Abstract
Thoracic endovascular aortic repair (TEVAR) effectively improved the results of thoracic aortic aneurysm treatment. TEVAR is a less invasive procedure that can be performed under local anesthesia with shorter hospital stay. The perioperative morbidity and mortality rates are lower for endovascular than open repair, but the rate of secondary interventions is higher for TEVAR. We report a case of an elderly man with synchronous abdominal and thoracic aortic aneurysms. A type III dangerous endoleak was recognized 3 years after TEVAR. It was successfully repaired during an endovascular procedure. There were no new endoleaks after 12 months of follow-up. TEVAR may be the only option of treatment for risky and elderly patients. However, postoperative monitoring is necessary to exclude different types of endoleaks. Most of them undergo effective endovascular repair.
Keywords: endoleak, thoracic aneurysm, endovascular aneurysm repair
Introduction
Thoracic aortic aneurysms (TAA), although not so frequent as abdominal, are observed with an incidence of 5.9 to 10.4 cases per 100,000 person-years. Among all TAA those of the ascending aorta are the most common (40%). Aortic arch aneurysms account for 15% of TAA, descending thoracic aorta for 35%, and thoracoabdominal aortic aneurysms for 10% [1]. In contrast to abdominal aortic aneurysms (AAA), which are more frequent in men (6 : 1), TAA are observed similarly often in men and women (1.7 : 1). The incidence of TAA is still growing due to better available diagnostic methods and the increasing ageing population of developed countries. Most patients with aortic aneurysms are asymptomatic and diagnosis is made following abdominal ultrasonography, chest X-ray or echocardiography. The mean age of TAA occurrence is 65 years. The main risk factors of aneurysm rupture are aortic diameter, concomitance of chronic obstructive pulmonary disease, old age and uncharacteristic continued chest pain [2]. Simultaneous occurrence of TAA and AAA may affect up to 25% of patients and is more often observed in the elderly (more than 76 years old) and women [3, 4]. Open surgery was for many years the only option of TAA treatment, with a high risk of paraplegia and mortality ranging from 5% (in the best centers) to 22% [1, 2]. Implementation of thoracic endovascular aortic repair (TEVAR) in recent years improved the results of TAA treatment. Similar experience was observed in AAA [5, 6]. The first implantation of a stainless steel stent-graft covered with woven Dacron was performed by Dake in 1994 [7]. During the last years TEVAR became the gold standard in treatment of aneurysms, dissections and posttraumatic rupture in descending thoracic aorta. Endovascular repair lowered the mortality and postoperative morbidity (paraplegia, respiratory and circulation insufficiency, renal failure). TEVAR is generally a less invasive procedure possible to perform in local anesthesia, associated with shorter hospital stay [5, 8, 9]. However, there are no randomized, prospective trials comparing endovascular and open TAA repair. The results of industry-sponsored trials are currently published. They confirm the perioperative lower mortality and morbidity rate for elective endovascular procedures. The late results are similar for open and endovascular groups [10, 11]. The authors of trials observed higher rates of secondary intervention in TEVAR. Those patients should have regular computed tomography (CT) imaging to detect endoleaks, sac enlargement, stent migration, stent rupture or component separation [8].
Case report
We report the case of an 88-year old man with coexistence of descending TAA and AAA. The patient had a long medical history of arterial hypertension, coronary disease and chronic obstructive pulmonary disease (COPD). He smoked about 20 cigarettes a day until 65 years old. At the age of 72 (in 2001) the patient had coronary artery bypass surgery. During coronary angiography in 2009 two drug-eluting stents were implanted in the anterior descending branch and right coronary artery. At the same time two aortic aneurysms were recognized (descending TAA with diameter 50 mm and AAA with diameter 42 mm) and kept under closed observation. In November 2012 when our patient was 84 years old the endovascular repair of abdominal aortic (54 mm) and left iliac common artery (25 mm) aneurysms with the implantation of a bifurcated Gore Excluder stent graft was performed. Preoperative echocardiography revealed akinesia of the inferior wall basal segment and lateral wall middle segment, with left ventricular ejection fraction (EF) = 47%. The essential aberrance in the preoperative laboratory test was thrombocytopenia with platelet level 96 000/ml. However, the endovascular aortic repair was successful and the patient was discharged on the fifth postoperative day. During subsequent hospitalization in January 2013 the TEVAR procedure of a 58 mm × 70 mm descending, angulated TAA aneurysm was performed. Two segments of Zenith TX2 TAA endovascular graft 40 mm in diameter were introduced through the right femoral approach. The proximal segment, 162 mm long, started just below the left subclavian artery. The distal segment, 198 mm long, overlapped partially the proximal one and finished over the diaphragm where the aorta ran at a right angle to the spine. There were no perioperative complications and the patient was discharged on the sixth day after TEVAR.
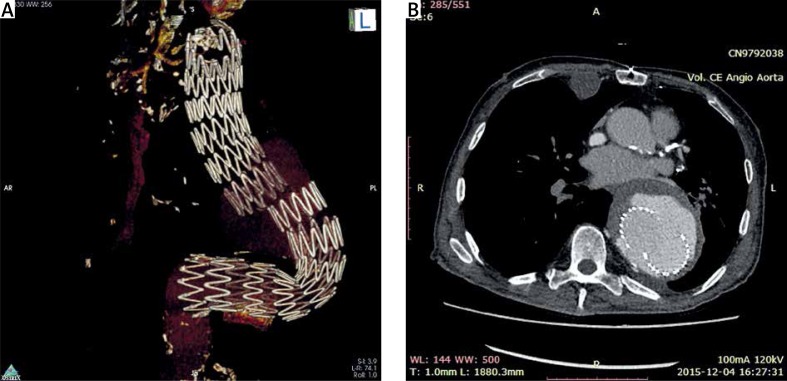
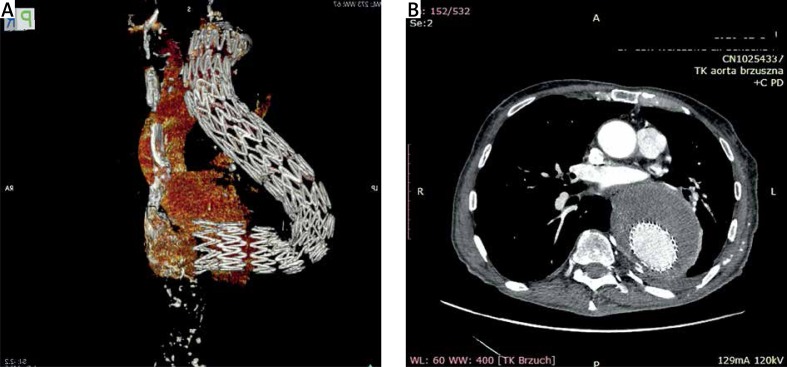
In 2013 and 2014 control spiral CT scan confirmed complete exclusion of the aneurysm sac. The next examination performed in December 2015 revealed excessive type III endoleak due to disconnection of proximal and distal stent graft segments in the descending TAA. The distal part moved in a lateral and dorsal direction (Photo 1). Maximal aneurysmal sac diameter was 88 mm (baseline 58 mm × 70 mm). There were no endoleaks or sac enlargement after endovascular aneurysm repair (EVAR) of the abdominal aorta. The patient was qualified for endovascular treatment of type III endoleak due to high risk of aneurysmal sac rupture. After initial angiography through the left femoral access disconnection of Zenith TX2 segments was confirmed. The attempt to introduce a stent graft over the stiff guidewire through the left groin was unsuccessful due to extreme angulation of the descending TAA. We decided to use brachial access, and a hydrophilic guidewire was inserted through the left brachial artery to the femoral artery. The tight guidewire between the left brachial and left femoral artery made it possible – despite the difficulties due to severe descending thoracic aorta angulation – to deliver the low profile Cook Zenith Alpha graft (diameter 42 mm, length 225 mm). The inserted segment successfully sealed the separated thoracic graft (Photo 2).
Photo 1.
Type III endoleak due to disconnection of thoracic stent graft segments
Photo 2.
Computed tomography scan – complete exclusion of type III endoleak after implantation of additional thoracic stent graft segment (6 months follow-up)
Instead of accurate hemostasis increased bleeding to the left groin and arm drains was observed during the first postoperative hours. Finally a pressure dressings to the both places of access stopped bleeding. The patient was discharged in good general condition on sixth postoperative day. There were no endoleaks detected during monitoring CT scan of the chest and abdomen at 3, 6 and 12 months follow up.
Discussion
Synchronous appearance of AAA and TAA is not rare and possibly affects up to 25% of patients with AAA. Routine screening with a chest CT scan in patients qualified for AAA repair should be recommended. It is especially indicated in geriatric age patients and women [3, 4, 12]. The currently observed ever increasing ageing population of developed countries is related to more frequent diagnosis of TAA in elderly patients with many intercurrent risk factors which disqualify them from surgical repair. Endovascular treatment of aneurysms, dissections and descending thoracic aorta trauma seems to be a safe method with lower morbidity and mortality than open surgery [5, 10, 13]. TEVAR has become the method of choice in the treatment of descending TAA and is increasingly used in many vascular centers. It can be the only management for risky and elderly patients which protects them against aneurysmal rupture [5, 14]. Currently we have industry-sponsored randomized trials comparing various stent-graft devices with a control group after open repair. A study with the Gore TAG device revealed that perioperative mortality was 1.5% in the TEVAR group compared to 12% for patients after open repair [15]. In the Valor study monitoring the Talent device, the perioperative mortality rate was 2% in TEVAR and 8% for the open repair group. Perioperative morbidity, especially spinal cord ischemia, occurred 2 times less often in the TEVAR group [5, 16]. The first reports about long-term (5 years) results of both methods show no major differences. Better perioperative results of TEVAR became similar in longer observation. The 5-year survival rate in the Gore TAG study for endovascular and open repair group was respectively 68% and 67%, whereas in the Zenith TX2 study the mortality rate after 5 years was 63% for both groups [17, 18]. A higher rate of aneurysm-related reinterventions during follow-up after endovascular treatment was observed [19, 20]. Their main causes are endoleaks, most often type I, associated with too short aneurysmal neck in relation to guidelines. Their repair requires proximal (less frequently distal) extension implantation, which carries the risk of left subclavian artery coverage. Sometimes it is necessary to extend the landing zone in the aortic arch. The most common procedures are extra-anatomic carotid-carotid bypass and ascending aorta to innominate artery and left common carotid artery bypass. In the case of persistent type I endoleak after secondary endovascular interventions conversion to open surgical repair may be necessary [21]. Type III endoleaks result from stent graft fabric damage, migration of distal or proximal segments and sometimes a leak between them. They are observed in about 2% of new generation devices [22]. There were no type III endoleak in the Zenith TX2 study and only one observed in Gore TAG [10, 11]. Most reinterventions in type III endoleak can be repaired with an endovascular approach [23].
Conclusions
Endovascular therapy is a safe and miniinvasive method of the treatment of descending TAA whose anatomy is suitable for graft implantation. TEVAR may be, as in the present case, the only one option in the management of elderly patients with important concomitant risk factors. Postoperative periodic monitoring (computed tomographic angiography or magnetic resonance angiography) is necessary to check for endoleak and aneurysmal sac enlargement. Type III endoleaks are rare (not exceeding 2% of new generation devices) and may undergo effective endovascular repair.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Singh MJ, Makaroun MS. Thoracic and thoracoabdominal aneurysms: endovascular treatment. In: Cronenwett JL, Johnston KW, editors. Rutherford’s Vascular Surgery. Philadelphia: Elsevier Saunders; 2014. pp. 2126–48. [Google Scholar]
- 2.Gilbert R, Upchurch JR. Thoracic and thoracoabdominal aortic aneurysms: evaluation and decision making. In: Cronenwett JL, Johnston KW, editors. Thoracic and thoracoabdominal aneurysms: endovascular treatment. In: Rutherford’s Vascular Surgery. Philadelphia: Elsevier Saunders; 2014. pp. 2084–101. [Google Scholar]
- 3.Larson E, Vishnevskaya L, Kalin B, et al. High frequency of thoracic aneurysms in patients with abdominal aortic aneurysms. Ann Surg. 2011;253:180–4. doi: 10.1097/SLA.0b013e3181d96498. [DOI] [PubMed] [Google Scholar]
- 4.Hultgren R, Larsson E, Wahlgrn CM, Swedenborg J. Female and elderly abdominal aortic aneurysm patients more commonly have concurrent thoracic aortic aneurysm. Ann Vasc Surg. 2012;26:918–23. doi: 10.1016/j.avsg.2012.01.023. [DOI] [PubMed] [Google Scholar]
- 5.Kilie A, Shah A, Black J, et al. Trends in repair of intact and ruptured descending thoracic aortic aneurysms in the United States: a population-based analysis. J Thorac Cardiovasc Surg. 2014;147:1855–60. doi: 10.1016/j.jtcvs.2013.06.032. [DOI] [PubMed] [Google Scholar]
- 6.Synowiec T, Warot M, Burchardt P, Chęciński P. All dangerous types of endoleaks after endovascular aneurysm repair in a single patient. Videosurgery Miniinv. 2015;10:290–4. doi: 10.5114/wiitm.2015.52600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dake MD, Miller DC, Semba CP, et al. Transluminal placement of endovascular stent-grafts for the treatment of descending thoracic aortic aneurysms. N Engl J Med. 1994;331:1729–34. doi: 10.1056/NEJM199412293312601. [DOI] [PubMed] [Google Scholar]
- 8.Wachal K, Szmyt K, Oszkinis G, et al. Diagnosis and treatment of patient with type IV endoleak as a late complication after endovascular aneurysm repair. Videosurgery Miniinv. 2014;9:667–70. doi: 10.5114/wiitm.2014.47264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheng D, Martin J, Shennib H, et al. Endovascular aortic repair versus open surgical repair for descending thoracic aortic disease a systematic review and meta-analysis of comparative studies. J Am Coll Cardiol. 2010;55:403–9. doi: 10.1016/j.jacc.2009.11.047. [DOI] [PubMed] [Google Scholar]
- 10.Scali ST, Goodney PP, Walsh DB, et al. National trends and regional variation of open and endovascular repair of thoracic and thoracoabdominal aneurysms in contemporary practice. J Vasc Surg. 2011;53:1499–505. doi: 10.1016/j.jvs.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matsumura JS, Cambria RP, Dake MD, et al. International controlled clinical trial of thoracic endovascular aneurysm repair with the Zenith TX2 endovascular graft: 1 year results. J Vasc Surg. 2008;47:247–57. doi: 10.1016/j.jvs.2007.10.032. [DOI] [PubMed] [Google Scholar]
- 12.Chaer RA, Vasoncelos R, Maroun LK, et al. Synchronous and metachronous thoracic aneurysms in patients with abdominal aortic aneurysms. J Vasc Surg. 2012;56:1262–5. doi: 10.1016/j.jvs.2012.04.056. [DOI] [PubMed] [Google Scholar]
- 13.Von Allmen RS, Anjum A, Powel JT. Incidence of descending aortic pathology and evaluation of the impact of thoracic endovascular aortic repair: a population based study in England and Wales from 1999 to 2010. Eur J Vasc Endovasc Surg. 2013;45:154–9. doi: 10.1016/j.ejvs.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 14.Gopaldas RR, Huh J, Dao TK, et al. Superior nationwide outcomes of endovascular versus open repair for isolated descending thoracic aortic aneurysm in 11,669 patients. J Thorac Cardiovasc Surg. 2010;140:1001–10. doi: 10.1016/j.jtcvs.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 15.Makaroun MS, Dillavou ED, Kee ST, et al. Endovascular treatment of thoracic aortic aneurysms: results of the phase II multicenter trial of the GORE TAG thoracic endoprosthesis. J Vasc Surg. 2005;41:1–9. doi: 10.1016/j.jvs.2004.10.046. [DOI] [PubMed] [Google Scholar]
- 16.Fairman RM, Criado FJ, Farber MA, et al. Pivotal results of the Medtronic Vascular Talent Stent Graft System: the VALOR trial. J Vasc Surg. 2008;48:546–54. doi: 10.1016/j.jvs.2008.03.061. [DOI] [PubMed] [Google Scholar]
- 17.Makaroun MS, Dillavou ED, Wheatley GH, Cambria RP. Five year results of endovascular treatment with the GORE TAG device compared with open repair of thoracic aortic aneurysms. J Vasc Surg. 2008;47:912–8. doi: 10.1016/j.jvs.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 18.Matsumura JS, Cambria P, Dake M, et al. Five-year results of thoracic endovascular aortic repair with the Zenith TX2. J Vasc Surg. 2014;60:1–10. doi: 10.1016/j.jvs.2014.01.043. [DOI] [PubMed] [Google Scholar]
- 19.Greenalgh RM, Brown LC, Powel JT, et al. Endovascular versus open repair of abdominal aortic aneurysms. N Engl J Med. 2010;362:1863–71. doi: 10.1056/NEJMoa0909305. [DOI] [PubMed] [Google Scholar]
- 20.Lederle FA, Freischlag JA, Kyriakides TC, et al. Long term comparison of endovascular and open repair of abdominal aortic aneurysm. N Engl J Med. 2012;367:1988–97. doi: 10.1056/NEJMoa1207481. [DOI] [PubMed] [Google Scholar]
- 21.Roselli EE, Abdel Halim M, Johnston DR, et al. Open aortic repair after prior thoracic endovascular aortic repair. Ann Thorac Surg. 2014;97:750–7. doi: 10.1016/j.athoracsur.2013.10.033. [DOI] [PubMed] [Google Scholar]
- 22.Appoo JJ, Moser WG, Fairman RM, et al. Thoracic aortic stent grafting: improving results with newer generation investigational devices. J Thorac Cardiovasc Surg. 2006;131:1087–94. doi: 10.1016/j.jtcvs.2005.12.058. [DOI] [PubMed] [Google Scholar]
- 23.Ellozy SH, Carroccio A, Minor M, et al. Challenges of endovascular tube graft repair of thoracic aortic aneurysm: midterm follow-up and lessons learned. J Vasc Surg. 2003;38:676–83. doi: 10.1016/s0741-5214(03)00934-0. [DOI] [PubMed] [Google Scholar]