Abstract
Endoscopic pancreatic stenting has been widely used in various pancreatic conditions. With the increasing use of pancreatic stents, many complications have been recognized. Especially, proximal stent migration presents a serious condition because of subsequent pancreatic duct obstruction, impaired drainage, ductal dilation, and pancreatic pain. Although endoscopic retrieval is the preferred treatment for proximally migrated pancreatic stents, it is not always successful, resulting in conversion to surgery. To date, endoscopic ultrasound-guided pancreatic duct drainage (EUS-PD) has never been reported for treatment of pancreatic duct obstruction caused by proximally migrated pancreatic stent. We herein describe a case of pancreatic duct rupture and obstruction caused by proximally migrated pancreatic stent that was successfully treated by EUS-guided pancreaticogastrostomy while keeping the former stent in situ after failed endoscopic retrograde cholangiopancreatography. We believe that this report adds to the increasing evidence of symptomatic pancreatic duct obstruction being successfully treated by EUS-PD.
Keywords: Endoscopic retrograde cholangiopancreatography, Pancreatic stent, Stent migration, Pancreatic duct obstruction, Endoscopic ultrasound-guided pancreatic duct drainage
Core tip: Stent migration is a rare complication of pancreatic stenting. Especially, proximal migration presents a serious condition because of subsequent pancreatic duct obstruction, impaired drainage, and pancreatic pain. We described a case of symptomatic pancreatic duct obstruction caused by proximally migrated pancreatic stent that was successfully treated by endoscopic ultrasound-guided pancreatic duct drainage (EUS-PD) while keeping the former stent in situ. To the best of our knowledge, EUS-PD has never been reported for relief of pancreatic duct obstruction caused by proximally migrated pancreatic stent, and this report adds to the increasing evidence of the safety and effectiveness of EUS-PD.
INTRODUCTION
Endoscopic pancreatic stenting has become an accepted therapy for various pancreatic diseases, including pancreatic duct obstruction due to benign strictures, stones, or tumors, drainage of pancreatic pseudocysts, symptomatic pancreaticobiliary anomalies, and preventing post-ERCP pancreatitis (PEP)[1,2]. With the increasing use of pancreatic stents, various complications have been recognized, such as bleeding, infection, stent occlusion, duodenal perforation, stent fracture, and PEP. Especially, proximal stent migration is a rare complication and presents a serious condition because of subsequent pancreatic duct obstruction, impaired drainage, ductal dilation, and pancreatic pain[3]. Although endoscopic removal of proximally migrated stents can be quite effective, it is not always successful, resulting in conversion to surgery[4]. Endoscopic ultrasound-guided pancreatic duct drainage (EUS-PD) is a promising option for pancreatic duct decompression after failed endoscopic retrograde cholangiopancreatography (ERCP)[5], however, it has never been reported for relief of pancreatic duct obstruction caused by proximally migrated pancreatic stent. We herein report a case of a 78-year-old woman with symptomatic pancreatic duct obstruction caused by proximally migrated pancreatic stent that was recovered via EUS-guided pancreaticogastrostomy (EPG).
CASE REPORT
A 78-year-old woman was admitted to our hospital with epigastric discomfort of three months’ history. On admission, she appeared ill, vitally stable, not jaundiced, and her abdomen was soft but mild tenderness over the epigastrium. Laboratory data were within the normal ranges. Abdominal computed tomography (CT) showed a bright linear object extending from the main pancreatic duct (MPD) and parenchyma into the lesser omental bursa along with a dilated distal MPD (Figure 1).
Figure 1.
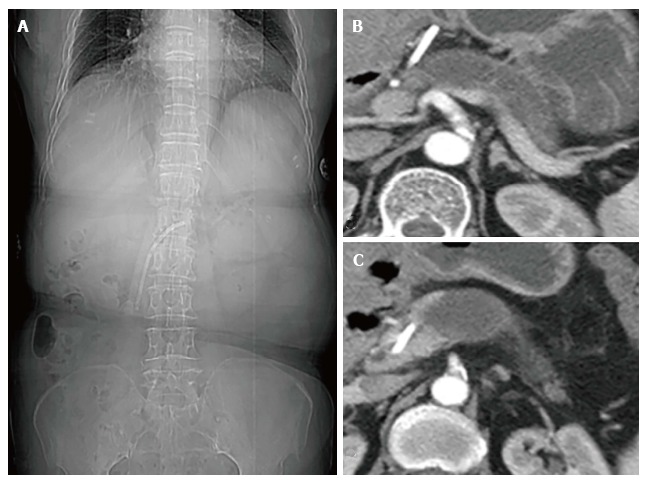
Abdominal computed tomography. A: Computed tomography image showing a pancreatic stent; B and C: An endoprosthesis extending from the main pancreatic duct (MPD) and parenchyma into the lesser omental bursa with a dilated distal MPD.
The patient’s medical history revealed recurrent acute pancreatitis during the past 7 years. At 71 years of age, she experienced the first attack of acute pancreatitis. Further examination excluded the possibilities of biliary, alcoholic or hyperlipidemic causes. ERCP was then performed and demonstrated a stricture of the head segment of MPD. A positron emission tomography/computed tomography (PET-CT) was performed for further evaluation and no pancreatic mass was detected. For reliving the stricture of MPD, a pancreatic stent was inserted by ERCP and the patient achieved symptomatic relief at discharge. However, regular stent exchange was refused by the patient for fear of endoscopic procedure. Thereafter, she had several episodes of acute pancreatitis and occasional epigastric pain which were all managed conservatively. She could not remember which type of pancreatic stent was used after 7 years.
In view of her medical history and imaging findings, a possibility of pancreatic duct obstruction due to a proximally migrated pancreatic stent was considered and we attempted to drain the MPD to relieve her symptoms. Endoscopic transpapillary treatment was failed because of pyloric deformation preventing access to the second portion of the duodenum. After a brief discussion with the patient’s family and obtaining their consent, we decided to perform endoscopic ultrasound-guided pancreaticogastrostomy (EPG) while keeping the former stent in situ. The dilated MPD was punctured transgastrically with a 19gauge needle (Echotip 19A; Cook Medical Inc., United States) (Figure 2A), and a sample was aspirated for further testing. Under fluoroscopy, pancreatogram displayed the dilated pancreatic duct proximal to complete obstruction (Figure 2B). After introduction of a 0.035-inch guidewire (Jagwire, Boston Scientific) into the MPD, the EUS needle was removed (Figure 2C), and a 6 Fr cystotome (Cook Endoscopy) was used to dilate the tract. Finally, the pancreaticogastrostomy was then stented with a 6-Fr double pigtail stent (Figure 2D). The amylase concentration of the effusion was 72450 U/L, while CEA and CA-199 were within the normal range. The patient revealed great resolution of abdominal pain, which was confirmed by CT scanning performed after 1 wk (Figure 3). There were no adverse events, and the patient remains asymptomatic at present (five months after the EPG procedure). We planned to make the follow-up investigations (endoscopic ultrasonography) for the possible stent occlusion and pancreatic duct obstruction after 6 mo and then once a year. Stent exchange under EUS is planned if recurrent acute pancreatitis occur.
Figure 2.
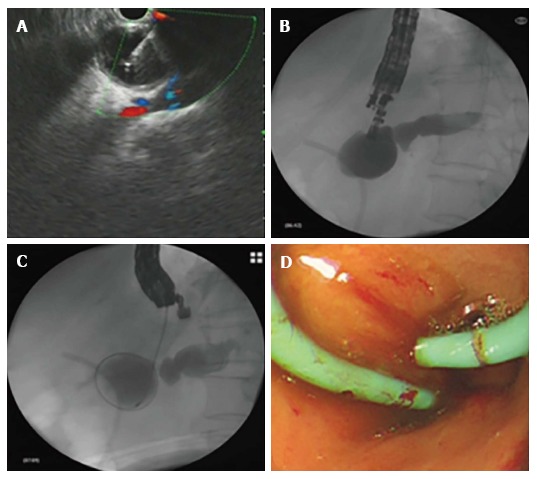
Endoscopic ultrasound-guided pancreaticogastrostomy. A: Endoscopic ultrasound-guided puncture; B and C: Contrast injection and cystotome advancement; D: Double pigtail stent placement.
Figure 3.
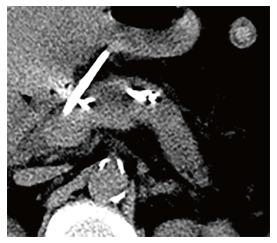
Successful decompression of the dilated main pancreatic duct.
DISCUSSION
Stent migration is an infrequent complication of endoscopic pancreatic stenting. Distal stent migration has been reported in 7.5% of pancreatic stent placement[3]. This rarely presents a problem since the stent can clear from the intestine spontaneously. However, proximal stent migration can result in serious complications, including ductal damage, recurrent pancreatitis, impaction and subsequent difficulty to retrieve the migrated stent[3]. In the case presented, the proximal stent tip migrated into the lesser omental bursa, which resulted in duct distortion and obstruction, and eventually symptomatic pancreatic duct hypertension. This patient had never undergone stent revision or retrieval since its placement 7 years earlier. Her history of long term recurrent acute pancreatitis might indicate stent migration and subsequent pancreatic duct obstruction, however, which was unfortunately ignored during her previous hospitalization.
Currently, ERCP is the preferred procedure for treating pancreatic duct obstruction. However, it may not be feasible in approximately 3% to 10% of patients because of surgically altered anatomy, complete ductal obstructions, or disrupted ducts. In these cases, percutaneous radiologic intervention or surgical treatment is required[6]. However, both methods have been associated with significant morbidity and mortality rates. The development of EUS allowed the ability to visualize the pancreatic ductal system, and introduction of the therapeutic linear echoendoscope allowed access to the pancreatic duct with a needle in the case of ERCP failure. EUS-PD was first described by Bataille et al[7] in 2002. Following this report, several case series with satisfactory results have been published[8-10]. Technically, EUS-PD can either be performed via a rendezvous technique, combining EUS and ERCP, or via a transluminal technique. The former should be attempted in patients with accessible ampulla. Actually, in the present case, the echoendoscope cannot access the second part of duodenum because of pyloric deformation, and EUS-PD with transmural stenting seems to be the primary intervention.
To date, EUS-PD remains one of the most technically challenging endosonography interventions[11]. Success rates vary widely and adverse events occur in approximately 15% of reported cases[12]. Mainly, EUS-PD might be associated with complications such as pancreatitis, hemorrhage, stent migration, stent dysfunction, perforation, pneumoperitoneum, pancreatic juice leakage as well as abscess formation. Although there was no procedure related mortality, severe adverse events were noted when pancreatic drainage failed, and EUS-PD should be performed in endoscopic units experienced in therapeutic endoscopy[13].
Endoscopic retrieval is the primary treatment modality for proximally migrated pancreatic stents[4]. Matsumoto et al[4] reported that the successful endoscopic retrieval rate for proximally migrated pancreatic stents was approximately 80%. In the presented case, endoscopic transpapillary removal of the migrated stent was impossible because of pyloric deformation, and surgical intervention is too invasive for patients with benign cause. Once the pancreatic duct decompression was achieved, it does not seem necessary to remove the migrated pancreatic stent, which entails little damage to her health.
In conclusion, proximal migration of a pancreatic stent into the lesser omental bursa resulting in distortion and obstruction of the MPD, and symptomatic pancreatic duct dilation is a rare and catastrophic complication of pancreatic stenting. EUS-PD appears to be an effective and safe treatment for MPD decompression when conventional ERCP fails. This report adds to the increasing evidence of symptomatic pancreatic duct obstruction being successfully treated by EUS-PD.
COMMENTS
Case characteristics
A 78-year-old woman with endoscopic pancreatic duct stenting 7 years earlier presented with epigastric discomfort of three months’ history.
Clinical diagnosis
The patient had a history of recurrent acute pancreatitis within 7 years. After admission to the hospital, CT scan showed a bright linear object extending from the main pancreatic duct (MPD) and parenchyma into the lesser omental bursa along with a dilated distal MPD.
Laboratory diagnosis
All laboratory data were within normal limits.
Imaging diagnosis
Computed tomography scan revealed a bright linear object extending from the MPD and parenchyma into the lesser omental bursa along with a dilated distal MPD.
Treatment
Endoscopic ultrasound-guided pancreatic duct drainage (EUS-PD) was performed after failed endoscopic retrieval.
Related reports
There is no related report about EUS-PD for pancreatic duct obstruction caused by proximally migrated pancreatic stent.
Experiences and lessons
Proximal stent migration is an infrequent complication of endoscopic pancreatic stenting and can sometimes result in serious complications including pancreatic duct obstruction, pancreatic pain and acute pancreatitis. Endoscopic retrieval is the primary treatment modality for proximal migrated pancreatic stents. EUS-PD is feasible and safe for pancreatic duct drainage, as well as symptomatic relief if endoscopic retrieval has failed.
Peer-review
The authors propose the migration of a proximal pancreatic duct stent, which cannot be removed by ERCP, as a new indication for EUS-PD. This interesting case report adds to the increasing evidence of the use of EUS-PD as an effective and safe treatment for pancreatic duct decompression.
Footnotes
Institutional review board statement: This case report was reviewed and approved by the Hangzhou First People’s Hospital Institutional Review Board.
Informed consent statement: All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement: All the authors have no conflicts of interests to declare.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: March 29, 2017
First decision: May 8, 2017
Article in press: July 3, 2017
P- Reviewer: Hijioka S, Nakai Y, Reeh M S- Editor: Qi Y L- Editor: A E- Editor: Lu YJ
Contributor Information
Lei Lu, Department of Gastroenterology, Hangzhou First People’s Hospital, Nanjing Medical University, Hangzhou 310000, Zhejiang Province, China.
Hang-Bin Jin, Department of Gastroenterology, Hangzhou First People’s Hospital, Nanjing Medical University, Hangzhou 310000, Zhejiang Province, China.
Jian-Feng Yang, Department of Gastroenterology, Hangzhou First People’s Hospital, Nanjing Medical University, Hangzhou 310000, Zhejiang Province, China.
Xiao-Feng Zhang, Department of Gastroenterology, Hangzhou First People’s Hospital, Nanjing Medical University, Hangzhou 310000, Zhejiang Province, China. zxf837@tom.com.
References
- 1.Binmoeller KF, Jue P, Seifert H, Nam WC, Izbicki J, Soehendra N. Endoscopic pancreatic stent drainage in chronic pancreatitis and a dominant stricture: long-term results. Endoscopy. 1995;27:638–644. doi: 10.1055/s-2007-1005780. [DOI] [PubMed] [Google Scholar]
- 2.Freeman ML, Guda NM. Prevention of post-ERCP pancreatitis: a comprehensive review. Gastrointest Endosc. 2004;59:845–864. doi: 10.1016/s0016-5107(04)00353-0. [DOI] [PubMed] [Google Scholar]
- 3.Johanson JF, Schmalz MJ, Geenen JE. Incidence and risk factors for biliary and pancreatic stent migration. Gastrointest Endosc. 1992;38:341–346. doi: 10.1016/s0016-5107(92)70429-5. [DOI] [PubMed] [Google Scholar]
- 4.Matsumoto K, Katanuma A, Maguchi H. Endoscopic removal technique of migrated pancreatic plastic stents. J Hepatobiliary Pancreat Sci. 2014;21:E34–E40. doi: 10.1002/jhbp.94. [DOI] [PubMed] [Google Scholar]
- 5.Kahaleh M, Artifon EL, Perez-Miranda M, Gaidhane M, Rondon C, Itoi T, Giovannini M. Endoscopic ultrasonography guided drainage: summary of consortium meeting, May 21, 2012, San Diego, California. World J Gastroenterol. 2015;21:726–741. doi: 10.3748/wjg.v21.i3.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fujii LL, Topazian MD, Abu Dayyeh BK, Baron TH, Chari ST, Farnell MB, Gleeson FC, Gostout CJ, Kendrick ML, Pearson RK, et al. EUS-guided pancreatic duct intervention: outcomes of a single tertiary-care referral center experience. Gastrointest Endosc. 2013;78:854–864.e1. doi: 10.1016/j.gie.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 7.Bataille L, Deprez P. A new application for therapeutic EUS: main pancreatic duct drainage with a “pancreatic rendezvous technique”. Gastrointest Endosc. 2002;55:740–743. doi: 10.1067/mge.2002.123621. [DOI] [PubMed] [Google Scholar]
- 8.Tessier G, Bories E, Arvanitakis M, Hittelet A, Pesenti C, Le Moine O, Giovannini M, Devière J. EUS-guided pancreatogastrostomy and pancreatobulbostomy for the treatment of pain in patients with pancreatic ductal dilatation inaccessible for transpapillary endoscopic therapy. Gastrointest Endosc. 2007;65:233–241. doi: 10.1016/j.gie.2006.06.029. [DOI] [PubMed] [Google Scholar]
- 9.Ergun M, Aouattah T, Gillain C, Gigot JF, Hubert C, Deprez PH. Endoscopic ultrasound-guided transluminal drainage of pancreatic duct obstruction: long-term outcome. Endoscopy. 2011;43:518–525. doi: 10.1055/s-0030-1256333. [DOI] [PubMed] [Google Scholar]
- 10.Oh D, Park do H, Cho MK, Nam K, Song TJ, Lee SS, Seo DW, Lee SK, Kim MH. Feasibility and safety of a fully covered self-expandable metal stent with antimigration properties for EUS-guided pancreatic duct drainage: early and midterm outcomes (with video) Gastrointest Endosc. 2016;83:366–373. doi: 10.1016/j.gie.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 11.Dhir V, Isayama H, Itoi T, Almadi M, Siripun A, Teoh AYB, Ho KY. Endoscopic ultrasonography-guided biliary and pancreatic duct interventions. Dig Endosc. 2017;29:472–485. doi: 10.1111/den.12818. [DOI] [PubMed] [Google Scholar]
- 12.Giovannini M. EUS-guided pancreatic duct drainage: ready for prime time? Gastrointest Endosc. 2013;78:865–867. doi: 10.1016/j.gie.2013.10.019. [DOI] [PubMed] [Google Scholar]
- 13.Itoi T, Yasuda I, Kurihara T, Itokawa F, Kasuya K. Technique of endoscopic ultrasonography-guided pancreatic duct intervention (with videos) J Hepatobiliary Pancreat Sci. 2014;21:E4–E9. doi: 10.1002/jhbp.43. [DOI] [PubMed] [Google Scholar]


