Abstract
Congenital hepatic fibrosis (CHF) is a rare, autosomal recessive disorder, clinically characterized by hepatic fibrosis and portal hypertension. CHF results from ductal plate malformation (DPM) of the intrahepatic bile ducts. Four clinical forms can be observed: portal hypertensive, cholangitic, mixed and latent. CHF is one of the “fibropolycystic diseases” which also include several conditions with a variety of intrahepatic bile duct dilatation and associated periportal fibrosis such as Caroli disease, autosomal recessive and dominant polycystic kidney disease (ARPKD or ADPKD), Ivemark, Jeune, Joubert, Bardet-Biedl, Meckel-Gruber and Arima syndromes. Most of them are accompanied by progressive cystic degeneration of the kidneys. We present the case of a 9-year-old female patient with CHF with nonspecific clinical manifestation and a review of the literature.
Keywords: congenital hepatic fibrosis, portal hypertension, ductal plate malformation, esophageal varices
Introduction
Congenital hepatic fibrosis (CHF) is an autosomal recessive disorder which was described by Dobbs in 1960 and later elaborated by Kerr et al. [1–3]. CHF results from a ductal plate malformation (DPM) of the intrahepatic bile ducts. Arrest of maturation of the ductal plate – the embryonic precursor of the intrahepatic bile ducts – stimulates the formation of portal fibrous tissue.
Due to the variable clinical description it is believed that CHF is not a single clinical entity but may have a broad spectrum of either hepatic or hepatic and renal lesions [4, 5]. Clinically in most patients it is characterized by hepatic fibrosis and portal hypertension (portal hypertensive), but in some patients cholangitic, mixed and latent forms are observed.
It is a rare disease, and up to 1988, only 200 patients had been reported in the literature. However, due to the development of visual, noninvasive diagnosis such as ultrasound it may now be detected more often [6, 7].
In most patients, the first symptoms, such as hepato- and/or splenomegaly, esophageal varices and gastrointestinal bleeding, occur in adolescence or young adulthood but may occur in early childhood and in the 5th or 6th decade of life [8]. In younger children CHF is often accompanied by renal cysts or increased renal echogenicity, while predominant hepatic manifestation is observed later [5].
We present the case of a 9-year-old female patient with CHF, with nonspecific clinical manifestation, which made it very difficult to diagnose this disease.
Case description
A previously healthy 9-year-old girl was referred to the hospital by her pediatrician with an asymptomatic splenomegaly which was revealed in a physical examination (4 cm below the left costal margin). The enlarged spleen was confirmed by abdominal ultrasonography (65 mm × 155 mm). The patient was referred to the Hematology-Oncology Ward to determine the cause of the splenomegaly. Laboratory tests showed leucopenia (WBC 2.8 G/l), low platelets (80 G/l) and normal liver function, without elevated cholestasis markers. Hepatotropic virus infection, cytomegalovirus, Epstein-Barr virus, and thrombophilia were excluded. Computed tomography (CT) imaging showed spleen enlargement (150 mm × 100 mm), normal liver size and also the presence of portosystemic collateral vessels along the lesser curvature of the stomach, cardiac region, body of the pancreas, in the porta hepatis area and in the splenic hilum.
The next diagnostic stage was performed in the reference center of a pediatric hepatology. The differential diagnosis excluded Wilson’s disease and α-1-antitrypsin deficiency. Gastroscopy visualized a low-grade esophageal varices (with trophic changes) located in the lower third and features of portal hypertensive gastropathy. There were no indications to perform endoscopic variceal ligation (EVL). The ultrasonography and CT scan excluded prehepatic flow block. There were no lesions in the kidneys, confirmed in imaging tests.
The endoscopic studies were repeated 6 months later. There was no progression of esophageal varices. Laboratory tests again revealed features of hypersplenism and confirmed normal liver function. The patient was qualified for a percutaneous liver biopsy.
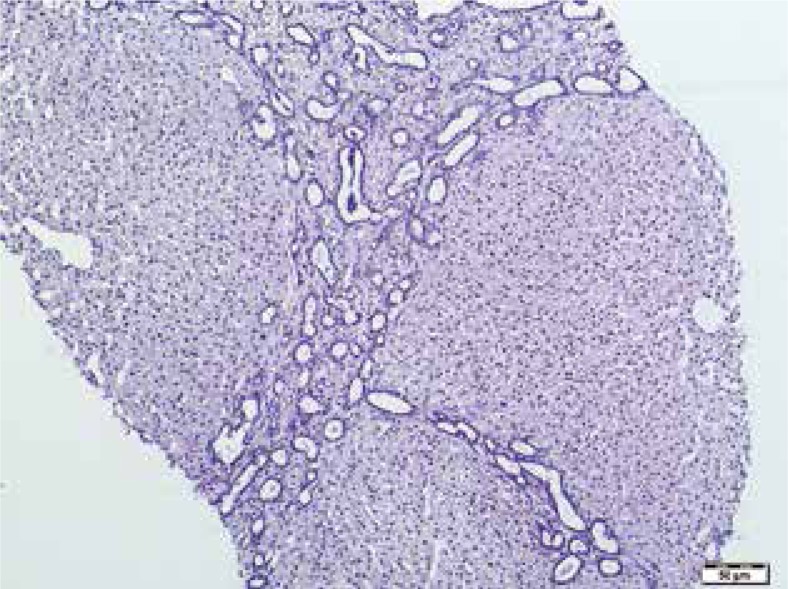
A histopathological examination of the liver biopsy showed portal and periportal fibrosis with the presence of fibrous bands between the portal tracts without signs of cirrhosis (Fig. 1). The blood vessels, especially the terminal hepatic veins, were incorporated into the fibrous tissue. Fusiform dilatation with mild proliferation of the intrahepatic bile ducts was observed in the portal tracts. Some of these irregularly shaped and rounded proliferating bile ducts were lined with cuboidal epithelium. Inflammatory infiltrates were absent. A microscopic examination revealed an early phase of hepatoportal sclerosis.
Fig. 1.
Periportal fibrosis and sclerosis, proliferation of bile ducts lined by cuboidal epithelial cells. Two central veins remain intact, without signs of central fibrosis. H&E, 200x
The clinical picture, liver function tests and histopathological results allowed us to diagnose congenital hepatic fibrosis. Currently, the patient is 14 years old and generally in good health. She requires systematic endoscopic monitoring of the portal hypertension progress and prevention of varices bleeding. Her synthetic liver function results such as INR and albumin are normal, as is her transaminases activity.
Discussion
Polycystic liver disease was first describe by Bristowe in 1856 [9]. The broad term “fibropolycystic diseases” includes several conditions, with a variety of intrahepatic bile duct dilatation and associated periportal fibrosis such as Caroli disease, autosomal dominant polycystic kidney disease (ADPKD) and autosomal recessive polycystic kidney disease (ARPKD).
Classically, CHF is associated with ARPKD, and some authors believe that CHF and ARPKD represent a single disorder, with a wide spectrum of manifestations. Others argue that there are two distinct disorders with similar hepatic and biliary lesions [10, 11].
CHF is also observed in other syndromes such as Meckel-Gruber, Ivemark, Jeune, Joubert, Bardet-Biedl and Arima syndromes (Table 1).
Table 1.
Syndromes with associated congenital fibrosis
| Disorder | Clinical features |
|---|---|
| Ivemark syndrome | Asplenia, heart malformations, abnormal lung lobation, localized renal dysplasia |
| Jeune syndrome | Small, narrow chest, shortened bones of the arms and legs, extra fingers and/or toes, renal dysfunction |
| Joubert syndrome | Cerebellar vermis hypoplasia, retinitis pigmentosa, ataxia |
| Bardet-Biedl syndrome | Retinitis pigmentosa, polydactyly, mental retardation, hypogonadism, renal dysfunction |
| Meckel-Gruber syndrome | Renal cystic disease, microcephaly, hypoplastic genitalia, congenital heart disease, polydactyly |
| Arima syndrome | Cerebellar vermis hypoplasia, renal abnormalities, psychomotor retardation |
Laboratory evaluation in portal hypertensive clinical form is usually unremarkable, with serum aminotransferase and bilirubin normal value and signs of hypersplenism, such as thrombocytopenia and neutropenia.
Wu et al. observed 60 children with CHF; 43% of them presented with portal hypertension form (PF CHF), 5% with cholangitic form, 50% with combined portal hypertensive and cholangitic form, and the remaining 2% a latent form. In their study, they confirmed that the plasma prothrombin time, serum levels of alanine and aspartate transaminase and gammaglutamyltransferase in children with mixed CHF were higher than in those with PH CHF (p < 0.05) [12]. In our patient with PH CHF, the liver function tests were normal.
Rawat et al. presented a group of 40 patients with CHF and Caroli syndrome treated in Birmingham Children’s Hospital, between 1990 and 2009 [5]. The majority (37 from 40) had associated renal disease, whereas only 3 children with isolated CHF had no renal involvement ,with normal renal ultrasound. The most common findings on ultrasound of the liver included coarse liver echotexture with splenomegaly (100%), intrahepatic (52%) and extrahepatic (33%) biliary dilatation, intraabdominal or splenic collaterals (52%), liver cysts (25%) and spontaneous splenorenal shunt (20%).
Shorbagi and Bayraktar reported 26 patients with CHF observed over a period of 35 years, between 1974 and 2009. Most of them were diagnosed after the year 2000 [13]. The most common symptom was abdominal distension, due to hepatosplenomegaly (42.3%), a history of recurrent cholangitis (23%) and only in the minority (two patients – 7.7%) portal hypertension with bleeding from varices. In 31% of their patients, CHF was associated with Caroli disease. It is now believed that in CHF there is an arrest of small interlobular bile ducts maturation, while in Caroli it is the medium intrahepatic bile ducts which are defective. If both medium and small bile ducts are involved, the result is what is known as Caroli syndrome. Clinically it is very difficult to distinguish between the cholangitic type of CHF and Caroli disease. An unequivocal diagnosis of CHF can only be made by an examination of a liver biopsy. A liver biopsy usually confirms the diagnosis and distinguishes between portal hypertensive, cholangitic and mixed hypertensive-cholangitic type [14]. Characteristic fusiform pattern of bile duct transformation indicates ductal plate malformation. The lack of central vein fibrosis is a good prognostic factor, despite the irregular shape of hepatic lobules. A liver biopsy allows for the exclusion of cirrhotic changes and the confirmation of hepatic fibrosis with signs of hepatoportal sclerosis. Unfortunately, in the eyes of an inexperienced pathologist, histopathological findings in CHF may be mistaken for cirrhosis [13].
Until now, there has been no treatment to stop or reverse the process of congenital hepatic fibrosis. Several anti-fibrotic drugs such as colchicine, interferon gamma, angiotensin II receptor blockers, pirfenidone, and ursodeoxycholic acid were evaluated in clinical trials, without marked benefit. Symptomatic therapy depends on the type of CHF. In portal hypertensive form, it is associated with the management of varices and bleeding. Endoscopic treatment, previously with sclerotherapy and now EVL, is used either for acute bleeding or for primary and secondary prophylactic. Most patients, as was described in our case, require systematic endoscopic monitoring of the portal hypertension progression and prevention of varices bleeding. Some patients may benefit from the use of beta blockers [15]. In some children portosystemic shunts may be necessary if there is a case of repeated bleeding. Fortunately, the incidence of hepatic encephalopathy in patients with CHF after shunting procedures is quite low.
In cholangitic and mixed clinical cases, antibiotics may be required.
Liver transplantation should be limited only to cases with progressive liver dysfunction. In Caroli syndrome repeated, severe cholangitis is also an indication for transplantation. In children with coexisting end-stage renal failure, as a result of polycystic kidney disease, combined liver and kidney transplantation should be considered [5, 16]. Rawat et al. showed that early (neonatal) presentation was the best predictor for the need for a transplant [5].
In general, isolated CHF is a disorder which is characterized by well-preserved liver function and a rather good prognosis, when complications such as portal hypertension and variceal bleeding or cholangitis are controlled. But still there is variability in the severity and progression of clinical manifestations, making it difficult to prognose an outcome.
It is much easier to make a diagnosis of CHF in the presence of other organ involvement such as is seen in ARPKD and several other mentioned syndromes. Isolated portal hypertension form makes the diagnosis more difficult.
Conclusions
Congenital hepatic fibrosis (CHF) is a rare, autosomal recessive disorder, clinically characterized by hepatic fibrosis and portal hypertension.
Laboratory evaluation in portal hypertensive clinical form is usually unremarkable with serum aminotransferase and bilirubin normal and signs of hypersplenism such as thrombocytopenia and neutropenia.
A liver biopsy usually confirms the diagnosis and may distinguish between portal hypertensive, cholangitic and mixed hypertensive-cholangitic type.
In general, CHF is a disorder which is characterized by well-preserved liver function with a rather good prognosis, when complications such as portal hypertension and variceal bleeding or cholangitis are controlled. However, there is variability in the severity and progression of clinical manifestations, making it difficult to prognose the outcome.
Disclosure
Authors report no conflict of interest.
References
- 1.Dobbs RH. Congenital hepatic fibrosis with portal hypertension. Proc R Soc Med. 1960;53:327–328. [PubMed] [Google Scholar]
- 2.Kerr DN, Harrison CV, Sherloc S, et al. Congental hepatic fibrosis. Q J Med. 1961;30:91–117. [PubMed] [Google Scholar]
- 3.Kerr DN, Okonkwo S, Choa RG. Congenital hepatic fibrosis: the long-term prognosis. Gut. 1978;19:514–520. doi: 10.1136/gut.19.6.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murray-Lyon IM, Ockenden BG, Williams R. Congenital hepatic fibrosis: is it a single clinical entity? Gastroenterology. 1973;64:653–656. [PubMed] [Google Scholar]
- 5.Rawat D, Kelly DA, Milford DV, et al. Phenotypic variation and long-term outcome in children with congenital hepatic fibrosis. J Pediatr Gastroenterol Nutr. 2013;57:161–166. doi: 10.1097/MPG.0b013e318291e72b. [DOI] [PubMed] [Google Scholar]
- 6.De Vos M, Barbier F, Cuvelier C. Congenital hepatic fibrosis. J Hepatol. 1988;6:91–117. doi: 10.1016/s0168-8278(88)80036-9. [DOI] [PubMed] [Google Scholar]
- 7.Gunay-Aygun M, Font-Montgomery E, Lukose L, et al. Characteristics of congenital hepatic fibrosis in a large cohort of patients with autosomal recessive polycystic kidney disease. Gastroenterology. 2013;144:112–121. doi: 10.1053/j.gastro.2012.09.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mainguene C, Clement N, Cassagnau E, et al. Congenital hepatic fibrosis. Five cases with late occurrence in adults. Ann Pathol. 1998;18:125–129. [PubMed] [Google Scholar]
- 9.Bristowe F. Cystic disease of the liver associated with similar disease of the kidneys. Tr Path Soc London. 1856;7:229–234. [Google Scholar]
- 10.D’Agata IDA, Johnas MM, Perez-Atayde AR, et al. Combined cystic disease of the liver and kidney. Seminars Liver Disease. 1994;14:215–228. doi: 10.1055/s-2007-1007313. [DOI] [PubMed] [Google Scholar]
- 11.Yönem O, Ozkayar N, Balkanci F, et al. Is congenital hepatic fibrosis a pure liver disease? Am J Gastroenterol. 2006;101:1253–1259. doi: 10.1111/j.1572-0241.2006.00642.x. [DOI] [PubMed] [Google Scholar]
- 12.Wu X, DU XR, Ding JF, et al. Clinical features of different clinical forms of childhood congenital hepatic fibrosis. Zhongguo Dang Dai Er Ke Za Zhi. 2016;18:335–339. doi: 10.7499/j.issn.1008-8830.2016.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shorbagi A, Bayraktar Y. Experience of a single center with congenital hepatic fibrosis: A review of the literature. World J Gastroenterol. 2010;16:683–690. doi: 10.3748/wjg.v16.i6.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giouleme O, Nikolaidis N, Tziomalos K, et al. Ductal plate malformation and congenital hepatic fibrosis Clinical and histological findings in four patients. Hepatol Res. 2006;35:147–150. doi: 10.1016/j.hepres.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 15.Mazigh MS, Aloui N, Fetni I, et al. Congential hepatic fibrosis in children. Report of 9 cases and review of the literature. Tunis Med. 2006;84:182–188. [PubMed] [Google Scholar]
- 16.Luoto TT, Pakarinen MP, Jahnukainen T, et al. Liver disease in autosomal recessive polycystic kidney disease: clinical characteristics and management in relation to renal failure. J Pediatr Gastroenterol Nutr. 2014;59:190–196. doi: 10.1097/MPG.0000000000000422. [DOI] [PubMed] [Google Scholar]