Abstract
Aim
Ileosigmoidal knotting is an unusual form of acute intestinal obstruction characterized by closed‐loop obstruction of both ileum and sigmoid colon. We present 36 cases of ileosigmoidal knotting.
Methods
A retrospective analysis was designed to examine preoperative, operative, and postoperative findings of the 36 patients with ileosigmoidal knotting who were surgically treated in Necmettin Erbakan University's Meram Medical Faculty (Konya, Turkey) throughout a 26‐year period.
Results
The mean age was 55 (range, 47–61) years. The most common symptoms were abdominal pain, distention, obstipation, and vomiting, and the most common signs were abdominal tenderness and distention. The preoperative diagnosis was acute obstructed bowel in all patients. After resuscitation, all patients underwent emergency laparotomy. The most common type of ileosigmoidal knotting was type IA, in which the active ileum encircled the passive sigmoid in a clockwise manner. There was gangrene in both ileum and sigmoid colon in all patients. All ischemic bowels including ileum and sigmoid colon were resected and the continuity was carried out using primary anastomosis or Hartmann's procedure.
Conclusions
Ileosigmoidal knotting is a rare disease but its preoperative diagnosis is difficult. In cases of knotting there is no form of conservative treatment. Resective surgery is absolutely necessary.
Keywords: Ileosigmoidal knotting, intestine, obstruction, surgery
Introduction
Ileosigmoidal knotting (ISK) is a rare cause of acute intestinal obstruction characterized by closed‐loop obstruction of both ileum and sigmoid colon.1 It may lead to gangrene of the involved loops, hypovolemic shock, peritonitis, and endotoxemia. Clinical features of ISK are symptoms and signs of small and large bowel obstruction. There are usually no features specific for these conditions, and the diagnosis is established at laparotomy.2 Early preoperative resuscitation, prompt surgical intervention, and effective postoperative care are life‐saving in ISK. Aggressive preoperative resuscitation, appropriate antibiotic therapy, effective surgery, and postoperative metabolic support help minimize the morbidity and mortality. Here we present 36 cases of ileosigmoidal knotting.
Methods
A retrospective analysis was designed to examine preoperative, operative, and postoperative findings of the 36 patients with ISK who were surgically treated in the Department of General Surgery at Necmettin Erbakan University's Meram Medical Faculty (Konya, Turkey) throughout a 26‐year period. The features of patients and preoperative findings (age, gender, living area, previous or associated medical and surgical problems, symptoms, signs, radiological examinations, and diagnosis), intraoperative observations (type, rotation degree, anatomic variations, gangrene, and surgical procedures), and postoperative findings (mortality, morbidity, hospitalization period, and recurrence) were evaluated.
We classified ISK into four types based on the mechanism of formation of the knot.3 In type I (the commonest), the ileum is the active component, wrapping itself around the sigmoid colon (passive component) to form the knot, whereas in type II, it is the other way round. In type III, the ileocecal segment acts as the active component, whereas in type IV (undetermined type) it is not possible to differentiate the two components from each other. Types I and II can be classified into subtypes A and B depending on whether the torsion is clockwise or counterclockwise, respectively.
Results
The mean age was 55 (range, 47–61) years. Sixteen (44.4%) of patients were female and 20 (55.6%) were male. The most common symptoms were abdominal pain and obstipation, and the most common signs were abdominal tenderness and distention. The symptom duration was between 36 and 84 h (mean, 55.4 h). The preoperative diagnosis was acute obstructed bowel in all patients. Plain abdominal X‐ray films revealed dilation of the sigmoid colon and multiple air‐fluid levels in the small intestine. After resuscitation, all patients underwent emergency laparotomy. The most common type of ISK was type IA (30/83.3%) and the other patients were type IIA (16/16.7%). The most common torsion degree was 360°. In 30 patients (83.3%), anatomic predisposing factors (hypermobile small intestine and redundant sigmoid colon with elongated mesentery having narrow base) were found as causative factors, whereas in four patients (11.1%) late pregnancy and in two (5.6%) mobile cecum were determined as secondary associated factors (Table 1).
Table 1.
Predisposing factors in patients with ileosigmoidal knotting (n = 36)
| Predisposing factors | n/% |
|---|---|
| Anatomic predisposing factors | 30/83.3 |
| Late pregnancy | 4/11.1 |
| Mobile cecum | 2/5.6 |
There was gangrene in both ileum and sigmoid colon in all patients (Fig. 1). All ischemic bowels including ileum and sigmoid colon were resected and continuity was achieved by primary anastomosis (10 patients) and Hartmann's procedure (26 patients). The decision to carry out primary anastomosis or ostomy was based on the following patient data: age, general condition, and laboratory values.
Figure 1.
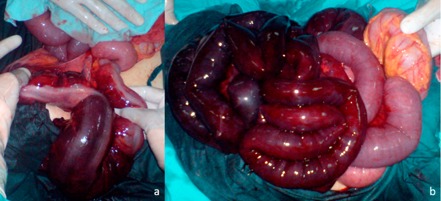
Representative photograph of gangrene evident in the ileum (A) and sigmoid colon (B) in all patients with ileosigmoidal knotting (n = 36).
There was no mortality. Total parenteral nutrition was used in all patients. In 12 patients (33.3%), incisional infection developed. The mean hospital stay was 7 days (range, 5–11 days).
Discussion
Ileosigmoidal knotting is an unusual form of intestinal obstruction, which is more common in African, Asian, and Middle Eastern countries.3 Ileosigmoidal knotting is likely to occur in developing or underdeveloped countries.
Its incidence in the general population is not known, but it is high in Turkey, especially in eastern Anatolia. ISK is common in adult males, and the peak incidence, as in our experience, is in the fourth decade. To explain the development of ISK, some anatomic predisposing factors are considered. These include a hypermobile small intestine and cecum with an elongated mesentery having a narrow base and a redundant sigmoid colon with a long mesocolon having a narrow base.4 Other factors include postoperative adhesions, internal herniation, intestinal malrotation, and omphalomesenteric abnormalities. Depending on the clinical features, the preoperative accurate diagnosis of ISK is very difficult. It is generally seen as an obstructive or non‐obstructive emergency; thus, the diagnosis is ultimately established during laparotomy, as was the case in our series. The main symptoms are vomiting, abdominal pain, obstipation and abdominal distention. Plain abdominal radiographs will usually show marked bowel dilatation and fluid levels.5 Although computed tomography and magnetic resonance imaging studies can demonstrate the dilatation of the bowels and the rotation of the mesenteries, the general condition of patients sometimes does not allow application of these diagnostic tools. Our series symptoms are abdominal pain, obstipation, abdominal distention, and vomiting. Our series signs are abdominal tenderness and distention, the others are hypokinetic–akinetic or hyperkinetic bowel sounds, muscular defense, and the presence of melanotic stool or sloughing of the colonic mucosa in proctoscopy.
Ileosigmoidal knotting was classified into three types by Alver et al.3 according to the active segment of the knot. In the present series, the rate of type I ISK was higher than that of other published series. In ISK, the presence of a double‐loop obstruction leads to rapid progression of gangrene in one or both loops. Shock, peritonitis, and endotoxemia occur because of volume loss into the involved loops, bacterial translocation from the lumen to the peritoneal cavity, and absorption of toxic products. Early and effective resuscitation is essential. In the presence of gangrene, resection is necessary. Gangrenous intestine should be resected and intestinal continuity restored by enteroenterostomy. If ascending colon and/or cecum gangrene is present, restoration may be carried out by enterocolostomy. Despite high morbidity, especially in borderline ischemic cases, ileostomy may be a lifesaving procedure. In cases with gangrenous sigmoid colon, there are different methods of surgical treatment. Resection and primary anastomosis with or without intraoperative colonic cleansing are carried out if the patient is stable and if anatomic conditions are appropriate for a tension‐free anastomosis. Otherwise, Hartmann's procedure or other stomas may be lifesaving procedures. Resection and Hartmann's procedure are preferred, especially when the distal segment is short.1 In the present series, primary anastomosis for ISK was carried out in 10 cases. Resection and Hartmann procedure's was carried out in four cases. Ileosigmoidal knotting has a grave prognosis, with a mean 40% (0%–100%) mortality and high morbidity rates. The most common cause of death is toxic shock. However, recent studies have reported decreased mortality. In the present series was no mortality.
In conclusion, ISK is an extremely rare cause of bowel obstruction and ischemic necrosis of the intestine. Its clinical features are a combination of small and large bowel obstruction findings. Its clinical presentation is not specific, and its preoperative diagnosis is very difficult, but preoperative diagnosis is possible when clinical and radiologic features are considered together. Resective surgery is absolutely necessary. Preoperative resuscitation, early surgery, and efficient postoperative intensive care are necessary. Principles of management for obstruction and ischemia are well established. In surgical treatment, primary anastomoses after resection of gangrenous bowel is a safe surgical treatment option in ileosigmoidal knotting and represents the most commonly recommended technique in suitable patients. The prognosis is good when there is aggressive resuscitation and prompt surgery.
Conflict of Interest
None.
Acknowledgment
We acknowledge the contribution of Dr. Adnan Kaynak.
References
- 1. Akgun Y. Management of ileosigmoidal knotting. Br. J. Surg. 1977; 84: 672–673. [PubMed] [Google Scholar]
- 2. Atamanalp SS, Oren D, Başoğlu M et al Ileosigmoidal knotting: Outcome in 63 patients. Dis. Colon Rectum 2004; 47: 906–910. [DOI] [PubMed] [Google Scholar]
- 3. Alver O, Oren D, Tireli M, Kayabası B, Akdemir D. Ileosigmoid knotting in Turkey: Review of 68 cases. Dis. Colon Rectum 1993; 36: 1139–1147. [DOI] [PubMed] [Google Scholar]
- 4. Atamanalp SS, Oren D, Yildirgan MI. Ileosigmoidal knotting in children: A review of 9 cases. World J. Surg. 2007; 31: 31–35. [DOI] [PubMed] [Google Scholar]
- 5. Baheti AD, Patel D, Hira P, Babu D. Ileosigmoid knot: A case report. Indian J. Radiol. Imaging 2011; 21: 147–149. [DOI] [PMC free article] [PubMed] [Google Scholar]


