Abstract
Background
Postoperative hypoparathyroidism is a common complication following total thyroidectomy. The aim of this study was to investigate the incidence of both transient and permanent hypoparathyroidism in patients undergoing total thyroidectomy in a tertiary referral centre and, furthermore, to identify early predictive risk factors.
Methods
Based on a single-institution retrospective review, we identified 582 patients who underwent total thyroidectomy between January 2010 and March 2015. Information on age, gender, pathological diagnosis, duration of surgery, autotransplantation of parathyroid glands, neck dissection, and experience and position of the surgeon was retrieved from the medical records. Furthermore, serum levels of parathyroid hormone and calcium were registered pre- and postoperatively and after 3 and 12 months.
Results
The incidence of transient hypoparathyroidism during the first 24 h and 3 months after surgery was 47.8 and 17.8%, respectively. Furthermore, the incidence of permanent hypoparathyroidism 1 year after surgery was 10.7%. A prolonged duration of surgery was significantly associated with hypoparathyroidism. Moreover, autotransplantation of parathyroid glands was a significant predictor of transient hypoparathyroidism after 24 h and 3 months, but was not associated with permanent hypoparathyroidism.
Conclusions
Transient and permanent hypoparathyroidism is common among patients undergoing total thyroidectomy in a tertiary referral centre. A duration of surgery >120 min constitutes an independent risk factor due to the risk of ischaemic damage. Regain of function of devascularized parathyroid glands must be expected to last at least 1 year postoperatively. Furthermore, the recovery of autotransplanted parathyroid glands should not be evaluated within 1–3 months after surgery.
Keywords: Calcium, Clinical variables, Surgery, Thyroid cancer, Total thyroidectomy, Treatment, Vitamin D
Introduction
One of the most common complications following total thyroidectomy is hypoparathyroidism [1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14] caused by devascularization or accidental resection of one or more of the parathyroid glands [15]. Hypoparathyroidism may be asymptomatic and self-limiting but can also lead to hypocalcaemia with symptoms of paraesthesia and muscle spasms manifesting within the first 24 h after surgery [14]. The incidence of complication varying from 1 to 50% [3, 10, 14, 15, 16] is in part related to the variety of methods used to define the condition. Recent studies have underlined the importance of not only the level of postoperative parathyroid hormone (PTH) but also the reduction in PTH of >50%, compared to the preoperative level, as an indicator of hypoparathyroidism [11, 12].
In the vast majority of cases, hypoparathyroidism is transient, lasting only a few days after surgery, with a temporary substitute treatment need. However, the condition is considered permanent when low PTH persists for at least 6–12 months after surgery [7, 10, 13, 15, 17], affecting only 0.2–10% of patients [3, 10, 15, 16, 17].
During the years, many studies have examined the possible associations between patient characteristics and transient and permanent postoperative hypoparathyroidism in order to prevent these complications and thereby reduce the time and costs associated with prolonged hospitalization [2, 4, 7, 8, 9, 10, 14, 15, 16, 17, 18, 19, 20, 21, 22]. However, conflicting results exist [21]. Thus, no consensus exists regarding the risk assessment of patients undergoing total thyroidectomy in a tertiary referral centre.
The aim of this retrospective study is to determine the risk of postoperative hypoparathyroidism in patients undergoing total thyroidectomy in a tertiary referral centre and, furthermore, to identify potential risk factors.
Methods
Study Design
This is a single-institution, retrospective review of all patients who underwent total thyroidectomy between January 2010 and March 2015 at the Department of Otorhinolaryngology, Rigshospitalet, Copenhagen University Hospital, Denmark. This department has a catchment area covering approximately 50% of the Danish population and represents a tertiary referral centre mainly performing surgery on thyroid cancers and intrathoracic goitres extending more than 5 cm substernally. Patients who underwent total thyroidectomy as part of laryngectomy or other comprehensive surgery or received calcium substitution prior to surgery were excluded.
Surgery
Surgery for thyroid cancer was performed in accordance with DATHYRCA [23], the Danish national guidelines, which were made according to the ATA guidelines, 2015 [24]. A fine needle aspiration biopsy (FNAB) was performed on scintigraphic cold nodules and determined the further surgical treatment. FNAB suspecting follicular, papillary, medullary, or anaplastic carcinoma led to hemithyroidectomy and lymph node exploration level 6. If FNAB or the hemithyroidectomized frozen section revealed carcinoma >2 cm total thyroidectomy was performed. If FNAB revealed a metastasis from a thyroid carcinoma total thyroidectomy was performed.
This study did not include the patients who underwent completion thyroidectomy. If a frozen section confirmed follicular or papillary carcinoma, bilateral central neck dissection was executed. Lateral neck dissection was completed if any perioperative suspicion of metastasis arose, or if the preoperative clinical, cytological, or imaging examination had revealed metastasis-suspected lymph nodes. A lateral neck dissection always followed the performance of a central neck dissection.
The parathyroid gland was transplanted in pieces of 1 × 1 × 1 mm to the sternocleidomastoid muscle if it had appeared devascularized or had been removed during surgery and confirmed by a frozen section.
Outcome Measures
Hypoparathyroidism was defined as serum level of PTH ≤1.6 pmol/L and/or a postoperative decline in serum level of PTH of >50% of the preoperative value.
The serum levels of PTH and calcium were measured preoperatively the day before surgery and postoperatively on the same day of surgery. In addition, patients who complained about mild hypocalcaemic symptoms such as oral paraesthesia, or had a serum level of ionized calcium <1.15 mmol/L but a normal level of PTH, were also categorized as hypoparathyroid. These patients recovered from only a single dose of calcium. Furthermore, the majority of patients had measurements performed 3 months after surgery at an outpatient clinic. Patients still suffering from hypoparathyroidism at the 3-month evaluation were further investigated 1 year after surgery.
From the medical records, we retrieved information on the patients' age, gender, pathological diagnosis, duration of surgery, autotransplantation of parathyroid glands, the experience and position of the surgeon, and duration of hospitalization. Finally, serum levels of PTH and calcium, pre- and postoperatively and after 3 months and 1 year, were collected from the medical records.
Statistics
The statistical analysis was conducted with SPSS version 21. All of the continuous variables showed no normal distribution (Kolmogorov-Smirnov test), hence non-parametric statistics were performed. When comparing 2 independent samples, either the χ2 test or the Mann-Whitney test were used. Multivariate analysis was performed using binary logistic regression. The level of significance was defined as p < 0.05.
Results
Patient Characteristics
A total of 602 patients underwent total thyroidectomy in the period from January 2010 to March 2015, of whom 582 were eligible for inclusion. The median age was 53.5 years and the majority were female (71.3%). In detail, 360 patients (61.9%) had a malignant thyroid diagnosis, 85 patients (14.6%) had a substernal goitre, and 137 (23.5%) underwent total thyroidectomy due to benign diagnoses, representing complicated surgical cases (comorbidity) (Table 1).
Table 1.
Demographic and clinical characteristics of patients undergoing total thyroidectomy between January 2010 and March 2015 at the Department of Otorhinolaryngology, Rigshospitalet, Copenhagen University Hospital, Denmark
| Patients (total) | 582 |
| Gender | |
| Male | 167 (28.7) |
| Female | 415 (71.3) |
| Age, years | 53.5 (11–95) |
| Diagnosis | |
| Benign | 222 (38.1) |
| Malignant | 360 (61.9) |
| Substernal goitre | 85 (14.6) |
| Autotransplantation | 125 (21.5) |
| Neck dissection | 310 (53.3) |
| Central | 214 (36.8) |
| Central + lateral | 96 (16.5) |
| Duration of surgery, min | 140.5 (35–478) |
| Hospitalization, days | 3 (2–34) |
Values are n (%) or median (range), as appropriate.
Surgery
A total of 437 total thyroidectomies (75.1%) were performed by consultants, and the remainder were performed by staff specialists (24.9%). The experience of the surgeons (defined as the number of total thyroidectomies performed by the individual surgeon in the 5-year study period) varied from 1 to 121 operations.
The median duration of surgery was 140.5 min, and autotransplantation of one or more of the parathyroid glands into the sternocleidomastoid muscle were performed in 125 patients (21.5%). Furthermore, 310 patients (53.2%) had a neck dissection done of which 214 (36.8%) involved the central lymph node compartment (level VI–VII), and the remaining 96 (16.5%) involved both the central and lateral compartments (level II–V).
Patient Outcomes
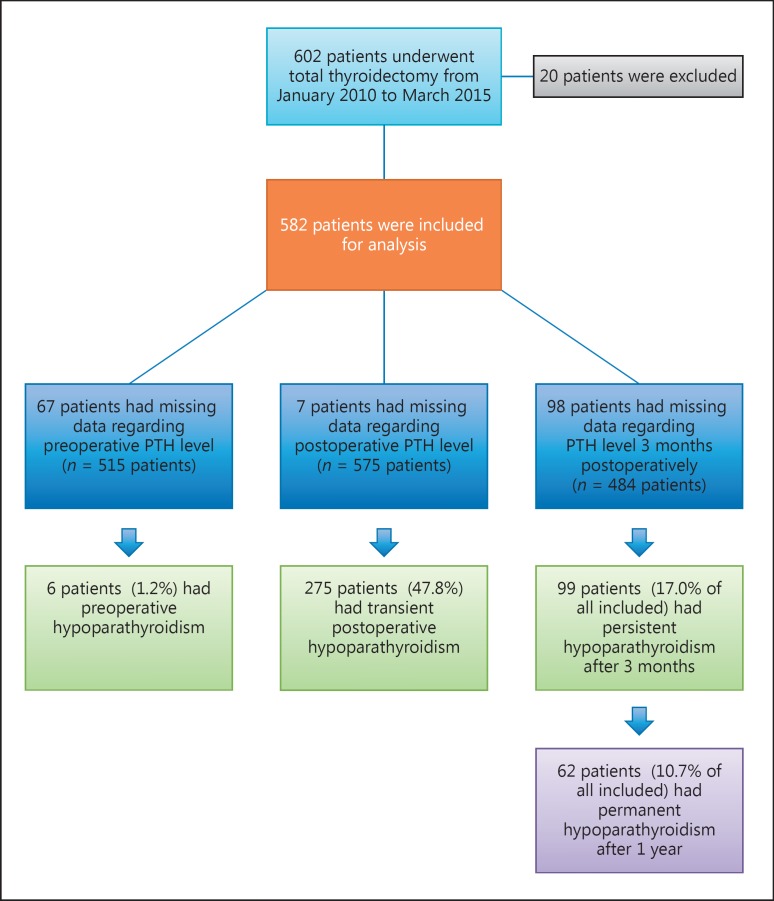
In 7 patients, information on postoperative level of PTH was missing. Of the remaining 575 patients, 275 (47.8%) developed transient biochemically defined hypoparathyroidism during the first 24 h after surgery.
Information on PTH level after 3 months was missing in 98 patients. Of the remaining patients, 99 (17%) still suffered from hypoparathyroidism at the 3-month evaluation. However, only 62 patients (10.7%) suffered from permanent hypoparathyroidism 1 year after surgery (Fig. 1).
Fig. 1.
Distribution of patients with hypoparathyroidism before and after total thyroidectomy. Patients with missing data were subtracted from the calculations except when evaluating the incidence of hypoparathyroidism after 3 and 12 months. Here, patients with missing PTH registration at an outpatient clinic were considered normoparathyroid.
Risk Factors
Incidence of acute hypoparathyroidism was significantly associated with a prolonged duration of surgery (p < 0.05). Approximately 30% of the hypoparathyroid patients had an autotransplantation of the parathyroid glands performed (p < 0.001), and furthermore, a combined central and lateral neck dissection was significantly associated with the development of hypoparathyroid ism (p < 0.05). Lastly, young patients had a higher risk of hypoparathyroidism during the first 24 h (p < 0.05) (Table 2).
Table 2.
Differences in demographic and clinical factors between postoperative hypoparathyroid (transient, persistent, and permanent) and normoparathyroid patients
| Variable | In the first 24 h |
After 3 months |
After 1 year |
||||||
|---|---|---|---|---|---|---|---|---|---|
| transient HPT |
NPT | p | persistent HPT |
NPT | p | permanent HPT |
NPT | p | |
| Patients | 275 (47.8) | 300 | 99 (17.0) | 483 | 62 (10.7) | 520 | |||
| Cancer | 183 (66.5) | 167 (55.6) | 0.057a | 82 (82.8) | 262 (68.1) | 0.004a | 50 (80.6) | 294 (69.7) | 0.098a |
| Substernal goitre | 38 (13.8) | 47 (15.6) | 0.246a | 7 (7.1) | 35 (8.2) | 0.689a | 6 (9.6) | 35 (8.2) | 0.808a |
| Duration of surgery, min | 152 | 131 | <0.001b | 163.0 | 137.0 | 0.001b | 151.0 | 138.0 | 0.035b |
| Autotransplantation of | <0.001a | ||||||||
| parathyroid glands | 86 (31.3) | 39 (13) | 33 (33.3) | 71 (18.4) | 0.002 | 18 (29.0) | 86 (20.4) | 0.136a | |
| Central neck dissection | 106 (38.5) | 108 (36.0) | 0.718a | 39 (39.4) | 158 (32.7) | 0.819a | 22 (35.5) | 175 (33.6) | 0.408a |
| Central + lateral neck dissection | 63 (22.9) | 33 (11.0) | 0.003a | 32 (32.3) | 61 (12.6) | 0.001a | 20 (32.3) | 73 (14.0) | 0.019a |
| Experience of surgeon | 57 | 57 | 0.111b | 62 | 57 | 0.188b | 62 | 57 | 0.116b |
| Female | 208 (75.6) | 197 (65.6) | 0.125a | 68 (68.7) | 272 (70.6) | 0.713a | 42 (67.7) | 298 (70.6) | 0.657a |
| Age, years | 51 | 56 | 0.048b | 49 | 52 | 0.171b | 50 | 52 | 0.371b |
Values are n (%) or medians, as appropriate. Experience of surgeon is the median total number of thyroidectomies/5 years. HPT, hypoparathyroidism; NPT, normoparathyroidism.
χ2 test.
Mann-Whitney test.
On multivariate analysis, only including the significant predictors on univariate analysis, age, autotransplantation of the parathyroid glands, and the duration of surgery were the only risk factors with an independent effect on acute hypoparathyroidism (Table 3).
Table 3.
Multivariate analysis examining the independent influence of different variables on the risk of transient, persistent, and permanent hypoparathyroidism
| Variable | Transient HPT | Persistent HPT | Permanent HPT |
|---|---|---|---|
| Age | p = 0.049 | p = 0.080 | p = 0.282 |
| Cancer | p = 0.543 | p = 0.021 | p = 0.159 |
| Autotransplantation of parathyroid glands | p = 0.000 | p = 0.015 | p = 0.313 |
| Central + lateral neck dissection | p = 0.093 | p = 0.516 | p = 0.554 |
| Duration of surgery | p = 0.033 | p = 0.019 | p = 0.085 |
HPT, hypoparathyroidism.
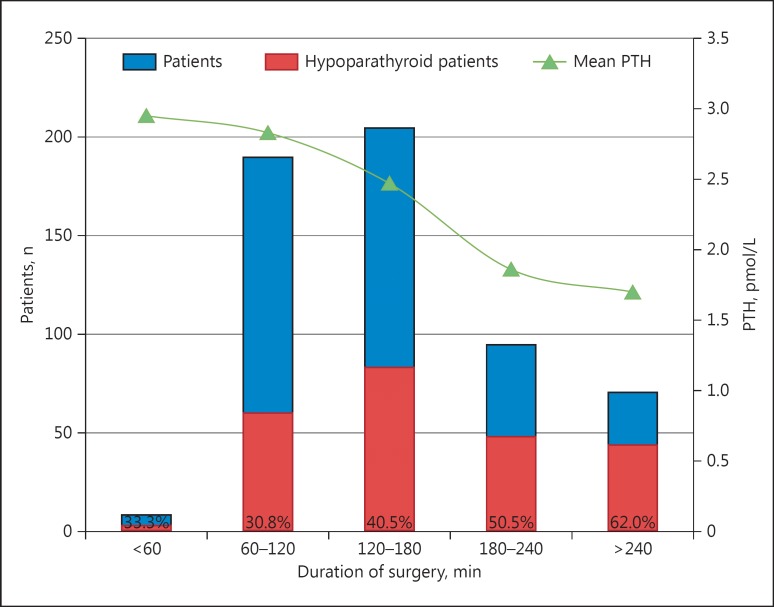
In order to visualize the relation between the duration of surgery and the risk of hypoparathyroidism, patients were divided into subgroups based upon the length of surgery lasting <60, 60–120, 120–180, 180–240, or >240 min. The incidences of hypoparathyroidism were 33, 31, 41, 51, and 62%, respectively. Furthermore, the mean level of postoperative PTH was calculated for each group of patients, and showed a steady decrease with increasing surgery duration (Fig. 2).
Fig. 2.
The figure shows how the proportion of acute hypoparathyroid patients increases and the mean level of PTH decreases with an extended duration of surgery. The percentages at the bottom of the columns represent the incidences of acute hypoparathyroidism in the different groups.
Examining the risk of persistent hypoparathyroidism after 3 months revealed almost the same results, showing cancer (p < 0.05), combined central and lateral neck dissection (p = 0.05), extended duration of surgery (p < 0.05), and autotransplantation of the parathyroid glands (p < 0.05) to be significantly associated with the complication (Table 2). On multivariate analysis only cancer, the reimplantation of parathyroid glands, and the duration of surgery had an independent significance (Table 3).
The risk of permanent hypoparathyroidism after 1 year was only significantly correlated with a prolonged duration of surgery (p < 0.05) and the performance of a combined central and lateral neck dissection (p < 0.05) (Table 2). Multivariate analysis, however, revealed that none of these variables had an independent effect (Table 3). No difference was observed for the experience of the surgeon between the patients with transient, persistent, or permanent hypoparathyroidism and those with normal gland function (p > 0.05).
Discussion
This study demonstrates a distribution of patients undergoing total thyroidectomy, similar to the examined literature with regard to age and gender, showing a clear predominance of middle-aged females. However, in our study a greater proportion of patients had a thyroid cancer diagnosis (62%), as the examined institution represents a tertiary referral centre. We found that 48% of the patients suffered from hypoparathyroidism during the first 24 h after surgery, which is in accordance with the literature, yet representing a high incidence. Our definition of hypoparathyroidism is in accordance with recent literature stating that not only the postoperative level of PTH but also a decline >50% predicts severe hypocalcaemia postoperatively [11, 12] and may in part explain our finding of a high incidence of hypoparathyroidism.
At the 3-month evaluation, 17% of the included patients in our study still suffered from hypoparathyroidism, and after 1 year this number decreased to 11%. These incidences constitute a minimum since the calculation is built on the assumption that the non-participants at the 3- and 12-month evaluation did not suffer from hypoparathyroidism. This seems like a reasonable hypothesis based upon the fact that patients' medical records are commonly shared in Denmark.
This study demonstrated that a long duration of surgery, autotransplantation of parathyroid glands, combined central and lateral neck dissection, and young age were all risk factors of acute postoperative hypoparathyroidism on univariate analysis. These relations have all been demonstrated before by several other studies [2, 4, 7, 8, 9, 10, 14, 15, 18, 19, 20]. Predictors of permanent hypoparathyroidism were prolonged duration of surgery and the performance of combined central and lateral neck dissection.
Multivariate analysis showed that age, parathyroid autotransplantation, and duration of surgery were all independent predictors of acute hypoparathyroidism, whereas no predictors could be independently related to permanent hypoparathyroidism.
According to the literature, most patients with parathyroid dysfunction following total thyroidectomy return to normal function within a few weeks to a month after surgery [13]. How and when to best define the recovery of parathyroid gland dysfunction remains uncertain, though most studies state that PTH measurements should be done 6 or 12 months after surgery [7, 10, 13, 15, 17]. Kim et al. [17] demonstrate that recovery from postoperative hypoparathyroidism may even occur as long as 2 years after surgery in patients not undergoing autotransplantation of the parathyroid glands. Our study supports the assumption that a continuous improvement of the parathyroid gland function exists during the first 12 months following surgery.
Our finding that autotransplantation of parathyroid tissue was significantly and independently associated with both transient and persistent hypoparathyroidism 3 months after surgery is partly conflicting with previous studies. Kim et al. [17] state that the return of parathyroid function is generally observed within a month in patients with an autotransplanted parathyroid gland compared to the much slower (up to 24 months) regain of function of preserved but devascularized parathyroid glands. The larger surface area for neovascularization in the sliced and reimplanted tissue explains the difference in recovery rate. However, the 1-month recovery rate is not present in our study, still causing a significant association between autotransplantation and persistent hypoparathyroidism after 3 months. At the 1-year post-surgery follow-up the association with permanent hypoparathyroidism was insignificant. Thus, our study does not question the benefit of the reimplantation procedure, but reinforces that a longer recovery phase must be expected.
Our study implies that the risk of hypoparathyroidism increases with extended duration of surgery. No specific cut-off values were calculated; however, our results show that surgery lasting longer than 120 min considerably increased the incidence of hypoparathyroidism and decreased the mean level of PTH (Fig. 2). Such long duration of surgery probably reflects surgical difficulties, as seen with invasive cancer and the extent of lymph node dissection, etc. However, as the multivariate analysis revealed (Table 3), the duration of surgery was an independent predictor of hypoparathyroidism during the first 24 h and after 3 months. After 1 year combined central and lateral neck dissection and long surgery duration are probably closely related, which explains why none of the variables have an independent significance. Most likely, a surgery lasting longer than 120 min causes ischaemic changes to the parathyroid glands due to a decrease in blood flow. The finding that long duration of surgery is a predictor of permanent hypoparathyroidism is therefore in accordance with the above-mentioned statement by Kim et al. [17] that regain of function of preserved but devascularized parathyroid glands can last up to 24 months.
Our finding that central neck dissection alone was not significantly related to hypoparathyroidism is probably explained by the fact that the procedure is carried out as a prophylactic intervention when thyroid cancer is diagnosed. In contrast, a combined central and lateral neck dissection is indicated when metastasis has already been identified, often involving the central lymph node compartment. Thus, a combined procedure causes greater damage to the parathyroid glands, making the association to hypoparathyroidism significant.
A study by Sosa et al. [19] found a significant association between increased surgeon experience and improved patient outcomes after surgical procedures for both benign and malignant thyroid disease. Our results showed no significant correlation between surgeon experience and the risk of transient, persistent, or permanent hypoparathyroidism. This may reflect a selection bias so that the most experienced surgeons perform the most complex and extensive surgeries and the less experienced surgeons receive thorough supervision.
This study confirms what has previous been stated by other studies: that the influence of specific variables differs and that the risk profile of postoperative hypoparathyroidism is complex. However, according to our data, the duration of surgery seems to be a consistent and important risk factor that can be used practically in the postoperative management of patients.
In conclusion, the risk of transient and permanent hypoparathyroidism after total thyroidectomy is high within the expected range among patients undergoing surgery in a tertiary referral centre. The only independent predictors of the acute complication are young age, reimplantation of parathyroid glands, and a duration of surgery extending >120 min. The regain of function of the parathyroid glands must be expected to last at least 1 year following surgery, and furthermore, the recovery potential of autotransplanted parathyroid glands should not be evaluated within 1–3 months after surgery.
A total thyroidectomy lasting longer than 120 min is common in a tertiary referral centre and probably reflects surgical difficulties, which are challenging to influence. Special attention should be given to these patients in the postoperative recovery phase in order to prevent and mitigate potential hypocalcaemic symptoms and thereby improve the patients' quality of life and decrease the duration of hospitalization.
Statement of Ethics
This retrospective study was part of the THYKIR Database, approved by the Danish Data Protection Agency (journal No. 2000-41-0010).
Disclosure Statement
The authors have no conflicts of interest to declare.
References
- 1.Koeppen BM, Stanton BS. Berne & Levy Physiology. ed 6. Philadelphia: Mosby/Elsevier; 2010. pp. 696–705. [Google Scholar]
- 2.Abdel-Halim CN, Rejnmark L, Egsgaard Nielsen V. Post-operative parathyroid hormone can be used as a predictor of normocalcaemia after total thyroidectomy. Danish Medical Journal. 2015;62:A5157. [PubMed] [Google Scholar]
- 3.Alhefdhi A, Mazeh H, Chen H. Role of postoperative vitamin D and/or calcium routine supplementation in preventing hypocalcemia after thyroidectomy: a systematic review and meta-analysis. Oncologist. 2013;18:533–542. doi: 10.1634/theoncologist.2012-0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ambe PC, Brömling S, Knoefel WT, Rehders A. Prolonged duration of surgery is not a risk factor for postoperative complications in patients undergoing total thyroidectomy: a single center experience in 305 patients. Patient Saf Surg. 2014;8:45. doi: 10.1186/s13037-014-0045-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carr AA, Yen TW, Fareau GG, Cayo AK, Misustin SM, Evans DB, Wang TS. A single parathyroid hormone level obtained 4 hours after total thyroidectomy predicts the need for postoperative calcium supplementation. J Am Coll Surg. 2014;219:757–764. doi: 10.1016/j.jamcollsurg.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 6.Carter Y, Chen H, Sippel RH. An intact parathyroid hormone–based protocol for the prevention and treatment of symptomatic hypocalcemia after thyroidectomy. J Surg Res. 2014;186:23–28. doi: 10.1016/j.jss.2013.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Pasquale L, Sartori PV, Vicentini L, Beretta E, Boniardi M, Leopaldi E, Gini P, La Manna L, Cozzaglio L, Steffano GB, Andreani S, Badiali S, Cantoni GM, Galimberti A, Ghilardi G, Gusmeroli M, Maggiore R, Morenghi E, Pauna J, Poggi L, Testa V. Necessity of therapy for post-thyroidectomy hypocalcaemia: a multi-centre experience. Langenbecks Arch Surg. 2015;400:319–324. doi: 10.1007/s00423-015-1292-0. [DOI] [PubMed] [Google Scholar]
- 8.Lee DR, Hinson AM, Siegel ER, Steelman SC, Bodenner DL, Stack BC. Comparison of intraoperative versus postoperative parathyroid hormone levels to predict hypocalcemia earlier after total thyroidectomy. Otolaryngol Head Neck Surg. 2015;153:343–349. doi: 10.1177/0194599815596341. [DOI] [PubMed] [Google Scholar]
- 9.Noureldine SI, Genther DJ, Lopez M, Agrawal N, Tufano RP. Early predictors of hypocalcemia after total thyroidectomy. JAMA Otolaryngol Head Neck Surg. 2014;140:1006. doi: 10.1001/jamaoto.2014.2435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Puzziello A, Rosato L, Innaro N, Orlando G, Avenia N, Perigli G, Caló PG, De Palma M. Hypocalcemia following thyroid surgery: incidence and risk factors. A longitudinal multicenter study comprising 2,631 patients. Endocrine. 2014;47:537–542. doi: 10.1007/s12020-014-0209-y. [DOI] [PubMed] [Google Scholar]
- 11.Rafaelli M, De Crea C, D'Amato G, Moscato U, Bellantone C, Carrozza C, Lombardi CP. Post-thyroidectomy hypocalcemia is related to parathyroid dysfunction even in patients with normal parathyroid hormone concentrations early after surgery. Surgery. 2016;159:78–85. doi: 10.1016/j.surg.2015.07.038. [DOI] [PubMed] [Google Scholar]
- 12.Noordzij JP, Lee SL, Bernet VJ, Payne RJ, Cohen SM, McLeod IK, Hier MP, Black MJ, Kerr PD, Richards ML, Lo CY, Rafaelli M, Bellantone R, Lombardi CP, Cohen JI, Dietrich MS. Early prediction of hypocalcemia after thyroidectomy using parathyroid hormone: an analysis of pooled individual patient data from nine observational studies. J Am Coll Surg. 2007;205:748–754. doi: 10.1016/j.jamcollsurg.2007.06.298. [DOI] [PubMed] [Google Scholar]
- 13.Ritter K, Elfenbein D, Schneider DF, Chen H, Sippel RS. Hypoparathyroidism after total thyroidectomy: incidence and resolution. J Surg Res. 2015;197:348–353. doi: 10.1016/j.jss.2015.04.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schlottmann F, Campos Arbulú AL, Sadava EE, Mendez P, Pereyra L, Fernandez Vila JM, Mezzadri NA. Algorithm for early discharge after total thyroidectomy using PTH to predict hypocalcemia: prospective study. Langenbecks Arch Surg. 2015;400:831–836. doi: 10.1007/s00423-015-1341-8. [DOI] [PubMed] [Google Scholar]
- 15.Seo ST, Chang JW, Jin J, Lim YC, Rha KS, Koo BS. Transient and permanent hypocalcemia after total thyroidectomy: early predictive factors and long-term follow-up results. Surgery. 2015;158:1492–1499. doi: 10.1016/j.surg.2015.04.041. [DOI] [PubMed] [Google Scholar]
- 16.Selberherr A, Scheuba C, Riss P, Niederle B. Postoperative hypoparathyroidism after thyroidectomy: efficient and cost-effective diagnosis and treatment. Surgery. 2015;157:349–353. doi: 10.1016/j.surg.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 17.Kim SM, Kim HK, Kim KJ, Chang HJ, Kim BW, Lee YS, Chang HS, Park CS. Recovery from permanent hypoparathyroidism after total thyroidectomy. Thyroid. 2015;25:830–833. doi: 10.1089/thy.2014.0500. [DOI] [PubMed] [Google Scholar]
- 18.Jensen PVF, Jelstrup SM, Homøe P. Long-term outcomes after total thyroidectomy. Dan Med J. 2015;62:A5156. [PubMed] [Google Scholar]
- 19.Sosa JA, Bowman HM, Tielsch JM, Powe NR, Gordon TA, Udelsman R. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg. 1998;228:320–330. doi: 10.1097/00000658-199809000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tartaglia F, Blasi S, Giuliani A, Merola R, Livadoti G, Krizzuk D, Tortorelli G, Tromba L. Parathyroid autotransplantation during total thyroidectomy: results of a retrospective study. Int J Surg. 2015;28((suppl 1)):S79–S83. doi: 10.1016/j.ijsu.2015.05.059. [DOI] [PubMed] [Google Scholar]
- 21.Edafe O, Antakia R, Laskar N, Uttley L, Balasubramanian SP. Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcemia. Br J Surg. 2014;101:307–320. doi: 10.1002/bjs.9384. [DOI] [PubMed] [Google Scholar]
- 22.Paek SH, Lee YM, Min SY, Kim SW, Chung KW, Youn YK. Risk factors of hypoparathyroidism following total thyroidectomy for thyroid cancer. World J Surg. 2013;37:94–101. doi: 10.1007/s00268-012-1809-4. [DOI] [PubMed] [Google Scholar]
- 23.Toniato A, Boschin IM, Piotto A, Pelizzo MR, Guolo A, Foletto M, Casalide E. Complications in thyroid surgery for carcinoma: one institution's surgical experience. World Journal of Surgery. 2008;32:572–575. doi: 10.1007/s00268-007-9362-2. [DOI] [PubMed] [Google Scholar]
- 24.Wang X, Xing T, Wei T, Zhu J. Completion thyroidectomy and total thyroidectomy for differentiated thyroid cancer: comparison and prediction of postoperative hypoparathyroidism. J Surg Oncol. 2016;113:522–525. doi: 10.1002/jso.24159. [DOI] [PubMed] [Google Scholar]