of women with gestational diabetes and preterm births and all these factors have been associated with telomere length in earlier investigations [15, 16, 18], we performed an ANCOVA to determine whether years of education, preterm birth, or gestational diabetes affected the association of telomere length and gravidity group. A chi-square test was performed to determine whether there was a difference in prevalence of high-risk, short telomere length, defined as the lowest quartile of telomere length (≤ 0.844) between groups. We also evaluated whether there was a difference in prevalence of low-risk, long telomere length, defined as the highest quartile, ≥ 1.098, between groups. We determined whether there was a difference in likelihood of having a high-risk or low-risk telomere length by gravidity group using logistic regression. We repeated all analyses stratified by race, as race has been shown to influence telomere length in women [18]. We also tested whether women with gestational diabetes or preterm birth had shorter telomeres than women without these complications in our sample because telomerase activity has been shown to be acutely affected by complications of pregnancy [15]. Next, we conducted two sensitivity analyses. First, we tested for the effect of parity (versus gravidity) by conducting an analysis in the same women after reclassifying them into the same four categories after subtracting any pregnancies lasting < 20 weeks from their total number of pregnancies. Second, we repeated our analyses after omitting participants with telomere length that was greater than 3SD from the mean. Data are presented as means and standard errors. A p-value less than 0.05 was considered significant. Analyses were conducted using STATA version 14.0 (STATA Corporation, College Station, TX).
Results
When we compared women by gravidity group, we observed similar rates of hypertension and diabetes. Blood pressure, blood chemistries, and smoking histories were also similar among groups. The women in the higher gravidity groups tended to have completed fewer years of education, had a greater percentage of percent of African-American women, and greater percentage of women with gestational diabetes, Table 2.
Table 2. Participant characteristics at time of telomere length measurement by gravidity group.
| 0 Pregnancy | 1 Pregnancy | 2–3 Pregnancies | ≥4 Pregnancies | |
|---|---|---|---|---|
| N | 101 | 83 | 264 | 172 |
| Age (yrs) | 41 ± 0.3 | 42 ± 0.3 | 41 ± 0.2 | 42 ± 0.2 |
| African-American (n, %)† | 33, 33 | 36, 40 | 119, 45 | 102, 59 |
| Education (yrs)† | 16 ± 0.2 | 15 ± 0.2 | 15 ± 0.1 | 14 ± 0.2 |
| Smoking (pack-yrs) | 0.37 ± 0.1 | 0.69 ± 0.2 | 0.57 ± 0.1 | 0.74 ± 0.1 |
| Alcohol (ml/day) | 7.5 ± 1.4 | 6.8 ± 1.2 | 6.8 ± 0.7 | 6.7 ± 1.0 |
| BMI (kg/m2) | 29.1 ± 0.7 | 28.7 ± 0.6 | 29.3 ± 0.4 | 29.6 ± 0.6 |
| Hypertension Meds (n, %) | 7, 7 | 10, 12 | 30, 11 | 21, 12 |
| SBP (mmHg) | 110 ± 1 | 113 ± 2 | 110 ± 1 | 112 ± 1 |
| DBP (mmHg) | 71 ± 2 | 73 ± 2 | 71 ± 1 | 72 ± 1 |
| Cholesterol Meds (n, %) | 5, 5 | 2, 2 | 9, 3 | 7, 4 |
| Cholesterol (mg/dL) | 185 ± 3 | 190 ± 4 | 182 ± 2 | 181 ± 2 |
| LDL-C (mg/dL) | 110 ± 3 | 113 ± 3 | 107 ± 2 | 108 ± 2 |
| HDL-C (mg/dL) | 56 ± 1 | 57 ± 2 | 55 ± 1 | 55 ± 1 |
| Triglycerides | 92 ± 4 | 98 ± 6 | 93 ± 4 | 95 ± 6 |
| Diabetes (n, %) | 3, 3 | 0, 0 | 12, 5 | 6, 3 |
| GDM (n, %)† | 0, 0 | 2, 2 | 8, 3 | 6, 3 |
| PTB (n, %)† | 0, 0 | 4, 5 | 34, 13 | 39, 23 |
| Telomere length ≤25% (n,%) | 29, 29 | 19, 23 | 73, 28 | 35, 20 |
| Telomere length ≥75% (n,%) | 20, 20 | 25, 30 | 63, 24 | 47, 27 |
Subject characteristics by gravidity group. Education: years of formal schooling, Smoking: pack-yrs, cumulative smoking score, 1 pack-yr = 7000 cigarettes, Hypertension Meds: percentage of women taking medication for high blood pressure, SBP: systolic blood pressure, DBP: diastolic blood pressure, Cholesterol Meds: percentage of women taking medication for high cholesterol, LDL-C: low-density lipoprotein cholesterol, HDL-C: high-density lipoprotein cholesterol, Diabetes diagnosis of diabetes mellitus, GDM: diagnosed gestational diabetes, PTB: preterm birth, any birth occurring before 37 weeks gestation, Telomere length ≤ 25%: high-risk, shortened telomere length ≤ 25th percentile for the cohort, Telomere length ≥ 75%: low-risk, longer telomere length ≥ 75th percentile for the cohort.
†Indicates a difference between groups. Data are mean ± SE unless otherwise indicated.
The overall mean and SD for telomere length was 0.98 ± 0.20 T/S. There was no difference in unadjusted mean telomere length between the four gravidity groups, p = 0.51, Fig 1.
Fig 1. Telomere length (mean and 95% CI) by gravidity group.
There were no differences in unadjusted telomere length between gravidity groups.
Telomere length was the same in the women who had had 2 or 3 pregnancies versus all the other women, mean telomere length = 0.97 ± 0.01 T/S in women with 2 or 3 pregnancies and mean telomere length = 0.99 ± 0.01 T/S in all other women, p = 0.34. There was no difference in telomere length between women who were nulliparous versus those who had had at least one pregnancy: mean telomere length = 0.98 ± 0.01 T/S in nulliparous women and mean telomere length = 0.98 ± 0.02 T/S in women who had had a pregnancy, p = 0.42.
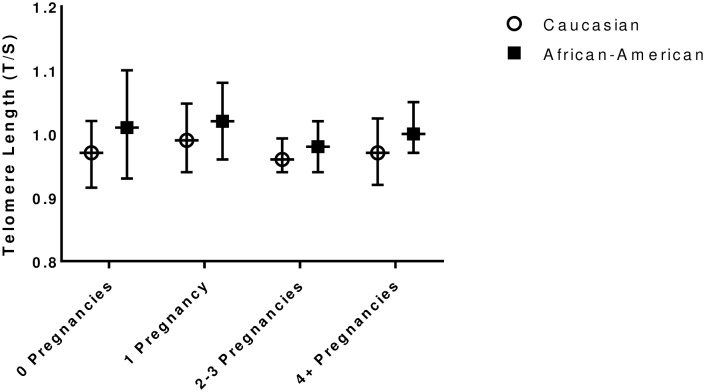
Mean telomere length did not differ by gravidity group in either African-American or Caucasian women, Fig 2, p = 0.55 for the difference between gravidity groups in African-American women, and p = 0.85 for the difference in telomere length between gravidity groups in Caucasian women. However, the effect of race on mean telomere length approached significance, 0.97 ± 0.01 in Caucasian and 1.00 ± 0.01 T/S in African-American women, p = 0.07.
Fig 2. Telomere length (mean and 95% CI) by gravidity group in Caucasian and African-American women.
There were no differences in unadjusted telomere length between gravidity groups in either race.
Furthermore, there was no association between gravidity group (β = 0.002 ± 0.01, p = 0.72), years of education (β = 0.0009 ± 0.003, p = 0.80), preterm birth (β = 0.01 ± 0.03, p = 0.63), or gestational diabetes status (β = -0.020 ± 0.04, p = 0.58), with telomere length.
One hundred fifty-six women had high-risk telomere length, defined as telomere length ≤ 0.8445 T/S, the cut-off for the 25th percentile. There was no difference in prevalence of high-risk telomere length between gravidity groups, p = 0.27, Table 2. One-hundred fifty-five women had a low-risk telomere length ≥ 1.099 T/S, the cut-off for the 75th percentile for the cohort, with no difference in prevalence of low-risk telomere length among gravidity groups, p = 0.35, Table 2.
In our first sensitivity analysis, there was no association of gravidity group with the likelihood of having high-risk (β = -0.099 ± 0.07, p = 0.14) or low-risk (β = 0.046 ± 0.07, p = 0.49) telomere length. Having had 0, 1, or ≥ 4 pregnancies was not associated with increased or decreased odds of having high-risk or low-risk telomere length after adjustment for age and race, Table A in S1 File and Table B in S1 File.
Next, we reclassified all women into parity groups (0, 1, 2–3, ≥ 4) after omitting any pregnancy that lasted less than 20 weeks from each woman’s total number of pregnancies to test for the effects of parity/births on telomere length. There were 174 total pregnancies lasting less than 20 weeks: 13 women who had reported 1 pregnancy, 69 women who had reported 2–3 pregnancies, and 92 women who had reported 4 or more pregnancies. There was also no difference in telomere length among these parity groups: 0.99 ± 0.02 in women with 0 births; 1.0 ± 0.02 in women with 1 birth; 0.98 ± 0.01 in women with 2–3 births; and 0.98 ± 0.02 T/S in women with 4 or more births; p = 0.43 for the difference between groups. There was no difference in mean telomere length by parity when we stratified by race, p = 0.27 in African-American and p = 0.37 in Caucasian women.
When we tested for differences in mean telomere length between gravidity groups after omitting subjects with telomere length >3 SD from the mean, (n = 596) the results were the same. In these women, telomere length was similar in all groups: 0.94 ± 0.02 in women with 0 pregnancies; 0.99 ± 0.02 in women with 1 pregnancy; 0.96 ± 0.01 in women with 2–3 pregnancies; and 0.97 ± 0.01 T/S in women with 4 or more pregnancies; p = 0.23 for the difference between groups.
Discussion
Our study showed that mean telomere length did not vary between women with different numbers of pregnancies or differences in parity in our middle-aged cohort. There was no difference in the prevalence of high or low-risk telomere length between gravidity groups and no difference in cardiovascular risk factor profiles between gravidity groups. These results persisted when we analyzed African-American and Caucasian women separately, indicating that there is no effect of gravidity on mid-life telomere length in either Caucasian or African-American women. Our study confirmed racial differences in telomere length between Caucasian and African-American women [18, 19], but we report for the first time that differences in gravidity or parity do not explain the race difference in telomere length in mid-life.
Notably, some earlier studies in telomere length were conducted in postmenopausal women, and the mean ages in these earlier investigations were in the early 60s and late 50’s. The average age in our study was 42 years. This is likely an important distinction as rate of telomere length attrition is rapid from birth to age 18 and then speeds up again after age 45, in late-middle life [11]. Measuring telomere length later in life (past age 45) may reveal differences in telomere length between gravidity groups that were not apparent at a younger age. Measurement later in life may also capture differences in clinical characteristics between groups. In our study, there also were no difference in traditional cardiovascular risk factors between the gravidity groups (Table 2).
Although the prior studies included age in their models, the difference in age at which telomere length was measured between our populations is important. Due to the non-linear pattern of telomere attrition, statistical adjustment for age may be inadequate. Indeed, the authors of previous related studies all reported that shorter telomere length was associated with age [18, 19]. Therefore, a strength of our study is the large sample size that allowed us to group subjects to ensure all participants minimize age differences at the time of telomere length measurement.
Although telomere length has been independently associated with cardiovascular disease, it has also been linked to social factors that influence cardiovascular outcomes and quality of life. Neighborhood social environment [20], neighborhood quality (a metric including crime, noise, and fear) [21], race discrimination [22], and education level [23] have all been associated with leukocyte telomere length. Telomere length is also associated with recent (< 6 yr ago) stressful life events [24]. In another study conducted in young-middle aged women (25–55 years), telomere length was associated with altered left ventricular filling dynamics but not with systolic function or left ventricular mass [25]. In our study, any group differences in education, prevalence of gestational diabetes, or preterm birth also did not influence our findings, despite the acute effects of pregnancy complications on telomerase activity [15].
Barha and colleagues hypothesized that social structure could moderate the effect of gravidity on telomere length in women [26]. In their study of 75 race/ethnically homogenous women with similar lifestyle habits, they found that the association between higher gravidity and longer telomere length approached significance, contrary to their a priori hypothesis that more child-bearing would be associated with greater cellular aging. They postulated that women who had more children may have developed a greater social support networks that buffered any detrimental effects of reproduction on telomere length [26]. Taken together, the results of these physiological and psychological studies suggest the influence of social factors and traditional cardiovascular risk factors are likely more important than gravidity alone in determining telomere length in early middle age in women.
A limitation of the study is the measurement of telomere length at a single time point in early middle age. Serial measurements would have allowed us to determine the rate of telomere shortening. Measuring telomere length later in life may allow the impact of life events from ~18–45 years (including gravidity) to affect telomere length more substantially and yield more separation in telomere length between groups. Not all women in CARDIA completed child-bearing by the Y20 exam, but there were only twenty-six new births reported in all of CARDIA at the Y25 exam, versus 132–546 new births reported at each of the Y0-Y20 exams. Our sample included only 620 of all CARDIA women, and so the subset of women with an additional birth in our study is quite small and likely minimally impacted our findings. Further, an earlier study found that maternal age at first birth was not independently associated with telomere length [26]. We tested for differences in telomere length between women who had had preterm birth and gestational diabetes compared to those who did not and found no difference, but this result should be confirmed in a larger cohort as we were underpowered to detect modest differences.
Conclusions
Gravidity is not associated with telomere length in our biracial cohort of women in early middle age. The protective effects of 2–3 pregnancies on overall and cardiovascular mortality do not appear to be mediated by reduced cellular aging in mid-life. Further investigations should examine the effects of gravidity on mean telomere length later in life, once the rate of telomere attrition has increased, or the effect of gravidity on the rate of telomere shortening from early adulthood to middle or older age.
Supporting information
No difference in odds of having high risk (Table A) or low risk (Table B) telomere length between gravidity groups.
(DOCX)
Data Availability
Data are available from the CARDIA Study, whose authors and paper proposal forms may be contacted at: http://www.cardia.dopm.uab.edu/. The contact person for paper proposals is Linda Sellers: lsellers@uabmc.edu. This dataset is not able to be provided as the data are controlled by the CARDIA investigators to ensure that there are no overlapping CARDIA paper and presentation publications. Any author who wishes to obtain the data may do so after having a manuscript proposal approved by the CARDIA steering committee.
Funding Statement
CARDIA is supported by the National Heart, Lung, and Blood Institute (NHLBI) HHSN268201300025C, HHSN268201300026C, HHSN268201300027C, HHSN268201300028C, HHSN268201300029C, HHSN268200900041C, and partially supported by the Intramural Research Program of the National Institute on Aging (NIA) and an intraagency agreement between NIA and NHLBI (AG0005). This manuscript was reviewed by CARDIA for scientific content. EP was funded by 4R00HL109247-03 and ALC is supported by an American Heart Association Strategically Focused Research Network (14SFRN20480260 Greenland, PI) Fellow Grant.
References
- 1.Morris EA, Hale SA, Badger GJ, Magness RR, Bernstein IM. Pregnancy induces persistent changes in vascular compliance in primiparous women. American journal of obstetrics and gynecology. 2015;212(5):633 e1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lv H, Wu H, Yin J, Qian J, Ge J. Parity and Cardiovascular Disease Mortality: a Dose-Response Meta-Analysis of Cohort Studies. Scientific reports. 2015;5:13411 doi: 10.1038/srep13411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Niemczyk NA, Catov JM, Barinas-Mitchell E, McClure CK, Roberts JM, Tepper PG, et al. Nulliparity is associated with less healthy markers of subclinical cardiovascular disease in young women with overweight and obesity. Obesity. 2015;23(5):1085–91. doi: 10.1002/oby.21044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vaidya D, Bennett WL, Sibley CT, Polak JF, Herrington DM, Ouyang P. Association of parity with carotid diameter and distensibility: multi-ethnic study of atherosclerosis. Hypertension. 2014;64(2):253–8. doi: 10.1161/HYPERTENSIONAHA.114.03285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanghavi M, Kulinski J, Ayers CR, Nelson D, Stewart R, Parikh N, et al. Association between number of live births and markers of subclinical atherosclerosis: The Dallas Heart Study. European journal of preventive cardiology. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buxton JL, Suderman M, Pappas JJ, Borghol N, McArdle W, Blakemore AI, et al. Human leukocyte telomere length is associated with DNA methylation levels in multiple subtelomeric and imprinted loci. Scientific reports. 2014;4:4954 doi: 10.1038/srep04954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cawthon RM, Smith KR, O'Brien E, Sivatchenko A, Kerber RA. Association between telomere length in blood and mortality in people aged 60 years or older. Lancet. 2003;361(9355):393–5. doi: 10.1016/S0140-6736(03)12384-7 [DOI] [PubMed] [Google Scholar]
- 8.Burnett-Hartman AN, Fitzpatrick AL, Kronmal RA, Psaty BM, Jenny NS, Bis JC, et al. Telomere-associated polymorphisms correlate with cardiovascular disease mortality in Caucasian women: the Cardiovascular Health Study. Mechanisms of ageing and development. 2012;133(5):275–81. doi: 10.1016/j.mad.2012.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kroenke CH, Pletcher MJ, Lin J, Blackburn E, Adler N, Matthews K, et al. Telomerase, telomere length, and coronary artery calcium in black and white men in the CARDIA study. Atherosclerosis. 2012;220(2):506–12. doi: 10.1016/j.atherosclerosis.2011.10.041 [DOI] [PubMed] [Google Scholar]
- 10.Strazhesko I, Tkacheva O, Boytsov S, Akasheva D, Dudinskaya E, Vygodin V, et al. Association of Insulin Resistance, Arterial Stiffness and Telomere Length in Adults Free of Cardiovascular Diseases. PloS one. 2015;10(8):e0136676 doi: 10.1371/journal.pone.0136676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Masi S, D'Aiuto F, Martin-Ruiz C, Kahn T, Wong A, Ghosh AK, et al. Rate of telomere shortening and cardiovascular damage: a longitudinal study in the 1946 British Birth Cohort. European heart journal. 2014;35(46):3296–303. doi: 10.1093/eurheartj/ehu226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Willerson JT, Ridker PM. Inflammation as a cardiovascular risk factor. Circulation. 2004;109(21 Suppl 1):II2–10. doi: 10.1161/01.CIR.0000129535.04194.38 [DOI] [PubMed] [Google Scholar]
- 13.Krauss J, Farzaneh-Far R, Puterman E, Na B, Lin J, Epel E, et al. Physical fitness and telomere length in patients with coronary heart disease: findings from the Heart and Soul Study. PloS one. 2011;6(11):e26983 doi: 10.1371/journal.pone.0026983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Donovan A, Pantell MS, Puterman E, Dhabhar FS, Blackburn EH, Yaffe K, et al. Cumulative inflammatory load is associated with short leukocyte telomere length in the Health, Aging and Body Composition Study. PloS one. 2011;6(5):e19687 doi: 10.1371/journal.pone.0019687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fragkiadaki P, Tsoukalas D, Fragkiadoulaki I, Psycharakis C, Nikitovic D, Spandidos DA, et al. Telomerase activity in pregnancy complications (Review). Molecular medicine reports. 2016;14(1):16–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davy P, Nagata M, Bullard P, Fogelson NS, Allsopp R. Fetal growth restriction is associated with accelerated telomere shortening and increased expression of cell senescence markers in the placenta. Placenta. 2009;30(6):539–42. doi: 10.1016/j.placenta.2009.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cawthon RM. Telomere measurement by quantitative PCR. Nucleic acids research. 2002;30(10):e47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carty CL, Kooperberg C, Liu J, Herndon M, Assimes T, Hou L, et al. Leukocyte Telomere Length and Risks of Incident Coronary Heart Disease and Mortality in a Racially Diverse Population of Postmenopausal Women. Arteriosclerosis, thrombosis, and vascular biology. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hunt SC, Chen W, Gardner JP, Kimura M, Srinivasan SR, Eckfeldt JH, et al. Leukocyte telomeres are longer in African Americans than in whites: the National Heart, Lung, and Blood Institute Family Heart Study and the Bogalusa Heart Study. Aging cell. 2008;7(4):451–8. doi: 10.1111/j.1474-9726.2008.00397.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Needham BL, Carroll JE, Diez Roux AV, Fitzpatrick AL, Moore K, Seeman TE. Neighborhood characteristics and leukocyte telomere length: the Multi-Ethnic Study of Atherosclerosis. Health & place. 2014;28:167–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park M, Verhoeven JE, Cuijpers P, Reynolds CF Iii, Penninx BW. Where You Live May Make You Old: The Association between Perceived Poor Neighborhood Quality and Leukocyte Telomere Length. PloS one. 2015;10(6):e0128460 doi: 10.1371/journal.pone.0128460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chae DH, Nuru-Jeter AM, Adler NE, Brody GH, Lin J, Blackburn EH, et al. Discrimination, racial bias, and telomere length in African-American men. American journal of preventive medicine. 2014;46(2):103–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Needham BL, Mezuk B, Bareis N, Lin J, Blackburn EH, Epel ES. Depression, anxiety and telomere length in young adults: evidence from the National Health and Nutrition Examination Survey. Molecular psychiatry. 2015;20(4):520–8. doi: 10.1038/mp.2014.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Verhoeven JE, van Oppen P, Puterman E, Elzinga B, Penninx BW. The Association of Early and Recent Psychosocial Life Stress With Leukocyte Telomere Length. Psychosomatic medicine. 2015;77(8):882–91. doi: 10.1097/PSY.0000000000000226 [DOI] [PubMed] [Google Scholar]
- 25.Denil SL, Rietzschel ER, De Buyzere ML, Van Daele CM, Segers P, De Bacquer D, et al. On cross-sectional associations of leukocyte telomere length with cardiac systolic, diastolic and vascular function: the Asklepios study. PloS one. 2014;9(12):e115071 doi: 10.1371/journal.pone.0115071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barha CK, Hanna CW, Salvate KG, Wilson SL, Robinson WP, Altman RM, Nepomnaschy PA. Number of Children and Telomere Length in Women: A Prospective, Longitudinal Evaluation. PloS one. 2016; 11(1):e0146424 doi: 10.1371/journal.pone.0146424 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
No difference in odds of having high risk (Table A) or low risk (Table B) telomere length between gravidity groups.
(DOCX)
Data Availability Statement
Data are available from the CARDIA Study, whose authors and paper proposal forms may be contacted at: http://www.cardia.dopm.uab.edu/. The contact person for paper proposals is Linda Sellers: lsellers@uabmc.edu. This dataset is not able to be provided as the data are controlled by the CARDIA investigators to ensure that there are no overlapping CARDIA paper and presentation publications. Any author who wishes to obtain the data may do so after having a manuscript proposal approved by the CARDIA steering committee.