Abstract
Aim
Drug overdose is an important issue in emergency medicine. However, studies covering overdose patients transported by ambulance have not been sufficiently carried out. We attempted to clarify problems of suspected drug overdose patients transported by ambulance.
Methods
This is a prospective population‐based cohort study. Data were collected by emergency medical service crews in Osaka City, Japan, between January 1998 and December 2010.
Results
Drug overdose cases increased annually from 1,136 in 1998 to 1,822 in 2010 (P < 0.0001 for trend). In these cases, the dominant age range was between 16 and 40 years and the age distribution did not change over time. The age of non‐overdose cases increased (P < 0.0001 for trend), with patients aged ≥66 years becoming most common in recent years, reflecting the aging of society. Males comprised most non‐overdose patients, but the percentage of females increased annually (P < 0.0001 in trend). Females comprised approximately 70% in overdose cases annually throughout the study period. The duration from the emergency call to the arrival at the hospital for overdose patients has increased markedly in recent years. It also takes more time to obtain acceptance from hospitals to care for patients of suspected overdose.
Conclusion
The characteristics of drug overdose patients are clearly different from those of non‐overdose patients. Recent trends of drug overdose patients indicate the accelerated burden on emergency medical services system.
Keywords: Ambulance diversion, drug overdose, emergency medical services, hospital arrival time, transportation of patients
Introduction
Background
Drug overdoses are among the most important issues in emergency medicine and comprise a diversity of problems, including epidemiological poisoning deaths,1, 2 poisoning by a specific drug,3, 4, 5, 6 issues concerning suicide,7 and preventive strategies for drug overdoses.8, 9, 10 However, the effect of drug overdoses on emergency medical services (EMS) system has not been examined in detail. Studies have been carried out for all cases treated in emergency departments or hospitals.11, 12 However, to our knowledge, a study of emergency cases focusing on drug overdose patients transported by ambulance has not been carried out sufficiently. This background led us to analyze emergency patients transported by ambulance in order to describe comprehensive information by covering all emergency patients in a certain area.
Recent studies based on EMS records have delivered considerable outcomes for resuscitation care of out‐of‐hospital arrest patients and traumatized patients.13, 14 These outcomes make our investigation consequential as the first step of analyzing overdose patients in EMS system as a population‐based study.
The aim of this study was to determine the characteristic features of overdose patients compared to non‐overdose patients based on the descriptive epidemiological data such as age and sex. Based on these data, we also carried out a longitudinal analysis of the increased burden on the emergency system due to overdose patients.
Methods
Setting
This is a population‐based observational study in Osaka City, which is a metropolis in the western part of Japan. The population of Osaka City was 2,665,314 as of October 1, 2010. The male and female populations were 1,293,798 and 1,371,516 (51.5%), respectively. The age distribution of this city's inhabitants was 12.7%, 34.1%, 32.2%, 20.9% for those aged 0–15 years, 16–40 years, 41–65 years, and ≥66 years, respectively.
Participants
Participants of our study were all emergency patients who called the ambulance in Osaka City from January 1, 1998 to December 31, 2010. The EMS system in Osaka City is operated by the Municipal Fire Department and is activated by dialing 119. All calls were received and recorded by a single dispatch center and ambulance were transferred from 25 fire stations distributed throughout the city. The EMS system is operated by a single‐tiered system. When the ambulance reaches the patients, the crew evaluates the patient's condition and determines the most suitable hospital for the patient. The crew then makes contact with a hospital by telephone to confirm availability for receiving the patient.
Outcome measures
Annual trends in demographic data such as age and sex were evaluated for emergency patients with a focus on drug overdose cases. The time for transportation was measured as the time from the emergency call to arrival at the hospital. Consciousness level was used as an indicator of the patient's condition, as this could influence the time factor. The number of hospitals telephoned by EMS personnel to confirm their availability to receive each patient was also evaluated.
We found in 1312 cases age or sex information were missing in 13 years of study period. We treated them as missing data.
Data collection and processing
Data from all emergency patients transported by ambulance were collected prospectively by EMS crews in Osaka City. These were typed and made electronically available by the EMS crews themselves. The research protocol was approved by the institutional review board of Kinki University, with the assent of the EMS Osaka.
Cases of drug overdose are usually termed “suspected” overdoses and most were caused by miscellaneous drugs. In the International Classification of Diseases, 10th Revision, the codes from T36 to T50 are used to categorize drug overdose cases based on the complexity of drug poisoning. We classified the drug types according to these codes based on information from ambulance crews collected in interviews with bystanders or objective evidence such as the label on a drug container. Data collected between January 1, 2010 and December 31, 2010 were used in this analysis.
Analysis
Temporal trends were tested using Cochrane–Armitage and Jonckheere–Terpstra tests based on the data distribution, after dividing the patients into overdose and non‐overdose cases. The independent association between calendar year and proportion of overdose patients compared to non‐overdose patients was evaluated, with adjustment for age and sex. All statistical analyses were carried out using SAS statistical software (version 9.3; SAS Institute, Cary, NC, USA). All tests were two‐tailed, and P‐values less than 0.05 were regarded as statistically significant.
Results
Increase in drug overdose patients
In 1998, 1,136 overdose and 134,098 non‐overdose patients were transported to hospitals by ambulance in Osaka City. The respective numbers increased to 1,822 and 163,367 (P < 0.0001 for trend) in 2010. The age‐ and sex‐adjusted odds ratio for the incidence of drug overdose compared to non‐overdose cases was 1.39 (95% confidence interval, 1.29–1.50) in 2010 as compared with 1998 (Fig. 1).
Figure 1.
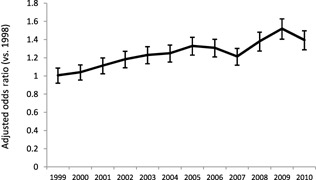
Adjusted odds ratio of number of overdose patients transported by ambulance by year in Osaka City, Japan, 1998–2010. The model was adjusted for patients' age and sex. The reference year was 1998. I bars represent 95% confidence intervals.
Characteristics of drug overdose patients
The age distribution of the drug overdose cases differed from those of non‐overdose patients. Patients aged 41–65 years accounted for the highest number of non‐overdose cases (37%) in 1998. In 2010, patients aged ≥66 years comprised 43% of these cases (P < 0.0001 for trend). This result reflects the general aging in society. Most overdose cases involved patients aged 16–40 years in each year (Table 1).
Table 1.
Annual trends in age and sex for emergency patients transported to hospital by ambulance in Osaka City, Japan, 1998–2010
| 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | Significant for trend | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non‐overdose cases | n | 134,098 | 136,807 | 146,778 | 154,100 | 156,476 | 164,046 | 170,767 | 176,669 | 177,707 | 172,177 | 159,440 | 159,266 | 163,367 | P < 0.0001 for number |
| Age, years, mean (SD) | 48.3 ± 23.6 | 48.9 ± 24.1 | 49.1 ± 24.0 | 49.5 ± 24.2 | 50.1 ± 24.4 | 50.4 ± 24.7 | 51.2 ± 24.8 | 51.9 ± 24.9 | 52.1 ± 25.0 | 52.8 ± 25.1 | 53.7 ± 25.0 | 53.9 ± 25.4 | 55.3 ± 25.2 | P < 0.0001 for age | |
| Median (IQR) | 51 (28–66) | 52 (29–68) | 52 (29–68) | 53 (29–69) | 54 (30–70) | 54 (30–70) | 55 (31–71) | 56 (31–72) | 57 (32–73) | 58 (32–74) | 59 (34–74) | 59 (34–75) | 61 (36–76) | ||
| Age distribution, years | |||||||||||||||
| 0–15 | 12,132 | 12,574 | 12,973 | 13,600 | 14,098 | 14,943 | 15,049 | 15,319 | 15,105 | 14,577 | 12,944 | 13,997 | 12,918 | ||
| (%) | (9.0) | (9.2) | (8.8) | (8.8) | (9.0) | (9.1) | (8.8) | (8.7) | (8.5) | (8.5) | (8.1) | (8.8) | (7.9) | ||
| 16–40 | 36,264 | 36,711 | 40,247 | 41,680 | 41,388 | 43,456 | 44,136 | 44,882 | 45,501 | 42,690 | 37,953 | 36,461 | 35,565 | ||
| (%) | (27.0) | (26.8) | (27.4) | (27.0) | (26.5) | (26.5) | (25.8) | (25.4) | (25.6) | (24.8) | (23.8) | (22.9) | (21.8) | ||
| 41–65 | 50,523 | 48,856 | 51,444 | 52,643 | 51,671 | 51,695 | 52,574 | 52,700 | 52,229 | 48,955 | 44,579 | 43,317 | 43,741 | ||
| (%) | (37.7) | (35.7) | (35.0) | (34.2) | (33.0) | (31.5) | (30.8) | (29.8) | (29.4) | (28.4) | (28.0) | (27.2) | (26.8) | ||
| ≥66 | 35,173 | 38,666 | 42,114 | 46,177 | 49,318 | 53,952 | 59,007 | 63,768 | 64,872 | 65,955 | 63,964 | 65,491 | 71,143 | ||
| (%) | (26.2) | (28.3) | (28.7) | (30.0) | (31.5) | (32.9) | (34.6) | (36.1) | (36.5) | (38.3) | (40.1) | (41.1) | (43.5) | ||
| Male, n | 82,664 | 83,150 | 88,522 | 92,153 | 92,380 | 95,774 | 97,940 | 100,006 | 99,167 | 95,723 | 88,174 | 88,111 | 89,110 | P < 0.0001 for sex | |
| (%) | (61.7) | (60.8) | (60.4) | (59.9) | (59.1) | (58.4) | (57.4) | (56.7) | (55.8) | (55.6) | (55.3) | (55.3) | (54.6) | ||
| Female, n | 51,264 | 53,522 | 58,134 | 61,805 | 63,949 | 68,162 | 72,701 | 76,559 | 78,409 | 76,337 | 71,266 | 71,155 | 74,257 | ||
| (%) | (38.3) | (39.2) | (39.6) | (40.1) | (40.9) | (41.6) | (42.6) | (43.4) | (44.2) | (44.4) | (44.7) | (44.7) | (45.6) | ||
| Overdose cases | n | 1,136 | 1,168 | 1,297 | 1,454 | 1,568 | 1,714 | 1,804 | 1,978 | 1,968 | 1,746 | 1,811 | 1,985 | 1,822 | P < 0.0001 for number |
| Age, years, mean (SD) | 37.9 ± 16.5 | 38.5 ± 17.1 | 37.4 ± 16.4 | 37.0 ± 15.9 | 36.6 ± 16.0 | 36.1 ± 16.0 | 36.4 ± 15.8 | 35.5 ± 15.4 | 35.4 ± 15.6 | 36.1 ± 16.0 | 36.8 ± 16.4 | 37.5 ± 16.4 | 38.6 ± 17.1 | P = 0.52 for age | |
| Median (IQR) | 34 (26–49) | 34 (26–50) | 33 (26–48) | 34 (26–47) | 33 (25–45) | 33 (25–45) | 34 (25–45) | 32 (25–43) | 33 (24–42) | 33 (24–43) | 34 (24–45) | 34 (25–46) | 35 (26–47) | ||
| Age distribution, years | |||||||||||||||
| 0–15 | 40 | 29 | 35 | 35 | 40 | 52 | 53 | 57 | 55 | 44 | 41 | 44 | 47 | ||
| (%) | (3.5) | (2.5) | (2.7) | (2.4) | (2.6) | (3.0) | (2.9) | (2.9) | (2.8) | (2.5) | (2.3) | (2.2) | (2.6) | ||
| 16–40 | 667 | 709 | 814 | 939 | 1,012 | 1,119 | 1,187 | 1,345 | 1,345 | 1,165 | 1,170 | 1,255 | 1,084 | ||
| (%) | (58.7) | (60.7) | (62.8) | (64.6) | (64.5) | (65.3) | (65.8) | (68.0) | (68.3) | (66.7) | (64.6) | (63.2) | (59.5) | ||
| 41–65 | 340 | 326 | 356 | 384 | 405 | 437 | 456 | 475 | 446 | 421 | 466 | 536 | 514 | ||
| (%) | (29.9) | (27.9) | (27.4) | (26.4) | (25.8) | (25.5) | (25.3) | (24.0) | (22.7) | (24.1) | (25.7) | (27.0) | (28.2) | ||
| ≥66 | 89 | 104 | 92 | 96 | 111 | 106 | 108 | 101 | 122 | 116 | 134 | 150 | 177 | ||
| (%) | (7.8) | (8.9) | (7.1) | (6.6) | (7.1) | (6.2) | (6.0) | (5.1) | (6.2) | (6.6) | (7.4) | (7.6) | (9.7) | ||
| Male, n | 369 | 392 | 448 | 479 | 487 | 541 | 516 | 557 | 501 | 465 | 489 | 611 | 541 | P < 0.0001 for sex | |
| (%) | (32.5) | (33.6) | (34.5) | (32.9) | (31.1) | (31.6) | (28.6) | (28.2) | (25.5) | (26.6) | (27.0) | (30.8) | (29.7) | ||
| Female, n | 767 | 776 | 849 | 975 | 1,081 | 1,173 | 1,288 | 1,421 | 1,467 | 1,281 | 1,322 | 1,374 | 1,281 | ||
| (%) | (67.5) | (66.4) | (65.5) | (67.1) | (68.9) | (68.4) | (71.4) | (71.8) | (74.5) | (73.4) | (73.0) | (69.2) | (70.3) |
IQR, interquartile range.
Females accounted for approximately 70% of overdose cases with no annual change in this value. In contrast, most non‐overdose patients were males throughout the study period, although the percentage of females increased annually (P < 0.0001 for trend) (Table 1).
Time factors
For drug overdose patients, the time from the emergency call to arrival at hospital has increased markedly in recent years (Fig. 2A). The percentage of these patients with impaired consciousness did not change during study period, suggesting this increased time period would not be attributable to increases in the number of critically ill patients (Fig. 2B). The number of contact calls for each overdose patient has increased in recent years (Fig. 2A).
Figure 2.
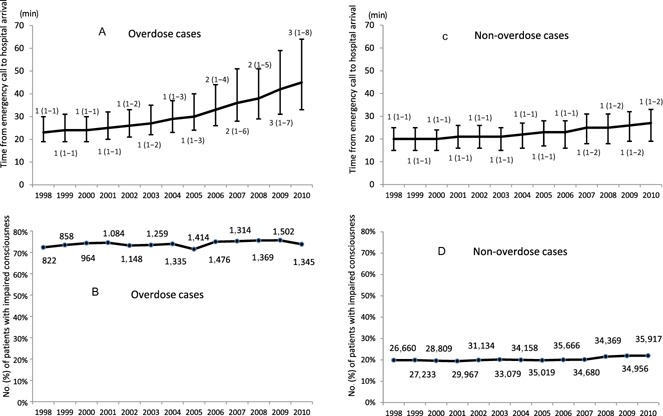
Annual trend for time factors concerning emergency patients transported to hospital by ambulance in Osaka City, Japan, 1998–2010. In overdose cases, time periods from emergency call to hospital arrival were markedly increased (P < 0.0001 for trend). The number of hospitals to which the emergency medical service crew made contact for each patient is labeled as the median (quartiles) (A). Although in non‐overdose cases time periods from emergency call to hospital arrival were increased (P < 0.0001), the increase was not accelerated compared to overdose cases. The number of hospitals to which the emergency medical service crew made contact is labeled as the median (quartiles) (C). Numbers and percentages of patients whose consciousness was impaired are shown in overdose cases (B) and non‐overdose cases (D).
For non‐overdose patients, the time from the emergency call to arrival at hospital has increased consistently from 20 min in 1998 to 27 min in 2010 (Fig. 2C). The median number of contact calls for each emergency non‐overdose patient remained at one during the study period. However, it has recently become common for EMS crews to contact two or three hospitals by telephone before transporting a patient.
Categories of causative drugs
Of the 1822 overdose cases in 2010, over half were coded in the T42 group of sedative, hypnotic, antiepileptic, and antiparkinsonism drugs as causative agents (Table 2). Cases classified to the T43 group of psychotropic drugs and the T42 group made up approximately two‐thirds of all cases. Only eight cases involved narcotics and psychodysleptics. The numbers of other cases were limited and EMS crews paid particular attention to cases in which somatic function might have been affected. In 30 such cases, we could not exclude the possibility that the dosage was in normal range. It is possible that the event was caused by an allergic reaction or adverse event to drugs, rather than an overdose. The number of multiple code cases, in which the patients took a variety of drugs, was 101. The EMS crews did not record the exact name of the causative drugs in 558 cases.
Table 2.
Number of emergency patients transported to hospital by ambulance in Osaka City, Japan, 1998–2010 by drug category, based on codes from the International Classification of Diseases, 10th Revision
| T36–50 Poisoning by drugs, medicaments and biological substances | |
|---|---|
| T36 Poisoning by systemic antibiotics | 8 |
| T37 Poisoning by other systemic anti‐infectives and antiparasitics | 2 |
| T38 Poisoning by hormones and their synthetic substitutes and antagonists, not classified elsewhere | 23 |
| T39 Poisoning by non‐opioid analgesics, antipyretics and antirheumatics | 60 |
| T40 Poisoning by narcotics and psychodysleptics (hallucinogens) | 6 |
| T41 Poisoning by anesthetics and therapeutic gases | 4 |
| T42 Poisoning by antiepileptic, sedative‐hypnotic and antiparkinsonism drugs | 1,038 |
| T43 Poisoning by psychotropic drugs, not classified elsewhere | 108 |
| T44 Poisoning by drugs primarily affecting the autonomic nervous system | 0 |
| T45 Poisoning by primarily systemic and hematological agents, not classified elsewhere | 0 |
| T46 Poisoning by agents primarily affecting the cardiovascular system | 13 |
| T47 Poisoning by agents primarily affecting the gastrointestinal system | 17 |
| T48 Poisoning by agents primarily acting on smooth and skeletal muscles and the respiratory system | 49 |
| T49 Poisoning by topical agents primarily affecting the skin and mucous membranes and by ophthalmological, otorhinolaryngological, and dental drugs | 3 |
| T50 Poisoning by diuretics and other and unspecified drugs, medicaments and biological substances | 35 |
| Unknown | 558 |
Discussion
Our results clearly show that cases of suspected drug overdose have increased. The number of all emergency cases has also increased, particularly due to the increase in the number of older emergency patients. However, the increase in overdose patients was demonstrated after the data were age and sex adjusted. Furthermore, we showed that the age and sex distribution patterns and trends in overdose cases differed from those in non‐overdose cases. Although time for emergency transport of non‐overdose patients has increased, this tendency has particularly accelerated in overdose patients in recent years.
The greater availability and use of drugs have placed more emphasis on the importance of emergency care for patients with drug overdose. It is one of the contemporary problems in emergency care. Population‐based analyses of prehospital data provide important information for understanding the features of specific kinds of emergency patients. These analyses have an impact on strategies for patient care or disease prevention, such as out‐of‐hospital cardiac arrest or trauma.13, 14 Data from this approach may give us a different view by analysis of the data from the cases in specific hospitals or for specific drugs.
Our results show that drug overdose patients represented approximately 1% of all emergency patients. This is consistent with other studies.15, 16 However, the number of opioid overdoses in our study was small compared to reports from other cities.17, 18 Merchant et al. found that 18.6% of ambulance runs for drug overdose were for cases with suspected opiate overdose.18 The small number of such cases in Osaka reflects the strict prohibition of illicit drugs and their extremely limited use in Japan compared with other countries. Osaka police statistics (including the city area and surrounding suburbs of Osaka prefecture) for 2010 showed only 20 arrests involving opiates including heroin and cocaine.19 The US Centers for Disease Control and Prevention emphasizes that not only opioid analgesics but also any drug of the codes T36–T50, except T40, should be noted as a cause of drug poisoning by overdose.1 Our results suggest that overdose with drugs other than opioid analgesics is a common and shared problem worldwide.3, 20 In opioid abuse in other countries, it has been reported that males represent the majority of overdose patients.17, 18, 21 In contrast, in our report in which sedative drugs other than opioid analgesics are the main causes of drug overdose, females were predominant. This has been also reported in other surveys from hospital‐based studies.22
Emergency needs in Japanese society have recently changed from a severe trauma model, for traffic accidents or work injuries, to a disease model for elderly patients. As aging in society proceeds, the number and proportion of older women has increased among emergency patients. In contrast to this trend for non‐overdose patients, the age and sex distribution of overdose patients has remained unchanged. This suggests that the increase overdose patients has not arisen from the aging of society, although it has been suggested that an aging society influences this problem due to an increased number of cases of self‐poisoning in older adults and adverse drug events in older patients.23, 24
Our findings clearly show an increased burden on the EMS system. A trend for an increased time from the emergency call to arrival at hospital was found for all emergency patients, and this increase was particularly marked for drug overdose cases. This problem may come from the increase in the total number of cases and the difficulty in obtaining permission from hospitals to transport these patients to their service. It is essential to overcome this problem by discussing sedative abuse in Japan, although this problem is related to various issues including the improvement of the EMS system.25 Characteristics of suspected overdose cases are unique among emergency cases and involve problems that are beyond the technical issues of medical care and are a potential threat to the whole EMS system.26, 27
Limitations
Limitations of this study include the fact that at data were collected in the process of prehospital care. Our information of events is limited in terms of causative drugs compared with a hospital study. The EMS crews could consult with emergency physicians about the type of overdose drugs on hospital arrival. However, their information is often limited in the initial phase of an event and ambulance crews did not necessarily follow the cases. In addition, we could not exclude the possibility that other substances, such as agricultural chemicals, were reporting errors of EMS crews.
Conclusion
In conclusion, this study shows that the characteristics and trends of drug overdose patients are clearly different from those of non‐overdose patients. The features of drug overdose cases suggest unique emergency needs in drug overdose. It takes more time to obtain acceptance from hospitals to care the patients with drug overdose in recent years. Recent trends of drug overdose patients demonstrate the accelerated burden on EMS system.
Conflict of Interest
None.
Acknowledgements
We thank all the EMS crews and concerned physicians in Osaka City, and the staff of Osaka City Municipal Fire Department, particularly Sumito Hayashida and Takeo Oka. This study was supported by Grants‐in‐Aid for Scientific Research (Kakenhi) from the Ministry of Education, Culture, Sports, Science and Technology, Japan (No.25670771).
References
- 1. Centers for Disease Control and Prevention . QuickStats: Number of poisoning deaths* involving opioid analgesics and other drugs or substances—United States, 1999–2007. MMWR Morb. Mortal. Wkly Rep. 2010; 59: 1026. [Google Scholar]
- 2. Centers for Disease Control and Prevention . Drug overdose deaths—Florida, 2003–2009. MMWR Morb. Mortal. Wkly Rep. 2011; 60: 869–872. [PubMed] [Google Scholar]
- 3. Fisher J, Sanyal C, Frail D, Sketris I. The intended and unintended consequences of benzodiazepine monitoring programmes: A review of the literature. J. Clin. Pharm. Ther. 2012; 37: 7–21. [DOI] [PubMed] [Google Scholar]
- 4. Li C, Martin BC. Trends in emergency department visits attributable to acetaminophen overdoses in the United States: 1993–2007. Pharmacoepidemiol. Drug Saf. 2011; 20: 810–818. [DOI] [PubMed] [Google Scholar]
- 5. Benson BE, Mathiason M, Dahl B et al Toxicities and outcomes associated with nefazodone poisoning: An analysis of 1,338 exposures. Am. J. Emerg. Med. 2000; 18: 587–592. [DOI] [PubMed] [Google Scholar]
- 6. Bailey B, McGuigan M. Lithium poisoning from a poison control center perspective. Ther. Drug Monit. 2000; 22: 650–655. [DOI] [PubMed] [Google Scholar]
- 7. Cheatle MD. Depression, chronic pain, and suicide by overdose: On the edge. Pain Med. 2011; 12 (Suppl. 2): S43–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Centers for Disease Control and Prevention . CDC grand rounds: Prescription drug overdoses—a U.S. epidemic. MMWR Morb. Mortal. Wkly Rep. 2012; 61: 10–13. [PubMed] [Google Scholar]
- 9. Buykx P, Loxley W, Dietze P, Ritter A. Medications used in overdose and how they are acquired—an investigation of cases attending an inner Melbourne emergency department. Aust. N. Z. J. Public Health 2010; 34: 401–404. [DOI] [PubMed] [Google Scholar]
- 10. Taylor DM, Cameron PA, Eddey D. Recurrent overdose: Patient characteristics, habits, and outcomes. J. Accid. Emerg. Med. 1998; 15: 257–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Prescott K, Stratton R, Freyer A, Hall I, Le Jeune I. Detailed analyses of self‐poisoning episodes presenting to a large regional teaching hospital in the UK. Br. J. Clin. Pharmacol. 2009; 68: 260–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Spiller HA, Gorman SE, Villalobos D et al Prospective multicenter evaluation of tramadol exposure. J. Toxicol. Clin. Toxicol. 1997; 35: 361–364. [DOI] [PubMed] [Google Scholar]
- 13. Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out‐of‐hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation 2010; 81: 1479–1487. [DOI] [PubMed] [Google Scholar]
- 14. Newgard CD, Sears GK, Rea TD et al The Resuscitation Outcomes Consortium Epistry‐Trauma: Design, development, and implementation of a North American epidemiologic prehospital trauma registry. Resuscitation 2008; 78: 170–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Togia A, Sergentanis TN, Sindos M et al Drug abuse‐related emergency calls: A metropolis‐wide study. Prehosp. Disaster Med. 2008; 23: 36–40. [DOI] [PubMed] [Google Scholar]
- 16. Seidler D, Schmeiser‐Rieder A, Schlarp O, Laggner AN. Heroin and opiate emergencies in Vienna: Analysis at the municipal ambulance service. J. Clin. Epidemiol. 2000; 53: 734–741. [DOI] [PubMed] [Google Scholar]
- 17. Clark MJ, Bates AC. Nonfatal heroin overdoses in Queensland, Australia: An analysis of ambulance data. J. Urban Health 2003; 80: 238–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Merchant RC, Schwartzapfel BL, Wolf FA, Li W, Carlson L, Rich JD. Demographic, geographic, and temporal patterns of ambulance runs for suspected opiate overdose in Rhode Island, 1997–20021. Subst. Use Misuse 2006; 41: 1209–1226. [DOI] [PubMed] [Google Scholar]
- 19. Osaka Police (Homepage on the internet) . [cited 25 Dec 2014]. Available from: http://www.police.pref.osaka.jp/05bouhan/yakubutsu/01genjo02_1.html.
- 20. Buckley NA, McManus PR. Changes in fatalities due to overdose of anxiolytic and sedative drugs in the UK (1983–1999). Drug Saf. 2004; 27: 135–141. [DOI] [PubMed] [Google Scholar]
- 21. Hasegawa K, Brown DF, Tsugawa Y, Camargo CA Jr. Epidemiology of emergency department visits for opioid overdose: A population‐based study. Mayo Clin. Proc. 2014; 89: 462–471. [DOI] [PubMed] [Google Scholar]
- 22. Ookura R, Mino K, Ogata M. Clinical characteristics of patients with psychotropic drug overdose admitted to the emergency department. J. Jpn. Soc. Emerg. Med. 2008; 19: 901–913. [Google Scholar]
- 23. Doak MW, Nixon AC, Lupton DJ, Waring WS. Self‐poisoning in older adults: Patterns of drug ingestion and clinical outcomes. Age. Ageing 2009; 38: 407–411. [DOI] [PubMed] [Google Scholar]
- 24. Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N. Engl. J. Med. 2011; 365: 2002–2012. [DOI] [PubMed] [Google Scholar]
- 25. Matsumoto T, Ozaki S, Kobayashi O, Wada K. Current situation and clinical characteristics of sedative‐related disorder patients in Japan: A comparison with methamphetamine‐related disorder patients. Seishin Shinkeigaku Zasshi 2011; 113: 1184–1188. [PubMed] [Google Scholar]
- 26. Degenhardt L, Hall W, Adelstein BA. Ambulance calls to suspected overdoses: New South Wales patterns July 1997 to June 1999. Aust. N. Z. J. Public Health 2001; 25: 447–450. [PubMed] [Google Scholar]
- 27. Perez A. Critical drug overdoses and emergency medical services: Where should we put our efforts? Acad. Emerg. Med. 2004; 11: 1369. [DOI] [PubMed] [Google Scholar]


