Abstract
Calbindin D-28K (CB), a Ca2+-binding protein, maintains Ca2+ homeostasis and protects neurons against various insults. Hyperthermia can exacerbate brain damage produced by ischemic insults. However, little is reported about the role of CB in the brain under hyperthermic condition during ischemic insults. We investigated the effects of transient global cerebral ischemia on CB immunoreactivity as well as neuronal damage in the hippocampal formation under hyperthermic condition using immunohistochemistry for neuronal nuclei (NeuN) and CB, and Fluoro-Jade B histofluorescence staining in gerbils. Hyperthermia (39.5 ± 0.2°C) was induced for 30 minutes before and during transient ischemia. Hyperthermic ischemia resulted in neuronal damage/death in the pyramidal layer of CA1–3 area and in the polymorphic layer of the dentate gyrus at 1, 2, 5 days after ischemia. In addition, hyperthermic ischemia significantly decreaced CB immunoreactivity in damaged or dying neurons at 1, 2, 5 days after ischemia. In brief, hyperthermic condition produced more extensive and severer neuronal damage/death, and reduced CB immunoreactivity in the hippocampus following transient global cerebral ischemia. Present findings indicate that the degree of reduced CB immunoreactivity might be related with various neuronal damage/death overtime and corresponding areas after ischemic insults.
Keywords: nerve regeneration, hyperthermic condition, ischemia/reperfusion injury, subregions of hippocampus, delayed neuronal death, calbindin D-28k, neural regeneration
Introduction
Transient global cerebral ischemia (tGCI) kills pyramidal neurons in the CA1 sector (CA1) of the hippocampal cornu ammonis because CA1 pyramidal neurons are most vulnerable after tGCI; however, neurons in the CA2/3 and dentate gyrus are essentially resistant to tGCI (Kirino, 1982; Pulsinelli et al., 1982). It is well known that death of CA1 pyramidal neurons is described as “delayed neuronal death” because the death takes place several days after tGCI in gerbils (Kirino, 1982).
Calbindin D-28K (CB) is a major endogenous Ca2+ buffer and modulates intracellular Ca2+ concentration to maintain calcium homeostasis (Heizmann and Braun, 1992). It is prominently expressed in neurons including Purkinje cells in the cerebellum and pyramidal cells in the CA1 throughout the central nervous system (CNS) (Baimbridge et al., 1992). Excessive Ca2+ influx into neurons is one of triggers to induce neuronal death after ischemic insults. Increased intracellular Ca2+ level under pathological condition causes mitochondrial damage, and enzymatic breakdowns of proteins and lipids, and finally evokes cell death (Bano and Nicotera, 2007; Kumar et al., 2014). However, the precise mechanism of ischemia-induced delayed neuronal death has not been clear.
Some studies have shown that CB-containing neuronal populations are better able to survive ischemic and excitotoxic insults than those that lack CB (Mattson et al., 1991; Lee et al., 2004), namely, the overexpression of CB could decrease neuronal death following transient focal ischemia. In contrast, some researchers have reported that CB-containing neurons may be even more vulnerable to ischemic insults (Tortosa and Ferrer, 1994; Klapstein et al., 1998).
Elevated body temperature is one of critical factors to enhance neuronal damage after brain ischemia (Minamisawa et al., 1990; Corbett and Thornhill, 2000). Clinical studies have provided that ischemic stroke patients with mild hyperthermia show expanded infarction and the deteriorated outcome of ischemic stroke (Wang et al., 2000; Seo et al., 2008). Preclinical data have suggested several evidences that the harmful effects of post-ischemic hyperthermia lead to more harmful effects in animal models of ischemic insults such as tGCI (Dietrich et al., 1990), permanent focal cerebral ischemia (Chen et al., 1991) and transient focal cerebral ischemia (Kim et al., 1996). We have recently reported that hyperthermic condition before and during tGCI results in severer neuronal damage and glial activation in the gerbil hippocampus following tGCI (Kim et al., 2015).
In this regard, we examined, in this study, whether hyperthermic condition before and during tGCI affects alteration in CB immunoreactivity in the hippocampus following tGCI in gerbils which have been used as an animal model of tGCI (Lee et al., 2013; Kim et al., 2015).
Materials and Methods
Male Mongolian gerbils (Meriones unguiculatus; weighing 65–75 g; 6 months old) were obtained from the Lanoratory Animal Center, Kangwon National University, Chuncheon, South Korea and divided into two groups: (1) hyperthermia + sham group, animals in which were subjected to sham operation under hyperthermic condition and (2) hyperthermia + ischemia group, animals in which were subjected to tGCI under hyperthermic condition. The procedures for animal handling and care adhered to guidelines that are in compliance with the current international laws and policies (Guide for the Care and Use of Laboratory Animals, The National Academies Press, 8th Ed., 2011). Procedures for animal handling and care were approved by the Institutional Animal Care and Use Committee (IACUC) in Kangwon National University (approval No. KW-160802-1).
Induction of tGCI
As previously described (Kim et al., 2015), in short, gerbils were anesthetized via a mask using a gas mixture of 2.5% isoflurane (Baxtor, Deerfield, IL, USA) in 33% oxygen and 67% nitrous oxide gas. Both common carotid arteries were ligated for 5 minutes. Hyperthermia was induced by exposing the gerbils to a heating pad connected to a rectal thermistor (TR-100; Fine Science Tools, Foster City, CA, USA). Body (rectal) temperature was controlled under hyperthermia (39.5 ± 0.2°C) for 30 minutes before and during tGCI surgery and controlled under normothermia (37.5 ± 0.2°C) after the surgery. Animals of the sham group were exposed to the same operation without the occlusion of carotid arteries. Gerbils in each group were sacrificed 1, 2 and 5 days after tGCI, because death of pyramidal neurons presented in the CA1 from 4 days after tGCI.
Tissue processing
Briefly, as previously described (Kim et al., 2015), gerbils were anesthetized with 40 mg/kg pentobarbital sodium dissolved in saline was injected intraperitoneally and perfused throughout the heart with 4% paraformaldehyde. Their brains were more fixed with 4% paraformaldehyde for 6 hours, and serially sectioned into 30 μm coronal sections.
Fluoro-Jade B histofluorescence staining
Fluoro-Jade B (F-J B, a marker for neuronal degeneration localization) histofluorescence staining was carried out to examine neuronal death after tGCI according to our published procedure (Kim et al., 2015). In short, the brain tissues were immersed in a 0.06 % potassium permanganate solution and stained with 0.0004% F-J B (Histochem, Jefferson, AR, USA) solution. The stained brain tissues were observed using an epifluorescent microscope (Carl Zeiss, Göttingen, Germany) with blue (450–490 nm) excitation light and a barrier filter.
Immunohistochemistry
Neuronal nuclei (NeuN) (a marker for neurons) and CB immunohistochemistry were conducted according to our published method (Bae et al., 2015). Briefly, sections were treated with 0.3% hydrogen peroxide (H2O2) and then with 10% normal goat serum. Next, the sections were incubated with mouse anti-NeuN (diluted 1:1,000, Chemicon International, Temecula, CA, USA) or rabbit anti-CB (1:500, Chemicon International) at 4°C for 24 hours. Thereafter, the tissues were incubated in biotinylated goat anti-mouse IgG (Vector, Burlingame, CA, USA), biotinylated goat anti-rabbit (1:250, Vector) and streptavidin peroxidase complex (diluted 1:200, Vector) at room temperature (22°C) for 2 hours. Finally, the sections were visualized by staining with 3,3′-diaminobenzidine tetrahydrochloride.
Data analysis
Counts of NeuN-immunoreactive (NeuN+) and F-J B-positive (F-J B+) structures were done following our published procedure (Bae et al., 2015). In brief, 15 sections were chosen in each animal with 120 μm interval. all NeuN+ and F-J B+ cells were taken in the pyramidal layer of CA1–3 and the polymorphic layer of dentate gyrus through an AxioM1 light microscope (Carl Zeiss) equipped with a digital camera (Axiocam, Carl Zeiss, Oberkochen, Germany) interlinked with a PC monitor. The numbers of the observed cells were counted in a 200 × 200 μm square at the center of the CA1. The cell counts were analyzed as a percent, with the sham group designated as 100%.
To quantitatively analyze CB immunoreactivity, in brief, according to our method (Lee et al., 2016), images were calibrated into an array of 512 × 512 pixels corresponding to a tissue area of 140 × 140 μm (40× primary magnification). Mean CB immunoreactivity was measured in pyramidal neurons in the CA1 by a 0–255 gray scale system. The background density was subtracted, and a ratio of the relative immunoreactivity of image file was calibrated as percent using Adobe Photoshop version 8.0 (Adobe Systems, San Jose, CA, USA), and the relative immunoreactivity (RI) was analyzed using NIH Image 1.59 software (developed at the U.S. National Institute of Heath and available on the Internet at http.//rsb.info.nih.gov./nih-image/). A ratio of the RI was calibrated as percent, with sham group designated as 100%.
Statistical analysis
Data are expressed as the mean ± SEM using SPSS 17.0 software (IBM, New York, NY, USA). Difference between the groups was statistically analyzed by one-way analysis of variance (ANOVA) and Tukey multiple range post hoc test. Statistical significance was considered at P < 0.05.
Results
Neuronal cell death
Neuronal damage/death were shown by NeuN immunohistochemistry and F-J B histofluorescence.
NeuN+ cells
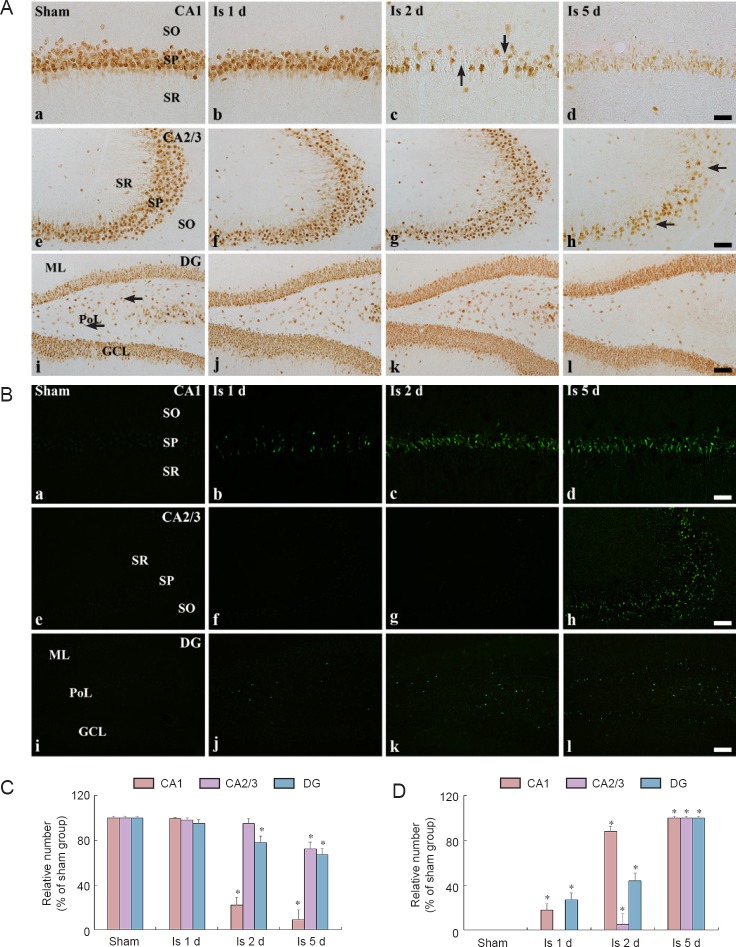
CA1: Pyramidal neurons in the CA1 of animals in the hyperthermia + sham group were distinctively immuno-stained with NeuN (Figure 1Aa). In the hyperthermia + ischemia group, the distribution pattern of NeuN+ neurons in the pyramidal layer was not significantly changed 1 day after tGCI (Figure 1Ab and 1C); however, at 2 days post-tGCI, most of NeuN+ neurons disappeared in the pyramidal layer (Figure 1Ac and 1C). Five days after tGCI, a few NeuN+ neurons were shown in the pyramidal layer, and they were shrunken in comparison to those in the hyperthermia + sham group (Figure 1Ad and 1C).
Figure 1.
Immunohistochemistry for NeuN (A) and F-J B (B) in the hippocampal subregions at sham (a, e, i), 1 (b, f, j), 2 (c, g, k) and 5 days (d, h, l) after tGCI.
(A) NeuN+ neurons were decreased in the pyramidal layer from 2 days post-tGCI (arrows) in the CA1. In the CA2/3, NeuN+ neurons were reduced in the pyramidal layer at 5 days post-tGCI (arrows). In the dentate gyrus (DG), NeuN+ neurons were decreased in the polymorphic layer (PoL) at 5 days post-tGCI (arrows). (B) In the CA1, F-J B+ cells were detected in the pyramidal layer (PL) from 1 day post-tGCI. In the CA2/3, F-J B+ cells were shown in the PL only at 5 days post-tGCI. In the dentate gyrus (DG), F-J B+ cells were found in the PoL from 1 day post-tGCI. Scale bars: 50 μm in a–d and 20 μm in e–l. Quantification of NeuN+ (C) and F-J B+ (D) cells. Data are expressed as the mean ± SEM (*P < 0.05, vs. the hyperthermia + sham group, n = 7; one-way analysis of variance (ANOVA) and Tukey multiple range post hoc test). tGCI: Transient global cerebral ischemia; GCL: Granule cell layer; ML: molecular layer; OL: oriens layer; RL: radiant layer; Is; ischemia; Sham group: hyperthermia + sham group.
CA2/3: Pyramidal neurons in the CA2/3 of the hyperthermia + sham group were also well stained by NeuN (Figure 1Ae). Pyramidal NeuN+ neurons in the hyperthermia + ischemia group were not different in morphology from those of the hyperthermia + sham group until 2 days post-tGCI (Figure 1Af, 1Ag and 1C). Five days after tGCI, NeuN+ neurons in the pyramidal layer were intensely decreased in comparison to those in the hyperthermia + sham group (Figure 1Ah and 1C).
Dentate gyrus: In the hyperthermia + sham group, neurons in the granule cell layer and polymorphic layer were immuno-stained with NeuN (Figure 1Ai). In the hyperthermia + ischemia group, NeuN+ neurons in the granule cell layer was not altered in number and morphology; however, the number of NeuN+ neurons in the polymorphic layer showed a tendency of gradual decrease after tGCI (Figure 1Aj – 1Al and 1C).
F-J B+ cells
CA1: Any F-J B+ cells were not shown in the CA1 of animals in the hyperthermia + sham group (Figure 1Ba). In the hyperthermia + ischemia group, weakly stained F-J B+ cells were observed in the pyramidal layer at 1 day post-tGCI (Figure 1Bb and 1N). Thereafter, many strong F-J B+ cells were detected in the pyramidal layer 2 days post-tGCI (Figure 1Bc, 1Bd and 1D).
CA2/3: No F-J B+ cells were found in the hyperthermia + sham group and hyperthermia + ischemia group until 2 days post-tGCI (Figure 1Be – 1Bg and 1D). However, many F-J B+ cells were easily detected in the pyramidal layer 5 days after tGCI (Figure 1Bh and 1D).
Dentate gyrus: No F-J B+ cells were observed in any layer of the dentate gyrus of animals in the hyperthermia + sham group (Figure 1Bi). In the hyperthermia + ischemia group, some F-J B+ cells were detected in the polymorphic layer at 1 day post-tGCI (Figure 1Bj and 1D), and their number was increased with time in the polymorphic layer from 2 days post-tGCI (Figure 1Bk, 1Bl and 1D).
CB immunoreactivity
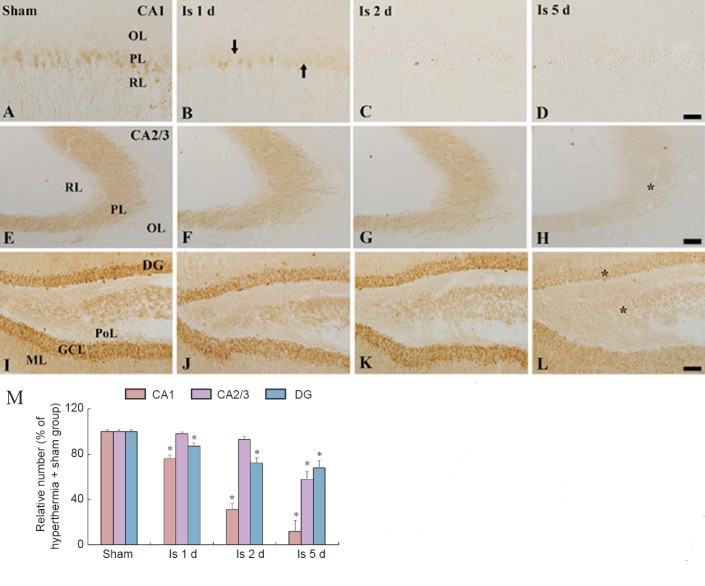
CA1: CB immunoreactivity was found in pyramidale neurons of hippocampal CA1 of animals in the hyperthermia + sham group (Figure 2A). In the hyperthermia + ischemia group, significant decrease in CB immunoreactivity was found in CA1 pyramidal neurons 1 day after tGCI (Figure 2B and 2M). Thereafter, CB immunoreactivity in pyramidal neurons was hardly detected from 2 days post-tGCI (Figure 2C, 2D and 2M).
Figure 2.
Immunohistochemistry for CB in the hippocampal subregions at sham (A, E, I), 1 (B, F, J), 2 (C, G, K) and 5 days (D, H, L) after tGCI.
(A–L) Representative immunohistochemical images of CB staining. CB immunoreactivity (arrows) was decreased in the pyramidal layer (PL) from 1 day post-tGCI in the CA1. In the CA2/3, CB immunoreactivity was significantly decreased in the PL at 5 days post-tGCI (asterisk). In the DG, CB immunoreactivity was significantly decreased in the granule cell layer (GCL) and polymorphic layer (PoL) at 5 days post-tGCI (asterisks). Scale bar: 50 μm in A–D and 20 μm in E –L. (M) Quantification of CB-immunoreactive cells. Data are expressed as the mean ± SEM (*P < 0.05, vs. the hyperthermia + sham group, n = 7; one-way analysis of variance (ANOVA) and Tukey multiple range post hoc test). CB: Calbindin D-28K; tGCI: Transient global cerebral ischemia; ML: molecular layer; OL: oriens layer; RL: radiant layer; DG: dentate gyrus.
CA2/3: CB immunoreactivity was shown in the pyramidal layer of animals in the hyperthermia + sham group (Figure 2E). In the hyperthermia + ischemia group, the pattern of CB immunoreactivity in the pyramidal layer was not significantly altered until 2 days post-tGCI (Figure 2F, 2G and 2M); however, at 5 days post-tGCI, a significant reduction of CB immunoreactivity was found in the pyramidal layer (Figure 2H and 2M).
Dentate gyrus: In the hyperthermia + sham group, CB immunoreactivity was detected in all layers of the dentate gyrus, in particular, CB immunoreactivity in the granule cell layer was strong (Figure 2I). In the hyperthermia + ischemia group, no change in CB immunoreactivity was found in all the layers until 2 days post-tGCI (Figure 2J, 2K and 2M); however, a significant reduction of CB immunoreactivity was found in the granule cell layer at 5 days post-tGCI (Figure 2L and 2M).
Discussion
We, in this study, reported that tGCI-induced neuronal damage in the gerbil hippocampus was more deteriorated by raised body temperature before and during tGCI and that the hyperthermic condition significantly decreased CB immunoreactivity in neurons in the hippocampus following tGCI.
It is well known that ischemia-induced cellular vulnerability differs from each subregion in the hippocampus. The CA1 is the most vulnerable to tGCI; however, the CA2/3 is resistant to tGCI (Schmidt-Kastner and Freund, 1991; Yu et al., 2012). Some researchers have reported that hyperthermia exacerbates neuronal death of pyramidal neurons in the CA1 after ischemia (Dietrich et al., 1990; Kil et al., 1996) and that hyperthermia accelerates DNA fragmentation in pyramidal neurons in the CA1 of the gerbil (Hara et al., 2000). Recently, we evaluated that hyperthermic pre-condition (39.5 ± 0.2°C) distinctively enhanced ischemic neuronal damage in the gerbil hippocampus in comparison with that induced by normothermic pre-condition (37 ± 0.2°C) through increasing astrocytosis and microgliosis (Kim et al., 2015). Thus, we had hypothesized that hyperthermic condition before and during tGCI can increase the death of pyramidal neurons not only in the CA1, but also in the CA2/3. In this regard, we, in this study, applied NeuN immunohistochemistry and F-J B histofluorescence staining, which provides a good data of degenerating neurons, to study neuronal death in hippocampal subregions following tGCI (Schmued and Hopkins, 2000). We found that hyperthermia-mediated tGCI more exacerbated cell death in subregions of the gerbil hippocampus, namely, neuronal death occurred rapidly (1 day after 5-minute tGCI) in the dentate gyrus as well as in the CA1, and neuronal death in the CA2/3, which is much more resistant to tGCI, was shown 5 days post-tGCI. Thus, the level of tGCI-induced pyramidal cell damage/death must be significantly influenced by hyperthermic condition.
Normal body temperature is 37°C in healthy humans and regulated by hypothalamic thermoregulatory center in the brain. However, the thermoregulatory control is sometimes worsened by serious diseases, namely, hyperthermia evokes severe alterations in structure and function, such as the damage of cytoskeletal proteins and change in enzyme activity (Busto et al., 1994; Morimoto et al., 1997). In addition, reactive oxygen species and neurotoxic excitatory neurotransmitters (Globus et al., 1995), Ca2+ influx (Castillo et al., 1999) and vascular permeability (Dietrich et al., 1991) are involved in the mechanisms by which hyperthermia induces tissue injury.
Ischemic damage leads to an increase in calcium through the hyper-activation of ionotropic glutamate receptors, and excessive Ca2+ influx is involved in ischemic neuronal degeneration (Kristian and Siesjo, 1998) via the activation of biochemical processes such as enzymatic breakdowns of proteins, lipids and nucleic acids, mitochondrial malfunction, and energy failure (Lee et al., 1999; Li et al., 2011). Several studies have demonstrated that limiting intracellular calcium accumulation either by using glutamate receptor antagonists or regulating voltage-gated Ca2+ channels protects against tGCI (Scharfman and Schwartzkroin, 1989; Perez-Pinzon et al., 1997). CB plays a major role in neuroprotective function via buffering intracellular Ca2+, although its exact physiological role is still unclear. In the hippocampus, CB is contained in pyramidal as well as non-pyramidal neurons (Celio, 1990; Greene et al., 2001), and about 10% of GABAergic interneurons in the hippocampus have CB and the CB+ interneurons receive inputs from many neurons, such as serotonergic neurons located in raphe nuclei, which are located in the brainstem (Halasy et al., 1992). In addition, a previous study (Keuker et al., 2003) reported that granule cells in the dentate gyrus contained CB.
A significant disproportion between the high amount of CB mRNA transcript and the low content of CB protein has been shown in neurons within several hours after ischemia (Lowenstein et al., 1994). The early loss of CB immunoreactivity in the rat cornu ammonis after tGCI was reported initially by Rami et al. (1992), who demonstrated a reduction of CB immunostaining in CA1 and CA2 pyramidal neurons, which peaked at 3 days post-tGCI. In addition, CB immunoreactivity disappears completely in CA1 pyramidal neurons 3 days after cardiac arrest in rats (Sadowski et al., 2002). The disappearance of CB immunoreactivity in hippocampal ischemic neurons may implicate a selective block of CB production at the level of either translation or transcription.
In this study, CB immunoreactivity in CA1 pyramidal cells in the hippocampus of animals in the hyperthermia + ischemia group began to be significantly decreased from 2 days, and hardly detected 5 days after tGCI, and a significant reduction of CB immunoreactivity was detected in pyramidal cells of the CA2/3, and in granule cells and polymorphic cells of the dentate gyrus at 5 days post-tGCI. Based on these findings, CB immunoreactivity might be different depending on the types of neurons and their location post-tGCI. In this regard, we previously reported that CB immunoreactivity in CA1 pyramidal neurons of younger gerbils was weaker than that in older ones (Lee et al., 2013) and that younger CA1 pyramidal neurons were much more resistant to tGCI than older ones after the same tGCI (Yan et al., 2012; Seo et al., 2013).
In conclusion, hyperthermia before and during tGCI significantly augmented ischemic neuronal damage/death in the gerbil hippocampus and CB immunoreactivity in damaged neurons reduced significantly and differently depending on the degree of ischemic damage post-tGCI. Therefore, findings from this study suggest that the reduction of CB immunoreactivity in neurons is different according to the type of neurons, which are very different in time of death following tGCI under hyperthermia.
Acknowledgments
The authors would like to thank Mr. Seung Uk Lee for his technical help in this study.
Footnotes
Funding: This study was supported by the Biomedical Technology Development Program of the NRF funded by the Korean Government, MSIP (NRF-2015M3A9B6066835), and by the Bio-Synergy Research Project (NRF-2015M3A9C4076322) of the Ministry of Science, ICT and Future Planning through the National Research Foundation.
Conflicts of interest: None declared.
Research ethics: The procedures for animal handling and care adhered to guidelines that are in compliance with the current international laws and policies (Guide for the Care and Use of Laboratory Animals, The National Academies Press, 8th Ed., 2011). Procedures for animal handling and care were approved by the Institutional Animal Care and Use Committee (IACUC) in Kangwon National University (approval No. KW-160802-1).
Data sharing statement: The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open peer reviewer: Muh-Shi Lin, Taipei City Hospital, Taiwan, China.
Copyedited by Li CH, Song LP, Zhao M
References
- Bae EJ, Chen BH, Shin BN, Cho JH, Kim IH, Park JH, Lee JC, Tae HJ, Choi SY, Kim JD, Lee YL, Won MH, Ahn JH. Comparison of immunoreactivities of calbindin-D28k, calretinin and parvalbumin in the striatum between young, adult and aged mice, rats and gerbils. Neurochem Res. 2015;40:864–872. doi: 10.1007/s11064-015-1537-x. [DOI] [PubMed] [Google Scholar]
- Baimbridge KG, Celio MR, Rogers JH. Calcium-binding proteins in the nervous system. Trends Neurosci. 1992;15:303–308. doi: 10.1016/0166-2236(92)90081-i. [DOI] [PubMed] [Google Scholar]
- Bano D, Nicotera P. Ca2+ signals and neuronal death in brain ischemia. Stroke. 2007;38:674–676. doi: 10.1161/01.STR.0000256294.46009.29. [DOI] [PubMed] [Google Scholar]
- Busto R, Globus MY, Neary JT, Ginsberg MD. Regional alterations of protein kinase C activity following transient cerebral ischemia: effects of intraischemic brain temperature modulation. J Neurochem. 1994;63:1095–1103. doi: 10.1046/j.1471-4159.1994.63031095.x. [DOI] [PubMed] [Google Scholar]
- Castillo J, Davalos A, Noya M. Aggravation of acute ischemic stroke by hyperthermia is related to an excitotoxic mechanism. Cerebrovasc Dis. 1999;9:22–27. doi: 10.1159/000015891. [DOI] [PubMed] [Google Scholar]
- Celio MR. Calbindin D-28k and parvalbumin in the rat nervous system. Neuroscience. 1990;35:375–475. doi: 10.1016/0306-4522(90)90091-h. [DOI] [PubMed] [Google Scholar]
- Chen H, Chopp M, Welch KM. Effect of mild hyperthermia on the ischemic infarct volume after middle cerebral artery occlusion in the rat. Neurology. 1991;41:1133–1135. doi: 10.1212/wnl.41.7.1133. [DOI] [PubMed] [Google Scholar]
- Corbett D, Thornhill J. Temperature modulation (hypothermic and hyperthermic conditions) and its influence on histological and behavioral outcomes following cerebral ischemia. Brain Pathol. 2000;10:145–152. doi: 10.1111/j.1750-3639.2000.tb00251.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietrich WD, Busto R, Valdes I, Loor Y. Effects of normothermic versus mild hyperthermic forebrain ischemia in rats. Stroke. 1990;21:1318–1325. doi: 10.1161/01.str.21.9.1318. [DOI] [PubMed] [Google Scholar]
- Dietrich WD, Halley M, Valdes I, Busto R. Interrelationships between increased vascular permeability and acute neuronal damage following temperature-controlled brain ischemia in rats. Acta Neuropathol. 1991;81:615–625. doi: 10.1007/BF00296371. [DOI] [PubMed] [Google Scholar]
- Globus MY, Busto R, Lin B, Schnippering H, Ginsberg MD. Detection of free radical activity during transient global ischemia and recirculation: effects of intraischemic brain temperature modulation. J Neurochem. 1995;65:1250–1256. doi: 10.1046/j.1471-4159.1995.65031250.x. [DOI] [PubMed] [Google Scholar]
- Greene JR, Kerkhoff JE, Guiver L, Totterdell S. Structural and functional abnormalities of the hippocampal formation in rats with environmentally induced reductions in prepulse inhibition of acoustic startle. Neuroscience. 2001;103:315–323. doi: 10.1016/s0306-4522(00)00560-1. [DOI] [PubMed] [Google Scholar]
- Halasy K, Miettinen R, Szabat E, Freund TF. GABAergic Interneurons are the major postsynaptic targets of median raphe afferents in the rat dentate gyrus. Eur J Neurosci. 1992;4:144–153. doi: 10.1111/j.1460-9568.1992.tb00861.x. [DOI] [PubMed] [Google Scholar]
- Heizmann CW, Braun K. Changes in Ca(2+)-binding proteins in human neurodegenerative disorders. Trends Neurosci. 1992;15:259–264. doi: 10.1016/0166-2236(92)90067-i. [DOI] [PubMed] [Google Scholar]
- Keuker JI, Rochford CD, Witter MP, Fuchs E. A cytoarchitectonic study of the hippocampal formation of the tree shrew (Tupaia belangeri) J Chem Neuroanat. 2003;26:1–15. doi: 10.1016/s0891-0618(03)00030-9. [DOI] [PubMed] [Google Scholar]
- Kil HY, Zhang J, Piantadosi CA. Brain temperature alters hydroxyl radical production during cerebral ischemia/reperfusion in rats. J Cereb Blood Flow Metab. 1996;16:100–106. doi: 10.1097/00004647-199601000-00012. [DOI] [PubMed] [Google Scholar]
- Kim MJ, Cho JH, Park JH, Ahn JH, Tae HJ, Cho GS, Yan BC, Hwang IK, Lee CH, Bae EJ, Won MH, Lee JC. Impact of hyperthermia before and during ischemia-reperfusion on neuronal damage and gliosis in the gerbil hippocampus induced by transient cerebral ischemia. J Neurol Sci. 2015;348:101–110. doi: 10.1016/j.jns.2014.11.015. [DOI] [PubMed] [Google Scholar]
- Kim Y, Busto R, Dietrich WD, Kraydieh S, Ginsberg MD. Delayed postischemic hyperthermia in awake rats worsens the histopathological outcome of transient focal cerebral ischemia. Stroke. 1996;27:2274–2280. doi: 10.1161/01.str.27.12.2274. discussion 2281. [DOI] [PubMed] [Google Scholar]
- Kirino T. Delayed neuronal death in the gerbil hippocampus following ischemia. Brain research. 1982;239:57–69. doi: 10.1016/0006-8993(82)90833-2. [DOI] [PubMed] [Google Scholar]
- Klapstein GJ, Vietla S, Lieberman DN, Gray PA, Airaksinen MS, Thoenen H, Meyer M, Mody I. Calbindin-D28k fails to protect hippocampal neurons against ischemia in spite of its cytoplasmic calcium buffering properties: evidence from calbindin-D28k knockout mice. Neuroscience. 1998;85:361–373. doi: 10.1016/s0306-4522(97)00632-5. [DOI] [PubMed] [Google Scholar]
- Kristian T, Siesjo BK. Calcium in ischemic cell death. Stroke. 1998;29:705–718. doi: 10.1161/01.str.29.3.705. [DOI] [PubMed] [Google Scholar]
- Kumar VS, Gopalakrishnan A, Naziroglu M, Rajanikant GK. Calcium ion--the key player in cerebral ischemia. Curr Med Chem. 2014;21:2065–2075. doi: 10.2174/0929867321666131228204246. [DOI] [PubMed] [Google Scholar]
- Lee JC, Hwang IK, Cho JH, Moon SM, Kang TC, Kim WK, Won MH. Expression and changes of calbindin D-28k immunoreactivity in the ventral horn after transient spinal cord ischemia in rabbits. Neurosci Lett. 2004;369:145–149. doi: 10.1016/j.neulet.2004.07.082. [DOI] [PubMed] [Google Scholar]
- Lee JC, Tae HJ, Kim IH, Cho JH, Lee TK, Park JH, Ahn JH, Choi SY, Bai HC, Shin BN, Cho GS, Kim DW, Kang IJ, Kwon YG, Kim YM, Won MH, Bae EJ. Roles of HIF-1alpha, VEGF, and NF-kappaB in ischemic preconditioning-mediated neuroprotection of hippocampal CA1 pyramidal neurons against a subsequent transient cerebral ischemia. Mol Neurobiol. 2016. doi: https://doi.org/10.1007/s12035-016-0219-2 . [DOI] [PubMed]
- Lee JM, Zipfel GJ, Choi DW. The changing landscape of ischaemic brain injury mechanisms. Nature. 1999;399:A7–14. doi: 10.1038/399a007. [DOI] [PubMed] [Google Scholar]
- Lee YJ, Yan BC, Park JH, Ahn JH, Kim IH, Lee JC, Lee HY, Kim YM, Won MH, Cho JH. Differences of calcium binding proteins immunoreactivities in the young hippocampal CA1 region from the adult following transient ischemic damage. J Neurol Sci. 2013;326:40–47. doi: 10.1016/j.jns.2012.12.026. [DOI] [PubMed] [Google Scholar]
- Li MH, Inoue K, Si HF, Xiong ZG. Calcium-permeable ion channels involved in glutamate receptor-independent ischemic brain injury. Acta Pharmacol Sin. 2011;32:734–740. doi: 10.1038/aps.2011.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattson MP, Rychlik B, Chu C, Christakos S. Evidence for calcium-reducing and excito-protective roles for the calcium-binding protein calbindin-D28k in cultured hippocampal neurons. Neuron. 1991;6:41–51. doi: 10.1016/0896-6273(91)90120-o. [DOI] [PubMed] [Google Scholar]
- Minamisawa H, Smith ML, Siesjo BK. The effect of mild hyperthermia and hypothermia on brain damage following 5, 10, and 15 minutes of forebrain ischemia. Ann Neurol. 1990;28:26–33. doi: 10.1002/ana.410280107. [DOI] [PubMed] [Google Scholar]
- Morimoto T, Ginsberg MD, Dietrich WD, Zhao W. Hyperthermia enhances spectrin breakdown in transient focal cerebral ischemia. Brain Res. 1997;746:43–51. doi: 10.1016/s0006-8993(96)01154-7. [DOI] [PubMed] [Google Scholar]
- Perez-Pinzon MA, Yenari MA, Sun GH, Kunis DM, Steinberg GK. SNX-111, a novel, presynaptic N-type calcium channel antagonist, is neuroprotective against focal cerebral ischemia in rabbits. J Neurol Sci. 1997;153:25–31. doi: 10.1016/s0022-510x(97)00196-2. [DOI] [PubMed] [Google Scholar]
- Pulsinelli WA, Brierley JB, Plum F. Temporal profile of neuronal damage in a model of transient forebrain ischemia. Ann Neurol. 1982;11:491–498. doi: 10.1002/ana.410110509. [DOI] [PubMed] [Google Scholar]
- Rami A, Rabie A, Thomasset M, Krieglstein J. Calbindin-D28K and ischemic damage of pyramidal cells in rat hippocampus. J Neurosci Res. 1992;31:89–95. doi: 10.1002/jnr.490310113. [DOI] [PubMed] [Google Scholar]
- Sadowski M, Lazarewicz JW, Jakubowska-Sadowska K, Wisniewski HM, Mossakowski MJ, Brown WT. Long-term changes in calbindin D(28K) immunoreactivity in the rat hippocampus after cardiac arrest. Neurosci Lett. 2002;321:90–94. doi: 10.1016/s0304-3940(01)02426-0. [DOI] [PubMed] [Google Scholar]
- Scharfman HE, Schwartzkroin PA. Protection of dentate hilar cells from prolonged stimulation by intracellular calcium chelation. Science. 1989;246:257–260. doi: 10.1126/science.2508225. [DOI] [PubMed] [Google Scholar]
- Schmidt-Kastner R, Freund TF. Selective vulnerability of the hippocampus in brain ischemia. Neuroscience. 1991;40:599–636. doi: 10.1016/0306-4522(91)90001-5. [DOI] [PubMed] [Google Scholar]
- Schmued LC, Hopkins KJ. Fluoro-Jade B: a high affinity fluorescent marker for the localization of neuronal degeneration. Brain Res. 2000;874:123–130. doi: 10.1016/s0006-8993(00)02513-0. [DOI] [PubMed] [Google Scholar]
- Seo JY, Yan BC, Park JH, Ahn JH, Kim IH, Lee JC, Kwon YG, Kim YM, Cho JH, Won MH. Comparison of the immunoreactivities of NMDA receptors between the young and adult hippocampal CA1 region induced by experimentally transient cerebral ischemia. J Neurol Sci. 2013;325:108–114. doi: 10.1016/j.jns.2012.12.012. [DOI] [PubMed] [Google Scholar]
- Seo WK, Yu SW, Kim JH, Park KW, Koh SB. The impact of hyperthermia and infection on acute ischemic stroke patients in the intensive care unit. Neurocrit Care. 2008;9:183–188. doi: 10.1007/s12028-008-9056-0. [DOI] [PubMed] [Google Scholar]
- Tortosa A, Ferrer I. Poor correlation between delayed neuronal death induced by transient forebrain ischemia, and immunoreactivity for parvalbumin and calbindin D-28k in developing gerbil hippocampus. Acta Neuropathol. 1994;88:67–74. doi: 10.1007/BF00294361. [DOI] [PubMed] [Google Scholar]
- Wang Y, Lim LL, Levi C, Heller RF, Fisher J. Influence of admission body temperature on stroke mortality. Stroke. 2000;31:404–409. doi: 10.1161/01.str.31.2.404. [DOI] [PubMed] [Google Scholar]
- Yan BC, Park JH, Kim SK, Choi JH, Lee CH, Yoo KY, Kwon YG, Kim YM, Kim JD, Won MH. Comparison of trophic factors changes in the hippocampal CA1 region between the young and adult gerbil induced by transient cerebral ischemia. Cell Mol Neurobiol. 2012;32:1231–1242. doi: 10.1007/s10571-012-9848-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu DK, Yoo KY, Shin BN, Kim IH, Park JH, Lee CH, Choi JH, Cho YJ, Kang IJ, Kim YM, Won MH. Neuronal damage in hippocampal subregions induced by various durations of transient cerebral ischemia in gerbils using Fluoro-Jade B histofluorescence. Brain Res. 2012;1437:50–57. doi: 10.1016/j.brainres.2011.12.029. [DOI] [PubMed] [Google Scholar]