Abstract
Aim
To investigate whether lower radiation doses may yield similar outcome measures to those from the COMS trial.
Methods
A literature review of English language articles was performed using the PubMed database of the U.S. National Library of Medicine and the Cochrane Central Register of Controlled Trials using the following keywords: uveal melanoma, choroidal melanoma, primary uveal malignant melanoma, iodine-125 brachytherapy, local recurrence, local treatment failure, and local tumor control. The relationships between study local recurrence rate and median dosage were tested by linear regression, with each study weighted by the number of patients included.
Results
Fifteen retrospective and prospective studies were selected for systematic review (2,662 patients). Ranges of reported mean or median radiation dose to tumor apex were 62.5–104.0 Gy. Local recurrence rates ranged from 0 to 24%. A 1.0-Gy increase in the average study dose was associated with a 0.14% decrease in local recurrence rate, which was not statistically significant (p value 0.336).
Conclusion
The gold standard empirically derived 85.0-Gy radiation dose for the treatment of uveal melanoma could be tested in a randomized study.
Keywords: Uveal melanoma, Brachytherapy, Radiation dose, COMS trial
Introduction
Historical Background
The treatment of uveal melanoma has evolved significantly, from enucleation to eye-preserving episcleral plaque brachytherapy, since the first implantation of mesothorium (radium-228) capsules in fractioned doses by Deutschmann [1] in Germany in 1915 [2]. R. Foster Moore [3] introduced intralesional implantation of radon seeds in England in 1929. A 1-millicurie seed was implanted for 2 weeks, but the tumor was later retreated with implantation of a 5-millicurie seed, due to the lack of tumor regression observed 3 months following initial treatment. One year following the first implantation, it was shown that the tumor had regressed and vision was preserved. In 1966, Lommatzsch and Vollmar [4] were among the first to describe dose parameters in the treatment of uveal melanoma with the use of ruthenium-106 applicators [2]. In their case series, they reported contact scleral doses between 20,000–60,000 rads (200.0–600.0 Gy). Although they did not state an apical dose, with a maximal contact scleral dose of 600.0 Gy, approximately 10% of isodose is expected at the depth of 6.8 mm. Therefore, a tumor measuring 7.0 mm would have been only treated with 60.0 Gy to tumor apex (10% of contact scleral dose of 600.0 Gy), which could explain their relatively large amount of local recurrences or re-treatments needed (approximately 30%).
In the 1960s, H.B. Stallard [5, 6] popularized the use of cobalt-60 episcleral plaques to treat choroidal melanomas. His initial clinical data and calculations from isodose curves suggested that episcleral brachytherapy delivering a range of 7,000–14,000 rads (equivalent to 70.0–140.0 Gy) to the tumor apex could be a globe-preserving therapeutic alternative to enucleation with non-inferior mortality rates. Due to the commercial availability of standardized cobalt plaques, the fact that the long half-life allowed for reuse, and the reproducibility of the technique, Stallard established this protocol as the best alternative to enucleation [7]. In the 1970s, Rotman et al. [8] reported survival rates similar to enucleation using cobalt-60 applicators with a dose of 85–100 Gy. They expressed their single-institution opinion based upon an unspecified number of patients that higher dose rates (50 rads/h) provided more effective local control than the lower dose rates (30 rads/h) with the same total dose of 8,500 rads to the tumor apex. Interestingly, they suggested that lowering total doses may be possible if an adequate dose rate was maintained. No statistical proof of these statements was reported.
Subsequent efforts to reduce the incidence of radiation-induced complications led to the introduction of low-emitting isotopes such as iodine-125. In the 1970s, the transition to iodine-125 plaques was led by Rotman and Packer [7, 8, 9, 10], when dosimetric comparisons between cobalt-60 and iodine-125 isotopes showed that for a depth of 10 mm there is basically no difference in dose penetration, and for depths at 15 mm there is only a 5% reduction in dose penetration of iodine-125 when compared to cobalt-60 [9]. The Greene melanoma rabbit model provided histological evidence of iodine-125 sparing adjacent tissue such as the lens and retina at more favorable rates than cobalt-60 brachytherapy [9]. The latter findings, in addition to a much safer profile by iodine-125 for both the patient and surgeon, given the ability to shield its radioactivity with merely a 0.5-mm gold sheet cover, led to the establishment of iodine-125 plaques as most widely used isotope for brachytherapy [11].
Current Practices
Beginning in 1986, the Collaborative Ocular Melanoma Study (COMS) was the first prospective randomized clinical trial comparing iodine-125 plaque brachytherapy with enucleation for patients with medium-sized tumors. The minimal radiation dose to the tumor apex used in the COMS trial was 85.0 Gy. A minimum of 85.0 Gy was prescribed to the depth of 5.0 mm from the inner sclera for tumors less than 5.0 mm in apical height. This dose was adjusted (originally 100.0 Gy) after the Task Group (TG 43) protocol was adopted by the American Association of Physicists in Medicine [12]. The dose of 85.0 Gy for the COMS trial was selected based upon expert consensus [9, 11, 13, 14, 15]. The COMS study showed that an eye-preserving, and potentially a vision-preserving, therapeutic regimen with iodine-125 plaque brachytherapy had a non-inferior mortality risk compared to enucleation up to 12 years following treatment [16]. These data established iodine-125 brachytherapy as the gold standard for treating medium-sized uveal melanoma with the 5-year risk of local treatment failure of 10.3% [17]. Published studies have suggested that local recurrence increases the potential for metastasis [18, 19, 20, 21].
Study Question
The lack of evidence regarding optimal plaque radiation dose presents an opportunity to investigate whether doses lower than the COMS standard of 85.0 Gy to the tumor apex would provide a comparable therapeutic profile with a non-inferior local control rate [17]. To our knowledge, there has been no systematic review of retrospective or prospective clinical studies evaluating the relationship between dose to tumor apex and local recurrence rates of patients with uveal melanoma treated with iodine-125 brachytherapy. This study aims to investigate whether lower radiation doses may yield similar outcome measures to those from the COMS trial, specifically as related to local control during the initial 5 years of posttreatment brachytherapy. Having lower radiation doses with a comparable local recurrence rate would represent a more efficient treatment profile that would limit secondary side effects from dose-related radiation toxicity.
Materials and Methods
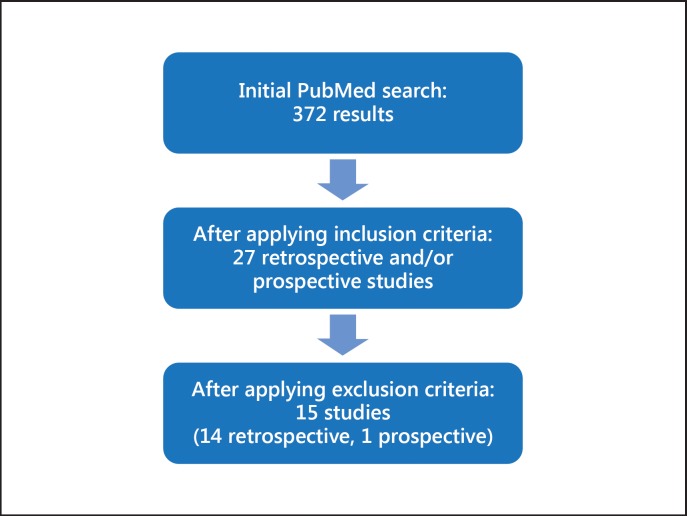
Since our study involves a review of previously published peer-reviewed literature, no institutional approval was required. Our literature review of English language articles was performed using the PubMed database of the U.S. National Library of Medicine and the Cochrane Central Register of Controlled Trials of the Cochrane Library using the following keywords: uveal melanoma, choroidal melanoma, primary uveal malignant melanoma, iodine-125 brachytherapy, local recurrence, local treatment failure, and local tumor control. Our initial search yielded 327 reports. We then applied the following inclusion criteria: (1) English language articles, (2) primary intervention with iodine-125 brachytherapy, (3) reported mean or median radiation dose to tumor apex, (4) reported local recurrence rate (%), (5) reported mean tumor dimensions of largest basal diameter and apical tumor height, and (6) reported mean follow-up time of 30 months (Fig. 1). These yielded a total of 27 studies. We then excluded those studies in which the dose to tumor apex had not been adjusted to the TG-43 protocol recommendations, which led to a final selection of 15 studies (14 retrospective, 1 prospective). The characteristics of each study selected for review included: number of patients, mean radiation dose to tumor apex (Gy), local recurrence rate (%), mean tumor largest basal diameter (mm), mean tumor apical height (mm), and mean follow-up time (months). For those studies that reported multiple data points corresponding to different lengths of follow-up, the local recurrence rate closest to 5 years (60 months) posttreatment follow-up was selected for our review (Table 1).
Fig. 1.
Flow diagram of systematic review of literature and study selection.
Table 1.
Characteristics of selected retrospective and prospective
| Study (first author) | Year | Type of study | Isotope | Mean dose, Gy | Patients, n | Local recurrence rate, % | Mean largest basal diameter, mm | Mean tumor height, mm | Mean follow-up, months |
|---|---|---|---|---|---|---|---|---|---|
| With echographic confirmation | |||||||||
| Tabandeh [22] | 2000 | retrospective | iodine-125 | 85 | 117 | 1.7 | 9.6 | 4.2 | 37 |
| Saconn [23] | 2010 | retrospective | iodine-125 | 62.5 | 62 | 8.7 | 11.4 | 4.6 | 58 (median) |
| McCannel [24] | 2012 | retrospective | iodine-125 | 85 | 170 | 0 | 10.8 | 4.8 | 32.4 |
| Badiyan [25] | 2014 | retrospective | iodine-125/supplemental TTT | 97.8 | 526 | 3.6 | 12.2 | 4.2 | 53.4 |
| Murray [26] | 2013 | retrospective | iodine-125 | 85 | 55 | 1 | 10.7 | 3.3 | 145.2 |
| Aziz [27] | 2016 | retrospective | iodine-125 and ruthenium-106 | 85 | 198 | 1.5 | 11.3 | 4.1 | 25.6 |
| Without echographic confirmation | |||||||||
| Jampol (COMS) | 2002 | prospective | iodine-125 | 85 | 650 | 10.3 | 11.5 | 4.2 | 60 |
| [17] | randomized | ||||||||
| Puusaari [28] | 2003 | retrospective | iodine-125 | 87 (median) | 97 | 6 | 16.1 | 10.7 | 43 |
| Jensen [29] | 2005 | retrospective | iodine-125 | 104 (median) | 156 | 7 | 11.2 | 4 | 74 (median) |
| Correa [30] | 2009 | retrospective | iodine-125 | 82.9 | 120 | 11.6 | 12.2 (median) | 5.9 (median) | 50.4 (median) |
| Leonard [31] | 2011 | retrospective | iodine-125 | 85 | 37 | 24 | 12.3 | 6.3 | 100 |
| Karlovits [32] | 2011 | retrospective | iodine-125 | 86 | 35 | 0 | 13.5 | 7.8 | 60 |
| Berry [14] | 2013 | retrospective | iodine-125 | 85 | 82 | 2.4 | 10.7 | 4.6 | 46.8 (median) |
| Perez [15] | 2014 | retrospective | iodine-125 | 190 | 9 | 11.0 (median) | 3.9 (median) | 49.2 (median) | |
| <69 | 48 | 6 | |||||||
| 69–81 | 47 | 11 | |||||||
| 81–89 | 48 | 15 | |||||||
| >89 | 47 | 4 | |||||||
| Wisely [34] | 2016 | retrospective | iodine-125 | 85.8 (median) | 113 | 5.3 | 10.5 (median) | 4 (median) | 65.5 (median) |
| Aziz [27] | 2016 | retrospective | iodine-125 and ruthenium-106 | 85 | 54 | 9.3 | 11.1 | 3.6 | 50.4 |
The relationships between study local recurrence rate and study features, like median dosage or median follow-up time, were tested by linear regression, with each study weighted by the number of patients included. All statistical analysis was conducted in R version 3.2.3. A regression coefficient was considered significant if the p value was <0.05.
Results
After a review of the literature, 15 retrospective and prospective studies were selected for systematic review for a total of 2,662 patients. Fourteen studies were retrospective clinical chart reviews [14, 15, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32], and 1 was a prospective, randomized trial, the COMS trial [17]. One retrospective study included patients from the COMS trial [15]. Ranges of number of patients per study were 35–650. Ranges of reported mean or median radiation dose to tumor apex were 62.5–104.0 Gy. Local recurrence rates ranged from 0 to 24%, mean largest basal diameter from 9.6 to 16.1 mm, and mean tumor height from 3.3 to 10.7 mm. A 1.0-Gy increase in the average study dose was associated with a 0.14% decrease in local recurrence rate, which was not statistically significant (p value 0.336) (Fig. 2). The mean follow-up time of the published studies varied from 25.6 to 145 months.
Fig. 2.
Published studies. Association between median dose and control rate. The x axis shows radiation dose in Gy. Points represent the median dose reported in a study. The size of the point corresponds to the number of subjects in the study. The y axis is the reported local control rate of the study. The blue line represents the line of best fit, weighted by the number of subjects in the study. The grey areas represent the standard error associated with the line of best fit. Because the grey area includes a potentially horizontal line, we cannot exclude that there is no relationship between study median dose and control rate.
Discussion
The COMS study design raises a dilemma as to whether the consensus-driven selection of the dose to the tumor apex (85.0 Gy) represents the most optimal dose. One of the limitations of the COMS trial was that patients with tumors with apical height ≤5.0 mm received the minimal radiation dose of 85.0 Gy, as indicated to 5.0 mm deep to the inner sclera and irrespective of true apical height. The possibility that these patients received a larger dose than required for adequate tumor regression is an important question, since a lower dose may render similar tumor regression with a lower incidence of secondary adverse effects from the radiation damage.
A previous review compared the local treatment failure rates of different globe-conserving therapies for choroidal melanoma, including photon-based external beam radiation, charged particle beam radiation, plaque brachytherapy treatment (iodine, ruthenium, palladium, cesium), transpupillary thermotherapy, and surgical resection [33]. Radiation therapy overall resulted in lower treatment failure rates compared to other treatment modalities, but no consideration was given to the average radiation dose used in each study. To our knowledge, there have been no prospective clinical trials comparing doses in the treatment of uveal melanoma. There have been a few single-institution retrospective studies suggesting that patients with tumors with an apical height of <5.0 mm benefit from lower doses of radiation [21, 23, 26]. Saconn et al. [23] reported a series of 62 patients treated with a dose-reduced COMS design regimen with a mean prescription dose of 62.5 Gy to the tumor apex. Their local control rate was comparable to the COMS trial (9 vs. 10.3%, respectively) with 73% of patients having a tumor height between 2.5 and 5.0 mm. In 2013, Murray et al. [26] reported no significant differences in local control rates between patients treated with an adjusted dose to the apical height and those treated with the standard COMS design dose of 85.0 Gy to a depth of 5.0 mm. The latter study suggested that dose to the true apical height may render a lower incidence of radiation-related complications. In another retrospective case study of 190 patients, Perez et al. [15] showed data stratified by varied dose quartiles (<65.0 to >85.0 Gy) and reported no association between dose to tumor apex and rate of local failure (9%), which was similar to the COMS trial despite having significantly reduced doses in 50% of their patients. By stratifying their treatment groups to different dose quartiles, they also found a direct relationship between radiation dose and ocular toxicity. They suggested a dose to the tumor apex of less than 85.0 Gy especially for tumors less than 5.0 mm in height. Although the above-mentioned studies argue in favor of a dose reduction for episcleral brachytherapy in the treatment of uveal melanoma, their retrospective designs and few numbers of patients limit their statistical power.
Our review of 2,662 patients from 15 clinical studies is the largest analysis of its kind comparing doses to tumor apex in relation to local control rates. Our study entails a systematic review of retrospective studies showing local control rates of uveal melanoma after treatment with episcleral iodine-125 brachytherapy. One of the limitations of our study is the inclusion of retrospective studies due to lack of prospective, randomized trials, which makes it difficult to perform a formal meta-analysis. This is due mainly to the lack of existing prospective, randomized trials for the treatment of uveal melanoma with episcleral iodine brachytherapy beyond the COMS trial. Any future prospective studies will have to standardize methodology of tumor height measurements and adjust for dosimetric variations due to episcleral plaque designs.
The systematic review of published data suggests that the gold standard for the treatment of uveal melanoma with iodine brachytherapy using a radiation dose of the empirically derived 85.0 Gy to tumor apex could be tested in a randomized study. Tumors less than 5.0 mm in height from lower doses adjusted to true apical height rather than those established by the COMS trial need further assessment.
Statement of Ethics
The study complied with the guidelines for human studies and animal welfare regulations. The subject gave informed consent and the study protocol was approved by the institute's committee on human research.
Disclosure Statement
The authors have no conflicts of interest to declare.
References
- 1.Deutschmann R. Ueber intraokularen Tumor und Strahlentherapie. Z Augenheilkd. 1915;33:206–209. [Google Scholar]
- 2.Bechrakis NE, Blatsios G, Haas G. Short review of the history of radiotherapy for intraocular tumours (in German) Klin Monbl Augenheilkd. 2015;232:834–837. doi: 10.1055/s-0035-1546187. [DOI] [PubMed] [Google Scholar]
- 3.Moore RF. Choroidal sarcoma treated by intraocular insertion of radon seeds. Br J Ophthalmol. 1930;14:145–152. doi: 10.1136/bjo.14.4.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lommatzsch P, Vollmar R. A new way in the conservative therapy of intraocular tumors by means of beta-irradiation (Ruthenium 106) with preservation of vision (in German) Klin Monbl Augenheilkd. 1966;148:682–699. [PubMed] [Google Scholar]
- 5.Stallard HB. Malignant Melanoma of the Choroid treated with Radioactive Applicators: Hunterian Lecture delivered at the Royal College of Surgeons of England on 29th November 1960. Ann R Coll Surg Engl. 1961;29:170–182. [PMC free article] [PubMed] [Google Scholar]
- 6.Stallard HB. Radiotherapy for malignant melanoma of the choroid. Br J Ophthalmol. 1966;50:147–155. doi: 10.1136/bjo.50.3.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Packer S, Rotman M. Radiotherapy of choroidal melanoma with iodine-125. Ophthalmology. 1980;87:582–590. doi: 10.1016/s0161-6420(80)35194-4. [DOI] [PubMed] [Google Scholar]
- 8.Rotman M, Long RS, Packer S, Moroson H, Galin MA, Chan B. Radiation therapy of choroidal melanoma. Trans Ophthalmol Soc UK. 1977;97:431–435. [PubMed] [Google Scholar]
- 9.Packer S, Rotman M, Fairchild RG, Albert DM, Atkins HL, Chan B. Irradiation of choroidal melanoma with iodine 125 ophthalmic plaque. Arch Ophthalmol. 1980;98:1453–1457. doi: 10.1001/archopht.1980.01020040305019. [DOI] [PubMed] [Google Scholar]
- 10.Rotman M, Packer S, Albert D, Fairchild R, Chan B. Removable iodine-125 ophthalmic applicators in the treatment of ocular tumors. Int J Radiat Oncol Biol Phys. 1978;4:238–239. [Google Scholar]
- 11.Earle J, Kline RW, Robertson DM. Selection of iodine 125 for the Collaborative Ocular Melanoma Study. Arch Ophthalmol. 1987;105:763–764. doi: 10.1001/archopht.1987.01060060049030. [DOI] [PubMed] [Google Scholar]
- 12.Nath R, Anderson LL, Luxton G, Weaver KA, Williamson JF, Meigooni AS. Dosimetry of interstitial brachytherapy sources: recommendations of the AAPM Radiation Therapy Committee Task Group No. 43. American Association of Physicists in Medicine. Med Phys. 1995;22:209–234. doi: 10.1118/1.597458. [DOI] [PubMed] [Google Scholar]
- 13.Design and methods of a clinical trial for a rare condition: the Collaborative Ocular Melanoma Study. COMS Report No. 3. Control Clin Trials. 1993;14:362–391. doi: 10.1016/0197-2456(93)90052-f. [DOI] [PubMed] [Google Scholar]
- 14.Berry JL, Dandapani SV, Stevanovic M, et al. Outcomes of choroidal melanomas treated with eye physics: a 20-year review. JAMA Ophthalmol. 2013;131:1435–1442. doi: 10.1001/jamaophthalmol.2013.4422. [DOI] [PubMed] [Google Scholar]
- 15.Perez BA, Mettu P, Vajzovic L, et al. Uveal melanoma treated with iodine-125 episcleral plaque: an analysis of dose on disease control and visual outcomes. Int J Radiat Oncol Biol Phys. 2014;89:127–136. doi: 10.1016/j.ijrobp.2014.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collaborative Ocular Melanoma Study Group The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma: V. Twelve-year mortality rates and prognostic factors: COMS report No. 28. Arch Ophthalmol. 2006;124:1684–1693. doi: 10.1001/archopht.124.12.1684. [DOI] [PubMed] [Google Scholar]
- 17.Jampol LM, Moy CS, Murray TG, et al. The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma: IV. Local treatment failure and enucleation in the first 5 years after brachytherapy. COMS report no. 19. Ophthalmology. 2002;109:2197–2206. doi: 10.1016/s0161-6420(02)01277-0. [DOI] [PubMed] [Google Scholar]
- 18.Vrabec TR, Augsburger JJ, Gamel JW, Brady LW, Hernandez C, Woodleigh R. Impact of local tumor relapse on patient survival after cobalt 60 plaque radiotherapy. Ophthalmology. 1991;98:984–988. doi: 10.1016/s0161-6420(91)32193-6. [DOI] [PubMed] [Google Scholar]
- 19.Char DH, Kroll S, Phillips TL. Uveal melanoma. Growth rate and prognosis. Arch Ophthalmol. 1997;115:1014–1018. doi: 10.1001/archopht.1997.01100160184007. [DOI] [PubMed] [Google Scholar]
- 20.Harbour JW, Murray TG, Byrne SF, et al. Intraoperative echographic localization of iodine 125 episcleral radioactive plaques for posterior uveal melanoma. Retina. 1996;16:129–134. doi: 10.1097/00006982-199616020-00008. [DOI] [PubMed] [Google Scholar]
- 21.Ophthalmic Oncology Task Force Local Recurrence Significantly Increases the Risk of Metastatic Uveal Melanoma. Ophthalmology. 2016;123:86–91. doi: 10.1016/j.ophtha.2015.09.014. [DOI] [PubMed] [Google Scholar]
- 22.Tabandeh H, Chaudhry NA, Murray TG, et al. Intraoperative echographic localization of iodine-125 episcleral plaque for brachytherapy of choroidal melanoma. Am J Ophthalmol. 2000;129:199–204. doi: 10.1016/s0002-9394(99)00315-3. [DOI] [PubMed] [Google Scholar]
- 23.Saconn PA, Gee CJ, Greven CM, McCoy TP, Ekstrand KE, Greven KM. Alternative dose for choroidal melanoma treated with an iodine-125 radioactive plaque: a single-institution retrospective study. Int J Radiat Oncol Biol Phys. 2010;78:844–848. doi: 10.1016/j.ijrobp.2009.08.059. [DOI] [PubMed] [Google Scholar]
- 24.McCannel TA, Chang MY, Burgess BL. Multi-year follow-up of fine-needle aspiration biopsy in choroidal melanoma. Ophthalmology. 2012;119:606–610. doi: 10.1016/j.ophtha.2011.08.046. [DOI] [PubMed] [Google Scholar]
- 25.Badiyan SN, Rao RC, Apicelli AJ, et al. Outcomes of iodine-125 plaque brachytherapy for uveal melanoma with intraoperative ultrasonography and supplemental transpupillary thermotherapy. Int J Radiat Oncol Biol Phys. 2014;88:801–805. doi: 10.1016/j.ijrobp.2013.12.014. [DOI] [PubMed] [Google Scholar]
- 26.Murray TG, Markoe AM, Gold AS, et al. Long-term followup comparing two treatment dosing strategies of (125) I plaque radiotherapy in the management of small/medium posterior uveal melanoma. J Ophthalmol. 2013;2013:517032. doi: 10.1155/2013/517032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aziz HA, Al Zahrani YA, Bena J, et al. Episcleral brachytherapy of uveal melanoma: role of intraoperative echographic confirmation. Br J Ophthalmol. 2016 doi: 10.1136/bjophthalmol-2016-309153. DOI: 10.1136/bjophthalmol-2016-309153. [DOI] [PubMed] [Google Scholar]
- 28.Puusaari I, Heikkonen J, Summanen P, Tarkkanen A, Kivela T. Iodine brachytherapy as an alternative to enucleation for large uveal melanomas. Ophthalmology. 2003;110:2223–2234. doi: 10.1016/S0161-6420(03)00661-4. [DOI] [PubMed] [Google Scholar]
- 29.Jensen AW, Petersen IA, Kline RW, Stafford SL, Schomberg PJ, Robertson DM. Radiation complications and tumor control after 125I plaque brachytherapy for ocular melanoma. Int J Radiat Oncol Biol Phys. 2005;63:101–108. doi: 10.1016/j.ijrobp.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 30.Correa R, Pera J, Gomez J, et al. (125)I episcleral plaque brachytherapy in the treatment of choroidal melanoma: a single-institution experience in Spain. Brachytherapy. 2009;8:290–296. doi: 10.1016/j.brachy.2009.03.189. [DOI] [PubMed] [Google Scholar]
- 31.Leonard KL, Gagne NL, Mignano JE, Duker JS, Bannon EA, Rivard MJ. A 17-year retrospective study of institutional results for eye plaque brachytherapy of uveal melanoma using (125)I, (103)Pd, and (131)Cs and historical perspective. Brachytherapy. 2011;10:331–339. doi: 10.1016/j.brachy.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 32.Karlovits B, Trombetta MG, Verstraeten T, Johnson M, Wong M, Karlovits S. Local control and visual acuity following treatment of medium-sized ocular melanoma using a contact eye plaque: a single surgeon experience. Brachytherapy. 2011;10:228–231. doi: 10.1016/j.brachy.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 33.Chang MY, McCannel TA. Local treatment failure after globe-conserving therapy for choroidal melanoma. Br J Ophthalmol. 2013;97:804–811. doi: 10.1136/bjophthalmol-2012-302490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wisely CE, Hadziahmetovic M, Reem RE, Hade EM, Nag S, Davidorf FH, Martin D, Cebulla CM. Long-term visual acuity outcomes in patients with uveal melanoma treated with 125I episcleral OSU-Nag plaque brachytherapy. Brachytherapy. 2016;15:12–22. doi: 10.1016/j.brachy.2015.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]