Abstract
Angiosarcoma of the heart is an uncommon soft tissue sarcoma. A few cases of disseminated intravascular coagulation (DIC) associated with angiosarcoma occurring in various organs, but not the heart, have been reported. Although taxane is commonly used in the treatment of metastatic angiosarcoma, data on the efficacy of nab-paclitaxel for angiosarcoma are limited. Here, we report probably the first case of a patient with primary cardiac angiosarcoma with coexisting DIC who was successfully treated with nab-paclitaxel. A 62-year-old female with chief complaints of nausea and shortness of breath was diagnosed as having cardiac angiosarcoma with liver metastases. Four months after the resection of her primary tumor, the hepatic metastatic lesions progressed rapidly accompanied by new metastatic lesions in the right iliac bone and signs of DIC. She received nab-paclitaxel as first-line chemotherapy. A response of stable disease was achieved after 2 treatment cycles and DIC was successfully controlled for at least 4 months. This report suggests potential utility of nab-paclitaxel for angiosarcoma complicated with DIC. We also review the literature for all cases of angiosarcoma with DIC reported so far.
Keywords: Angiosarcoma, Heart, Disseminated intravascular coagulation, Kasabach-Merritt phenomenon, Nab-paclitaxel
Introduction
Angiosarcoma is a rare malignancy of endothelial origin, accounting for about 2–4% of all soft tissue sarcomas [1]. Angiosarcomas can originate in any part of the body such as the skin, viscera, and soft tissue. In a pooled data analysis involving 534 patients, the prevalence of angiosarcoma was 27.0% in the head and neck, 19.7% in the breast, 15.3% in extremities, 9.5% in the trunk, 6.0% in the liver, and 4.7% in the heart [1]. Cardiac angiosarcoma typically occurs in the right atrium and is usually advanced at presentation. Cardiac angiosarcoma is often overlooked as an initial diagnosis because of its rarity and lack of specific symptoms.
There have been a few reported cases of angiosarcoma with coagulation abnormalities including disseminated intravascular coagulation (DIC) [2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17]. In one report, 7 (16.7%) of 42 patients who had angiosarcoma were diagnosed as having DIC [2]. Thus, DIC is not an uncommon complication associated with angiosarcoma and offers a challenge to angiosarcoma treatment.
Anthracyclines, ifosfamide, and taxanes are used to treat metastatic angiosarcoma [1]. In contrast to other soft tissue sarcomas, angiosarcomas are particularly responsive to taxanes, especially paclitaxel [1]. Although 2 case reports regarding the use of nab-paclitaxel for treating angiosarcoma are available, there is no report on successful treatment of angiosarcoma complicated with DIC [18, 19]. Nab-paclitaxel is nanoparticle albumin-bound paclitaxel and is approved for the treatment of breast cancer, gastric cancer, non-small cell lung cancer, and pancreatic cancer in Japan.
Here, we report a rare case of an advanced primary cardiac angiosarcoma associated with DIC who was successfully treated with nab-paclitaxel.
Case Presentation
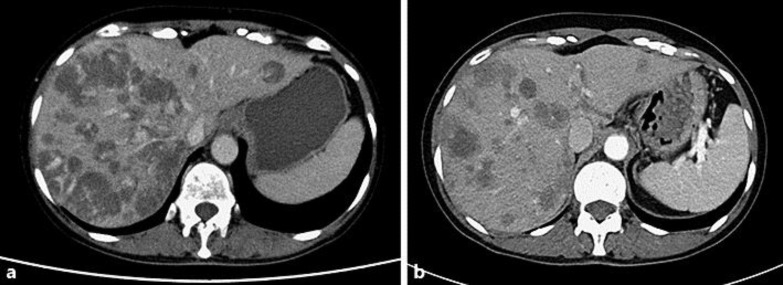
A 62-year-old woman presented to her primary physician with complaints of nausea for 3 days. Radiographic evaluation revealed a tumor of 6 cm in the right atrium and multiple liver metastases. She already had symptoms of heart failure, such as shortness of breath, at presentation. Resection of the primary tumor was performed urgently on the next day of her first visit. The tumor was located in the right atrium and invaded the superior vena cava and right ventricle. The resection margin was positive. Histological examination showed several vascular lumens surrounded by round or spindle tumor cells. Immunohistochemistry revealed CD34 positive, CD31 positive, FVIIIa positive, S-100 negative, and a Ki-67 index of 10%, corresponding to angiosarcoma. TNM staging was T2N0M1, but no additional treatment (such as chemotherapy) was performed for reasons not clearly known. She presented with right proximal leg pain 4 months after surgery, and CT scan revealed rapid progression of multiple liver metastases well enhanced by contrast as well as multiple metastases to the right ilium (Fig. 1a).
Fig. 1.
CT evaluation before (a) and after (b) the start of chemotherapy.
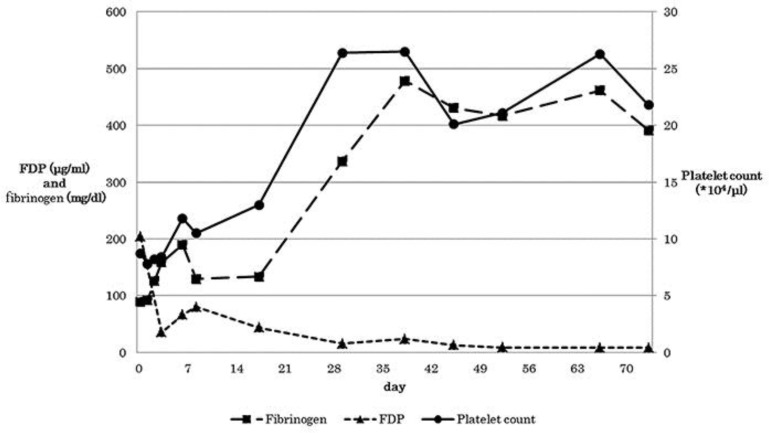
She was referred to our hospital immediately after confirmation of disease progression. She had no family history of malignancy. She had never smoked and was allergic to alcohol. Physical examination showed no abnormalities except for multiple hemorrhagic macules at extremities. Blood test showed coagulation abnormalities (platelets 8.7 × 104 /µl, a low fibrinogen level of 89.3 mg/dL, prolonged prothrombin and activated partial thromboplastin time of 65.7% and 40.5 s, respectively) and high levels of fibrin degradation products (203.6 μg/mL) and D-dimer (110.3 μg/mL). Based on these data, we diagnosed her condition as DIC associated with angiosarcoma. She was admitted immediately and received fresh-frozen plasma and recombinant thrombomodulin-α. Recombinant thrombomodulin-α was used for 6 days in order to reduce the consumption of coagulation factors induced by thrombosis. Nab-paclitaxel was started on the next day at a dose of 100 mg/m2 as a 3 weeks on/1 week off regimen. We selected nab-paclitaxel instead of paclitaxel because paclitaxel contains alcohol and the patient was allergic to alcohol. Coagulation abnormalities improved shortly after the initiation of chemotherapy (Fig. 2). She was discharged on day 11 after starting nab-paclitaxel. After 2 cycles of nab-paclitaxel, CT scan showed shrinkage in tumor size by around 9% with appreciable decrease in enhancement among the multiple liver metastases (Fig. 1b). There was no relapse of DIC and no evidence of local recurrence despite positive surgical margin. Response evaluation according to Response Evaluation Criteria in Solid Tumor version 1.1 was stable disease. Adverse events were relatively mild, except for cumulative sensory peripheral neuropathy up to grade 2 according to Common Terminology Criteria for Adverse Events version 4.0. Currently, 4 months after the initial chemotherapy, the patient is continuing to receive nab-paclitaxel at our outpatient chemotherapy center without disease progression and relapse of DIC. She is currently on her 6th cycle of nab-paclitaxel.
Fig. 2.
Changes in platelet count and coagulation parameters during treatment. Closed squares, closed triangles, and closed circles describe fibrinogen, FDP, and platelet counts, respectively. Day 0 was the day on which the patient was referred to our hospital.
Discussion
To our knowledge, this is the first report of a patient with cardiac angiosarcoma with DIC who was successfully treated with nab-paclitaxel. Primary angiosarcoma of the heart is an uncommon tumor; however, angiosarcoma is the most common histologic subtype among all cardiac sarcomas.
DIC is often observed as a complication of advanced disease in several malignancies. Advanced angiosarcoma is more frequently associated with coagulation disorders than other sarcomas [2], although the reasons for this association are unclear. One possible hypothesis for this association could be the Kasabach-Merritt phenomenon (KMP). The KMP is a life-threatening complication occurring in approximately 70% of cases of kaposiform hemangioendothelioma and 10% of tufted angioma, and is characterized by severe thrombocytopenia and consumption coagulation abnormality such as DIC [20, 21]. However, the term KMP has recently been used indiscriminately to describe thrombocytopenia or coagulation abnormalities associated with any vascular anomaly.
Anthracyclines, ifosfamide, and taxanes are the standard cytotoxics used to treat metastatic angiosarcoma [1]. In addition, several molecular targeted agents, including bevacizumab, sunitinib, and sorafenib, have shown potential efficacy in the treatment of angiosarcoma [1]. However, the experience with the use of molecular targeted agents among patients with DIC is limited because these are newer agents that have only been recently available. These targeted drugs are also usually contraindicated in DIC because of their propensity to cause bleeding or thrombosis due to the inhibition of the antivascular endothelial growth factor/antivascular endothelial growth factor receptor axis. So far, to the best of our knowledge, there are only 2 case reports of treatment with nab-paclitaxel in patients with angiosarcoma; both without associated DIC [18, 19]. In a report by Hara et al. [18], remarkable regression was achieved in a patient with recurrent angiosarcoma of the chest wall after first-line nab-paclitaxel therapy, and the disease was well controlled for a relatively long period. In a report by Olawaiye et al. [19], a patient with angiosarcoma of the uterus experienced complete disappearance of ascites following surgery after having received 6 cycles of nab-paclitaxel and bevacizumab as second-line treatment.
Our literature search identified 22 cases of angiosarcoma associated with coagulation abnormalities reported so far in various primary organs (Table 1) [2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17]. The median age was 67 years (range, 28–87) and 12 patients (55%) were male. The sites of primary tumor were the scalp (n = 6, 27%), liver (n = 6, 27%), breast (n = 5, 23%), heart (n = 1, 5%) and others (n = 4, 18%). There was only 1 case with primary cardiac angiosarcoma [2]. The patient was a 54-year-old female with multiple metastases to the lung, pleura, bones, and bone marrows. She received doxorubicin plus ifosfamide, and DIC was temporarily resolved. However, she died 6 months after her first presentation. Several other patients with angiosarcoma-associated coagulopathy were successfully treated by resection, radiotherapy, or chemotherapy. However, most cases had poor survival of less than 1 year after any type of treatment. Only 1 patient received nab-paclitaxel as fourth-line treatment; however, efficacy was not reported [2]. This patient was a 42-year-old female with primary angiosarcoma in the breast that had metastasized to the chest wall, ribs, and lung. She underwent mastectomy for the treatment of localized disease and received 6 cycles of gemcitabine plus docetaxel followed by radiation as adjuvant therapy. She developed relapse within 11 months after surgery and received various treatments including liposomal doxorubicin plus carboplatin, sirolimus, pazopanib, nab-paclitaxel, bevacizumab, and vinorelbine. She died 11 months after the diagnosis of recurrence.
Table 1.
Literature review of patients with angiosarcoma complicated with DIC
| Case | First author [ref.] | Primary site | Treatment | Survival |
|---|---|---|---|---|
| 1 | Alliot [3] | liver | – | 3 months |
| 2 | Bernathova [4] | breast | C (unknown), S | alive |
| 3 | Farid [2] | liver | C (liposomal doxorubicin) | 9 months |
| 4 | breast | C (liposomal doxorubicin, carboplatin, sirolimus, pazopanib, nab-paclitaxel, bevacizumab, and vinorelbine) | 11 months | |
| 5 | mediastinal | C (doxorubicin, paclitaxel, ifosfamide, cisplatin, gemcitabine, and vinorelbine) | 5 months | |
| 6 | heart | C (doxorubicin and ifosfamide) | 6 months | |
| 7 | breast | C (doxorubicin and ifosfamide) | 11 months | |
| 8 | skull, meninges | – | 1 month | |
| 9 | foot (bony) | – | 2 months | |
| 10 | Fujisawa [5] | spleen | C (docetaxel and paclitaxel) | alive |
| 11 | Habringer [6] | liver | – | – |
| 12 | Imafuku [7] | scalp | C (docetaxel), R | alive (>36 months) |
| 13 | Lespi [8] | liver | – | – |
| 14 | Maeda [9] | scalp | – | – |
| 15 | Massarweh [10] | scalp | – | – |
| 16 | Mazharuddin [11] | liver | – | – |
| 17 | Mazzocchi [12] | breast | S | 8 years |
| 18 | Moussa [13] | breast | – | – |
| 19 | Read [14] | scalp | C (paclitaxel, liposomal doxorubicin, gemcitabine, and vinorelbine) | – |
| 20 | Tan [15] | scalp | R | – |
| 21 | Tordjman [16] | liver or spleen | C (unknown) | 15 months |
| 22 | Wen [17] | scalp | – | – |
C, chemotherapy; S, surgery; R, radiation.
To the best of our knowledge, our report is the first case in the literature describing successful treatment of angiosarcoma complicated with DIC with nab-paclitaxel. However, our report is a case report of a single patient and further studies are necessary to evaluate the true efficacy of nab-paclitaxel in angiosarcoma complicated with DIC.
In conclusion, we report for the first time a case of primary cardiac angiosarcoma complicated with DIC who achieved both improvement in DIC and modest tumor shrinkage with the administration of nab-paclitaxel.
Statement of Ethics
Consent was obtained from the patient and her family for the publication of this case report.
Disclosure Statement
All authors have no conflicts of interest to disclose for this case report.
Acknowledgements
The authors would like to thank Dr. Bishal Gyawali, Nagoya University Hospital for his technical and linguistic assistance.
References
- 1.Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ. Angiosarcoma. Lancet Oncol. 2010;11:983–991. doi: 10.1016/S1470-2045(10)70023-1. [DOI] [PubMed] [Google Scholar]
- 2.Farid M, Ahn L, Brohl A, Cioffi A, Maki RG. Consumptive coagulopathy in angiosarcoma: a recurrent phenomenon? Sarcoma. 2014;2014:617102. doi: 10.1155/2014/617102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alliot C, Tribout B, Barrios M, Gontier MF. Angiosarcoma variant of Kasabach-Merritt syndrome. Eur J Gastroenterol Hepatol. 2001;13:731–734. doi: 10.1097/00042737-200106000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Bernathova M, Jaschke W, Pechlahner C, Zelger B, Bodner G. Primary angiosarcoma of the breast associated Kasabach-Merritt syndrome during pregnancy. Breast. 2006;15:255–258. doi: 10.1016/j.breast.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 5.Fujisawa Y, Nakamura Y, Kawachi Y, Otsuka F. Docetaxel was effective in the management of metastatic angiosarcoma associated with disseminated intravascular coagulation syndrome. Int J Dermatol. 2014;53:e138–e140. doi: 10.1111/j.1365-4632.2012.05671.x. [DOI] [PubMed] [Google Scholar]
- 6.Habringer S, Boekstegers A, Weiss L, Hopfinger G, Meissnitzer T, Melchardt T, et al. Kasabach-Merritt phenomenon in hepatic angiosarcoma. Br J Haematol. 2014;167:716–718. doi: 10.1111/bjh.13049. [DOI] [PubMed] [Google Scholar]
- 7.Imafuku S, Hosokawa C, Moroi Y, Furue M. Kasabach-Merritt syndrome associated with angiosarcoma of the scalp successfully treated with chemoradiotherapy. Acta Derm Venereol. 2008;88:193–194. doi: 10.2340/00015555-0378. [DOI] [PubMed] [Google Scholar]
- 8.Lespi PJ, Alvarez GR, Iannariello MB, Wisnowski C. Hepatic angiosarcoma with disseminated intravascular coagulation. Medicina (B Aires) 1997;57:587–590. [PubMed] [Google Scholar]
- 9.Maeda T, Uchino K, Otani T, Ueda Y. Cutaneous angiosarcoma with difficulty in differential diagnosis of thrombocytopenia. Rinsho Ketsueki. 2010;51:402–406. [PubMed] [Google Scholar]
- 10.Massarweh S, Munis A, Karabakhtsian R, Romond E, Moss J. Metastatic angiosarcoma and Kasabach-Merritt syndrome. Rare Tumors. 2014;6:5366. doi: 10.4081/rt.2014.5366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mazharuddin S, Podduturi V, Guileyardo JM, Cooper B. Hepatic angiosarcoma associated with disseminated intravascular coagulation. Proc (Bayl Univ Med Cent) 2015;28:54–56. doi: 10.1080/08998280.2015.11929186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mazzocchi A, Foschini MP, Marconi F, Eusebi V. Kasabach-Merritt syndrome associated to angiosarcoma of the breast. A case report and review of the literature. Tumori. 1993;79:137–140. doi: 10.1177/030089169307900212. [DOI] [PubMed] [Google Scholar]
- 13.Moussa SH, Oliveira AL, de Amorim AP, Scandiuzzi D, Murta EF, Soares S. Angiosarcoma of the breast associated with Kasabach-Merritt syndrome. Arch Gynecol Obstet. 2002;267:43–45. doi: 10.1007/s004040100224. [DOI] [PubMed] [Google Scholar]
- 14.Read WL, Williams F. Metastatic angiosarcoma with Kasabach-Merritt syndrome responsive to gemcitabine and vinorelbine after failure of liposomal doxorubicin and paclitaxel: a case report. Case Rep Oncol. 2016;9:177–181. doi: 10.1159/000444747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tan SM, Tay YK, Liu TT, Mancer K. Cutaneous angiosarcoma associated with the Kasabach-Merritt syndrome. Ann Acad Med Singapore. 2010;39:941–942. [PubMed] [Google Scholar]
- 16.Tordjman R, Eugene C, Clouet O, Wesenfelder L, Collet C, Bergue A. Hepatosplenic angiosarcoma complicated by hemoperitoneum and disseminated intravascular coagulation. Treatment by arterial embolization and chemotherapy. Gastroenterol Clin Biol. 1995;19:625–628. [PubMed] [Google Scholar]
- 17.Wen S, Zhang W, Yang Y, Sun J. Angiosarcoma of the scalp and face associated with Kasabach-Merritt syndrome and disseminated intravascular coagulation. Indian J Dermatol Venereol Leprol. 2016;82:96–97. doi: 10.4103/0378-6323.172900. [DOI] [PubMed] [Google Scholar]
- 18.Hara N, Fujimoto N, Miyamoto Y, Yamagishi T, Asano M, Fuchimoto Y, et al. Angiosarcoma of the thoracic wall responded well to nanoparticle albumin-bound paclitaxel: a case report. Drug Discov Ther. 2016;10:114–116. doi: 10.5582/ddt.2016.01005. [DOI] [PubMed] [Google Scholar]
- 19.Olawaiye AB, Morgan JA, Goodman A, Fuller AF, Jr, Penson RT. Epithelioid angiosarcoma of the uterus: a review of management. Arch Gynecol Obstet. 2008;278:401–404. doi: 10.1007/s00404-008-0727-z. [DOI] [PubMed] [Google Scholar]
- 20.Croteau SE, Liang MG, Kozakewich HP, Alomari AI, Fishman SJ, Mulliken JB, et al. Kaposiform hemangioendothelioma: atypical features and risks of Kasabach-Merritt phenomenon in 107 referrals. J Pediatr. 2013;162:142–147. doi: 10.1016/j.jpeds.2012.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kelly M. Kasabach-Merritt phenomenon. Pediatr Clin North Am. 2010;57:1085–1089. doi: 10.1016/j.pcl.2010.07.006. [DOI] [PubMed] [Google Scholar]