Abstract
Both daily stress and the tendency to react to stress with heightened levels of negative affect (i.e., stress sensitivity) are important vulnerability factors for adverse mental health outcomes. Mindfulness-based stress reduction (MBSR) may help to reduce perceived daily stress and stress sensitivity. The purpose of this study was to examine how change in perceived stress, negative affect (NA), and the decoupling between perceived stress and NA evolved over the course of a MBSR program, without making any a priori assumptions on the shape of change. Seventy-one adults from the general population participating in MBSR provided daily diary assessments of perceived stress and NA during MBSR. The time-varying effect model (TVEM) indicated that perceived stress and NA decreased in a linear fashion rather than in a non-linear fashion, both as a function of time and as a function of the cumulative number of days of mindfulness practice. Both TVEM and multilevel growth modeling showed that the association between perceived stress and NA did not decrease over the course of MBSR. The findings support the hypothesis that MBSR reduces NA and also reduces the extent to which individuals perceive their days as stressful. Also, the results suggest that there is a dose-response relationship between the amount of mindfulness practice and reductions in daily stress and NA.
Keywords: Daily diary studies, intensive longitudinal methods, stress reactivity, emotional regulation, mindfulness, time-varying effect model
Introduction
Heightened reactivity to daily stressors is an important risk factor for negative mental health outcomes (Wichers et al., 2009). Perceived stress is associated with higher levels of depression (Roberts & Kassel, 1997) as well as recurrence of depressive symptoms in remitted patients (Kok et al., 2014). Perceiving daily events as highly stressful may not only be maladaptive in itself, but may also set other unhelpful processes in motion, such as responding to stress with heightened levels of negative emotions (i.e., stress sensitivity) (Hammen, 2015). The tendency to display increased negative affect (NA) when experiencing stress in daily life may make individuals more vulnerable for psychopathology (Gunthert, Cohen, Butler, & Beck, 2007; Luyten et al., 2011; Myin-Germeys et al., 2003; van Winkel et al., 2015; Wichers et al., 2007). Because perceived daily stress and stress-sensitivity seem to be related to risk of adverse mental health outcomes, they may be promising targets for intervention.
In fact, interventions are available which hold promise for helping reduce stress and stress sensitivity. In particular, mindfulness-based interventions such as Mindfulness-Based Stress Reduction (MBSR) (Kabat-Zinn, 1990) focus on training individuals to respond more mindfully to experiences, including negative thoughts and feelings. The capacity to be aware of experiences without judging them or reacting to them (i.e., mindfulness; Kabat-Zinn, 1994) is especially useful when experiencing daily stress. Dispositional mindfulness has been associated with lower levels of reported stress (Bao, Xue, & Kong, 2015; Weinstein, Brown, & Ryan, 2009) and lower emotional reactivity to lab-induced stress (Arch & Craske, 2010; Brown, Weinstein, & Creswell, 2012; Bullis, Bøe, Asnaani, & Hofmann, 2014; Feldman, Lavallee, Gildawie, & Greeson, 2016). Moreover, randomized controlled studies suggest that mindfulness-based interventions can reduce stress appraisal after lab-induced stress (Britton, Shahar, Szepsenwol, & Jacobs, 2012; Creswell, Pacilio, Lindsay, & Brown, 2014; Hoge et al., 2013), reduce overall perceptions of stress (van Son et al., 2013; Zainal, Booth, & Huppert, 2013), and reduce blood pressure (Nyklíček, Mommersteeg, Van Beugen, Ramakers, & Van Boxtel, 2013). There have been fewer attempts to explore the effect of mindfulness-based interventions on stress sensitivity. The available studies suggest that mindfulness-based interventions reduce daily levels of stress-related anxious affect (Davis, Zautra, Wolf, Tennen, & Yeung, 2015) and distress in response to lab-induced social stress (Creswell et al., 2014; Hoge et al., 2013).
Because intervention studies predominantly focused on pre-post treatment change in stress, little is known about how change in stress and sensitivity to stress evolves over time in the course of mindfulness-based interventions. Simply comparing assessments pre- and post-treatment does not reveal details such as the amount of time or treatment required for average patients to noticeably improve (Vittengl, Clark, Thase, & Jarrett, 2013), whether the effects of treatment accumulate over time, and whether average change trajectories are linear or non-linear (Hayes, Laurenceau, Feldman, Strauss, & Cardaciotto, 2007). To our knowledge, only one study examined change in perceived stress with repeated assessments (i.e., weekly) over the course of a MBSR program (Baer, Carmody, & Hunsinger, 2012) and the course of change in stress sensitivity has yet to be investigated. There may be multiple routes to improvement (Barkham, Stiles, & Shapiro, 1993) and change may be non-linear, as can be the case during psychotherapy (Schiepek, Tominschek, & Heinzel, 2014).
Intensive longitudinal data (i.e., many repeated assessments within individuals over time (Bolger & Laurenceau, 2013)) over the course of an intervention make it possible to study whether improvement occurs incrementally and at a constant rate (linear) or non-linear (e.g., curve linear) and how quickly individuals improve (Chu, Skriner, & Zandberg, 2013; Hayes et al., 2007). Although a number of quantitative techniques are available to examine such change over time (e.g., multilevel modeling and latent growth curve modeling), these are not sensitive to plausible non-linearity in change over time. A method that addresses this issue is Time-Varying Effect Modeling (TVEM; (Tan, Shiyko, Li, Li, & Dierker, 2012). TVEM can flexibly accommodate nonlinear change, because it does not involve a priori assumptions about the shape of change, such as linearity or quadraticity (Shiyko, Burkhalter, Li, & Park, 2014). Moreover, TVEM analyses allow investigators to examine whether the association between two variables changes over time (Tan et al., 2012), as regression coefficients are estimated as smooth, nonparametric functions of time instead of fixed constants (Hastie & Tibshirani, 1993). Because of these features, TVEM has recently been advocated as a promising method to examine processes of change during psychotherapy (Wright, Hallquist, Swartz, Frank, & Cyranowski, 2014).
In the current study, we will apply TVEM to examine 1) the shape of change in perceived daily stress and in NA over the course of MBSR and 2) the extent to which the association between perceived daily stress and daily negative affect changes over the course of a MBSR program. It is hypothesized that perceived stress and NA will decrease over the course of the program. Furthermore, we hypothesize that the strength of the association between perceived stress and NA (stress sensitivity) will decrease (decouple) over the course of the MBSR program. Because some individuals will perform more daily mindfulness practice than others, not every participant may actually receive the same dose of mindfulness practice. Therefore, we not only examine the shape of change as a function of time in days since the beginning of the MBSR program, but also as a function of the cumulative number of days on which individuals indeed performed a formal mindfulness exercise.
Method
Participants
Participants were individuals from the general population who signed up for a MBSR program between January 2010 and June 2012 (see Snippe, Nyklíček, Schroevers, & Bos, 2015 for a more elaborate description of the participants and procedures). Individuals were offered a 10% discount on the MBSR program if they were willing to participate in an accompanying diary study. Eligibility criteria were the ability to read and write in Dutch and the absence of severe psychiatric disorders, such as severe major depressive disorder, suicidal ideation, or psychotic symptoms. All of the 187 individuals who signed up for the MBSR program during the study period were eligible for the study. Of these 187 individuals, 85 (45%) were willing to participate in the study and provided written informed consent.
Individuals who participated in the diary study were on average younger (M = 40.2, SD = 10.1) compared to individuals who did not provide consent to participate (M = 45.4, SD = 9.4, t = 3.6, p <0.01). There were no other significant differences between participants of the diary study and individuals who did not agree to participate regarding gender, employment, presence of a chronic somatic disease, use of antidepressants, baseline scores on the Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1983), baseline scores on the Depression, Tension, Anger, and Fatigue subscales from the short form of the Profile of Mood States (POMS-SF) (Shacham, 1983; Wald & Mellenbergh, 1990), or change from pre-treatment to post-treatment on the Perceived Stress Scale and the subscales of the POMS-SF.
Procedure
Participants completed baseline questionnaires online before the first session of the MBSR program. The diary study started the day after the first MBSR session and ended at the day of the last session of the MBSR program (study period = 49 days). During the MBSR program, participants received a link to the online diary questions on a daily basis. Participants were instructed to complete the daily questions each day after 5 PM. When the daily questions were filled out on fewer than six days a week, participants received an e-mail reminder to promote adherence.
Intervention
The MBSR program was based on the program as developed by Jon Kabat-Zinn (1990). This 8-week group program aims at training mindfulness by means of mindfulness meditation practice, yoga exercises, psychoeducation, and group sharing of experiences. The program also includes training to become aware of one's responses to stress and provides techniques that may bring about healthier stress responses. The MBSR program consists of weekly 2.5 hour group sessions and an optional 6 hour retreat. Participants were encouraged to perform homework meditation and practices for 40 minutes per day. The primary instructor for the MBSR program was certified by the Dutch Association for Mindfulness.
Measures
Perceived stress
Perceived stress during the past day was assessed with four items. Participants rated the extent to which they experienced their day as being busy, demanding, hectic and out of control on a 5-point Likert scale ranging from 1 (not at all) to 5 (extremely). Similar measures of perceived daily stress have been used previously (von Haaren et al., 2013). A daily perceived stress score was calculated by taking the mean of the four items (range 1 to 5). The internal consistency of perceived stress, considering only the first day of the study to avoid having to account for within-person clustering, was sufficient (Cronbach α = 0.88).
Negative affect
Items of the Depression, Tension, Anger, and Fatigue subscales from the short form of the Profile of Mood States (POMS-SF) (Shacham, 1983; Wald & Mellenbergh, 1990) were used to assess daily Negative Affect (NA). For each of the four subscales, two items were selected based on high factor loadings on the original subscales of the POMS-SF (Baker, Denniston, Zabora, Polland, & Dudley, 2002): blue and miserable (Depression), tense and nervous (Tension), angry and peeved (Anger), and exhausted and fatigued (Fatigue). Participants rated the presence of each mood state during the past day on a 5-point Likert scale ranging from 1 (not at all) to 5 (extremely). The daily NA score was calculated by taking the mean of the eight NA items (range: 1 to 5). In a previous study, we showed that the internal consistency and the convergent validity of the daily NA scale involving all eight items is sufficient (Snippe et al., 2015).
Factor analyses, using varimax rotation, were performed on the NA items and the perceived stress items to test whether perceived stress and NA can indeed be regarded as separate constructs in the current data set. When imposing an orthogonal two-factor structure, the analyses supported treating stress and NA as separate, with all perceived stress items loading on one factor (average factor loading: 0.84) and the NA items loading on a second factor (average factor loading: 0.64).
Mindfulness practice
Participants recorded whether they performed a formal mindfulness practice exercise during the past day (yes or no).
Baseline Negative Affect
Baseline NA was assessed with the subscales Depression, Tension, Anger, and Fatigue from the 32-item POMS-SF (Shacham, 1983; Wald & Mellenbergh, 1990) before the start of the MBSR program.
Statistical analyses
Data preparation and checks
Fewer observations were present at the end of the mindfulness training. This may result in biased results at the end of the training because the sample at the end of the training differs from the sample at the start of the training. Therefore, we included a period during which most observations were present. Based on an examination of attrition over time, we chose to analyze data from all individuals who were still participating on study day 40. Participants that fulfilled this criterion but missed a session in between were not excluded as this group was expected to still perform daily homework assignments during the included period. This resulted in a sample of 71 (out of 85) participants.
Analyses
Time Varying Effect Modeling (TVEM; Tan et al., 2012) was applied to examine the shape of change. TVEM, which is based on varying-coefficient modeling (see Hastie & Tibshirani, 1993), estimates regression coefficients as smooth functions of time rather than constants. With TVEM, splines are used to flexibly estimate the coefficient functions across continuous time, allowing conditional means and associations to change with time. All models were estimated with the MixTVEM software (Dziak, Li, Tan, Shiffman, & Shiyko, 2015) in R. MixTVEM also allows the sample to be modeled as a mixture of latent classes with different parameters, but we chose to treat the whole sample as a single class because of the modest sample size.
We first examined how perceived stress and NA changed as a function of i) time in days and ii) days of mindfulness practice using intercept-only TVEM models:
where tij denotes time in days (or in days of mindfulness practice, depending on the analysis) for subject i at assessment j, yij is negative affect or perceived stress (depending on the analysis), β0(tij) is the time-varying average level of Y at any given time point, and ɛij is the random error. β0(tij) can be thought of as a smooth function giving the estimated time-varying average level of y at any given time point, that is, a smooth nonparametric growth curve for y.
We then examined how the association between perceived stress and NA changed as function of time (measured either in total days or in days of mindfulness practice) with a model of the form:
where tij denotes time in days or days of mindfulness practice for subject i at assessment j, yij represents negative affect, β0(tij) is the time varying average level of y at any given time point when x is 0, β1(tij) is the time varying effect of perceived stress, and ɛij is the random error.
The functions were estimated using the penalized cubic B-spline method of Eilers and Marx (1996) using 5 equally spaced knots. In theory this allows a very rich and flexible estimate of a smooth function without specifying a specific shape of change in advance. In order to prevent overfitting (fitting noise), a penalty function is added to the likelihood function, which acts similar to a Bayesian prior to bias the solution towards a straight line. The size of the penalty function and thus the degree of departure from a straight line was chosen using a Bayesian Information Criterion (BIC) measure. The errors are assumed to be independent between subjects, but correlated within subjects following a modified autoregressive model that allows discontinuities (Dziak et al., 2015).
When the TVEM models indicated that the shape of change was linear, linear multilevel growth curve modeling was performed. A parametric model such as a linear growth curve is less flexible than a nonparametric curve, but has the advantage of summarizing a relationship in a way that is more parsimonious and easier to interpret. To examine whether perceived stress and NA changed over time, multilevel analyses were performed with either NA or perceived stress as the dependent variable. A variable denoting time, as well as a lagged value of the dependent variable (yt-1), were included as predictors. Time was included either in total days/7 (i.e., weeks) or in days of mindfulness practice/7, to put the coefficient estimates on a more familiar scale.
To examine change in the associations between perceived stress and NA over time, NA was included as the dependent variable in a multilevel analysis, and the predictors included perceived stress, lagged NA, time, and the interaction (product) of time and perceived stress. Such an interaction between a covariate and time can be seen as a simple form of TVEM, where the relationship is constrained to be linear. All linear growth curve models included a random intercept and random slopes for the time-varying variables.
Results
The 71 participants included in the analyses completed a total of 2,182 assessments (average of 31 assessments per participant across 40 days). The average level of NA over the course of the MBSR program was 1.8, with a minimum person mean of 1.1 and a maximum person mean of 3.7. The average level of perceived stress over the course of the MBSR program was 1.3, with a minimum person mean of 0.04 and a maximum person mean of 2.6.
Change over time in perceived stress and negative affect
The average shape of change in perceived stress and NA appeared to be linear rather than non-linear (see graphs based on the TVEM in Figure 1). Both stress and NA decreased as a function of time and as a function of mindfulness practice. Linear growth curve models showed an average linear decrease of 0.03 per week both in NA and in perceived stress (see Table 1). For each additional week of mindfulness practice, the average linear decrease in perceived stress was 0.06 and the average linear decrease in NA was 0.04 (see Table 1).
Figure 1. Change in negative affect and perceived stress over the course of the MBSR program.
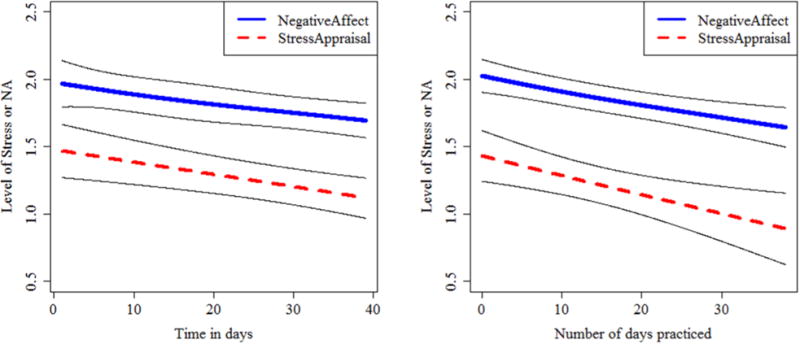
Note: The graphs represent the change in perceived stress and NA over time in days (left) or number of days practiced (right). The graphs are based on intercept-only TVEM analyses.
Table 1. Change in perceived stress and negative affect as estimated with Linear Growth Curve Modeling.
| Perceived stress | Negative affect | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Fixed effect β (SE) | t | p | Random Effect: SD | β (SE) | t | p | Random Effect: SD | |
|
|
|
|||||||
| Time in weeks | ||||||||
| Intercept | 1.04 (0.09) | 11.57 | < 0.01 | 0.61 | 1.43 (0.08) | 17.32 | < 0.01 | 0.56 |
| Perceived stress t-1 | 0.25 (0.03) | 9.21 | < 0.01 | 0.12 | 0.26 (0.03) | 8.45 | < 0.01 | 0.17 |
| NA t-1 | ||||||||
| Time in weeks | -0.03 (0.02) | -1.94 | 0.05 | 0.09 | -0.03 (0.01) | -3.68 | < 0.01 | 0.03 |
| N weeks practiced | ||||||||
| Intercept | 1.01 (0.08) | 12.26 | < 0.01 | 0.56 | 1.49 (0.08) | 19.70 | < 0.01 | 0.49 |
| Perceived stress t-1 | 0.25 (0.03) | 9.53 | < 0.01 | 0.13 | 0.25 (0.03) | 8.39 | < 0.01 | 0.16 |
| NA t-1 | ||||||||
| Weeks of practice | -0.06 (0.03) | -2.16 | 0.03 | 0.14 | -0.04 (0.01) | -4.36 | < 0.01 | 0.02 |
Note: Time in weeks = days since the start of MBSR/7, weeks of practice = number of days of mindfulness practice so far/7. The presented multilevel models included 71 individuals and 2111 observations.
Change in the association between perceived stress and NA over the course of MBSR
TVEM analyses indicated a positive association between perceived stress and daily NA (see Figure 2). There did not appear to be a significant change in this association between perceived stress and NA as a function of time or as a function of the number of mindfulness practice days. Linear growth curve modeling also indicated no significant linear change in the association between perceived stress and NA as a function of time in weeks or as a function of amount of mindfulness practice (see Table 2).
Figure 2. Change in the association between perceived stress and NA over the course of the MBSR program.
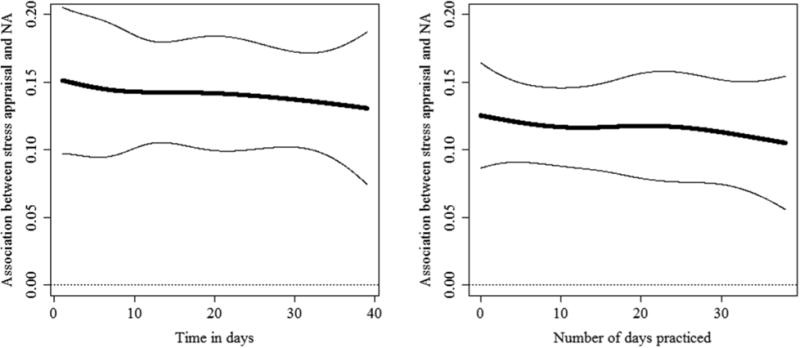
Note: Graphs are based on TVEM analyses representing the time-varying effect of perceived stress on NA over time in days (left) or number of days of mindfulness practice (right).
Table 2. Change in the association between perceived stress and negative affect as estimated with Linear Growth Curve Modeling.
| Outcome | Negative Affect | |||
|---|---|---|---|---|
|
|
||||
| Fixed effect β (SE) | t | p | Random Effect: SD | |
|
|
||||
| Time in weeks | ||||
| Intercept | 1.24 (0.08) | 15.00 | < 0.01 | 0.53 |
| NA t-1 | 0.25 (0.03) | 8.18 | < 0.01 | 0.17 |
| Perceived stress | 0.14 (0.02) | 6.18 | < 0.01 | 0.07 |
| Time in weeks | - 0.02 (0.01) | - 1.97 | 0.05 | 0.04 |
| Time × Stress | <0.01 (0.01) | - 0.34 | 0.93 | 0.01 |
| N days practiced | ||||
| Intercept | 1.35 (0.07) | 18.54 | < 0.01 | 0.46 |
| NA t-1 | 0.24 (0.03) | 7.87 | < 0.01 | 0.17 |
| Perceived stress | 0.12 (0.02) | 7.57 | < 0.01 | 0.06 |
| Weeks practice | -0.03 (0.01) | - 2.61 | < 0.01 | 0.04 |
| Weeks practice × Stress | <-0.01 (0.01) | - 0.23 | 0.82 | 0.02 |
Note: Time in weeks = days since the start of MBSR/7, weeks practice = number of days of mindfulness practice so far/7, Stress = perceived stress. The presented multilevel models included 71 individuals and 2111 observations.
Sensitivity analyses
Several sensitivity analyses were performed to examine the robustness of the results. First, the linear growth curve models were repeated in a subgroup of observations using only days on which a given participant reported at least some level of stress (at least 1 on a scale from 0 to 5). This led to comparable estimates for change over time in days in stress ( β = -0.04, SE = 0.01, t = - 2.91 , p < 0.01) and NA (β = -0.02 , SE = 0.01 , t = -2.52, p = 0.01 ), as well as the association between stress and NA (β < -0.01, SE = 0.01, t = - 0.07 , p = 0.94).
Second, the linear growth curve models were repeated for various subgroups of the sample. These analyses did not yield relevant differences in the estimates, although the decrease in perceived stress was not significant any more in the smaller subgroups because of reduced sample size (only 35 participants). Specifically, analyses to predict change in NA and stress as a function of time in days were performed in a subgroup of individuals who scored above the median level of NA at baseline (Stress: β = -0.03, SE = 0.02, t = - 1.10 , p = 0.27 ; NA: β = -0.04 , SE = 0.01 , t = -2.88, p < 0.01 ), in a subgroup of individuals who scored above the median for total number of days on which they performed at least one formal mindfulness exercise (Stress: β = -0.02 , SE = 0.03, t = -0.81, p = 0.42; NA: β = 0.03, SE = 0.01, t = -3.27, p < 0.01) in men (Stress: β = -0.02, SE = 0.03, t = - 0.71 , p = 0.48 ; NA: β = -0.04 , SE = 0.01 , t = -2.99, p < 0.01 ), and in women (Stress: β = -0.04, SE = 0.02, t = - 1.78 , p = 0.08 ; NA: β = -0.02 , SE < 0.01 , t = -2.52, p = 0.01 ). Similarly, sensitivity analyses also indicated no change in the associations between perceived stress and NA as a function of time in days, in the subgroup of individuals scoring higher on NA at baseline (β < -0.01, SE = 0.01, t = 0.08 , p = 0.94), in the subgroup of individuals who performed more than the median amount of mindfulness practice (β = 0.01, SE = 0.01, t = 0.80 , p = 0.42), in men (β < 0.01, SE = 0.01, t = 0.56 , p = 0.58), or in women (β < 0.01, SE = 0.01, t = 0.21 , p = 0.84).
Discussion
The aim of the study was to elucidate the nature of change in perceived stress, negative affect (NA), and their association, using daily measures over the course of a MBSR program. Applying TVEM to daily diary data indicated that perceived stress and NA decreased in a linear fashion, both as a function of time and as a function of the cumulative number of days of mindfulness practice. Stress sensitivity, operationalized as the association between perceived stress and NA, did not change over time or as a function of days of mindfulness practice. This study suggests that the MBSR program may reduce the extent to which individuals perceive daily events as stressful, but beyond this does not seem to further reduce the negative affect that comes along with perceiving a given day as being stressful. That is, MBSR seems to reduce both perceived stress and NA, but not to decouple them.
Whether our findings support or do not support the hypothesis that MBSR reduces stress reactivity depends on the exact definition of stress reactivity used. Stress reactivity and stress sensitivity have been operationalized in various ways. Some researchers have studied reactivity as the experience of negative emotions in response to naturally occurring external stressors (Bolger & Schilling, 1991) or to lab induced stressors (Chida & Hamer, 2008; Hoorelbeke, Koster, Vanderhasselt, Callewaert, & Demeyer, 2015). Other researchers, including ourselves in the current study, examined negative emotions in response to perceived stress (e.g., perceiving events as unpleasant, stressful or uncontrollable) (Luyten et al., 2011; Wichers et al., 2010). Stress reactivity, when defined as the association between external daily events and perceived stress, did decrease over the course of the MBSR program, as evidenced by the reduction in subjectively rated stress. However, stress sensitivity, when defined as the association between perceived stress and negative emotions, showed no evidence of decreasing over the course of the program.
It has indeed been observed in previous studies that mindfulness-based interventions decrease emotional reactivity to the stressor of being socially evaluated (Creswell et al., 2014; Hoge et al., 2013). Yet, only one study showed that a mindfulness-based treatment for chronic pain reduced stress sensitivity as operationalized by an anxiety response to daily perceived social stress (Davis et al., 2015). A number of previous studies did indicate that mindfulness-based exercises can decouple other internal experiences (for an overview see Levin, Luoma, & Haeger, 2015), such as negative affect and urges to smoke. Future studies should examine whether the association between the experience of daily external stressors and high perceived stress can be decoupled in a MBSR program.
With TVEM analyses, we were able to demonstrate that the shape of change in the appraisal of daily life stress and NA was rather linear over the course of the study. This finding corresponds with a recent study showing that the average course of change in worry and rumination was also rather linear during Mindfulness-Based Cognitive Therapy (Ietsugu et al., 2014) and that there were no sudden reductions in worry and rumination. The results suggest a dose-response relationship; the more sessions of MBSR individuals received and the more days they performed a formal mindfulness exercise, the more their daily stress and negative affective states decreased. Although this linear improvement presumably does not continue forever, it appears relevant for participants to know that the first 40 days of training and practice lead to continually improving outcomes without reaching a point of diminishing returns. This knowledge may help participants to maximize their benefits from MBSR.
It should be noted that our study focused on an average pattern of change and that individual pathways of change may deviate from this average course. If there are sudden transitions in perceived stress, NA, or their relationship, but these transitions follow very different timing for different people, this may result in an average linear shape of change, even when individual patterns are in fact non-linear. Also, the association between stress and NA may have diminished within some individuals and not for others, as supported by the random effects which indicate inter-individual heterogeneity in the effects. Personalized models with more observations within each individual could give insight into whether individuals' trajectories are also linear or have times of more abrupt change, and also into whether the effect of stress at one moment in time on NA at a subsequent moment in time decreases over time within some individuals.
Sensitivity analyses were performed to rule out some of the possible explanations for our failure to show that perceived stress and NA decoupled during MBSR. One explanation is that stress sensitivity only changes in individuals with certain characteristics. However, the findings did not differ across individuals based on initial levels of NA or gender. Furthermore, one could argue that a change in stress sensitivity can only be detected on days that individuals experience at least some amount of stress. Yet, the analyses did not yield different results when only the days with at least some amount of stress were included. Another plausible explanation is that stress sensitivity did not change as a function of time because participants did not practice mindfulness enough. This explanation also does not hold as stress sensitivity did not change as a function of the number of days on which individuals performed mindfulness practice. Finally, it could be that the association between stress and NA did not change because they are too highly related and can be regarded as a single construct. This does not seem plausible as factor analyses supported a two-factor structure, with one factor representing perceived stress and another representing NA.
The current study has a number of noteworthy strengths. Whereas most studies have examined stress sensitivity in the lab, the present study was conducted in daily life. To our knowledge, this is the first study to explore the possibility of non-linear change during a MBSR program and the first to examine change in the coupling between perceived stress and NA over time. We did so using daily assessments over the course of MBSR and using of a unique non-parametric growth model (TVEM), with which we could detect plausible non-linear changes and change in dynamic associations over time. Furthermore, the use of multiple analytic approaches and the performance of sensitivity analyses strengthens confidence in the reliability of the findings.
However, the study has also several notable limitations. First, we did not directly control or measure the extent to which participants encountered external events that could be seen as stressful. Thus, we cannot rule out that the decrease in perceived stress was due to participants exposing themselves to fewer daily stressors as a result of the MBSR program, rather than becoming more resilient to those stressors as we claim. Second, perceived stress and NA were measured at the same moment in time. Therefore, it could be that the amount of daily negative emotions influenced individuals' perceived stress, instead of NA being a response to perceived stress. Third, the study did not include a control group. We therefore cannot rule out that perceived stress and NA changed for other reasons than following the MBSR program. However, previous controlled studies on mindfulness-based interventions only showed small decreases in stress and NA in the control group (Nyklíček et al., 2013; van Son et al., 2013) so it seems more plausible that the observed decreases in perceived stress and NA are at least in part due to the MBSR program. Fourth, it could be that the included period of 40 days during the MBSR program was not sufficient to be able to observe a change in stress sensitivity. Future studies should reveal whether more mindfulness practice is needed to observe decoupling between perceived stress and NA. Finally, we did not include a detailed assessment of the amount of daily mindfulness practice. Although we do think that our assessment of the number of days on which individuals performed at least one formal mindfulness exercise gives an indication of the amount of home practice, future studies should consider to record the total time spent on mindfulness practice per day and the total number of mindfulness exercises performed per day.
The current study shows how the effects of following an MBSR program on perceived stress and NA unfold incrementally over time and over days of mindfulness practice. Our results suggest that an MBSR course will reduce both stress and NA. However, when individuals do perceive their day as being stressful, it is likely that they will still experience negative emotions even after having followed an MBSR course. As high levels of stress and NA are risk factors for negative mental health outcomes, mindfulness practice might help to prevent these adverse outcomes as well. The average reduction in stress and in NA over the course of treatment seems to be a gradual, linear decline rather than a sudden drop. The linear decrease in stress and NA as a function of the amount of mindfulness practice suggest that this decline in stress and NA could continue to some extent after the end of the training period if the individual continues to practice. This would be a reason to encourage individuals to continue practicing mindfulness even after finishing an MBSR program.
Acknowledgments
This project was supported by the Foundation “De Drie Lichten” in the Netherlands, an Aspasia Grant (NWO; to M. Wichers), and Award P50 DA010075 from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health. Data analysis was done using the R 3.2.1 software packages. The R software is copyright 2015 by The R Foundation for Statistical Computing. Finally, we thank Bethany Bray and Runze Li for the very helpful discussions.
This project was supported by the Foundation "De Drie Lichten" in the Netherlands, an Aspasia Grant (NWO; to M. Wichers), and Award P50 DA010075 from the National Institute on Drug Abuse (Linda Collins, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health.
Footnotes
Conflict of interest: The authors declare that they have no conflict of interest.
Compliance with Ethical Standards: Ethical approval: All procedures contributing to this work were in accordance with the ethical standards of the relevant national research committees and with the Helsinki Declaration of 1964 and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- Arch JJ, Craske MG. Laboratory stressors in clinically anxious and non-anxious individuals: The moderating role of mindfulness. Behaviour Research and Therapy. 2010;48(6):495–505. doi: 10.1016/j.brat.2010.02.005. [DOI] [PubMed] [Google Scholar]
- Baer RA, Carmody J, Hunsinger M. Weekly change in mindfulness and perceived stress in a mindfulness-based stress reduction program. Journal of Clinical Psychology. 2012;68(7):755–765. doi: 10.1002/jclp.21865. [DOI] [PubMed] [Google Scholar]
- Baker F, Denniston M, Zabora J, Polland A, Dudley WN. A POMS short form for cancer patients: Psychometric and structural evaluation. Psycho-Oncology. 2002;11(4):273–281. doi: 10.1002/pon.564. [DOI] [PubMed] [Google Scholar]
- Bao X, Xue S, Kong F. Dispositional mindfulness and perceived stress: The role of emotional intelligence. Personality and Individual Differences. 2015;78:48–52. doi: 10.1016/j.paid.2015.01.007. [DOI] [Google Scholar]
- Barkham M, Stiles WB, Shapiro DA. The shape of change in psychotherapy: Longitudinal assessment of personal problems. Journal of Consulting and Clinical Psychology. 1993;61(4):667–677. doi: 10.1037/0022-006X.61.4.667. [DOI] [PubMed] [Google Scholar]
- Bolger N, Laurenceau J. Intensive longitudinal methods: An introduction to diary and experience sampling research. New York, NY US: Guilford Press; 2013. [Google Scholar]
- Bolger N, Schilling EA. Personality and the problems of everyday life: The role of neuroticism in exposure and reactivity to daily stressors. Journal of Personality. 1991;59(3):355–386. doi: 10.1111/j.1467-6494.1991.tb00253.x. [DOI] [PubMed] [Google Scholar]
- Britton WB, Shahar B, Szepsenwol O, Jacobs WJ. Mindfulness-based cognitive therapy improves emotional reactivity to social stress: Results from a randomized controlled trial. Behavior Therapy. 2012;43(2):365–380. doi: 10.1016/j.beth.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, Weinstein N, Creswell JD. Trait mindfulness modulates neuroendocrine and affective responses to social evaluative threat. Psychoneuroendocrinology. 2012;37(12):2037–2041. doi: 10.1016/j.psyneuen.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullis JR, Bøe HJ, Asnaani A, Hofmann SG. The benefits of being mindful: Trait mindfulness predicts less stress reactivity to suppression. Journal of Behavior Therapy and Experimental Psychiatry. 2014;45(1):57–66. doi: 10.1016/j.jbtep.2013.07.006. [DOI] [PubMed] [Google Scholar]
- Chida Y, Hamer M. Chronic psychosocial factors and acute physiological responses to laboratory-induced stress in healthy populations: A quantitative review of 30 years of investigations. Psychological Bulletin. 2008;134(6):829–885. doi: 10.1037/a0013342. doi:10.1037/a0013342;101037/a0013342.supp (Supplemental) [DOI] [PubMed] [Google Scholar]
- Chu BC, Skriner LC, Zandberg LJ. Shape of change in cognitive behavioral therapy for youth anxiety: Symptom trajectory and predictors of change. Journal of Consulting and Clinical Psychology. 2013;81(4):573–587. doi: 10.1037/a0033390. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Creswell JD, Pacilio LE, Lindsay EK, Brown KW. Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology. 2014;44:1–12. doi: 10.1016/j.psyneuen.2014.02.007. [DOI] [PubMed] [Google Scholar]
- Davis MC, Zautra AJ, Wolf LD, Tennen H, Yeung EW. Mindfulness and cognitive–behavioral interventions for chronic pain: Differential effects on daily pain reactivity and stress reactivity. Journal of Consulting and Clinical Psychology. 2015;83(1):24–35. doi: 10.1037/a0038200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dziak JJ, Li R, Tan X, Shiffman S, Shiyko MP. Modeling intensive longitudinal data with mixtures of nonparametric trajectories and time-varying effects. Psychological Methods. 2015;20(4):444–469. doi: 10.1037/met0000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eilers P, Marx B. Flexible smoothing with B-splines and penalties. Statistical Science. 1996;11(2):89–102. doi: 10.1214/ss/1038425655. [DOI] [Google Scholar]
- Feldman G, Lavallee J, Gildawie K, Greeson JM. Dispositional mindfulness uncouples physiological and emotional reactivity to a laboratory stressor and emotional reactivity to executive functioning lapses in daily life. Mindfulness. 2016;7(2):527–541. doi: 10.1007/s12671-015-0487-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunthert KC, Cohen LH, Butler AC, Beck JS. Depression and next-day spillover of negative mood and depressive cognitions following interpersonal stress. Cognitive Therapy and Research. 2007;31(4):521–532. doi: 10.1007/s10608-006-9074-1. [DOI] [Google Scholar]
- Hammen C. Stress sensitivity in psychopathology: Mechanisms and consequences. Journal of Abnormal Psychology. 2015;124(1):152–154. doi: 10.1037/abn0000040. [DOI] [PubMed] [Google Scholar]
- Hastie T, Tibshirani R. Varying-coefficient models. Journal of the Royal Statistical Society Series B-Methodological. 1993;55(4):757–796. [Google Scholar]
- Hayes AM, Laurenceau JP, Feldman G, Strauss JL, Cardaciotto L. Change is not always linear: The study of nonlinear and discontinuous patterns of change in psychotherapy. Clinical Psychology Review. 2007;27(6):715–723. doi: 10.1016/j.cpr.2007.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge EA, Bui E, Marques L, Metcalf CA, Morris LK, Robinaugh DJ, Simon NM. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: Effects on anxiety and stress reactivity. Journal of Clinical Psychiatry. 2013;74(8):786–792. doi: 10.4088/JCP.12m08083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoorelbeke K, Koster EHW, Vanderhasselt M, Callewaert S, Demeyer I. The influence of cognitive control training on stress reactivity and rumination in response to a lab stressor and naturalistic stress. Behaviour Research and Therapy. 2015;69:1–10. doi: 10.1016/j.brat.2015.03.010. [DOI] [PubMed] [Google Scholar]
- Ietsugu T, Crane C, Hackmann A, Brennan K, Gross M, Crane RS, Barnhofer T. Gradually getting better: Trajectories of change in rumination and anxious worry in mindfulness-based cognitive therapy for prevention of relapse to recurrent depression. Mindfulness. 2014 doi: 10.1007/s12671-014-0358-3. [DOI] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, US: Delacourt; 1990. [Google Scholar]
- Kabat-Zinn J. Wherever you go, there you are: Mindfulness meditation in everyday life. New York: Hyperion; 1994. [Google Scholar]
- Kok G, van Rijsbergen G, Burger H, Elgersma H, Riper H, Cuijpers P, Bockting C. The scars of childhood adversity: Minor stress sensitivity and depressive symptoms in remitted recurrently depressed adult patients. PLoS ONE. 2014;9(11) doi: 10.1371/journal.pone.0111711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin ME, Luoma JB, Haeger JA. Decoupling as a mechanism of change in mindfulness and acceptance: A literature review. Behavior Modification. 2015;39(6):870–911. doi: 10.1177/0145445515603707. [DOI] [PubMed] [Google Scholar]
- Luyten P, Kempke S, Van Wambeke P, Claes S, Blatt SJ, Van Houdenhove B. Self-critical perfectionism, stress generation, and stress sensitivity in patients with chronic fatigue syndrome: Relationship with severity of depression. Psychiatry: Interpersonal and Biological Processes. 2011;74(1):21–30. doi: 10.1521/psyc.2011.74.1.21. [DOI] [PubMed] [Google Scholar]
- Myin-Germeys I, Peeters F, Havermans R, Nicolson NA, de Vries MW, Delespaul P, van Os J. Emotional reactivity to daily life stress in psychosis and affective disorder: An experience sampling study. Acta Psychiatrica Scandinavica. 2003;107(2):124–131. doi: 10.1034/j.1600-0447.2003.02025.x. [DOI] [PubMed] [Google Scholar]
- Nyklíček I, Mommersteeg PMC, Van Beugen S, Ramakers C, Van Boxtel GJ. Mindfulness-based stress reduction and physiological activity during acute stress: A randomized controlled trial. Health Psychology. 2013;32(10):1110–1113. doi: 10.1037/a0032200. doi:10.1037/a0032200;10 1037/a0032200.supp. [DOI] [PubMed] [Google Scholar]
- Roberts JE, Kassel JD. Labile self-esteem, life stress, and depressive symptoms: Prospective data testing a model of vulnerability. Cognitive Therapy and Research. 1997;21(5):569–589. doi: 10.1023/A:10218615030721023/A:1021861503072. [DOI] [Google Scholar]
- Schiepek GK, Tominschek I, Heinzel S. Self-organization in psychotherapy: Testing the synergetic model of change processes. Frontiers in Psychology. 2014;51089 doi: 10.3389/fpsyg.2014.01089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shacham S. A shortened version of the profile of mood states. Journal of Personality Assessment. 1983;47(3):305–306. doi: 10.1207/s15327752jpa4703_14. [DOI] [PubMed] [Google Scholar]
- Shiyko MP, Burkhalter J, Li R, Park BJ. Modeling nonlinear time-dependent treatment effects: An application of the generalized time-varying effect model (TVEM) Journal of Consulting and Clinical Psychology. 2014;82(5):760–772. doi: 10.1037/a0035267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snippe E, Nyklíček I, Schroevers MJ, Bos EH. The temporal order of change in daily mindfulness and affect during mindfulness-based stress reduction. Journal of Counseling Psychology. 2015;62(2):106–114. doi: 10.1037/cou0000057. [DOI] [PubMed] [Google Scholar]
- Tan X, Shiyko MP, Li R, Li Y, Dierker L. A time-varying effect model for intensive longitudinal data. Psychological Methods. 2012;17(1):61–77. doi: 10.1037/a0025814;101037/a0025814.supp. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Son J, Nyklíček I, Pop VJ, Blonk MC, Erdtsieck RJ, Spooren PF, Pouwer F. The effects of a mindfulness-based intervention on emotional distress, quality of life, and HbA(1c) in outpatients with diabetes (DiaMind) Diabetes Care. 2013;36(4):823–830. doi: 10.2337/dc12-1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Winkel M, Nicolson NA, Wichers M, Viechtbauer W, Myin-Germeys I, Peeters F. Daily life stress reactivity in remitted versus non-remitted depressed individuals. European Psychiatry. 2015;30(4):441–447. doi: 10.1016/j.eurpsy.2015.02.011. [DOI] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Thase ME, Jarrett RB. Nomothetic and idiographic symptom change trajectories in acute-phase cognitive therapy for recurrent depression. Journal of Consulting and Clinical Psychology. 2013;81(4):615–626. doi: 10.1037/a0032879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Haaren B, Loeffler SN, Haertel S, Anastasopoulou P, Stumpp J, Hey S, Boes K. Characteristics of the activity-affect association in inactive people: An ambulatory assessment study in daily life. Frontiers in Psychology. 2013;4 doi: 10.3389/fpsyg.2013.00163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wald FD, Mellenbergh GJ. De verkorte versie van de nederlandse vertaling van de profile of mood states (POMS) Nederlands Tijdschrift Voor De Psychologie En Haar Grensgebieden. 1990;45(2):86–90. [Google Scholar]
- Weinstein N, Brown KW, Ryan RM. A multi-method examination of the effects of mindfulness on stress attribution, coping, and emotional well-being. Journal of Research in Personality. 2009;43(3):374–385. doi: 10.1016/j.jrp.2008.12.008. [DOI] [Google Scholar]
- Wichers M, Peeters F, Geschwind N, Jacobs N, Simons CJP, Derom C, van Os J. Unveiling patterns of affective responses in daily life may improve outcome prediction in depression: A momentary assessment study. Journal of Affective Disorders. 2010;124(1-2):191–195. doi: 10.1016/j.jad.2009.11.010. [DOI] [PubMed] [Google Scholar]
- Wichers M, Geschwind N, Jacobs N, Kenis G, Peeters F, Derom C, van Os J. Transition from stress sensitivity to a depressive state: Longitudinal twin study. The British Journal of Psychiatry. 2009;195(6):498–503. doi: 10.1192/bjp.bp.108.056853. [DOI] [PubMed] [Google Scholar]
- Wichers M, Myin-Germeys I, Jacobs N, Peeters F, Kenis G, Derom C, van Os J. Genetic risk of depression and stress-induced negative affect in daily life. The British Journal of Psychiatry. 2007;191(3):218–223. doi: 10.1192/bjp.bp.106.032201. [DOI] [PubMed] [Google Scholar]
- Wright AGC, Hallquist MN, Swartz HA, Frank E, Cyranowski JM. Treating co-occurring depression and anxiety: Modeling the dynamics of psychopathology and psychotherapy using the time-varying effect model. Journal of Consulting and Clinical Psychology. 2014;82(5):839–853. doi: 10.1037/a0034430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zainal NZ, Booth S, Huppert FA. The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: A meta-analysis. Psycho-Oncology. 2013;22(7):1457–1465. doi: 10.1002/pon.3171. [DOI] [PubMed] [Google Scholar]


