Abstract
Individuals with autism spectrum disorder (ASD) show deficits in social and emotional reciprocity, which often include empathic responding. The younger siblings of children with ASD (high-risk siblings) are at elevated risk for ASD and for subclinical deficits in social-emotional functioning. Higher levels of empathy in high-risk siblings during the second and third years of life predict fewer ASD symptoms and likelihood of diagnosis. We conducted a multi-method investigation of empathic responding to an examiner’s accident in 30 low-risk and 48 high-risk siblings with (n=12) and without ASD outcomes (n=36) at 4–6 years of age. Empathic responding was measured through behavioral observation and parent report. Prosocial behavior did not differ by ASD outcome. Children with ASD exhibited lower levels of personal distress than high-risk and low-risk siblings without ASD. Per parent report, high-risk siblings without ASD demonstrated higher levels of empathic responding than low-risk children, while the ASD group did not differ from children without ASD on this measure. Higher levels of observed empathic concern, but not prosocial behavior, were associated with lower Social Affect scores on the ADOS in high-risk children. Results suggest that ASD diagnosis and symptoms are associated with reduced emotional responsiveness to an adult’s distress, but not associated with deficits in prosocial behavior at preschool age. Results do not support the idea that empathic responding is negatively impacted in a broader autism phenotype. Findings extend previous research by suggesting that empathy may be a protective factor in the social-emotional development of children with familial risk for ASD.
Lay summary
We examined empathic responding to an adult’s accident in children with and without familial risk for ASD at 4–6 years of age. Results suggest that ASD diagnosis and symptoms are associated with reduced emotional responsiveness to an adult’s distress, but not with deficits in helping behavior at preschool age. Findings do not support the idea that deficits in empathic responding are part of a broader autism phenotype.
Keywords: Empathic responding, High-risk siblings, Autism spectrum disorder, Preschool age, Familial risk
Empathy, the ability to recognize and experience the emotions of others, is a key component of social-emotional functioning. Empathy is associated with positive social outcomes, including prosocial behavior (Eisenberg et al., 2010) and social competence (Zhou et al., 2002) at preschool age. Empathic responding is often impaired in individuals with autism spectrum disorder (ASD; Sigman et al., 1992). High-risk siblings (i.e., younger siblings of children with ASD) with ASD outcomes show deficits in empathic responding during the first years of life (Hutman et al., 2010; McDonald & Messinger, 2012). To extend this area of research, we conducted a multi-modal investigation of associations between empathic responding and ASD diagnosis and symptoms in high-risk and low-risk siblings at preschool age.
Empathy is often studied via behavioral responses to distress. Infants demonstrate precursors to empathy through crying in response to other infants’ distress (Sagi & Hoffman, 1976). Personal distress, a self-oriented aversive emotional reaction, is characterized by discomfort after experiencing the emotions of another (Batson et al., 1987; Eisenberg et al., 2010). Personal distress can act as both an early developmental precursor to empathic responses (Hoffman et al., 2008), as well as an independent response to emotional situations (Batson et al., 1987; Eisenberg & Eggum, 2009). By 2 years old, children typically transition from self-oriented responses to the capacity for other-oriented concern (Zahn-Waxler et al., 1992). While children are capable of limited prosocial responses (e.g., instrumental helping) by 18 months of age (Zahn-Waxler et al., 1992), 30-month-old children can understand others’ emotions and engage in helping behaviors based on implicit emotional cues (Svetlova et al., 2010). By 3 to 5 years, children typically evidence theory of mind and perspective-taking skills (Wellman et al., 2001) and regularly display prosocial behaviors (Eisenberg et al., 2006).
High-risk siblings with ASD show deficits in empathic responding to familiar and unfamiliar adults in distress from 12 to 36 months of age (Hutman et al., 2011; McDonald & Messinger, 2012). Likewise, higher levels of empathic responding at 24 months are associated with fewer ASD symptoms at 30 months, suggesting a possible protective role of early empathy abilities in young children with familial risk for ASD (McDonald & Messinger, 2012). It is less clear, however, how deficits in empathic responding present at preschool age—a critical time for social-emotional development (Denham et al., 2003). This period is characterized by increased exposure to peers, necessitating increasingly sophisticated social-emotional behaviors, such as emotion identification and communication (Denham et al., 2003) and cooperative play (Coplan & Arbeau, 2009). Empathy is an important factor in this developing social-emotional competence (Eisenberg et al., 1996; Eisenberg et al., 2006).
Earlier work comparing preschool and school-aged children with ASD to children with typical development and developmental disabilities indicated that ASD was associated with deficits in empathic responding to adults in distress, which were not fully accounted for by differences in intellectual ability (Bacon et al., 1998; Dawson et al., 2004; Sigman et al., 1992). However, more recent findings suggest that empathy deficits in ASD may not be as pervasive as these earlier studies suggested. Rather, empathy deficits in ASD may be particular to the type of empathy (i.e., cognitive vs. emotional), type of responding (e.g., attention to examiner, prosocial behavior), and mode of measurement (e.g., behavioral observation vs. parent-report; Scheeren et al., 2013, Deshamps et al., 2014; Tsang, Gillespie-Lynch, & Hutman, 2016), highlighting the need for further investigation of individual components of empathy using multiple measures of empathic responding.
There is also a lack information on the degree to which empathy deficits are associated with the broader autism phenotype (BAP), which refers to subclinical ASD characteristics in biological relatives of individuals on the spectrum (e.g., Piven, 2001). Parents of children with ASD demonstrate lower cognitive empathy abilities than adults with low genetic risk for autism, suggesting a possible role of mild empathy deficits in the BAP (Grove, Baillie, Allison, Baron-Cohen, & Hoekstra, 2014). A study of high-risk siblings indicated mild deficits in parent-reported cognitive empathy and theory of mind abilities in high-risk siblings without ASD, while deficits in parent-reported emotional empathy and attention to an examiner in distress were not apparent (Tsang, Gillespie-Lynch, & Hutman, 2016).
In the current study, we investigated whether 4- to 6-year-old children with and without familial risk for ASD differed in observed and parent-reported empathic responding based on ASD outcome and level of symptomatology. Children were divided into low risk/no ASD, high risk/no ASD, and ASD groups, and covariates including age, gender, and intellectual ability were evaluated. Individual aspects of empathic responding (empathic concern, prosocial behavior, personal distress) were utilized to uniquely assess whether children with ASD show general or more distinct areas of deficit in their response to an adult in distress. We hypothesized that: 1) children with ASD would show lower levels of emotional responsiveness (empathic concern and personal distress) to an adult in distress than children without ASD, 2) parents of children with ASD would report lower levels of empathic responding than parents of children without ASD, and 3) children with familial risk who had higher levels of empathic responding would have fewer ASD symptoms. We did not expect children without ASD to differ based on familial risk status, nor did we expect group differences in prosocial behavior.
Method
Participants
Participants were part of a longitudinal study examining the development of infants at elevated risk for ASD due to having an older sibling with ASD. The sample consisted of 78 children with data from an empathic elicitation task and/or parent report of empathic responding, and ASD outcome data at 4–6 years. There were no differences in demographic variables between ASD outcome groups (see Table 1). Children with ASD had lower IQs and higher Calibrated Severity Scores (CSS; Hus, Gotham, & Lord, 2014) on the Autism Diagnostic Observation Schedule (ADOS; Lord et al., 2000) than high-risk and low-risk siblings without ASD.
Table 1.
Participant information by ASD outcome group
| Demographic variable | Total n (%) | Low risk/no ASD n (%) | High risk/no ASD n (%) | ASD n (%) | p |
|---|---|---|---|---|---|
| ASD outcome | 78 (100%) | 30 (39%) | 36 (46%) | 12 (15%) | |
| Gender | .27 | ||||
| Male | 47 (60%) | 15 (50%) | 23 (64%) | 9 (75%) | |
| Female | 31 (40%) | 15 (50%) | 13 (36%) | 3 (25%) | |
| Race/ethnicity | .79 | ||||
| White/Caucasian | 30 (38%) | 12 (40%) | 12 (33%) | 6 (50%) | |
| Black/African-American | 2 (3%) | 1 (3%) | 1 (3%) | 0 (0%) | |
| Hispanic/Latino | 32 (41%) | 11 (37%) | 17 (47%) | 4 (33%) | |
| Asian/Asian-American | 2 (3%) | 1 (3%) | 0 (0%) | 1 (8%) | |
| More than one race/Other | 12 (15%) | 5 (17%) | 6 (17%) | 1 (8%) | |
| Maternal education | .38 | ||||
| High school | 3 (4%) | 0 (0%) | 3 (8%) | 0 (0%) | |
| Some college | 3 (4%) | 1 (3%) | 2 (6%) | 0 (0%) | |
| 2-year college | 11 (14%) | 5 (17%) | 5 (14%) | 1 (8%) | |
| 4-year college | 25 (32%) | 11 (38%) | 12 (33%) | 2 (17%) | |
| Advanced/professional degree | 35 (45%) | 12 (41%) | 14 (39%) | 9 (75%) | |
|
| |||||
| Measure | M (SD) | ||||
|
| |||||
| Age at visit (months) | 61.87 (9.86) | 63.00 (11.82) | 62.23 (8.58) | 57.96 (7.57) | .32 |
| WPPSI-III Full Scale IQ | 102.20 (15.07) | 107.59 (11.58) | 102.06 (13.13) | 89.58 (20.46) | <.01 |
| ADOS-CSS | 2.47 (2.20) | 1.69 (1.14) | 1.83 (1.46) | 6.25 (2.18) | <.001 |
| SA-CSS | 2.87 (2.51) | 2.11 (1.75) | 2.25 (1.95) | 6.50 (2.51) | <.001 |
| RRB-CSS | 3.09 (2.96) | 1.29 (1.05) | 2.92 (2.58) | 7.83 (1.70) | <.001 |
Note. Maternal education was unavailable for one child in the low risk/no ASD group. ADOS-CSS was missing for one child in the low risk/no ASD group. WPPSI-III Full Scale IQ scores were missing for one child in the low risk/no ASD group and two children in the high risk/no ASD group. ASD = autism spectrum disorder. WPPSI-III = Wechsler Preschool and Primary Scale of Intelligence, Third Edition. ADOS = Autism Diagnostic Observation Schedule. CSS = Calibrated Severity Score. SA = Social Affect. RRB = Restricted and Repetitive Behaviors. For ADOS severity scores: Autism Spectrum cutoff = 4, Autism cutoff = 6 (Gotham et al., 2009). SA-CSS and RRB-CSS calculated based on criteria presented in Hus et al. (2014).
Procedure
Children visited the laboratory with a caregiver at 4–6 years old. They participated in a battery of behavioral tasks, followed by a diagnostic assessment, which included the Wechsler Preschool and Primary Scale of Intelligence, Third Edition (Wechsler, 2002) and ADOS (Lord et al., 2000).
Measures
Empathic responding
Children’s empathic responses were measured with an observational task and a parent questionnaire.
Behavior observation
Following parent-child interaction tasks, the parent was escorted from the room by a research associate and told: “One of the examiners will pretend to hurt herself. We want to see how [child] will respond without anyone else in the room.” A second examiner briefly chatted with the child, then picked up a bin of toys and pretended to hurt herself by dropping it on her foot and saying, “Ow, I hurt my foot. Ow, that really hurt.” This portion of the task was focused on eliciting children’s emotional response to distress. After about 10 seconds, if the child had not started picking up the toys, the examiner said “Oh, what a mess!” After several seconds, if the child did not start picking up, the examiner began slowly picking up the toys. This portion of the task was focused on eliciting prosocial behavior. The task ended when the toys were all picked up.
Based on previous work (Young et al., 1999; McDonald & Messinger, 2012), a coding system was developed to measure children’s responses along three dimensions: empathic concern, prosocial behavior, and personal distress. See Table 2 for a detailed description of the coding system. A research associate blind to ASD risk group and outcome coded each episode. Approximately 20% of the videos were double coded to assess inter-rater reliability. Intra-class correlations indicated high reliability for each dimension (>.85; see Table 2).
Table 2.
Description of empathy-related dimensions
| Measure | Description | Ratings | ICC |
|---|---|---|---|
| Empathic Concern | Facial, gestural, and vocal signs of sympathy and concern | 1 – no signs of concern; may ignore examiner, show inappropriate affect, or otherwise seem unconcerned | .87 |
| 2 – sobering of attention, slight concern expressed | |||
| 3 – moderate concern, relatively clear but brief change to sad/sympathetic affect | |||
| 4 – expressed clear facial concern and/or sympathetic vocal expression | |||
| Prosocial Behavior | Attempts to help the examiner | 1 – no helping behavior or only after a direct prompt | .95 |
| 2 – helped after multiple indirect prompts | |||
| 3 – helped after one indirect prompt | |||
| 4 – spontaneously began helping | |||
| Personal Distress | Physical/bodily signs of tension/anxiety | 1 – no apparent distress, child appears relaxed | .95 |
| 2 – brief, relatively minor tension or anxiety expressed, child is able to overcome quickly | |||
| 3 – moderate body tension/freezing or apparent anxiety, which may delay helping | |||
| 4 – significant distress as evident by prolonged body tension/freezing, significantly interrupts behavioral response |
Note. ICC = Intra-class correlations (absolute agreement, single measure)
Parent report
Empathic responding was also assessed with the Empathy and Prosocial Response subscale of the Conscience Questionnaire (see Kochanska et al., 1994). This subscale consists of 13 items measuring children’s empathic responding rated by parents on a 7-point Likert scale (e.g., “Will try to comfort or reassure another in distress,” “Is not likely to become upset if a playmate cries,” “Can tell at just a glance how others are feeling”). Internal consistency within the sample was good (Cronbach’s alpha = .80).
ASD outcome
Following the 4–6-year visit, children fell into three outcome groups: low risk/no ASD, high risk/no ASD, and ASD. A licensed psychologist who was blind to risk group made diagnoses according to DSM-IV-TR criteria (American Psychiatric Association, 2000), and informed by results from the Autism Diagnostic Inventory-Revised (administered at 36 months; Lord et al., 1994) and ADOS (administered at 4–6 years; Lord et al., 2000). Within the high risk group, 12 of 48 (25%) children were diagnosed with ASD. Calibrated Severity Scores for the Social Affect (SA-CSS) and Restricted and Repetitive Behaviors (RRB-CSS) ADOS subdomains were calculated as a measure of ASD symptoms (Hus et al., 2014). SA-CSS and RRB-CSS ranged from 1 to 10, indicating scores comprising the full CSS range—from a lack of symptomatology to severe symptoms. ADOS protocols were scored by research-reliable clinicians.
Analytic Plan
Preliminary analyses examined associations between empathic responding and possible covariates. Analysis of variance models were then conducted for each empathic responding variable to assess ASD outcome group differences. Significant models were followed up by post hoc comparisons of the three outcome groups (Bonferroni-corrected p = .017). Finally, correlations and regression models predicting SA-CSS and RRB-CSS from empathic responding variables were conducted within the high risk group to examine ASD-related differences in empathy on a continuous metric.
Results
For the sample as a whole, correlations among empathic responding variables (see Table 3) indicated that children who responded with higher levels of visible distress to an examiner’s distress displayed more empathic concern and less prosocial behavior. There was a trend-level correlation suggesting that children with higher levels of parent-reported empathic responding tended to show more observed empathic concern. These correlations were similar in magnitude when examined when children in the ASD group were removed from the sample (see Table 3), although personal distress and empathic concern were no longer correlated in the reduced sample, indicating that inclusion of the ASD group was central to this association.
Table 3.
Correlations among study variables
| Variable | EC | PB | PD | PR |
|---|---|---|---|---|
| Entire sample | ||||
| Empathic concern (EC) | — | .17 | .25* | .24† |
| Prosocial behavior (PB) | — | −.42** | .14 | |
| Personal distress (PD) | — | −.04 | ||
| Parent report (PR) | — | |||
| Age | .19 | .03 | .05 | .15 |
| Full Scale IQ | −.09 | −.16 | .23† | .26* |
|
| ||||
| No ASD only | ||||
| EC | — | .21 | .13 | .26† |
| PB | — | −.46** | .16 | |
| PD | — | −.14 | ||
| PR | — | |||
| Age | .16 | .04 | .01 | .13 |
| Full Scale IQ | −.15 | −.17 | .19 | .11 |
Note.
p < .10,
p < .05,
p < .01.
N = 70-74 for observed variables and N = 62-66 for parent report (entire sample). N = 63-64 for observed variables and N = 55 for parent report in (no ASD only).
Associations between child age and IQ, and empathic responding variables were also assessed. There were no significant correlations between child age and empathic responding variables regardless of inclusion of the ASD group (see Table 3); age was not included in further analyses. Children with higher IQs had higher reported empathic responding and tended to show more personal distress. Thus, IQ was included as a covariate in subsequent analyses. One-way ANOVAs were conducted to assess gender differences in empathic responding (see Table 4), none of which reached significance (empathic concern: F(1, 71) = 3.18, p = .08; prosocial behavior: F(1, 72) = .00, p = .98; personal distress: F(1, 72) = .85, p = .36; parent report: F(1, 64) = 1.74, p = .19). Given the lack of gender differences in measures of empathic responding and ASD outcome groups, gender was not included in subsequent analyses1.
Table 4.
Descriptive information by gender and ASD outcome
| Empathic responding variable M (SD) | Male | Female | |
|---|---|---|---|
| Empathic concern | 2.19 (.98) | 2.60 (.97) | |
| Prosocial behavior | 2.65 (1.07) | 2.65 (1.28) | |
| Personal distress | 2.09 (1.07) | 2.32 (1.05) | |
| Parent report | 4.83 (.89) | 5.12 (.81) | |
|
| |||
| Empathic responding variable EMM* (SE) | Low risk/no ASD | High risk/no ASD | ASD |
|
| |||
| Empathic concern | 2.42 (.19) | 2.51 (.17) | 1.69 (.32) |
| Prosocial behavior | 2.44 (.22) | 2.78 (.20) | 2.70 (.37) |
| Personal distress | 2.50 (.19)a | 2.28 (.17)a | 1.39 (.32)b |
| Parent report | 4.66 (.16)b | 5.33 (.14)a | 4.76 (.28)ab |
Note.
EMM = Estimated marginal means after adjusting for IQ. Parent report is the Empathy and Prosocial Response scale from Conscience Questionnaire (Kochanska et al., 1994). ASD = autism spectrum disorder. Groups with different superscripts significantly differ at p = .017 level (Bonferroni-corrected).
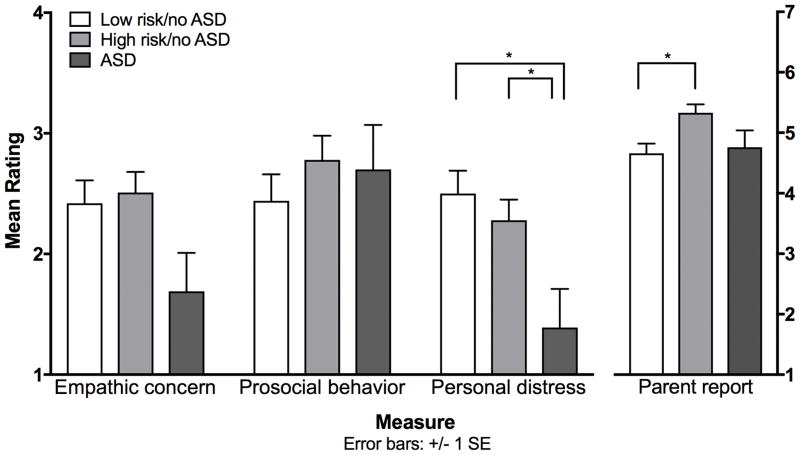
ANCOVA models assessed ASD outcome group differences on the four outcome measures while covarying IQ (see Figure 1 and Table 4). Differences in empathic concern by ASD outcome group did not reach significance, F(2, 66) = 2.72, p = .07, partial η2 = .08. Likewise, there was no difference in prosocial behavior between ASD outcome groups, F(2, 67) = .67, p = .52, partial η2 = .02.
Figure 1.
* Significant difference between groups in post hoc analyses (Bonferroni-corrected p = .017), following significant ANCOVA model. Empathic concern, personal distress, and prosocial behavior were rated on a 1–4 scale based on observed behavioral responses to an examiner’s accident. The parent report was the Empathy/Prosocial Response subscale from the Conscience Questionnaire (Kochanska et al., 1994). Parents rated children’s behaviors on a 1–7 scale. Estimated marginal means and standard errors (controlling for IQ) are presented.
There was a difference in personal distress2 based on ASD outcome, F(2, 67) = 4.24, p < .05, partial η2 = .11. The ASD group showed less personal distress than the low risk/no ASD group, F(1, 67) = 8.35, p = .005, and the high risk/no ASD group, F(1, 67) = 6.00, p = .017, while the high risk/no ASD and low risk groups did not differ, F(1, 67) = .72, p = .40. Parent-reported empathic responding differed by ASD outcome, F(2, 59) = 5.48, p < .01, partial η2 = .16. The high risk/no ASD group had higher levels of empathic responding than the low risk group, F(1, 59) = 9.73, p = .003. The ASD group did not differ from the high risk/no ASD group, F(1, 59) = 3.24, p = .08, or the low risk/no ASD group, F(1, 59) = .09, p = .77.
Pearson’s correlations quantifying zero-order associations between empathic responding and ADOS SA-CSS and RRB-CSS within the high risk group are presented in Table 5. SA-CSS was moderately negatively correlated with observed empathic concern and personal distress, as well as parent-reported empathic responding. RRB-CSS was negatively correlated only with personal distress.
Table 5.
Correlations between ADOS severity and empathic responding variables
| Variable | Empathic concern | Prosocial behavior | Personal distress | Parent report |
|---|---|---|---|---|
| ADOS severity | ||||
| SA-CSS | −.39** | −.07 | −.41** | −.41* |
| RRB-CSS | −.17 | −.04 | −.29* | −.31† |
Note.
p < .10,
p < .05,
p < .01.
Correlations included only children with familial risk for autism. ADOS = Autism Diagnostic Observation Schedule. SA = Social Affect. RRB = Restricted, Repetitive Behaviors. CSS = Calibrated Severity Scores. Observed variables n = 45, parent report n = 39.
We further assessed the relationship between empathic responding and ADOS severity scores in regressions controlling for IQ. A model predicting SA-CSS from observed empathic responding variables was significant, F(4, 38) = 3.87, p = .01, R2 = .29; in this model, empathic concern significantly predicted SA-CSS, β = −.32, p = .04. The model predicting RRB-CSS from observed empathy was not significant, F(4, 38) = 1.24, p = .31, R2 = .12, nor was the model predicting RRB-CSS from parent-reported empathic responding, F(2, 34) = 3.15, p = .06, R2 = .16. The overall model predicting SA-CSS from parent-reported empathic responding was significant, F(2, 34) = 6.64, p < .01, R2 = .28. However, when controlling for IQ, β = −.47, p < .01, parent report ratings were no longer associated with SA-CSS, β = −.12, p = .47.
Discussion
The current study examined observed and parent-reported empathic responding in 4- to 6-year-old children with familial risk for ASD, with and without ASD outcomes, as well as low-risk siblings. Both high-risk and low-risk siblings without ASD displayed more personal distress in response to an examiner’s distress than children with ASD. Strikingly, high-risk siblings without ASD were reported by their parents to show higher levels of empathic responding than the low-risk children, while the ASD group did not differ from either group in their level of parent-reported empathic responding. Within the high-risk sibling group, level of observed empathic concern was the strongest predictor of children’s Social Affect symptoms on the ADOS, although this variable did not significantly differentiate the ASD outcome groups. There was no evidence of an association between prosocial behavior and ASD outcome or symptoms. In sum, children with ASD showed a lack of emotional responsiveness but adequate helping behavior, while high-risk siblings without significant ASD symptomatology were unimpaired.
The finding that early deficits in emotional responsiveness to distress in high-risk siblings with ASD persist into preschool age supplements previous studies of high-risk siblings during the first years of life (Hutman et al., 2010; McDonald & Messinger, 2012). As in past studies, empathy deficits were specific to ASD outcome and not familial risk status, indicating a lack of support for the involvement of (emotional) empathy deficits in the BAP. In fact, parents in this study reported higher levels of empathic responding in high-risk siblings without ASD than in low-risk siblings. Additionally, higher levels of observed and parent-reported empathic responding were associated with fewer social-communication deficits. Our findings are consistent with a separate early school-age follow-up study of high-risk siblings indicating a lack of significant difference in parent-reported affective empathy abilities, and non-significantly higher mean scores in the high-risk siblings without ASD vs. the ASD and low risk groups (Tsang et al., 2016).
It is possible that an increased capacity for empathy has a protective effect in children who did not develop ASD despite elevated familial risk, or that these children may have learned to show more empathy toward others because of experience with their affected siblings. Alternately, parent perception may play a role. For example, parents of high-risk siblings without ASD may perceive their child without ASD as more empathic because of implicit comparisons with the older sibling with ASD. Similarly, parents of two children with ASD may have favorably compared their younger child with ASD to an older, more affected child, which may, in part, explain why ratings of children with ASD were similar to those of low-risk children. The lack of difference in parent-reported empathic responding between the ASD and non-ASD groups may also reflect the limited inclusion of cognitive aspects of empathy in our parent report measure, the area in which deficits were most evident in previous studies examining parent-reported empathy in children with ASD (e.g., Tsang et al., 2016).
Results from this study contribute to the literature on empathic responding in preschool-aged children with ASD. Children with ASD showed different patterns of responses to an examiner’s accident than children without ASD. Specifically, children with ASD showed less personal distress than high-risk and low-risk siblings without ASD. ASD outcome group differences in empathic concern did not reach significance, although empathic concern proved the strongest predictor of ADOS Social Affect scores in high-risk siblings. Together, these results indicate that children with higher levels of ASD symptoms, as indicated by both ASD diagnosis and more severe social-communication deficits, show less emotional responsiveness to an examiner’s distress. The low levels of apparent personal distress in the children with ASD and the association between ASD symptoms and empathic concern are consistent with previous literature showing lower physiological responsiveness (Corona et al., 1998) and reduced attention and facial affect (Sigman et al., 1992) in response to adult distress in children with ASD. It was somewhat unexpected that personal distress, which is considered a less developmentally mature response to distress, best differentiated the groups. The observational measure of empathy occurred in a fairly unfamiliar lab space with a relatively unfamiliar adult. It is possible that the unfamiliarity of the situation may have differentially elicited initial anxiety or wariness in some of the non-ASD children, which they were then able to regulate to subsequently express concern or provide help.
Although ASD-related deficits in the emotional aspects of empathic responding were evident, children with ASD were as likely to provide help to an unfamiliar adult as children without ASD. This is consistent with earlier work in high-risk siblings (McDonald & Messinger, 2012) and previous studies in children with ASD (Deschamps et al., 2014; Liebal et al., 2008), suggesting that empathic responding deficits in ASD may not be as pervasive as was once believed. These findings are in contrast with evolutionary arguments that empathy is the primary mechanism for motivating prosocial and altruistic behavior (de Waal, 2008), suggesting the possibility of a different mechanism for motivating prosocial behavior in children with ASD. Motivation for the prosocial behavior of the children with ASD may have instead come from a belief in a sense of fairness or learned responding.
Inter-correlations among empathic responding variables indicated that parent-reported empathic responding was marginally associated with empathic concern, indicating that the questionnaire may have most closely reflected individual differences in behaviors signifying concern for others. Observed empathic concern was also positively associated with personal distress, although this association was no longer significant when children with ASD were removed from the sample. This pattern of findings suggests that the children with ASD may have had an outsized effect on the correlation between personal distress and empathic concern. For children with ASD, personal distress may have been a signal that they were emotionally affected by the examiner’s distress, which then may have motivated a display of empathic concern.
With regard to prosocial behavior, a negative correlation between prosocial behavior and personal distress was observed, which was unsurprising as high levels of personal distress are thought to interfere with helping behavior (Eisenberg et al., 2010). The lack of correlation between empathic responding and prosocial behavior was not expected (e.g., Eisenberg et al, 2010). Research suggests, however, that not all types of prosocial behavior are associated with empathy (e.g., Carlo & Randall, 2002). While it is possible that helping behavior measured by the current task was not motivated by empathic concern, the lack of significant correlation may have been due to limited power.
Study limitations impact the interpretation of these findings and suggest avenues for future research. Although overall sample size was moderate, there were relatively few children with ASD outcomes (n = 12); thus, the null findings reported with respect to the ASD sample in this study must be considered with caution and may not generalize to the broader population of children with ASD. In particular, for observed empathic concern, the small ASD group size may have limited our power to detect a significant group difference, given the trend toward lower ratings for the children with ASD (p = .07). Further, while we included a parent report and observational measure of empathic responding, it would be informative if future research examined children’s responses to a range of social partners, including peers, as well as empathy-inducing situations. Along these lines, the addition of a specific measure of cognitive empathy would have allowed for a clearer comparison with previous studies (e.g., Deschamps et al., 2014; Tsang et al., 2016). This study also did not include physiological measures that would provide information on children’s internal responses to distress.
The current study provides a detailed examination of empathic responding, including parent report and an analysis of different components of empathy-related behavioral responses. This analysis indicated areas of deficit (i.e., emotional responsiveness) and areas of relative strength (i.e., helping behavior) associated with ASD outcome and symptoms. The unique sample, children with familial risk for ASD, also allowed us to investigate whether high-risk siblings without ASD showed evidence of (lower-level) empathy deficits related to the broader autism phenotype. We did not find such deficits. Rather, high-risk siblings without ASD showed evidence of comparable (or even higher) levels of empathy as low-risk children. This finding, together with evidence that empathy deficits precede diagnosis and predict the severity of later autism symptoms in high-risk siblings (Hutman et al., 2010; McDonald & Messinger, 2012) suggests that empathy may be protective in high-risk siblings. Our findings highlight the importance of examining children’s empathic responding as a multi-dimensional construct when examining individual differences and support empathic responding as a therapeutic target in children at risk for ASD.
Acknowledgments
Grant sponsor NICHD; Grant numbers: R01 HD047417 & R01 HD057284.
Grant sponsor NIGMS; Grant number: R01 GM105004.
The research reported in this article was supported by grants from the National Institute of Child Health and Development (R01HD057284 & R01HD047417), the National Institute of General Medical Sciences (R01GM105004), and the Marino Autism Research Institute. We thank the families who participated in this research.
The authors do not have any conflicts of interest associated with this study.
Footnotes
Including gender in an ANCOVA analysis of empathic concern yielded results equivalent to the reported analysis without gender.
Levene’s test (p = .047) for the personal distress variable, indicated differences in error variances between groups. Non-parametric tests confirmed differences in personal distress between groups (Kruskal-Wallis Test, p = .009).
Contributor Information
Nicole M. McDonald, UCLA Semel Institute of Neuroscience and Human Behavior, David Geffen School of Medicine, 760 Westwood Plaza, Suite 68-237, Los Angeles, CA 90095
Haley G. Murphy, Virginia Polytechnic Institute and State University, Department of Psychology, 109 Williams Hall, Blacksburg, VA 24061
Daniel S. Messinger, University of Miami, Departments of Psychology, Pediatrics, Electrical & Computer Engineering, and Music Engineering, 5665 Ponce de Leon Blvd., Coral Gables, FL 33146
References
- American Psychiatric Association. DSM-IV-TR: Diagnostic and statistical manual of mental disorders, text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Bacon AL, Fein D, Morris R, Waterhouse L, Allen D. The responses of autistic children to the distress of others. Journal of Autism and Developmental Disorders. 1998;28:129–142. doi: 10.1023/a:1026040615628. [DOI] [PubMed] [Google Scholar]
- Batson CD, Fultz J, Schoenrade PA. Distress and empathy: Two qualitatively distinct vicarious emotions with different motivational consequences. Journal of Personality. 1987;55:19–39. doi: 10.1111/j.1467-6494.1987.tb00426.x. [DOI] [PubMed] [Google Scholar]
- Carlo G, Randall BA. The development of a measure of prosocial behaviors for late adolescents. Journal of Youth and Adolescence. 2002;31:31–44. [Google Scholar]
- Coplan RJ, Arbeau KA. Peer interactions and play in early childhood. In: Rubin KH, Bukkowski B, Laursen B, editors. Handbook of peer interactions, relationships, and groups. New York, NY: Guilford Press; 2009. pp. 143–161. [Google Scholar]
- Corona R, Dissanayake C, Arbelle S, Wellington P, Sigman M. Is affect aversive to young children with autism? Behavioral and cardiac responses to experimenter distress. Child Development. 1998;69:1494–1502. [PubMed] [Google Scholar]
- Dawson G, Toth K, Abbott R, Osterling J, Munson J, Estes A, Liaw J. Early social attention impairments in autism: Social orienting, joint attention, and attention to distress. Developmental Psychology. 2004;40:271–283. doi: 10.1037/0012-1649.40.2.271. [DOI] [PubMed] [Google Scholar]
- Denham SA, Blair KA, DeMulder E, Levitas J, Sawyer K, Auerbach–Major S, Queenan P. Preschool emotional competence: Pathway to social competence? Child Development. 2003;74:238–256. doi: 10.1111/1467-8624.00533. [DOI] [PubMed] [Google Scholar]
- Deschamps PK, Been M, Matthys W. Empathy and empathy induced prosocial behavior in 6-and 7-year-olds with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2014;44:1749–1758. doi: 10.1007/s10803-014-2048-3. [DOI] [PubMed] [Google Scholar]
- De Waal FB. Putting the altruism back into altruism: The evolution of empathy. Annual Review of Psychology. 2008;59:279–300. doi: 10.1146/annurev.psych.59.103006.093625. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Eggum ND. Empathic responding: Sympathy and personal distress. In: Decety J, Ickes W, editors. The social neuroscience of empathy. Cambridge, MA: The MIT Press; 2009. [Google Scholar]
- Eisenberg N, Eggum ND, Giunta LD. Empathy-related responding: Associations with prosocial behavior, aggression, and intergroup relations. Social Issues Policy Review. 2010;4:143–180. doi: 10.1111/j.1751-2409.2010.01020.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Murphy B, Karbon M, Smith M, Maszk P. The relations of children’s dispositional empathy-related responding to their emotionality, regulation, and social functioning. Developmental Psychology. 1996;32:195–209. [Google Scholar]
- Eisenberg N, Fabes RA, Spinrad A. Prosocial development. In: Damon W, Eisenberg N, editors. Handbook of child psychology. New York: Wiley; 2006. pp. 646–718. [Google Scholar]
- Grove R, Baillie A, Allison C, Baron-Cohen S, Hoekstra RA. The latent structure of cognitive and emotional empathy in individuals with autism, first-degree relatives and typical individuals. Molecular Autism. 2014;5:42. doi: 10.1186/2040-2392-5-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutman T, Rozga A, DeLaurentis AD, Barnwell JM, Sugar CA, Sigman M. Response to distress in infants at risk for autism: A prospective longitudinal study. Journal of Child Psychology and Psychiatry. 2010;51:1010–1020. doi: 10.1111/j.1469-7610.2010.02270.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hus V, Gotham K, Lord C. Standardizing ADOS domain scores: Separating severity of social affect and restricted and repetitive behaviors. Journal of Autism and Developmental Disorders. 2014;44:2400–2412. doi: 10.1007/s10803-012-1719-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanska G, DeVet K, Goldman M, Murray K, Putnam SP. Maternal reports of conscience development and temperament in young children. Child Development. 1994;65:852–868. [PubMed] [Google Scholar]
- Liebal K, Colombi C, Rogers SJ, Warneken F, Tomasello M. Helping and cooperation in children with autism. Journal of Autism and Developmental Disorders. 2008;38:224–238. doi: 10.1007/s10803-007-0381-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Jr, Leventhal BL, DiLavore PC, et al. The Autism Diagnostic Observation Schedule—Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders. 2000;30:205–223. [PubMed] [Google Scholar]
- Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- McDonald NM, Messinger DS. Empathic responding in toddlers at risk for an autism spectrum disorder. Journal of Autism and Developmental Disorders. 2012;42:1566–1573. doi: 10.1007/s10803-011-1390-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piven J. The broad autism phenotype: a complementary strategy for molecular genetic studies of autism. American Journal of Human Genetics. 2001;105:34–35. [PubMed] [Google Scholar]
- Sagi A, Hoffman ML. Empathic distress in the newborn. Developmental Psychology. 1976;12:175–176. [Google Scholar]
- Sigman MD, Kasari C, Kwon JH, Yirmiya N. Responses to the negative emotions of others by autistic, mentally retarded, and normal children. Child Development. 1992;63:796–807. [PubMed] [Google Scholar]
- Scheeren AM, Koot HM, Mundy PC, Mous L, Begeer S. Empathic responsiveness of children and adolescents with high-functioning autism spectrum disorder. Autism Research. 2013;6:362–371. doi: 10.1002/aur.1299. [DOI] [PubMed] [Google Scholar]
- Svetlova M, Nichols SR, Brownell CA. Toddlers’ prosocial behavior: From instrumental to empathic to altruistic helping. Child Development. 2010;81:1814–1827. doi: 10.1111/j.1467-8624.2010.01512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsang T, Gillespie-Lynch K, Hutman T. Theory of mind indexes the broader autism phenotype in siblings of children with autism at school age. Autism Research and Treatment. 2016;2016:1–13. doi: 10.1155/2016/6309189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. The Wechsler Preschool and Primary Scale of Intelligence, Third Edition (WPPSI-III) San Antonio, TX: The Psychological Corporation; 2002. [Google Scholar]
- Wellman HM, Cross D, Watson J. Meta-analysis of theory-of-mind development: the truth about false belief. Child Development. 2001;72:655–684. doi: 10.1111/1467-8624.00304. [DOI] [PubMed] [Google Scholar]
- Young SK, Fox NA, Zahn-Waxler C. The relations between temperament and empathy in 2-year-olds. Developmental Psychology. 1999;35:1189–1197. doi: 10.1037//0012-1649.35.5.1189. [DOI] [PubMed] [Google Scholar]
- Zahn-Waxler C, Radke-Yarrow M, Wagner E, Chapman M. Development of concern for others. Developmental Psychology. 1992;28:126–136. [Google Scholar]
- Zhou Q, Eisenberg N, Losoya SH, Fabes RA, Reiser M, Guthrie IK, et al. The relations of parental warmth and positive expressiveness to children’s empathy-related responding and social functioning: A longitudinal study. Child Development. 2002;73:893–915. doi: 10.1111/1467-8624.00446. [DOI] [PubMed] [Google Scholar]