Abstract
AIM
To compare radiation dose and image quality of low-dose computed tomography (CT) protocol combined with hybrid-iterative reconstruction algorithm with standard-dose CT examinations for follow-up of oncologic patients.
METHODS
Fifty-one patients with known malignant diseases which underwent, during clinical follow-up, both standard-dose and low-dose whole-body CT scans were enrolled. Low-dose CT was performed on 256-row scanner, with 120 kV and automated mA modulation, and iterative reconstruction algorithm. Standard-dose CT was performed on 16-rows scanner, with 120 kV, 200-400 mAs (depending on patient weight). We evaluated density values and signal-to-noise ratio, along with image noise (SD), sharpness and diagnostic quality with 4-point scale.
RESULTS
Density values in liver, spleen and aorta were higher in low-dose images (liver 112.55 HU vs 103.90 HU, P < 0.001), as SD values in liver and spleen (liver 16.81 vs 14.41). Volumetric-Computed-Tomographic-Dose-Index (CTDIvol) and Dose-Length-Product (DLP) were significantly lower in low-dose CT as compared to standard-dose (DLP 1025.6 mGy*cm vs 1429.2 mGy*cm, P < 0.001) with overall dose reduction of 28.9%. Qualitative analysis did not reveal significant differences in image noise and diagnostic quality.
CONCLUSION
Automatic tube-current modulation combined with hybrid-iterative algorithm allows radiation dose reduction of 28.9% without loss of diagnostic quality, being useful in reducing dose exposure in oncologic patients.
Keywords: Computed tomography, Low-dose computed tomography, Tube current modulation, Oncologic imaging, Radiation dose
Core tip: Introduction of new generation of multidetector computed tomography (MDCT) scanner allowed thin-collimation scanning and high spatial resolution, and reducing at same time the delivered radiation dose to patients by using new iterative reconstruction algorithm. This new mathematical model approach permits to reduce the radiation dose, expecially in patients who undergo serial follow-up study for oncologic (staging and restaging) purpose. On these basis in our study we evaluated radiation dose and image quality of CT examinations in a population of oncologic patients undergoing follow-up examinations with a new generation MDCT scanner (256-rows) using automatic modulation of tube current and iterative reconstruction algorithm (DoseRight system).
INTRODUCTION
Since the advent of computed tomography (CT) and, more recently, the development of multidetector computed tomography (MDCT) technique, the number of CT scans have increased significantly[1,2]; according to National Council on Radiation Protection and Measurements (NCRP) report 160, in 2006 United States population was exposed to more than seven times ionizing radiation from medical procedures than in the early 1980’s, and CT contributes to nearly one-half of all this radiation imaging exposure[1,2]. This high number of CT examinations have raised concern because of the potential risk of radiation-induced malignancy[3].
In the clinical management of patients with malignant diseases CT, with other cross-sectional imaging techniques such as MRI and FDG-PET/CT, has a major role for initial diagnosis of the disease, for staging, and during follow-up to monitor response to treatment and evaluate disease remission or relapse[4]. CT of the chest, abdomen and pelvis has the ability to obtain a global evaluation of the patient and to depict both primary tumor and metastasis in most cases, more quickly, safely and accurately than other more invasive or less sensitive imaging techniques. On these bases, oncologic patients typically undergo multiple CT investigations during their clinical follow-up, and risks derived from repeated scans and exposure to ionizing radiation should be balanced against the benefits of diagnostic imaging: CT examinations must have a correct clinical justification, and every CT scans must be technically optimized to keep radiation doses as low as possible while providing requested diagnostic information[5,6].
To optimize radiation dose in CT various technological strategies can be applied: These include active management of individual acquisition parameters (number of phases, section thickness, peak voltage, tube current-time product, pitch) or using an automated exposure control system[7]. Recently, iterative reconstruction algorithms have been introduced to reduce image noise, allowing further reduction in radiation dose beyond levels previously achievable with filtered back projection reconstruction (FBP)[7]. iDose4 is a hybrid iterative algorithm that is able to reduce noise on both the raw and image data[8,9]. The purpose of our study was to evaluate the radiation dose and image quality of CT examinations in a population of oncologic patients undergoing follow-up examinations comparing a new generation MDCT scanner (256-rows), using automatic modulation of tube current and iterative reconstruction algorithm (DoseRight system and iDose4), with a 16-MDCT scanner using standard dose protocol and FBP.
MATERIALS AND METHODS
Patients population
Institutional research board approval was obtained for this retrospective study with waiver of the requirement for written consent.
Between August 2013 and April 2015, 259 adult patients (> 18 years old) with known malignant diseases (32 lung, 9 colorectal, 3 ovarian, 3 stomach, 2 uterine, 1 non hodgkin lymphoma and 1 testicular) underwent contrast enhanced chest-abdomen-pelvis CT examination in a single venous phase during their clinical follow-up on a 256-MDCT scanner with a protocol implemented in our institution from August 2013 (with automatic modulation of current tube and iDose4 reconstruction algorithm). These examinations were identified with a retrospective review of CT studies archived with PACS system (AGFA Diagnostic Software, Impax, version 6.4.0.3125; Agfa, Mortsel; Belgium). In this group we selected patients which had undergone also standard-dose contrast enhanced CT scan on a 16-MDCT in a different time. Fifty-one patients were finally selected as our study group and were categorized into four groups according to their weight (kg): 41-60 kg (group A), 61-80 kg (group B), 81-90 kg (group C) and > 90 kg (group D) (Table 1). Total mean weight was not statistically different between the two scans (74.1 ± 14.9 kg for lower dose scans and 73.9 ± 15.0 kg for standard dose scans, P = 0.705). The mean time interval between CT acquisitions was 4.8 ± 2.9 mo. Patients’ mean age, calculated at the time of the most recent CT scan, was 68.3 ± 10.4 years old.
Table 1.
Descriptive table of weight groups in the patients population (n = 51)
| Weight groups | No. of patients | M/F | Mean ± SD (yr) |
| Group A (41-60 kg) | 8 | 3/5 | 70.5 ± 8.6 |
| Group B (61-80 kg) | 25 | 9/16 | 67.6 ± 11.5 |
| Group C (81-90 kg) | 13 | 11/2 | 71.8 ± 7.4 |
| Group D ( > 90 kg) | 5 | 4/1 | 59.2 ± 10.1 |
| All patients | 51 | 34/18 | 68.3 ± 10.4 |
M: Male; F: Female.
MDCT technique and image reconstruction
All 51 patients had undergone thorax-abdomen-pelvis CT examinations both on a 16-rows MDCT scanner (Brilliance, Philips Medical Systems, Eindhoven, The Netherlands) and on a 256-rows MDCT (iCT, Philips).
For both examinations, CT data were acquired after the intravenous bolus injection of non-ionic iodinated contrast material (Xenetix 350; Guerbet, Aulnay, France), injected using a 18-gauge catheter positioned into the antecubital vein at a rate of 3.5 mL/s, with image acquisition during portal venous phase (55-70 s after the initiation of the contrast bolus), in accordance with an institutionally defined protocol. The volume of contrast agent was calculated on the basis of the patient’s body weight, with total dose ranging from 80 to 130 mL, and it was followed by a saline flush of 50 mL of NaCl at 3.5 mL/s. The patients were instructed to hold their breath during scanning. All studies were started from the lung apices and proceeded in a cephalocaudal direction until ischial tuberosity, to include chest, abdomen and pelvis of the patients.
The technical parameters for scanning included: (1) for 16-rows CT scanner: 120 kVp, mAs depending on patients’ weight (41-60 kg: 200 mAs; 61-80 kg: 300 mAs; 81-90 kg: 350 mAs; > 90 kg: 400 mAs), section thickness 2 mm, pitch 0.813, 0.75 s rotation time, display field of view (FOV) depending on the patient’s physique (median values of 350), beam collimation 16 × 1.5; (2) for 256-rows CT scanner: 120 kVp, automated mAs with X-ray tube current automatic modulation system (range of mean mAs: 103-468 mAs), section thickness 2 mm, pitch 0.984, 0.75 s rotation time, display field of view (FOV) depending on the patient’s physique (median values of 350), beam collimation 64 mm × 0.625 mm (to reduce the overranging and to improve the Z-DOM modulation performance). The Brilliance iCT scanner can control radiation exposure with advanced dose reduction tools, such as X-ray tube current automatic modulation system (the automatic current selection ACS, which automatically suggests tube current settings according to estimated patient diameter in the scan region, and the Z-axis dose modulation system Z-DOM, that modulates mA along the patient longitudinal axis using the attenuation profile estimated from the Surview), SmartShape and IntelliBeam shaping filters, the Eclipse asymmetric collimator for over-ranging reduction, NanoPanel3D detectors and ClearRay 2D anti-scatter grid[10].
The 16-MDCT images were reconstructed using a standard FBP algorithm with a standard soft-tissue kernel, while the 256-MDCT images were reconstructed with hybrid iterative reconstruction algorithm (iDose4): iDose4Level 3 was chosen[8].
At the end of every examinations, the volumetric computed tomographic dose index (CTDIvol) and the dose-length product (DLP) were provided by the scanners in the dosimetric report.
CT values (HU) and standard deviation of CT values (SD) were also measured by placing one ROI (2 cm2) within the subcutaneous fat of the anterior abdominal wall. SNR was calculated for the liver and the spleen as: SNR = HUROI/SDROI, where HUROI is the mean CT value in Hounsfield units of the tissue and SDROI the standard deviation of CT values in the same ROI.
Statistical analysis
Continuous variables (HU, SD, SNR, DLP, CTDIvol, patients weight) were presented as means ± SD. The Wilcoxon signed-rank test for paired samples or paired Student t-test were used, where appropriate, to compare values of continuous variables between standard dose protocol images and lower dose protocol images. To evaluate differences in qualitative analysis between the two protocols the Wilcoxon signed-rank test for paired samples was applied. A P-value < 0.05 was considered statistically significant.
Cohen’s kappa was used to evaluate agreement between the two readers[11]. Analysis was performed with commercially available statistical software (SPSS Statistics 17.0, Chicago, IL).
RESULTS
Radiation dose
Mean values of obtained DLP and CTDIvol were significantly lower with low-dose protocol in comparison with standard dose protocol (P < 0.001): For lower-dose CT, DLP and CTDIvol were respectively 1025.6 ± 370.9 mGy*cm and 15.4 ± 5.2 mGy, compared with 1429.2 ± 297.7 mGy*cm and 21.4 ± 4.0 mGy for standard-dose protocol. The low-dose protocol provided a mean DLP reduction of 28.9% compared to standard-dose protocol (Figure 1).
Figure 1.
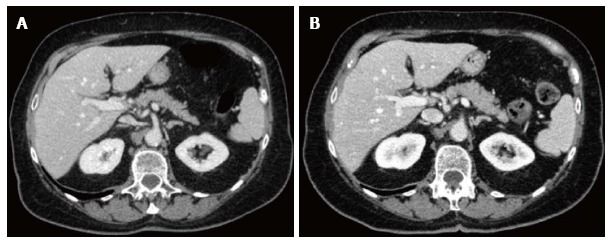
Axial contrast-enhanced computed tomography images at the level of upper abdomen obtained in a 81 years old female patient with lung cancer (height 160 cm, weight 61 kg). A: Standard dose protocol (120 kV, 300 mAs, DLP 1317.4 mGy*cm, CDTI 21.1 mGy); B: Lower dose protocol (120 kV, 142-222 mAs, DLP 846.0 mGy*cm, CDTI 13.6 mGy): Lower dose image shows increased sharpness and enhancement in comparison with standard dose image in spite of mild increase of noise, and similar diagnostic quality with a 35.8% Dose-Length-Product reduction.
The average weight was 74.1 ± 14.9 kg for low dose scans (range 41-114 kg) and 73.9 ± 15.0 kg for standard dose scans (range 43-114 kg) (P = 0.705). By dividing patients into four groups of weight, we obtained a higher rate of DLP reduction in patients in groups A, B and C with a statistically significant difference between the two protocols; in patients with high weight (> 90 kg, group D), for values of DLP and CTDIvol only few differences between the two protocols were recorded, not statistically significant, with a radiation dose reduction of 2.5% (Table 2).
Table 2.
Comparison of Dose-Length Product and Volumetric Computed Tomographic Dose Index obtained with standard-dose and low-dose protocols in all patients (n = 51) and according to weight (kg)
| BMI groups | No. of patients |
CTDIvol (mGy) |
DLP (mGy*cm) |
% DLP reduction | ||||
| Standard-dose | Low-dose | P-value | Standard-dose | Low-dose | P-value | |||
| Group A (41-60 kg) | 8 | 14.1 ± 0.0 | 9.8 ± 1.5 | 0.012 | 891.9 ± 36.3 | 627.5 ± 92.9 | 0.012 | 29.6 |
| Group B (61-80 kg) | 25 | 21.1 ± 0.0 | 14.0 ± 2.8 | < 0.001 | 1386.6 ± 65.9 | 920.0 ± 175.0 | < 0.001 | 33.5 |
| Group C (81-90 kg) | 13 | 24.6 ± 0.0 | 17.2 ± 2.9 | 0.001 | 1656.8 ± 61.2 | 1162.6 ± 204.2 | 0.001 | 29.9 |
| Group D ( > 90 kg) | 5 | 27.4 ± 1.5 | 26.5 ± 5.4 | 0.5 | 1910.4 ± 147.6 | 1835.1 ± 359.5 | 0.5 | 2.5 |
| All patients | 51 | 21.4 ± 4.0 | 15.4 ± 5.2 | < 0.001 | 1429.2 ± 297.7 | 1025.6 ± 370.9 | < 0.001 | 28.9 |
DLP: Dose-Length-Product; CTDIvol: Volumetric Computed Tomographic Dose Index.
Qualitative analysis
Qualitative analysis results are shown in Table 3. There was a good inter-reader agreement, as shown by k Cohen values. There weren’t significant differences in the qualitative evaluation of image noise and diagnostic quality for both readers (Figure 2), and of image sharpness for one reader. The other reader assigned to low-dose images superior grades for sharpness, with a significant difference (P = 0.012).
Table 3.
Qualitative scoring of image noise, image sharpness and diagnostic quality of computed tomography images from Reader 1 and Reader 2
|
Image noise |
Image sharpness |
Diagnostic quality |
||||
| Reader 1 | Reader 2 | Reader 1 | Reader 2 | Reader 1 | Reader 2 | |
| Low-dosea | 3.4 ± 0.6 | 3.6 ± 0.6 | 3.7 ± 0.5 | 3.7 ± 0.5 | 3.7 ± 0.5 | 3.8 ± 0.4 |
| Group A (n = 8) | 3.6 ± 0.7 | 3.8 ± 0.5 | 3.6 ± 0.5 | 3.5 ± 0.5 | 3.9 ± 0.4 | 3.8 ± 0.5 |
| Group B (n = 25) | 3.4 ± 0.6 | 3.6 ± 0.6 | 3.8 ± 0.5 | 3.8 ± 0.4 | 3.7 ± 0.6 | 3.8 ± 0.4 |
| Group C (n = 13) | 3.1 ± 0.4 | 3.6 ± 0.5 | 3.6 ± 0.5 | 3.9 ± 0.4 | 3.6 ± 0.5 | 4.0 ± 0.0 |
| Group D (n = 5) | 3.3 ± 0.6 | 3.0 ± 1.0 | 4.0 ± 0.0 | 3.3 ± 0.6 | 4.0 ± 0.0 | 3.7 ± 0.6 |
| Standard-doseb | 3.6 ± 0.7 | 3.5 ± 0.6 | 3.3 ± 0.7 | 3.5 ± 0.6 | 3.7 ± 0.5 | 3.8 ± 0.4 |
| Group A (n = 8) | 3.9 ± 0.4 | 3.5 ± 0.5 | 3.1 ± 0.6 | 3.4 ± 0.5 | 3.9 ± 0.4 | 3.8 ± 0.5 |
| Group B (n = 25) | 3.7 ± 0.5 | 3.7 ± 0.5 | 3.5 ± 0.6 | 3.5 ± 0.6 | 3.8 ± 0.4 | 3.8 ± 0.4 |
| Group C (n = 13) | 3.3 ± 0.5 | 3.3 ± 0.5 | 2.9 ± 0.7 | 3.9 ± 0.4 | 3.6 ± 0.5 | 4.0 ± 0.0 |
| Group D (n = 5) | 2.3 ± 1.5 | 3.0 ± 1.0 | 3.0 ± 1.0 | 3.3 ± 0.6 | 2.7 ± 1.2 | 3.7 ± 0.6 |
| P-valuea-b | 0.292 | 0.655 | 0.012 | 0.088 | 0.437 | 0.206 |
| k Cohen Reader 1-Reader 2 | 0.694a-0.756b | 0.783a-0.672b | 0.704a-0.786b | |||
Figure 2.
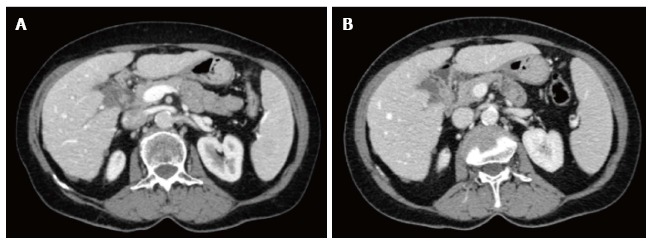
Axial contrast-enhanced computed tomography images at the level of upper abdomen obtained in a 70 years old female patient with ovarian cancer and some small hypoattenuating hepatic subcapsular implants with well-defined margins (height 160 cm, weight 68 kg). A: Standard dose protocol (120 kV, 300 mAs, Dose-Length-Product 1304.6 mGy*cm, CDTI 21.0 mGy); B: Lower dose protocol (120 kV, 123-231 mAs, Dose-Length-Product 840.9 mGy*cm, CDTI 13.1 mGy).
Quantitative analysis
CT values of density (HU) measured within abdominal aortic lumen and liver and spleen parenchyma were significantly higher using low-dose CT with iDose4 (P < 0.001) (Table 4). The mean liver and spleen parenchymal noise (SD) was higher with low-dose protocol as well, while SD of abdominal subcutaneous fat was higher but without reaching statistical significance. The measured noise varied according to the weight of the patients, with higher values of SD in patients with higher weight; values of SD in the liver parenchyma with low-dose protocol vs standard protocol were respectively 14.62 ± 1.80 vs 11.62 ± 2.03 in group A, 16.66 ± 1.45 vs 13.10 ± 2.18 in group B, 18.03 ± 1.98 vs 16.26 ± 1.54 in group C and 17.91 ± 2.24 vs 20.59 ± 3.28 in group D.
Table 4.
Computed tomography values (HU), standard deviation of computed tomography values (SD) and signal-to-noise ratio obtained with standard-dose and low-dose protocols
| Low-dose | Standard-dose | P-value | |
| HUaorta (n = 51) | 166.20 ± 18.83 | 154.17 ± 24.82 | < 0.001 |
| HUliver (n = 51) | 112.55 ± 16.49 | 103.90 ± 17.49 | < 0.001 |
| HUspleen (n = 51) | 126.24 ± 13.60 | 112.77 ± 15.66 | < 0.001 |
| SDliver (n = 51) | 16.81 ± 2.02 | 14.41 ± 3.33 | < 0.001 |
| SDspleen (n = 51) | 16.78 ± 2.04 | 14.72 ± 3.26 | < 0.001 |
| SDfat (n = 51) | 12.17 ± 2.77 | 12.07 ± 2.98 | 0.307 |
| SNRliver (n = 51) | 6.94 ± 1.32 | 7.80 ± 2.30 | 0.002 |
| SNRliver Group A (n = 8) | 8.09 ± 1.63 | 9.36 ± 2.27 | 0.05 |
| SNRliver Group B (n = 25) | 6.95 ± 1.22 | 8.53 ± 1.97 | < 0.001 |
| SNRliver Group C (n = 13) | 6.47 ± 1.00 | 6.66 ± 1.34 | 0.972 |
| SNRliver Group D (n = 5) | 6.29 ± 1.19 | 4.60 ± 1.77 | 0.08 |
| SNRspleen (n = 51) | 7.73 ± 1.46 | 8.10 ± 2.04 | 0.153 |
| SNRspleen Group A (n = 8) | 9.25 ± 2.31 | 10.53 ± 1.69 | 0.092 |
| SNRspleen Group B (n = 25) | 7.60 ± 1.10 | 8.04 ± 1.86 | 0.177 |
| SNRspleen Group C (n = 13) | 7.26 ± 1.11 | 7.20 ± 1.45 | 0.65 |
| SNRspleen Group D (n = 5) | 7.21 ± 0.82 | 6.86 ± 1.89 | 0.893 |
SNR: Signal-to-noise ratio.
SNR values, calculated as SNR = HUROI/SDROI, were lower in low-dose images, reaching a significant difference within the liver parenchyma (6.94 ± 1.32 vs 7.80 ± 2.30, P = 0.002) and without statistical significance within spleen parenchyma (7.73 ± 1.46 vs 8.10 ± 2.04, P = 0.153). When SNR data were reviewed according to the weight of patients, SNR values decreased as patients’ weight increased. SNR values were lower in low-dose protocol in comparison with standard-dose protocol in groups A and B, comparable between two protocols in group C and higher in group D (Table 3).
DISCUSSION
In the latest years many studies investigating the potential of radiation dose reduction by applying different iterative reconstruction algorithms have been published for abdomen, chest, head, coronary and chest angiography, and they showed significant dose reduction while maintaining, or sometimes improving, image quality[12-26].
Arapakis et al[12] addressed the effect of iterative algorithm on radiation dose and image quality of chest-abdomen-pelvis (CAP) CT scans. They applied iDose4 hybrid iterative reconstruction algorithm in a group of 84 patients and compared images to those obtained with “old standard” protocol with filtered back projection reconstruction algorithm in a group of 99 patients, obtaining an overall 46.5% decrease in effective dose with lower image noise and higher values of SNR and CNR; in their study, the greatest dose reduction was recorded in patients with lower weight[12].
Karpitschka et al[13] retrospectively evaluated 40 patients which underwent CT scans for staging of malignancy with both a standard-dose (tube current time product 250 mAs and FBP reconstruction) and a reduced-dose CT scan (150 mAs and with Iterative Reconstruction in Image Space IRIS), obtaining a greater than 45% dose reduction at maintained image quality; the authors recommend the use of IR in oncological patients in order to reduce radiation dose to patients.
Moreover, for abdominal CT scans, Prakash et al[14] showed a reduction of radiation dose by 25% using weight-based adjustment of automatic exposure control technique and Adaptive Statistical Iterative Reconstruction (ASIR) in comparison with FBP reconstructed scans, while May et al[15] obtained a 50% reduction in abdominal CT by using IRIS.
In our study, values of DLP obtained using a low-dose protocol with iDose4 iterative algorithm were, on average, 28.9% lower compared to our standard dose with FBP reconstruction. Despite higher levels of quantitative noise (as demonstrated by SD values) within liver and spleen parenchyma, however, qualitative analysis didn’t reveal significant differences in overall image noise and diagnostic quality when compared with standard-dose images in the same patients (Table 2). These results and lower rate of dose reduction in comparison with other CAP studies may be correlated to a different level of strength of the iterative reconstruction of iDose4 applied in our institution (L3) which determines less noise reduction and, with a fixed noise index, can be associated with higher levels of tube current and radiation dose.
The measured noise and SNR in low-dose images varied according to the weight of the patients, with higher values of SD and lower values of SNR in patients with higher weight (Table 3). These data were confirmed by qualitative analysis, which showed increasing levels of subjective noise by increasing patients weight, but without significant differences in image sharpness and diagnostic quality between the four groups (Table 2). In our patient group with weight greater than 90 kg (group D), values of SD within liver and spleen parenchyma and abdominal fat were the highest, with worst values of SNR; however, compared to standard-dose images, these values of SNR were higher indicating a better image contrast, although the difference was not statistically significant.
In group D the DLP reduction rate was substantially lower than those in the other patient groups (2.5% vs 29.6%, 33.5% and 29.9%). With automatic tube current modulation, tube current is automatically adjusted to the X-ray attenuation of the patient to keep the radiation dose as low as possible while maintaining a constant image noise level and specified image quality as in a previously defined reference image. In patients with large body habitus, to maintain a constant image quality, there is a risk of high radiation doses when this technique is applied in abdominal MDCT[23]. Our results could be explained then by the higher tube current needed and used in this group of patients to fulfill the fixed noise level and desired final image quality. In heavy patients, the optimal noise indexes and image quality should be adjusted to patient habitus, considering that subjective image quality in abdomen CT of these patients is usually higher because of the amount of fat deposition around the abdominal organ that improve tissue contrast[23].
There were several limitations in our study. First of all, it was a retrospective study and acquisition of CT paired studies in our patients were not realized on the same scanner; despite many technical parameters were identical between the two protocols, some of them and the scanners were different and it may have introduced some bias. Because of the interval time between studies, which was remarkable in a small number of patients, and the retrospective nature of the study, we couldn’t compare conspicuity or detection rate of the primary tumor and secondary lesions between the two protocols, which should be addressed in further prospective studies.
In conclusion, in our sample of oncologic patients, automatic modulation of tube current and iDose4 reconstruction algorithm allowed a mean radiation dose reduction of 28.9%, without significant loss of subjective diagnostic quality, and this protocol could be useful in reducing dose exposure in patients with malignancy which undergo a high number of chest-abdomen-pelvis CT scan during their clinical follow-up.
COMMENTS
Background
In the latest years, the number of computed tomography (CT) scans have increased significantly and this high number of examinations has raised concern because of the potential risk of radiation-induced malignancy. CT has a major role in the clinical management of patients with malignant diseases, which typically undergo multiple CT investigations during their follow-up, and risks derived from repeated scans and exposure to ionizing radiation should be balanced against the benefits of diagnostic imaging. On this basis in the study authors compared the diagnostic quality and the radiation dose of whole body CT scan examination obtained with a low-dose setting protocol combined with the new state of art iterative reconstruction algorithm with those obtained with a standard-dose protocol.
Research frontiers
New generation of high row number multidetector computed tomography (MDCT) scans allow thin-collimation, high spatial resolution and better multiplanar reconstructions (MPRs), and are increasingly used in clinical practice in oncologic field, because MDCT can assess in a single examination, the entire abdomen, pelvis and chest, allowing for local tumour staging and distant metastases evaluation. Several dose reduction tools are actually integrated in these new CT-scanners, including hardware components as dynamic helical collimator, adaptive axial collimator and tube-current modulation, and software post-acquisition improvements as iterative reconstruction algorithms. These technical solutions permit to reduce the dose delivered to the patients, maintaining high diagnostic quality of images.
Innovations and breakthroughs
CT protocols should be properly designed and carefully applied in order to obtain the highest amount of information by using the lowest radiation dose achievable, since the theoretical risk of radiation-induced cancer from CT examinations has been reported as not negligible. New CT scanners are equipped with several iterative reconstruction (IR) algorithms that allow a reduction of the radiation dose without theoretically affecting the image quality, especially if used in association with a low kV scanning protocol. The study was designed in order to obtain the best image quality with the lowest effective dose, using dose reduction strategies available with our scanner. iDose4 is a fourth-generation hybrid IR algorithm introduced by Philips Healthcare, and the major component of this algorithm deals with subtraction of the image noise while preserving the underlying edges associated with true anatomy or pathology.
Applications
In this study the authors compared radiation dose and image quality of CT examinations in a population of oncologic patients undergoing follow-up examinations with a new generation MDCT scanner (256-rows) using automatic modulation of current tube and iterative reconstruction algorithm (DoseRight system and iDose4) and with a 16-MDCT scanner with standard dose protocol and FBP. The importance of this work relies on the fact that the results confirm the high diagnostic quality and the important radiation dose sparing of whole body CT scan examination obtained with a low-dose setting protocol combined with the new state of art iterative reconstruction algorithm in comparison with a standard-dose protocol. Moreover in this manuscript the authors compared and commented the results with those of previous literature on this field by using different vendor approach.
Terminology
MDCT: Multidetector row-CT are new generation of CT scanner with high number of detector, which allow to obtain high spatial resolution images with thinner collimation; FBP: Filtered back projection (FBP) has been the industry standard for CT image reconstruction for decades, representing a very fast and fairly robust method to reconstruct the raw data obtained from routinely CT scan acquisition; Hybrid Iterative Reconstruction Algorithms: In the literature, the term hybrid IR usually refers to algorithms that mainly decrease image noise by iterative methods. IR approaches are not new and were, in fact, the initially proposed method for data reconstruction in the early days of CT technology during the 1970s. However, due to its mathematically demanding properties and the large amount of data in CT imaging, until recently IR has not been practical for clinical purposes. The current evidence on the clinical implementation of IR into CT protocols shows substantial promise for major improvements in image quality, chiefly noise reduction-with subsequent radiation dose reduction-and artifact suppression; iDose4: iDose4 is a fourth-generation hybrid IR algorithm introduced by Philips Healthcare. With this algorithm the noise can be controlled for high spatial resolution reconstructions, hence providing high-quality, low-contrast, and spatial resolution within the same image, when radiologist work with low dose approach; through an iterative mathematical process, the noisy data are penalized and edges are preserved.
Peer-review
This is a very interesting attempt to achieve lower radiation dose in follow-up CT of oncologic patients with parallel comparison of thorax-abdomen-pelvis CT with 4th generation hybrid iterative reconstruction algorithm and standard dose examination.
Footnotes
Institutional review board statement: The study was reviewed and approved by the H. San Gerardo Institutional Review Board.
Informed consent statement: Every patient gave his informed consent, as required by our Institution.
Conflict-of-interest statement: All the authors are aware of the content of the manuscript and have no conflict of interest.
Data sharing statement: No additional data are available.
Manuscript source: Invited manuscript
Specialty type: Oncology
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: May 17, 2017
First decision: July 11, 2017
Article in press: August 17, 2017
P- Reviewer: Funel N, Mastoraki A S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
Contributor Information
Davide Ippolito, Department of Diagnostic Radiology, “San Gerardo” Hospital, 20900 Monza, Italy; School of Medicine, University of Milano-Bicocca, 20900 Monza, Italy. davide.atena@tiscalinet.it.
Alessandra Silvia Casiraghi, Department of Diagnostic Radiology, “San Gerardo” Hospital, 20900 Monza, Italy; School of Medicine, University of Milano-Bicocca, 20900 Monza, Italy.
Cammillo Talei Franzesi, Department of Diagnostic Radiology, “San Gerardo” Hospital, 20900 Monza, Italy; School of Medicine, University of Milano-Bicocca, 20900 Monza, Italy.
Davide Fior, Department of Diagnostic Radiology, “San Gerardo” Hospital, 20900 Monza, Italy; School of Medicine, University of Milano-Bicocca, 20900 Monza, Italy.
Franca Meloni, School of Medicine, University of Milano-Bicocca, 20900 Monza, Italy.
Sandro Sironi, School of Medicine, University of Milano-Bicocca, 20900 Monza, Italy; Department of Diagnostic Radiology, “Papa Giovanni XXIII” Hospital, 24127 Bergamo, Italy.
References
- 1.Schauer DA, Linton OW. NCRP Report No. 160, Ionizing Radiation Exposure of the Population of the United States, medical exposure--are we doing less with more, and is there a role for health physicists? Health Phys. 2009;97:1–5. doi: 10.1097/01.HP.0000356672.44380.b7. [DOI] [PubMed] [Google Scholar]
- 2.Schauer DA, Linton OW. National Council on Radiation Protection and Measurements report shows substantial medical exposure increase. Radiology. 2009;253:293–296. doi: 10.1148/radiol.2532090494. [DOI] [PubMed] [Google Scholar]
- 3.Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 4.Padhani AR. Imaging in the evaluation of cancer. Recommendations for cross-sectional imaging in cancer management, Second edition. In: Nicholson T (ed), editor. London: The Royal College of Radiologists; 2014. [Google Scholar]
- 5.Williams S. General techniques for examinations discussing CT, biopsy and MRI. Recommendations for cross-sectional imaging in cancer management, Second edition. In: Nicholson T, editor. London: The Royal College of Radiologists; 2014. [Google Scholar]
- 6.European Society of Radiology (ESR) White paper on radiation protection by the European Society of Radiology. Insights Imaging. 2011;2:357–362. doi: 10.1007/s13244-011-0108-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tamm EP, Rong XJ, Cody DD, Ernst RD, Fitzgerald NE, Kundra V. Quality initiatives: CT radiation dose reduction: how to implement change without sacrificing diagnostic quality. Radiographics. 2011;31:1823–1832. doi: 10.1148/rg.317115027. [DOI] [PubMed] [Google Scholar]
- 8.iDose4 iterative reconstruction technique, White Paper. Philips Healthcare, 2011. [Google Scholar]
- 9.Willemink MJ, de Jong PA, Leiner T, de Heer LM, Nievelstein RA, Budde RP, Schilham AM. Iterative reconstruction techniques for computed tomography Part 1: technical principles. Eur Radiol. 2013;23:1623–1631. doi: 10.1007/s00330-012-2765-y. [DOI] [PubMed] [Google Scholar]
- 10.Healthcare P. 2009. The Brilliance iCT and DoseWise strategies. Healthcarepapers; pp. 1–24. [Google Scholar]
- 11.Landis JR, Koch GG. A one-way components of variance model for categorical data. Biometrics. 1977;33:67–679. [Google Scholar]
- 12.Arapakis I, Efstathopoulos E, Tsitsia V, Kordolaimi S, Economopoulos N, Argentos S, Ploussi A, Alexopoulou E. Using “iDose4” iterative reconstruction algorithm in adults’ chest-abdomen-pelvis CT examinations: effect on image quality in relation to patient radiation exposure. Br J Radiol. 2014;87:20130613. doi: 10.1259/bjr.20130613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karpitschka M, Augart D, Becker HC, Reiser M, Graser A. Dose reduction in oncological staging multidetector CT: effect of iterative reconstruction. Br J Radiol. 2013;86:20120224. doi: 10.1259/bjr.20120224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prakash P, Kalra MK, Kambadakone AK, Pien H, Hsieh J, Blake MA, Sahani DV. Reducing abdominal CT radiation dose with adaptive statistical iterative reconstruction technique. Invest Radiol. 2010;45:202–210. doi: 10.1097/RLI.ob013e3181dzfeec. [DOI] [PubMed] [Google Scholar]
- 15.May MS, Wüst W, Brand M, Stahl C, Allmendinger T, Schmidt B, Uder M, Lell MM. Dose reduction in abdominal computed tomography: intraindividual comparison of image quality of full-dose standard and half-dose iterative reconstructions with dual-source computed tomography. Invest Radiol. 2011;46:465–470. doi: 10.1097/RLI.0b013e31821690a1. [DOI] [PubMed] [Google Scholar]
- 16.Chang W, Lee JM, Lee K, Yoon JH, Yu MH, Han JK, Choi BI. Assessment of a model-based, iterative reconstruction algorithm (MBIR) regarding image quality and dose reduction in liver computed tomography. Invest Radiol. 2013;48:598–606. doi: 10.1097/RLI.0b013e3182899104. [DOI] [PubMed] [Google Scholar]
- 17.Kaul D, Grupp U, Kahn J, Ghadjar P, Wiener E, Hamm B, Streitparth F. Reducing radiation dose in the diagnosis of pulmonary embolism using adaptive statistical iterative reconstruction and lower tube potential in computed tomography. Eur Radiol. 2014;24:2685–2691. doi: 10.1007/s00330-014-3290-y. [DOI] [PubMed] [Google Scholar]
- 18.Vardhanabhuti V, Riordan RD, Mitchell GR, Hyde C, Roobottom CA. Image comparative assessment using iterative reconstructions: clinical comparison of low-dose abdominal/pelvic computed tomography between adaptive statistical, model-based iterative reconstructions and traditional filtered back projection in 65 patients. Invest Radiol. 2014;49:209–216. doi: 10.1097/RLI.0000000000000017. [DOI] [PubMed] [Google Scholar]
- 19.Ren Q, Dewan SK, Li M, Li J, Mao D, Wang Z, Hua Y. Comparison of adaptive statistical iterative and filtered back projection reconstruction techniques in brain CT. Eur J Radiol. 2012;81:2597–2601. doi: 10.1016/j.ejrad.2011.12.041. [DOI] [PubMed] [Google Scholar]
- 20.Singh S, Kalra MK, Shenoy-Bhangle AS, Saini A, Gervais DA, Westra SJ, Thrall JH. Radiation dose reduction with hybrid iterative reconstruction for pediatric CT. Radiology. 2012;263:537–546. doi: 10.1148/radiol.12110268. [DOI] [PubMed] [Google Scholar]
- 21.Pontana F, Duhamel A, Pagniez J, Flohr T, Faivre JB, Hachulla AL, Remy J, Remy-Jardin M. Chest computed tomography using iterative reconstruction vs filtered back projection (Part 2): image quality of low-dose CT examinations in 80 patients. Eur Radiol. 2011;21:636–643. doi: 10.1007/s00330-010-1991-4. [DOI] [PubMed] [Google Scholar]
- 22.Hosch W, Stiller W, Mueller D, Gitsioudis G, Welzel J, Dadrich M, Buss SJ, Giannitsis E, Kauczor HU, Katus HA, et al. Reduction of radiation exposure and improvement of image quality with BMI-adapted prospective cardiac computed tomography and iterative reconstruction. Eur J Radiol. 2012;81:3568–3576. doi: 10.1016/j.ejrad.2011.06.055. [DOI] [PubMed] [Google Scholar]
- 23.Schindera ST, Nelson RC, Toth TL, Nguyen GT, Toncheva GI, DeLong DM, Yoshizumi TT. Effect of patient size on radiation dose for abdominal MDCT with automatic tube current modulation: phantom study. AJR Am J Roentgenol. 2008;190:W100–W105. doi: 10.2214/AJR.07.2891. [DOI] [PubMed] [Google Scholar]
- 24.Scharf M, Brendel S, Melzer K, Hentschke C, May M, Uder M, Lell MM. Image quality, diagnostic accuracy, and potential for radiation dose reduction in thoracoabdominal CT, using Sinogram Affirmed Iterative Reconstruction (SAFIRE) technique in a longitudinal study. PLoS One. 2017;12:e0180302. doi: 10.1371/journal.pone.0180302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bodelle B, Isler S, Scholtz JE, Frellesen C, Luboldt W, Vogl TJ, Beeres M. Benefits of sinogram-affirmed iterative reconstruction in 0.4 mSv ultra-low-dose CT of the upper abdomen following transarterial chemoembolisation: comparison to low-dose and standard-dose CT and filtered back projection technique. Clin Radiol. 2016;71:e11–e15. doi: 10.1016/j.crad.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 26.Song JS, Lee JM, Sohn JY, Yoon JH, Han JK, Choi BI. Hybrid iterative reconstruction technique for liver CT scans for image noise reduction and image quality improvement: evaluation of the optimal iterative reconstruction strengths. Radiol Med. 2015;120:259–267. doi: 10.1007/s11547-014-0441-9. [DOI] [PubMed] [Google Scholar]


