ABSTRACT
Clinical outcomes of melioidosis patients improve when the infecting agent, Burkholderia pseudomallei, is rapidly detected and identified by laboratory testing. Detection of B. pseudomallei DNA or recovery of the pathogen by culture from urine can support a diagnosis of melioidosis and guide patient care. Two new methods, designated filter-capture DNA isolation (FCDI) and filter cellular recovery (FCR), were developed to increase the sensitivity of detection and recovery of viable B. pseudomallei cells from small volumes (0.45 ml) of urine. DNA from eight strains of B. pseudomallei that were spiked into synthetic urine at low concentrations (1 × 102 CFU/ml) was detected in FCDI cell lysates using real-time PCR with greater consistency than with preparations from a QIAamp DNA Blood minikit. The FCR method showed greater B. pseudomallei detection sensitivity than conventional urine culture methods and resulted in typical colony growth at 24 h from as few as 1 × 102 CFU/ml. In addition, the FCR method does not rely on precipitation of a urine pellet by centrifugation and requires a smaller volume of urine. The FCDI and FCR methods described here could improve time-to-results and decrease the number of negative B. pseudomallei reports that are currently observed from urine culture as a consequence of samples containing low or variable bacterial cell concentrations.
KEYWORDS: melioidosis, urine, detection, Burkholderia pseudomallei
INTRODUCTION
Melioidosis is an infectious disease with a high case fatality rate in humans that is caused by the Gram-negative, soil-dwelling bacterium Burkholderia pseudomallei (1–5). Common to Southeast Asia and northern Australia, melioidosis is recognized as endemic in 48 equatorial-zone nations (6, 7). A 2015 study suggests that melioidosis cases are underreported in regions of endemicity and estimates that 165,000 cases occur annually, leading to 89,000 deaths (6). As a result of global travel, melioidosis can also be diagnosed in regions where it is not endemic. A recent review by Michael Dan indicates that 72 melioidosis cases in travelers returning from regions of endemicity were reported in the literature through July 2015 (8).
Although healthy individuals infected by B. pseudomallei may develop melioidosis, most patients have established risk factors such as diabetes, alcoholism, renal disease, or frequent exposure to stagnant water (9). Clinical manifestations of melioidosis can result in acute or chronic infections with diverse disease presentations that severely hinder diagnosis and may delay appropriate treatment (10). Prompt detection of B. pseudomallei and administration of effective antimicrobial therapy can improve patient outcomes, with significant reductions in mortality rates (2, 11–16).
Laboratory culture with isolation of B. pseudomallei is considered the gold standard for diagnosis of melioidosis. Blood, urine, pus, and throat swabs are useful human sample types for laboratory analysis and accurate diagnosis (13, 17–19). A broad range of B. pseudomallei cell concentrations has been reported in each specimen type (18, 19). Recovery of B. pseudomallei from human clinical specimens is challenging. Ashdown's (ASH) is a selective medium that improves detection of B. pseudomallei by mitigating the overgrowth of normal microbiota found in human clinical specimens (20–25). Certain clinical sample types such as swabs from pus or skin lesions are not routinely collected for diagnosis of melioidosis, and other sample types may not be collected at adequate volumes for reliable B. pseudomallei detection (26).
Urine culture is an inexpensive conventional laboratory diagnostic method but can require 3 to 7 days of processing and incubation (21). The isolation of a single colony of B. pseudomallei from the urine of a suspected melioidosis patient is sufficient for laboratory confirmation since this organism is not a member of the human commensal microbiota (27, 28). In a 10-year investigation, Limmathurotsakul et al. estimated that 28% of confirmed melioidosis cases were positive for B. pseudomallei by conventional urine culture. When urine cultures were negative, a 39% death rate was observed, and the death rate increased to 58% when bacteria were cultured from a pellet (<103 CFU/ml) formed by centrifugation of the urine sample (27). These observations highlight (i) the importance of developing highly sensitive laboratory detection methods for this pathogen and (ii) the difficulty in reliably detecting low cell concentrations of B. pseudomallei in urine from melioidosis patients.
Real-time PCR detection of the type III secretion system (TTS1) is considered a reliable, DNA-based, species-specific laboratory assay for rapid identification of B. pseudomallei (29–31). This method has been routinely performed using DNA prepared by the commercially available QIAamp DNA Blood minikit (Qiagen, Hilden, Germany) (26, 29). Other laboratory assays have been described for the rapid detection and identification of B. pseudomallei from urine specimens (29, 32–34). Houghton et al. recently developed and described the Active Melioidosis Detect (AMD) lateral flow immunoassay (LFI) as a point-of-care test for the detection of capsular polysaccharide (CPS) of B. pseudomallei and Burkholderia mallei directly from clinical specimens, with a sensitivity of ∼2.3 × 104 CFU/ml from melioidosis urine samples (33). When a urine sample contains low concentrations of a bacterial pathogen(s), concentrating the sample by centrifugation or filtration can improve laboratory detection by culture and alternative methods. These approaches can improve detection but often require diligent pellet isolation, a lengthy enrichment period, large minimum sample volumes, and/or specialized laboratory equipment (32, 34–38).
Here, we describe two filtration-based laboratory methods for the sensitive detection of B. pseudomallei using relatively small volumes of synthetic urine: filter capture DNA isolation (FCDI) for B. pseudomallei DNA preparation and filter cellular recovery (FCR) for culture of viable B. pseudomallei cells. Sterile synthetic urine was used throughout this proof-of-principle investigation as a diluent for all cell suspensions to eliminate the potential bias introduced by variability between human urine specimens. We compared the new FCDI method to the QIAamp DNA Blood minikit (here, QIAamp) and evaluated FCDI for detection of low, clinically relevant concentrations of wild-type B. pseudomallei strains spiked into synthetic urine. Finally, the new FCR method was compared to conventional methods for the culture detection of viable B. pseudomallei from urine.
RESULTS
Comparison of FCDI and QIAamp methods for preparation of B. pseudomallei Bp82 DNA template detection by real-time PCR.
Bp82 DNA isolated by the QIAamp method was detected in 5/5 real-time PCRs for each of the five total Bp82 cell concentrations in synthetic urine (from 5.7 × 107 to 5.7 × 103 CFU/ml), with an r2 value of 0.9865 (see Fig. S1 in the supplemental material). By the FCDI method, Bp82 DNA was detected in 5/5 real-time PCRs for each of six total Bp82 cell concentrations in synthetic urine (from 5.7 × 107 to 5.7 × 102 CFU/ml), with an r2 of 0.9952 (Fig. S2).
Comparison of the FCDI and QIAamp preparation methods for detection of B. pseudomallei DNA from two clinical strains spiked at low concentrations.
Based on the above results from experiments with Bp82, wild-type bacterial concentrations at ∼103 and ∼102 CFU/ml were used to further assess the FCDI and QIAamp methods. Bacterial cell counts were quantified for every experiment to ensure that the desired concentrations were achieved. Bacterial cell counts for strain 1162 spiked into synthetic urine at ∼103 CFU/ml were 1.09 × 103 CFU/ml for experiment one and 6.55 × 103 CFU/ml for experiment two. Bacterial cell counts for strain 1634 spiked at ∼103 CFU/ml were 7.35 × 103 CFU/ml for experiment one and 1.04 × 103 CFU/ml for experiment two. B. pseudomallei DNA in FCDI lysates was detected by real-time PCR at ∼103 and ∼102 CFU/ml for all replicates, or 24 of 24 lysates, in two independent experiments (Table 1). By the FCDI method, the range of real-time PCR cycle threshold (CT) values was 32.91 to 40.53 at ∼103 CFU/ml and 35.77 to 41.01 at ∼102 CFU/ml (Table 1). B. pseudomallei DNA was detected by real-time PCR in 10 of 12 QIAamp preparations at ∼103 CFU/ml and in 6 of 12 QIAamp preparations at ∼102 CFU/ml (Table 1). The CT values measured from QIAamp templates ranged from 34.90 to not detected (ND) at ∼103 CFU/ml and from 38.95 to ND at ∼102 CFU/ml (Table 1).
TABLE 1.
Comparison of real-time PCR results using FCDI and QIAamp DNA lysatesa
| Strain and method | Estimated concn in urine (CFU/ml)b | Experiment day | Observed PCR CT valuesc |
|---|---|---|---|
| Strain 1162 | |||
| QIAamp | ∼103 | 1 | 36.12, 37.62, 37.23 |
| 2 | 34.90, 34.98, 36.71 | ||
| ∼102 | 1 | ND, ND, 41.26 | |
| 2 | 39.15, 38.95, 39.42 | ||
| FCDI | ∼103 | 1 | 33.98, 33.64, 32.91 |
| 2 | 33.47, 33.79, 33.68 | ||
| ∼102 | 1 | 38.18, 36.60, 36.82 | |
| 2 | 35.77, 36.82, 36.47 | ||
| Strain 1634 | |||
| QIAamp | ∼103 | 1 | 36.89, 37.21, 37.78 |
| 2 | ND, ND, 40.03 | ||
| ∼102 | 1 | ND, 40.13, 40.65 | |
| 2 | ND, ND, ND | ||
| FCDI | ∼103 | 1 | 40.53, 35.58, 36.43 |
| 2 | 36.03, 36.95, 37.01 | ||
| ∼102 | 1 | 38.90, 40.66, 38.36 | |
| 2 | 38.42, 37.66, 41.01 |
Lysates were from two clinical isolates of B. pseudomallei spiked in synthetic urine. Triplicate lysates were prepared and tested on 2 days.
Actual plate count values are given in Results.
Values are from three lysates. ND, not detected (>45 cycles).
Real-time PCR detection of B. pseudomallei DNA in cell lysates prepared by the FCDI method from six wild-type strains spiked at low cell concentrations in synthetic urine.
Bacterial cell counts for strains 1618, 1620, 1623, 1625, 1626, and 1628 at ∼103 CFU/ml were 7.8 × 103, 5.9 × 103, 5.5 × 103, 5.5 × 103, 9.3 × 103, and 1.1 × 103 CFU/ml, respectively. B. pseudomallei DNA was detected at ∼103 CFU/ml for all six strains or from 12 of 12 FCDI lysates in duplicate preparations (Table 2). In synthetic urine spiked at the lower dilution of ∼102 CFU/ml, B. pseudomallei DNA was detected by real-time PCR for all FCDI lysate preps with the exception of one strain. Strain 1618 was detected in only one of the two FCDI lysates at ∼102 CFU/ml. The observed CT values for the six wild-type B. pseudomallei strains at ∼103 CFU/ml ranged from 32.84 to 38.10 and from 35.07 to ND at the lower dilution of ∼102 CFU/ml (Table 2).
TABLE 2.
Detection of six wild-type B. pseudomallei strains spiked at low concentrations in synthetic urine using the FCDI method DNA lysates by real-time PCR
| Estimated concn in urine (CFU/ml)a | Strain | Observed PCR CT valuesb |
|---|---|---|
| ∼103 | 1618 | 37.10, 34.51 |
| 1620 | 33.02, 33.00 | |
| 1623 | 34.68, 33.12 | |
| 1625 | 33.43, 32.84 | |
| 1626 | 35.12, 33.58 | |
| 1628 | 38.10, 36.33 | |
| ∼102 | 1618 | ND, 38.06 |
| 1620 | 37.06, 36.81 | |
| 1623 | 38.10, 36.33 | |
| 1625 | 38.37, 35.07 | |
| 1626 | 37.32, 36.05 | |
| 1628 | 40.18, 39.53 |
Actual plate count values are given in Results.
Values are from lysates prepared in duplicate. ND, not detected (>45 cycles).
Comparison of FCR and conventional urine culture methods for the recovery of viable B. pseudomallei using two clinical isolates, each spiked into synthetic urine at low cell concentrations.
In two independent experiments, the B. pseudomallei FCR and conventional urine culture methods were compared using the same cell suspensions of strains 1162 and 1634 that were prepared in synthetic urine for the real-time PCR detection experiments at ∼103 and ∼102 CFU/ml. For all experiments and with both strains, the FCR method resulted in colony growth from these clinical B. pseudomallei strains after 24 h of incubation on ASH agar (Table 3). In contrast, at ∼103 and ∼102 CFU/ml of strains 1162 and 1634, conventional cultures using a 1-μl loopful of synthetic urine resulted in colony formation of B. pseudomallei in 3 of 8 samples for both strains on ASH agar and 1 of 8 samples on MacConkey (MAC) agar at 35 ± 2°C and required 48 h of incubation (Table 3). For both strains, the conventional culture method using the pellet from 2-ml volumes of each urine suspension resulted in B. pseudomallei colonies from 7 of 8 pellets at ∼103 and ∼102 CFU/ml on either ASH or MAC agar after incubation for 24 to 48 h at 35 ± 2°C (Table 3). For all conventional culture experiments on MAC and ASH agar, using either a 1-μl loopful of urine or urine pellet, no growth of B. pseudomallei was observed after 24 h of incubation (data not shown).
TABLE 3.
B. pseudomallei strains spiked at concentrations at and below 103 CFU/ml in synthetic urine using conventional urine culture methods and the FCR method in two independent experiments
| Strain and medium | Method | Incubation time (h) | Growth at the estimated concn of:a |
|||
|---|---|---|---|---|---|---|
| ∼103 CFU/ml |
∼102 CFU/ml |
|||||
| Expt no. 1 | Expt no. 2 | Expt no. 1 | Expt no. 2 | |||
| Strain 1162 | ||||||
| MAC agar | Conventional 1-μl loop | 48 | − | − | − | + |
| Conventional pellet | 48 | + | + | + | + | |
| ASH agar | Conventional 1-μl loop | 48 | − | + | − | + |
| Conventional pellet | 48 | + | + | + | + | |
| FCR | 24 | + | + | + | + | |
| Strain 1634 | ||||||
| MAC agar | Conventional 1-μl loop | 48 | − | − | − | − |
| Conventional pellet | 48 | + | + | + | − | |
| ASH agar | Conventional 1-μl loop | 48 | + | − | − | − |
| Conventional pellet | 48 | + | + | + | − | |
| FCR | 24 | + | + | + | + | |
Actual plate count values are given in Results. +, growth; −, no growth.
DISCUSSION
A direct relationship between melioidosis mortality rates and bacterial concentrations has been reported from previous studies where B. pseudomallei was cultured directly from urine (27). While human urine is recognized as a sample type that is useful for B. pseudomallei detection, the recovery of B. pseudomallei from urine at concentrations below 103 CFU/ml is inconsistent and unreliable (27). Rapid and accurate laboratory detection of B. pseudomallei is critical to support a melioidosis diagnosis and guide patient care. The FCDI method generated lysates from synthetic urine in which B. pseudomallei was consistently detected by real-time PCR over a broad range of concentrations, including detection below 103 CFU/ml. The FCDI method showed superior detection consistency compared to that of the QIAamp method since every FCDI DNA lysate was detected by real-time PCR from synthetic urine spiked with low (103 and 102 CFU/ml) B. pseudomallei concentrations. The FCDI method was finished in less than 0.5 h with minimal specialized laboratory equipment. In contrast, nearly 1 h of laboratory time was required to complete the QIAamp protocol as the method relied on enzymatic and chemical treatments, as well as an inactivation step at 56°C. The FCDI method with real-time PCR is a potential process for the rapid and sensitive detection of B. pseudomallei in presumptive melioidosis patients.
For laboratories with real-time PCR instruments, the FCDI method offers a rapid approach to the preparation of cell lysates for real-time PCR detection of B. pseudomallei at low concentrations. TTS1 real-time PCR is a validated method for species-specific detection of B. pseudomallei (29–31); BLAST alignments using publicly available genomes identified a single target per B. pseudomallei genome. The FCDI method was developed using commercially available spin filter columns with 0.1-μm-pore-size polyvinylidene difluoride (PVDF) membranes and common laboratory reagents. Minimal equipment beyond standard laboratory accessories, such as micropipettes, a microcentrifuge, and incubators set to 35 ± 2°C, are required. All reagents for FCDI are shelf stable at room temperature and have no enzyme components, so cold-chain storage is unnecessary. Also, less than 0.5 ml of patient urine is required to perform the FCDI method. Other processing methods for real-time PCR detection of B. pseudomallei from patient urine recommend centrifuging up to 10 ml of urine, collecting a pellet, and using commercial kits for DNA lysate preparation. Furthermore, most of these commercial DNA isolation kits require cold-chain storage of enzymes and reagents, include buffers containing chaotropic salts, and require heat incubation (26, 29, 34, 39).
Richardson et al. assessed DNA extraction methods for melioidosis clinical samples and found no statistically significant difference in B. pseudomallei detection by QIAamp/TTS1 real-time PCR from pellets of 5 to 10 ml of centrifuged urine (26). In the same study, B. pseudomallei DNA was detected in 19 of 41 samples collected from 30 culture-confirmed melioidosis patients, and the CT values ranged from 27.0 to 36.0 (26). The authors of the study could not confirm whether all 41 samples contained B. pseudomallei at the time of testing. Chantratita et al. centrifuged 10 ml of urine from suspected melioidosis patients, prepared DNA from the pellet using an automated extraction instrument, and reported detection of B. pseudomallei in only 6 of 8 urine culture-confirmed samples by TTS1 real-time PCR (34). Formation and isolation of a urine pellet by centrifugation are not required for the FCDI method since the B. pseudomallei cells are separated from the liquid urine sample by filtration, and the flowthrough is discarded (Fig. 1). Urea is a component of human urine and considered a major inhibitor in real-time PCRs due to polymerase degradation, which is initiated at concentrations as low as 50 mM (40). Urea concentrations in healthy human urine range from 245 to 267 mM (41); the synthetic urine reagent used in this study contained a higher urea concentration of approximately 316.4 mM.
FIG 1.
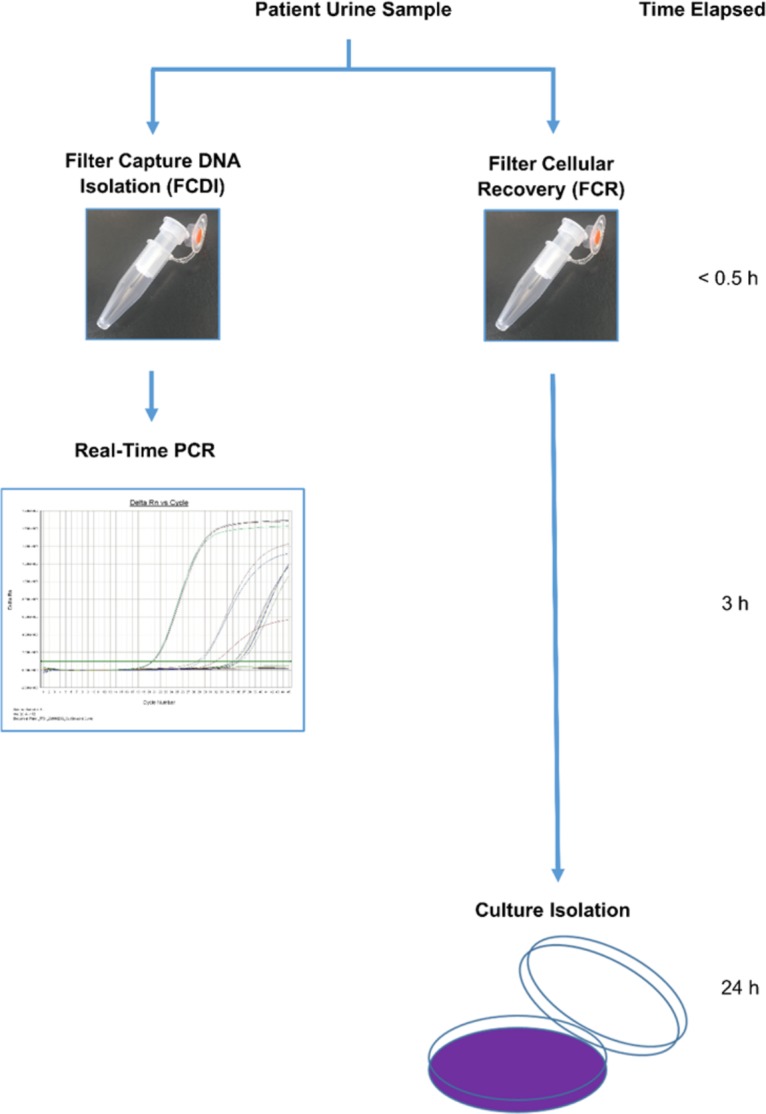
Laboratory time-to-results for real-time PCR and culture isolation of B. pseudomallei from a urine sample using the FCDI and FCR methods. Less than 1.5 ml of urine is required to perform both procedures.
We developed the FCR method to increase the recovery of viable B. pseudomallei cells at low concentrations for culture from a small volume of urine within 24 h. With a sensitivity comparable to that of conventional urine culture at 48 h, FCR is an alternative to conventional urine culture for detection of B. pseudomallei in half the time. For laboratories that rely on conventional urine culture methods and not DNA-based methods, the FCR method could improve the sensitivity and time-to-results for culture detection of B. pseudomallei. Other benefits of the FCR method are the minimal sample handling, low (<0.5 ml) sample volume requirement, and elimination of the need for careful isolation and manipulation of a urine pellet. When the FCR method is performed as described in this study (Fig. 1), evidence of low B. pseudomallei concentrations in urine from suspected melioidosis patients can be attained about 24 h sooner than with conventional urine culture. One reason for greater sensitivity and rapid recovery of B. pseudomallei by the FCR method is the potential reduction of urea by filtration. Urea has been noted as an inhibitor of bacterial growth (42, 43), and the FCR method relies on an initial filtration step that isolates bacterial cells from urine that could significantly reduce urea concentrations. Limmathurotsakul et al. reported lower rates of positivity with conventional urine culture from individuals with diabetes (27). The filtration step of the FCR method could increase culture sensitivity by reducing or eliminating culture-inhibiting factors in urine that are associated with diabetes.
For laboratories without access to real-time PCR, lysates generated by the FCDI method could be used to detect B. pseudomallei DNA by other lower-cost, DNA-based methods such as conventional PCR, loop-mediated isothermal amplification (LAMP), or methods that lack reagents requiring cold-chain storage, such as shelf-stable fluorogenic isothermal amplification (44). While laboratory detection by DNA-based methods is more rapid than conventional culture, additional steps are required for B. pseudomallei confirmation when access to this technology is not available. Antimicrobial susceptibility testing (AST) is commonly used in some areas of endemicity during B. pseudomallei identification (17) and was recently employed to characterize a rare isolate resistant to ceftazidime, imipenem, doxycycline, trimethoprim-sulfamethoxazole, and amoxicillin-clavulanic acid (45). The FCR and FCDI methods can be performed in parallel (Fig. 1) to provide an immediate presumptive result and to provide culture isolates for downstream characterization assays such as AST. Laser light scattering technology has been shown to significantly reduce time-to-results during B. pseudomallei AST (46); using this technology with viable B. pseudomallei recovered by FCR may improve melioidosis patient outcomes.
The FCDI and FCR methods demonstrated a robust approach to the detection of B. pseudomallei in synthetic urine with consistent sensitivity (≤1.0 × 103 CFU/ml) at clinically relevant concentrations (18, 27). While this may be a promising technology that can lead to improved patient outcomes through the rapid detection and recovery of B. pseudomallei from clinical urine specimens, urine collected from suspected melioidosis patients could contain factors that slow the recovery and detection of low concentrations of B. pseudomallei, so additional studies with actual human urine are necessary. High and variable PCR CT values (Tables 1 and 2) observed during assessment of FCDI sensitivity indicate that the method is approaching the limits of detection for B. pseudomallei. Additional evaluations of these assays to determine true limits of detection and the use of human urine and/or confirmed clinical melioidosis urine samples would strengthen the recommendation of FCDI and FCR as methods for melioidosis diagnosis.
MATERIALS AND METHODS
Biosafety.
All procedures involving virulent B. pseudomallei strains were performed in a class II type A2 biological safety cabinet located in a biosafety level 3 (BSL-3) laboratory registered with the U.S. Federal Select Agent Program. All procedures were performed by trained personnel wearing personal protective equipment, including protective laboratory clothing, and a powered air-purifying respirator.
Strains.
B. pseudomallei strain Bp82 is a select-agent-excluded, avirulent ΔpurM mutant of strain 1026b that is deficient in purine biosynthesis (47). Bp82 was used to compare the commercial QIAamp DNA Blood miniprep kit (Qiagen, Hilden, Germany) and the new FCDI method for DNA isolation from cell suspensions that were serially diluted in synthetic urine. B. pseudomallei strains 1162 and 1634, isolated previously from clinical human specimens (Table 4), were used to compare the QIAamp kit with the FCDI method and to compare the FCR method with conventional culture methods from spiked synthetic urine (Table 4). Six additional wild-type strains of B. pseudomallei, designated strains 1618, 1620, 1623, 1625, 1626, and 1628, were used to assess detection of B. pseudomallei DNA in FCDI lysates by real-time PCR (Table 4).
TABLE 4.
B. pseudomallei strains used in this study
| B. pseudomallei strain | Other identifiera | Origin | Source (sample type) | Yr of isolation | Reference |
|---|---|---|---|---|---|
| Bp82 | Derivative of 1026b | 2010 | 47 | ||
| 1618 | PHLS 14 | Philippines | Monkey (liver) | 1990 | 33 |
| 1620 | PHLS 24, 7641 | France | Horse (stool) | 1976 | 33 |
| 1623 | PHLS 92, 84-109 | Australia | Cow (spleen) | 1985 | 33 |
| 1625 | PHLS 19 | Singapore | Environment | 1991 | 33 |
| 1626 | PHLS 216 | Thailand | Environment | 1990 | 33 |
| 1628 | PHLS 25 | Madagascar | Environment (soil) | 1977 | 33 |
| 1162 | B7210 | Australia | Human | 1970 | 33 |
| 1634 | PHLS 112 | Thailand | Human | 1992 | 23 |
PHLS, Public Health Laboratory Service, London, United Kingdom.
Growth conditions and preparation of B. pseudomallei cell suspensions in synthetic urine.
For every spiking experiment, strains were cultured overnight in ambient air at 35 ± 2°C on tryptic soy agar with 5% sheep's blood (TSA II–5% SB) (Becton Dickinson, Franklin Lakes, NJ, USA) until isolated colonies were visible. For strain Bp82, all culture media were supplemented with 5 μg/ml adenine. For spiking experiments, bacterial cells from each strain were suspended in sterile synthetic urine (Ricca Chemical Company, Arlington, TX, USA). The bacterial suspensions were standardized to a turbidity equivalent of a 0.5 McFarland standard using a MicroScan turbidity meter (Siemens Healthcare, Erlangen, Germany). Tenfold serial dilutions of B. pseudomallei cell suspensions were prepared in sterile synthetic urine to compare DNA isolation methods and cell recovery by culture on agar medium. The composition of synthetic urine (pH 7.8 to 8.0) is described by the manufacturer as water (97.17%), urea (1.90%), sodium chloride (0.77%), magnesium sulfate heptahydrate (0.09%), and calcium chloride (0.06%). For every experiment, estimates in number of CFU/milliliter were determined for each strain by immediately spread plating the spiked synthetic urine directly onto TSA II–5% SB medium and enumerating growth after incubation overnight at 35 ± 2°C in ambient air.
Cell lysis by the FCDI method.
For each B. pseudomallei spiked synthetic urine suspension tested, 225 μl was used for the FCDI method. Before filtration, an equal volume (225 μl) of 4% Triton X-100 buffer (4% Triton X-100, 100 mM NaCl, 50 mM Tris-Cl, pH 7.5) was added to the spiked synthetic urine suspension and mixed gently by pipetting. The entire 450-μl mixture was transferred to an Ultrafree-MC spin filter column with a 0.1-μm-pore-size PVDF membrane (Millipore, Billerica, MA, USA) and centrifuged at 2,000 × g for 2 min to capture cells on the filter. All flowthrough was discarded. A 450-μl volume of a 2% Triton X-100 wash buffer (2% Triton X-100, 100 mM NaCl, 50 mM Tris-Cl, pH 7.5) was then added to the filter, and the filter unit was centrifuged at 2,000 × g for 2 min. After the flowthrough was discarded, an additional centrifugation step of 5,600 × g for 1 min was performed to remove residual buffer from the filter. To lyse B. pseudomallei cells captured on the filter, 65 μl of NaOH lysis buffer (0.05 N NaOH, 250 mM NaCl, 1 mM EDTA) was deposited onto the filter, and the spin column unit was incubated at 35 ± 2°C for 15 min. The filters were then centrifuged at 8,000 × g for 2 min, and the flowthrough lysate was collected. The lysates were immediately neutralized by the addition of 10 μl of 0.5 M Tris-Cl, pH 7.5. Lysates were stored at −20°C until used for real-time PCR.
B. pseudomallei DNA isolation by QIAamp.
B. pseudomallei DNA was isolated from 200-μl volumes of spiked synthetic urine according to the manufacturer's protocol (Qiagen) for “DNA Purification from Blood or Body Fluids (Spin Protocol)” (48) with the following modification: samples were incubated with 200 μl of buffer AL at 56°C for 15 min. DNA was eluted using 200 μl of buffer EB.
Real-time PCR.
B. pseudomallei DNA was detected using the DNA primer and probe sequences/concentrations from the TTS1 real-time PCR method described by Novak et al. (30). Real-time PCR was performed on an AB 7500 Fast DX real-time instrument (Life Technologies, Carlsbad, CA, USA) as follows: 5 μl of template (FCDI lysate or QIAamp DNA) was added to a 20-μl reaction mixture (25-μl final volume) of PerfeCTa Multiplex qPCR ToughMix Low ROX (Quantabio, Beverly, MA, USA) with 5 mM MgCl2. Thermocycling conditions consisted of 50°C for 2 min, 95°C for 10 min, and 45 cycles of 95°C for 15 s to 59°C for 1 min, performed in standard mode. All real-time PCR results generating a positive amplification curve with a cycle threshold (CT) value of <45 have been reported.
Comparison of the FCDI and QIAamp methods for detection of Bp82 by real-time PCR.
B. pseudomallei strain Bp82 was spiked and serially diluted to extinction into sterile synthetic urine. Cell lysate or DNA was prepared from each dilution by both the FCDI and QIAamp methods. Five independent samples were prepared from each 10-fold dilution using both methods. The sensitivity of Bp82 DNA detection was assessed by real-time PCR.
Comparison of the FCDI and QIAamp preparation methods with two clinical strains at low concentrations.
Two clinical strains of B. pseudomallei (strains 1162 and 1634) were each spiked into synthetic urine and then serially diluted to final concentrations of approximately 103 and 102 CFU/ml. For each suspension, both the FCDI and QIAamp methods were performed in triplicate in two independent experiments, and the sensitivity of DNA detection was measured using real-time PCR.
Real-time PCR detection of B. pseudomallei DNA in cell lysates prepared by the FCDI method from six wild-type strains.
Six wild-type B. pseudomallei strains were spiked into synthetic urine to concentrations of approximately 103 and 102 CFU/ml, and cell lysates were prepared by the FCDI method. B. pseudomallei detection sensitivity was assessed by real-time PCR.
Detection of B. pseudomallei by conventional urine culture.
Conventional B. pseudomallei urine culture was performed as previously described (18). Calibrated 1-μl disposable loops (Copan, Murrieta, CA, USA) were used to spread 1 μl of synthetic urine directly onto ASH and onto MacConkey (MAC) agar plates. Plates were incubated at 35 ± 2°C in ambient air and observed for growth after 24 and 48 h. In addition, a 2-ml volume of synthetic urine was centrifuged at 1,500 × g for 5 min, and 1.9 ml of clear supernatant was discarded. Each pellet was resuspended and inoculated onto ASH and MAC agar plates, which were incubated at 35 ± 2°C in ambient air and observed for growth after 48 h.
Isolation of B. pseudomallei cells using the FCR method from synthetic urine.
Ultrafree-MC spin filter columns with 0.1-μm-pore-size PVDF membranes were sterilized using an ethylene oxide gas treatment before use. For each B. pseudomallei-spiked synthetic urine suspension, 450 μl was applied to a spin filter column and centrifuged at 2,000 × g for 2 min in a microcentrifuge, and the flowthrough was discarded. To each filter column, 120 μl of sterile 0.85% physiological saline was added and mixed by gently pipetting up and down to resuspend cells. From the filter, 100 μl of each saline suspension was transferred and spread onto ASH agar, incubated in ambient air at 35 ± 2°C, and observed for growth after 24 and 48 h. Positive culture isolates were defined as the appearance of at least one colony.
Comparison of FCR and conventional urine culture methods for the recovery of viable B. pseudomallei using two clinical isolates spiked into synthetic urine at low cell concentrations.
In two independent experiments, the B. pseudomallei FCR and conventional urine culture methods were compared using the same cell suspensions of strains 1162 and 1634 diluted in synthetic urine for real-time PCR detection experiments at ∼103 and ∼102 CFU/ml. Observations for growth were made at 24 and 48 h. Culture detection was defined as the appearance of at least one colony with morphology consistent with that known for B. pseudomallei.
Verification of B. pseudomallei DNA and lysate sterility.
All DNA and cell lysate preparations were filtered through an Ultrafree-MC spin filter column with a 0.1-μm-pore-size PVDF membrane for 2 min at 8,000 × g in a microcentrifuge to remove any whole cells that might remain. DNA and cell lysates used for real-time PCR were verified as free of cultivatable B. pseudomallei cells by inoculating 10% of each final volume directly onto TSA II–5% SB. Growth was evaluated after 5 days of incubation at 35 ± 2°C in ambient air.
Supplementary Material
ACKNOWLEDGMENTS
We thank Alex R. Hoffmaster for technical advice during this study.
This work was supported in part by funds made available from the CDC Office for Public Health Preparedness and Response.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The mention of company names or products does not constitute endorsement by the CDC.
Footnotes
Supplemental material for this article may be found at https://doi.org/10.1128/JCM.00764-17.
REFERENCES
- 1.Sprague LD, Neubauer H. 2004. Melioidosis in animals: a review on epizootiology, diagnosis and clinical presentation. J Vet Med B Infect Dis Vet Public Health 51:305–320. doi: 10.1111/j.1439-0450.2004.00797.x. [DOI] [PubMed] [Google Scholar]
- 2.White NJ. 2003. Melioidosis. Lancet 361:1715–1722. doi: 10.1016/S0140-6736(03)13374-0. [DOI] [PubMed] [Google Scholar]
- 3.Cheng AC, Currie BJ. 2005. Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev 18:383–416. doi: 10.1128/CMR.18.2.383-416.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Currie BJ, Mayo M, Anstey NM, Donohoe P, Haase A, Kemp DJ. 2001. A cluster of melioidosis cases from an endemic region is clonal and is linked to the water supply using molecular typing of Burkholderia pseudomallei isolates. Am J Trop Med Hyg 65:177–179. doi: 10.4269/ajtmh.2001.65.177. [DOI] [PubMed] [Google Scholar]
- 5.Currie BJ, Jacups SP.. 2003. Intensity of rainfall and severity of melioidosis, Australia. Emerg Infect Dis 9:1538–1542. doi: 10.3201/eid0912.020750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Limmathurotsakul D, Golding N, Dance DA, Messina JP, Pigott DM, Moyes CL, Rolim DB, Bertherat E, Day NP, Peacock SJ, Hay SI. 2016. Predicted global distribution of Burkholderia pseudomallei and burden of melioidosis. Nat Microbiol 1:15008. doi: 10.1038/nmicrobiol.2015.8. [DOI] [PubMed] [Google Scholar]
- 7.Currie BJ, Kaestli M. 2016. Epidemiology: a global picture of melioidosis. Nature 529:290–291. doi: 10.1038/529290a. [DOI] [PubMed] [Google Scholar]
- 8.Dan M. 2015. Melioidosis in travelers: review of the literature. J Travel Med 22:410–414. doi: 10.1111/jtm.12236. [DOI] [PubMed] [Google Scholar]
- 9.Raja NS, Ahmed MZ, Singh NN. 2005. Melioidosis: an emerging infectious disease. J Postgrad Med 51:140–145. doi: 10.5005/jp/books/11617_52. [DOI] [PubMed] [Google Scholar]
- 10.Benoit TJ, Blaney DD, Gee JE, Elrod MG, Hoffmaster AR, Doker TJ, Bower WA, Walke HT, Centers for Disease C, Prevention. 2015. Melioidosis cases and selected reports of occupational exposures to Burkholderia pseudomallei—United States, 2008–2013. MMWR Surveill Summ 64:1–9. [PubMed] [Google Scholar]
- 11.Currie BJ, Ward L, Cheng AC. 2010. The epidemiology and clinical spectrum of melioidosis: 540 cases from the 20 year Darwin prospective study. PLoS Negl Trop Dis 4:e900. doi: 10.1371/journal.pntd.0000900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Limmathurotsakul D, Jamsen K, Arayawichanont A, Simpson JA, White LJ, Lee SJ, Wuthiekanun V, Chantratita N, Cheng A, Day NP, Verzilli C, Peacock SJ. 2010. Defining the true sensitivity of culture for the diagnosis of melioidosis using Bayesian latent class models. PLoS One 5:e12485. doi: 10.1371/journal.pone.0012485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarovich DS, Ward L, Price EP, Mayo M, Pitman MC, Baird RW, Currie BJ. 2014. Recurrent melioidosis in the Darwin Prospective Melioidosis Study: improving therapies mean that relapse cases are now rare. J Clin Microbiol 52:650–653. doi: 10.1128/JCM.02239-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leelarasamee A, Bovornkitti S. 1989. Melioidosis: review and update. Rev Infect Dis 11:413–425. doi: 10.1093/clinids/11.3.413. [DOI] [PubMed] [Google Scholar]
- 15.Eickhoff TC, Bennett JV, Hayes PS, Feeley J. 1970. Pseudomonas pseudomallei: susceptibility to chemotherapeutic agents. J Infect Dis 121:95–102. doi: 10.1093/infdis/121.2.95. [DOI] [PubMed] [Google Scholar]
- 16.Chaowagul W. 2000. Recent advances in the treatment of severe melioidosis. Acta Trop 74:133–137. doi: 10.1016/S0001-706X(99)00062-5. [DOI] [PubMed] [Google Scholar]
- 17.Hoffmaster AR, AuCoin D, Baccam P, Baggett HC, Baird R, Bhengsri S, Blaney DD, Brett PJ, Brooks TJ, Brown KA, Chantratita N, Cheng AC, Dance DA, Decuypere S, Defenbaugh D, Gee JE, Houghton R, Jorakate P, Lertmemongkolchai G, Limmathurotsakul D, Merlin TL, Mukhopadhyay C, Norton R, Peacock SJ, Rolim DB, Simpson AJ, Steinmetz I, Stoddard RA, Stokes MM, Sue D, Tuanyok A, Whistler T, Wuthiekanun V, Walke HT. 2015. Melioidosis diagnostic workshop, 2013. Emerg Infect Dis doi: 10.3201/eid2102.141045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wuthiekanun V, Limmathurotsakul D, Wongsuvan G, Chierakul W, Teerawattanasook N, Teparrukkul P, Day NP, Peacock SJ. 2007. Quantitation of B. Pseudomallei in clinical samples. Am J Trop Med Hyg 77:812–813. [PubMed] [Google Scholar]
- 19.Wongsuvan G, Limmathurotsakul D, Wannapasni S, Chierakul W, Teerawattanasook N, Wuthiekanun V. 2009. Lack of correlation of Burkholderia pseudomallei quantities in blood, urine, sputum and pus. Southeast Asian J Trop Med Public Health 40:781–784. [PubMed] [Google Scholar]
- 20.Ashdown LR. 1979. An improved screening technique for isolation of Pseudomonas pseudomallei from clinical specimens. Pathology 11:293–297. doi: 10.3109/00313027909061954. [DOI] [PubMed] [Google Scholar]
- 21.Wuthiekanun V, Dance DA, Wattanagoon Y, Supputtamongkol Y, Chaowagul W, White NJ. 1990. The use of selective media for the isolation of Pseudomonas pseudomallei in clinical practice. J Med Microbiol 33:121–126. doi: 10.1099/00222615-33-2-121. [DOI] [PubMed] [Google Scholar]
- 22.Peacock SJ, Chieng G, Cheng AC, Dance DA, Amornchai P, Wongsuvan G, Teerawattanasook N, Chierakul W, Day NP, Wuthiekanun V. 2005. Comparison of Ashdown's medium, Burkholderia cepacia medium, and Burkholderia pseudomallei selective agar for clinical isolation of Burkholderia pseudomallei. J Clin Microbiol 43:5359–5361. doi: 10.1128/JCM.43.10.5359-5361.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Glass MB, Beesley CA, Wilkins PP, Hoffmaster AR. 2009. Comparison of four selective media for the isolation of Burkholderia mallei and Burkholderia pseudomallei. Am J Trop Med Hyg 80:1023–1028. [PubMed] [Google Scholar]
- 24.Brett PJ, DeShazer D, Woods DE. 1998. Burkholderia thailandensis sp. nov., a Burkholderia pseudomallei-like species. Int J Syst Bacteriol 48:317–320. doi: 10.1099/00207713-48-1-317. [DOI] [PubMed] [Google Scholar]
- 25.Glass MB, Steigerwalt AG, Jordan JG, Wilkins PP, Gee JE. 2006. Burkholderia oklahomensis sp. nov., a Burkholderia pseudomallei-like species formerly known as the Oklahoma strain of Pseudomonas pseudomallei. Int J Syst Evol Microbiol 56:2171–2176. doi: 10.1099/ijs.0.63991-0. [DOI] [PubMed] [Google Scholar]
- 26.Richardson LJ, Kaestli M, Mayo M, Bowers JR, Tuanyok A, Schupp J, Engelthaler D, Wagner DM, Keim PS, Currie BJ. 2012. Towards a rapid molecular diagnostic for melioidosis: comparison of DNA extraction methods from clinical specimens. J Microbiol Methods 88:179–181. doi: 10.1016/j.mimet.2011.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Limmathurotsakul D, Wuthiekanun V, Chierakul W, Cheng AC, Maharjan B, Chaowagul W, White NJ, Day NP, Peacock SJ. 2005. Role and significance of quantitative urine cultures in diagnosis of melioidosis. J Clin Microbiol 43:2274–2276. doi: 10.1128/JCM.43.5.2274-2276.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holm A, Aabenhus R. 2016. Urine sampling techniques in symptomatic primary-care patients: a diagnostic accuracy review. BMC Fam Pract 17:72. doi: 10.1186/s12875-016-0465-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meumann EM, Novak RT, Gal D, Kaestli ME, Mayo M, Hanson JP, Spencer E, Glass MB, Gee JE, Wilkins PP, Currie BJ. 2006. Clinical evaluation of a type III secretion system real-time PCR assay for diagnosing melioidosis. J Clin Microbiol 44:3028–3030. doi: 10.1128/JCM.00913-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Novak RT, Glass MB, Gee JE, Gal D, Mayo MJ, Currie BJ, Wilkins PP. 2006. Development and evaluation of a real-time PCR assay targeting the type III secretion system of Burkholderia pseudomallei. J Clin Microbiol 44:85–90. doi: 10.1128/JCM.44.1.85-90.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kaestli M, Mayo M, Harrington G, Watt F, Hill J, Gal D, Currie BJ. 2007. Sensitive and specific molecular detection of Burkholderia pseudomallei, the causative agent of melioidosis, in the soil of tropical northern Australia. Appl Environ Microbiol 73:6891–6897. doi: 10.1128/AEM.01038-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tandhavanant S, Wongsuvan G, Wuthiekanun V, Teerawattanasook N, Day NP, Limmathurotsakul D, Peacock SJ, Chantratita N. 2013. Monoclonal antibody-based immunofluorescence microscopy for the rapid identification of Burkholderia pseudomallei in clinical specimens. Am J Trop Med Hyg 89:165–168. doi: 10.4269/ajtmh.13-0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Houghton RL, Reed DE, Hubbard MA, Dillon MJ, Chen H, Currie BJ, Mayo M, Sarovich DS, Theobald V, Limmathurotsakul D, Wongsuvan G, Chantratita N, Peacock SJ, Hoffmaster AR, Duval B, Brett PJ, Burtnick MN, Aucoin DP. 2014. Development of a prototype lateral flow immunoassay (LFI) for the rapid diagnosis of melioidosis. PLoS Negl Trop Dis 8:e2727. doi: 10.1371/journal.pntd.0002727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chantratita N, Meumann E, Thanwisai A, Limmathurotsakul D, Wuthiekanun V, Wannapasni S, Tumapa S, Day NP, Peacock SJ. 2008. Loop-mediated isothermal amplification method targeting the TTS1 gene cluster for detection of Burkholderia pseudomallei and diagnosis of melioidosis. J Clin Microbiol 46:568–573. doi: 10.1128/JCM.01817-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bernhardt M, Pennell DR, Almer LS, Schell RF. 1991. Detection of bacteria in blood by centrifugation and filtration. J Clin Microbiol 29:422–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boardman AK, Campbell J, Wirz H, Sharon A, Sauer-Budge AF. 2015. Rapid microbial sample preparation from blood using a novel concentration device. PLoS One 10:e0116837. doi: 10.1371/journal.pone.0116837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fothergill A, Kasinathan V, Hyman J, Walsh J, Drake T, Wang YF. 2013. Rapid identification of bacteria and yeasts from positive-blood-culture bottles by using a lysis-filtration method and matrix-assisted laser desorption ionization–time of flight mass spectrum analysis with the SARAMIS database. J Clin Microbiol 51:805–809. doi: 10.1128/JCM.02326-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Friedman MP, Danielski JM, Day TE, Dunne JC, Evangelista AT, Freeman TR. 1991. Rapid isolation and presumptive diagnosis of uropathogens by using membrane filtration and differential media. J Clin Microbiol 29:2385–2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gal D, Mayo M, Spencer E, Cheng AC, Currie BJ. 2005. Short report: application of a polymerase chain reaction to detect Burkholderia pseudomallei in clinical specimens from patients with suspected melioidosis. Am J Trop Med Hyg 73:1162–1164. [PubMed] [Google Scholar]
- 40.Schrader C, Schielke A, Ellerbroek L, Johne R. 2012. PCR inhibitors—occurrence, properties and removal. J Appl Microbiol 113:1014–1026. doi: 10.1111/j.1365-2672.2012.05384.x. [DOI] [PubMed] [Google Scholar]
- 41.Liu L, Mo H, Wei S, Raftery D. 2012. Quantitative analysis of urea in human urine and serum by 1H nuclear magnetic resonance. Analyst 137:595–600. doi: 10.1039/C2AN15780B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ghosh HK. 1970. Role of bacterial growth inhibitors in urine in diagnostic culture. J Clin Pathol 23:627–628. doi: 10.1136/jcp.23.7.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chambers ST, Peddie BA, Randall K, Lever M. 1999. Inhibitors of bacterial growth in urine: what is the role of betaines? Int J Antimicrob Agents 11:293–296. doi: 10.1016/S0924-8579(99)00033-3. [DOI] [PubMed] [Google Scholar]
- 44.Michelle Wong Tzeling J, Yean Yean C. 2016. A shelf-stable fluorogenic isothermal amplification assay for the detection of Burkholderia pseudomallei. Analyst 141:1246–1249. doi: 10.1039/C5AN01741F. [DOI] [PubMed] [Google Scholar]
- 45.Bugrysheva JV, Sue D, Hakovirta J, Loparev VN, Knipe K, Sammons SA, Ranganathan-Ganakammal S, Changayil S, Srinivasamoorthy G, Weil MR, Tatusov RL, Gee JE, Elrod MG, Hoffmaster AR, Weigel LM. 2015. Finished annotated genome sequence of Burkholderia pseudomallei strain Bp1651, a multidrug-resistant clinical isolate. Genome Announc 3:e01427-15. doi: 10.1128/genomeA.01427-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bugrysheva JV, Lascols C, Sue D, Weigel LM. 2016. Rapid antimicrobial susceptibility testing of Bacillus anthracis, Yersinia pestis, and Burkholderia pseudomallei by use of laser light scattering technology. J Clin Microbiol 54:1462–1471. doi: 10.1128/JCM.03251-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Propst KL, Mima T, Choi KH, Dow SW, Schweizer HP. 2010. A Burkholderia pseudomallei ΔpurM mutant is avirulent in immunocompetent and immunodeficient animals: candidate strain for exclusion from select-agent lists. Infect Immun 78:3136–3143. doi: 10.1128/IAI.01313-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Qiagen. 2016. QIAamp DNA mini and blood mini handbook. Qiagen, Hilden, Germany. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


